Microparasitology Finals Lec - Parasitology (Protozoans v2)
1/523
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
524 Terms
What is the primary pathogenic amoeba responsible for intestinal amoebiasis?
Entamoeba histolytica.

What is the mode of transmission (MOT) for Entamoeba histolytica?
Ingestion of mature quadrinucleated cysts through contaminated food or water.

What are the two life stages of Entamoeba histolytica?
Trophozoite and Cyst.

What is the diagnostic stage of Entamoeba histolytica?
Trophozoite.
What are the symptoms of amoebic dysentery caused by Entamoeba histolytica?
Diarrhea, abdominal pain, chronic weight loss, anorexia, and fatigue.

What is the treatment for symptomatic infections caused by Entamoeba histolytica?
A combination of metronidazole (Flagyl) and diloxanide furoate (Furamide).
What is the role of encystation in the life cycle of Entamoeba histolytica?
Encystation occurs in the intestine, allowing the organism to survive outside the host.

What is the significance of the chromatoidal bars found in young Entamoeba histolytica?
They are a source of RNA.

What distinguishes Entamoeba coli from Entamoeba histolytica?
Entamoeba coli is non-pathogenic and typically asymptomatic.
What is the primary characteristic of Entamoeba polecki?
It can cause extraintestinal amoebiasis and is transmitted from human to human and pig to human.
What is the treatment for asymptomatic infections caused by Entamoeba histolytica?
Paromomycin or diloxanide furoate.

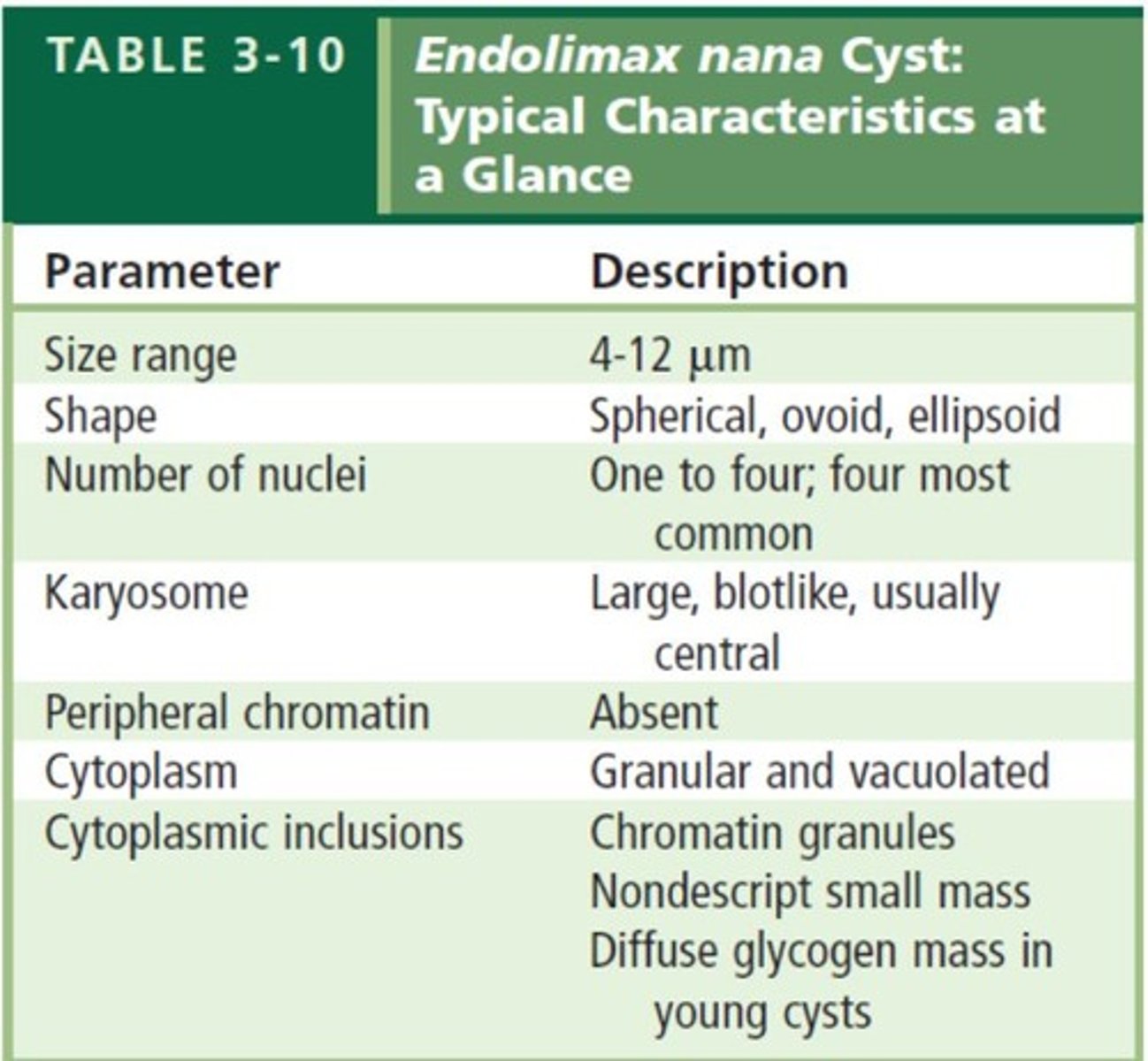
What is the most common form of cyst for Endolimax nana?
A mature cyst with 4 nuclei.
How can Entamoeba dispar be differentiated from Entamoeba histolytica?
Using DNA probes and electrophoresis techniques.

What is the motility characteristic of Entamoeba hartmanni?
Nonprogressive motility with finger-shaped pseudopods.
What is the specimen associated with Iodamoeba butschlii?
Trophozoites may be found in the gum line of the teeth, sputum, and pulmonary abscess.

What is the only known form of Iodamoeba butschlii to humans?
Trophozoite.

What is the significance of the karyosome in Entamoeba histolytica?
It is centrally located within the nucleus.

What are the potential complications of Entamoeba histolytica infection?
Migration to the liver causing extraintestinal amoebiasis.
What is the epidemiological significance of Entamoeba histolytica?
It is one of the leading causes of parasitic death, thriving in tropical and subtropical areas.

What laboratory methods are used for diagnosing Entamoeba histolytica?
Wet mount and permanent stain.
What is the role of flies and cockroaches in the transmission of Entamoeba histolytica?
They can act as vectors by contaminating food and water.
What is the primary characteristic of the cyst stage of Entamoeba histolytica?
It is resistant to chlorination and can survive in feces for long periods.
What is the typical number of nuclei found in Entamoeba histolytica?
1-4 nuclei.
What are trophozoites and where can they be found?
Trophozoites are the active form of certain protozoa, found in gingival pockets, sputum, pulmonary abscess, and vaginal and cervical specimens.
What is the replication method of trophozoites?
Trophozoites replicate through binary fission.
What is unique about the cyst stage of trophozoites?
There is no known cyst stage for some trophozoites, while others may have a cyst stage.
What is the mode of transmission (MOT) for trophozoites?
Transmission occurs through droplet contamination and contaminated drinking utensils.
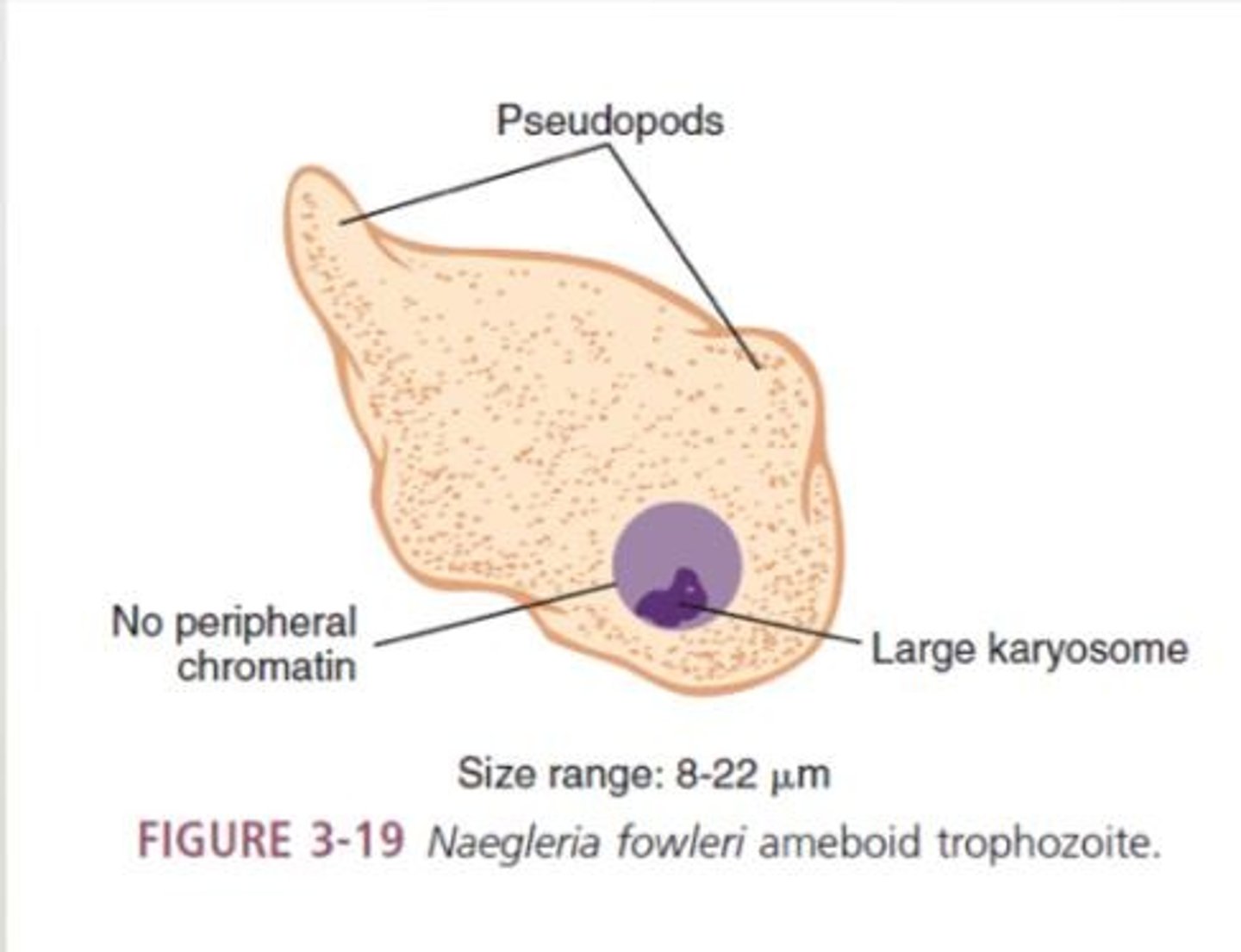
What is Naegleria fowleri and what disease does it cause?
Naegleria fowleri is a free-living amoeba that causes Primary Amoebic Meningoencephalitis.
What are the initial symptoms of Naegleria fowleri infection?
Symptoms include fever, headache, sore throat, nausea, vomiting, stiff neck, and seizures.
What is the typical outcome of Naegleria fowleri infection without treatment?
Death usually occurs within 3-6 days.
What are the morphological forms of Naegleria fowleri?
The three morphological forms are trophozoites, flagellates, and cysts.
What is the treatment for Naegleria fowleri infection?
Treatment includes Amphotericin B and miconazole.
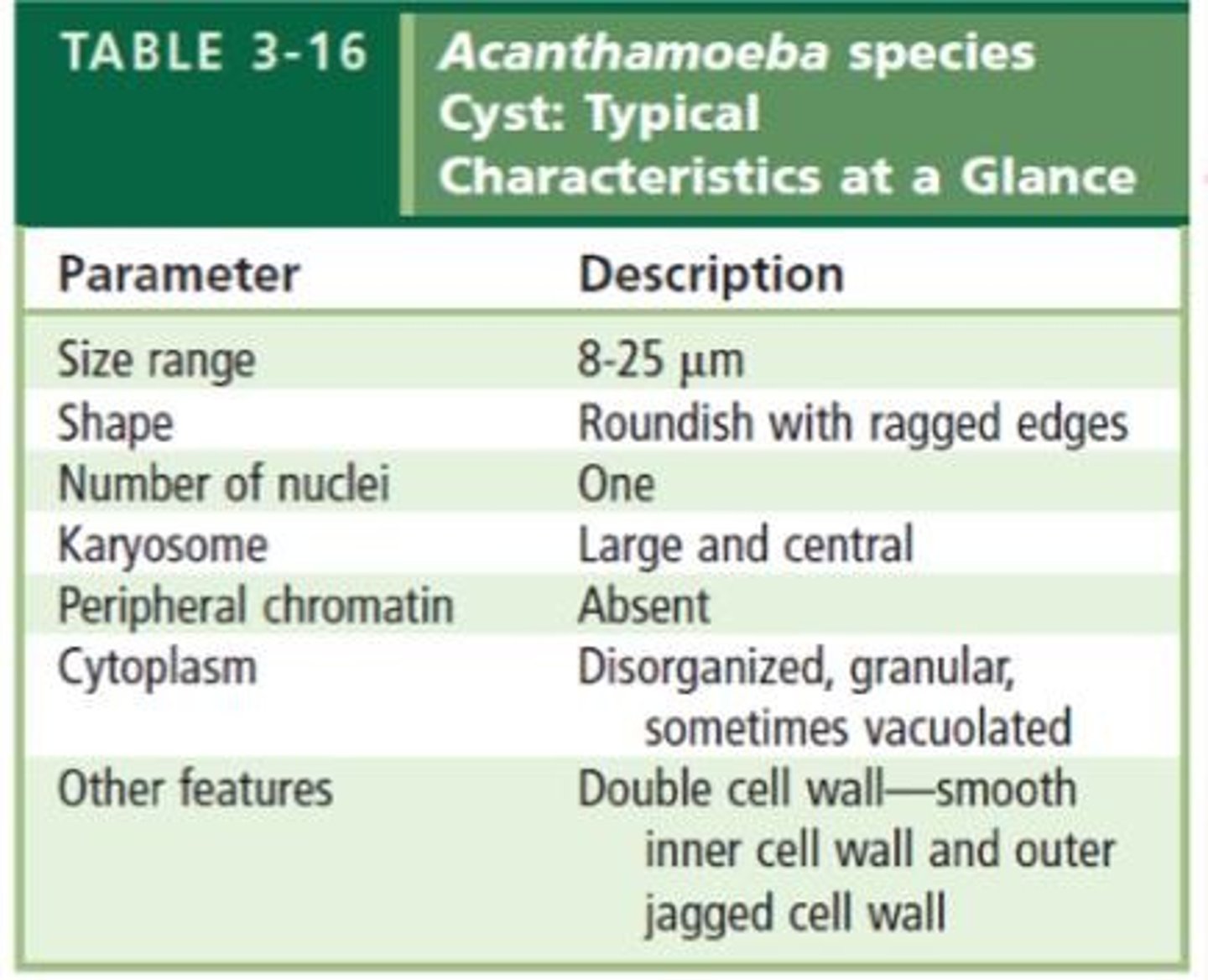
What conditions can Acanthamoeba spp. cause?
Acanthamoeba spp. can cause granulomatous amoebic encephalitis and Acanthamoeba keratitis.
What are the characteristics of Acanthamoeba?
Acanthamoeba has spine-like pseudopods known as acanthopodia and one nucleus.
What are the symptoms of granulomatous amoebic encephalitis?
Symptoms include headache, seizures, stiff neck, nausea, and vomiting.
What is amoebic keratitis and its main symptom?
Amoebic keratitis is an eye infection characterized by severe ocular pain and vision problems.
What is the most successful treatment for amoebic keratitis?
The most successful treatment is propamidine.
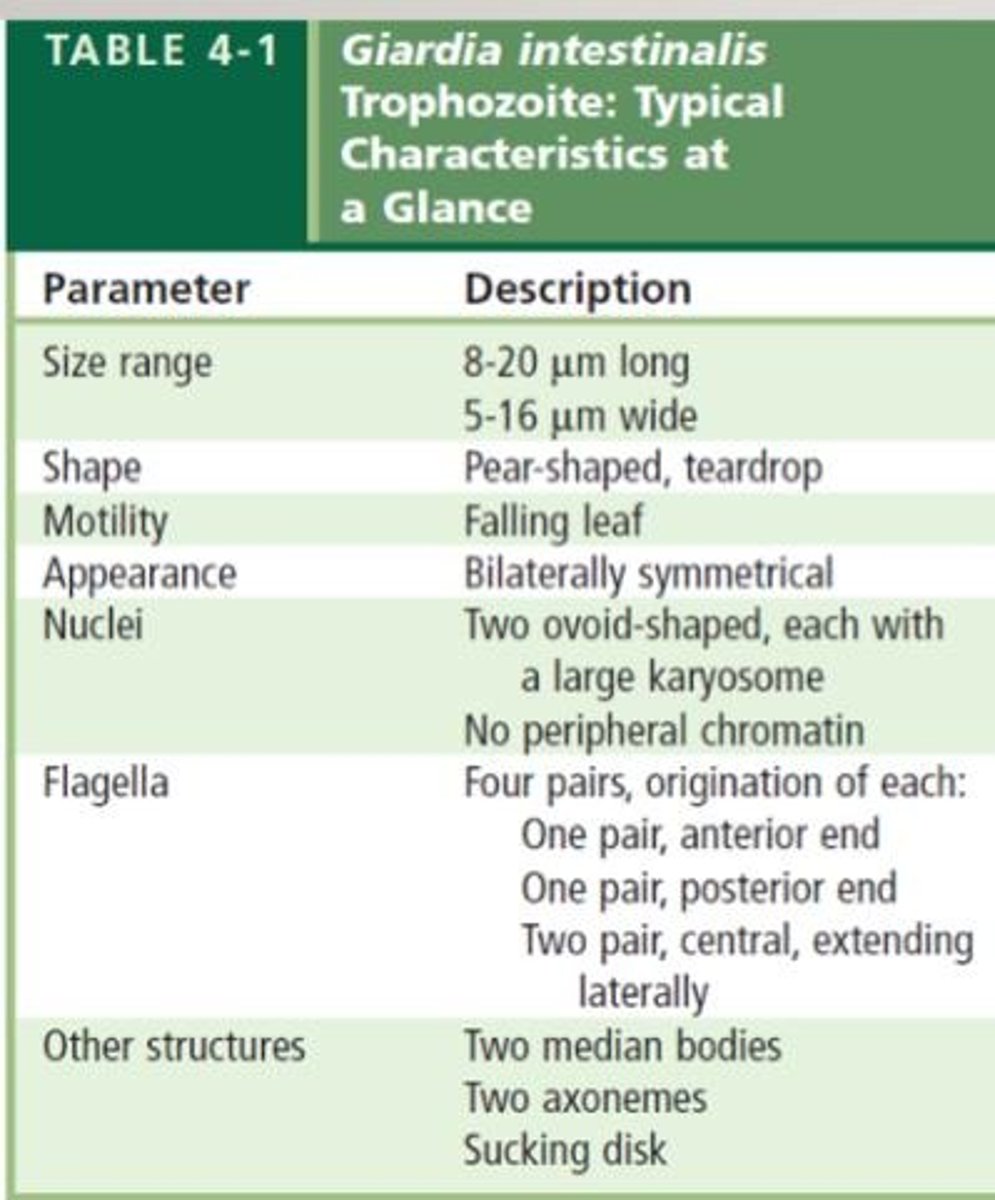
What is Giardia intestinalis and what disease does it cause?
Giardia intestinalis, previously known as G. lamblia, causes giardiasis or traveler's diarrhea.
What is the primary mode of transmission for Giardia intestinalis?
Transmission occurs through ingestion of contaminated food and water.
What are the morphological characteristics of Giardia intestinalis?
Giardia intestinalis has bilateral symmetry, two oval-shaped nuclei, a sucking disk, and median bodies.
What triggers the excystation of Giardia intestinalis?
Infective cysts enter the stomach, and gastric juice triggers excystation in the duodenum.
Who is at risk for infections caused by Acanthamoeba?
Contact lens wearers are at higher risk for Acanthamoeba infections.
What is the significance of the sucking disk in Giardia intestinalis?
The sucking disk helps Giardia intestinalis attach to the intestine, making it pathogenic.
What are the main symptoms of granulomatous lesions in the brain caused by amoebic infections?
Granulomatous lesions may lead to the presence of trophozoites and cysts, causing headaches, seizures, and other neurological symptoms.
What condition is caused by Acanthamoeba keratitis?
Trauma to the cornea.
How do trophozoites of Trichomonas tenax enter the body?
They enter via the lower respiratory tract or through ulcers.
What type of specimen is used to diagnose Trichomonas tenax?
Mouth scrapings from tonsillar crypts and pyorrhea pockets.
What is the mode of transmission (MOT) for Trichomonas tenax?
Use of contaminated dishes and utensils, and droplet contamination.
What are the symptoms of Giardiasis?
Mild diarrhea, abdominal cramps, and anorexia.
What is the treatment for Trichomonas vaginalis infection?
Tinidazole (Tindamax) and nitazoxanide (Alinia).
What is the prevention method for Trichomonas vaginalis infection?
Using double strength saturated iodine solution to treat contaminated water.
What is the characteristic of Diantemoeba fragilis nuclei?
One large karyosome with no peripheral chromatin.
What is the mode of transmission for Diantemoeba fragilis?
The exact mode of transmission is unknown.
What is the primary site of infection for Trichomonas vaginalis in males?
The prostate gland.
What are the symptoms of persistent urethritis in males?
Enlarged prostate, dysuria, nocturia, and epididymitis.
What is the infective stage of Psychodopygus?
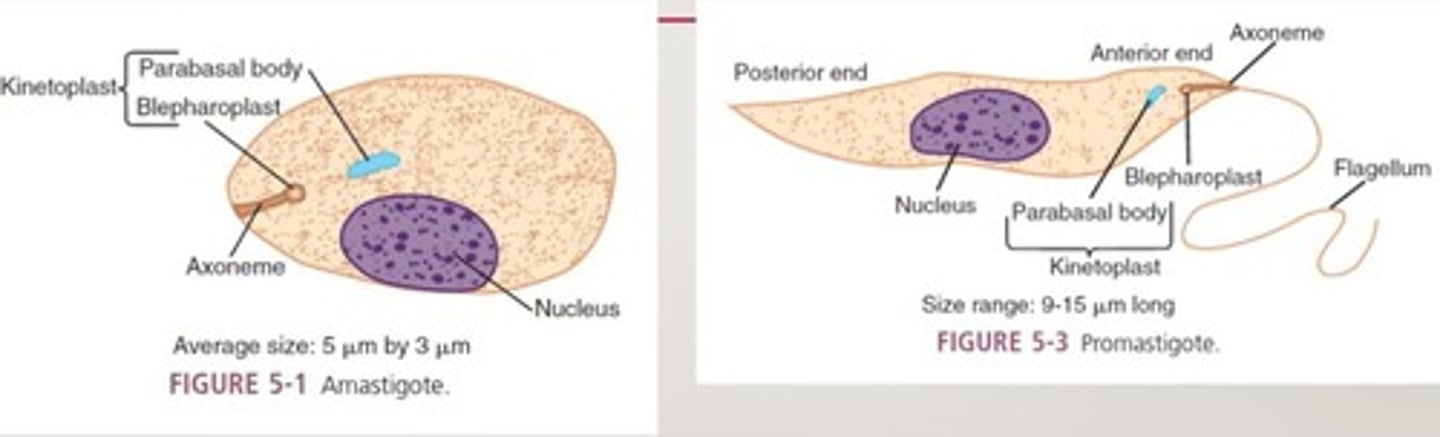
Promastigote.
What is the diagnostic stage of Psychodopygus?
Amastigote.
What is the life cycle of Leishmania spp. and Trypanosoma spp.?
Promastigotes invade the reticuloendothelial system (RES) and reproduce as amastigotes, causing tissue destruction.
What is the treatment for severe Trichomonas vaginalis infection?
Flagyl.
What is the symptom of Trichomonas vaginalis infection in women?
Foul smelling, greenish-yellow vaginal discharge.
What is the asymptomatic carrier state associated with Diantemoeba fragilis?
Most frequent in men.
What is the symptom of Trichomonas vaginalis infection?
Burning, itching, and chafing may be present.
What is the characteristic of the trophozoid stage of Trichomonas vaginalis?
It has an undulating membrane that aids in motion.
What is the symptom of persistent vaginitis caused by Trichomonas vaginalis?
Persistent vaginitis in women.
What is the mode of transmission for Trichomonas hominis?
Ingestion of infected milk or fecal-oral route.
What is a common symptom of Trichomonas vaginalis infection?
Thin, white urethral discharge.
What are the forms of Leishmania?
Amastigote, promastigote, epimastigote.
What is mucocutaneous leishmaniasis characterized by?
Large ulcers in the oral/nasal mucosa.
What is the mode of transmission (MOT) for mucocutaneous leishmaniasis?
Bite of an insect vector.
What is the diagnostic stage of mucocutaneous leishmaniasis?
Invasion of the reticuloendothelial system (RES).
What is a common cause of death in mucocutaneous leishmaniasis?
Secondary bacterial infection.
What is the treatment for mucocutaneous leishmaniasis?
Antimony compounds, such as sodium stibogluconate (Pentosam).
What is the Leishmania donovani complex associated with?
Visceral leishmaniasis, also known as kala-azar or dum dum fever.
What are the key symptoms of visceral leishmaniasis?
Fever, diarrhea, kidney involvement, and potential mental retardation.
What is the vector for Leishmania species?
Phlebotomus and Lutzomyia sandflies.
What is the Montenegro skin test used for?
Screening large populations at risk of leishmaniasis.
What are the symptoms of Leishmania braziliensis complex?
Hepatosplenomegaly and nondescript abdominal illness.
What is the treatment for Trypanosoma cruzi infection?
Amphotericin B (Ambisome).
What is the primary vector for Trypanosoma brucei?
Tsetse flies, specifically Glossina palpalis and Glossina tachioides.
What is the infective and diagnostic stage of Trypanosoma brucei?
Trypomastigotes.
What is the lifecycle of Trypanosoma brucei?
Trypomastigotes migrate to the lymphatic system and CNS after being bitten by a tsetse fly.
What is the causative agent of Nagana and sleeping sickness?
Trypanosoma brucei.
What are the symptoms of cutaneous leishmaniasis?
Small red papule with pruritis and single pus-containing ulcer.
What is the treatment for New World leishmaniasis?
Pentavalent antimonials (sodium stibogluconate).
What is the infective stage of Leishmania species?
Promastigotes.
What is the significance of amastigotes in Leishmania?
They are usually seen within macrophages.
What is the characteristic of the advanced stages of Leishmania mexicana complex?
Progression to an incurable diffuse cutaneous form of the disease.
What are the symptoms of Old World cutaneous leishmaniasis?
Dry or urban cutaneous sores, also known as Delhi boils or Baghdad boils.
What is the vector for Chagas disease?
The vector is the Phlebotomus fly.
What are the initial symptoms of Chagas disease?
Painful chancre (ulcer) with white halo at the bite site, fever, malaise, headache, and anorexia.
What is Romana's sign?
Conjunctivitis with unilateral edema of the eyelids.
What is a common treatment for Chagas disease?
Melarsoprol, suramin, pentamidine, and eflornithine.
What is the causative agent of East African sleeping sickness?
Trypanosoma brucei rhodesiense.
What are the symptoms of East African sleeping sickness?
Erythematous nodule (chagoma), fever, chills, fatigue, myalgia, and malaise.
What is the vector for East African sleeping sickness?
Glossina morsitans and Glossina pallidipes.
What is the treatment for East African sleeping sickness?
Nifurtrimox (Lampit).
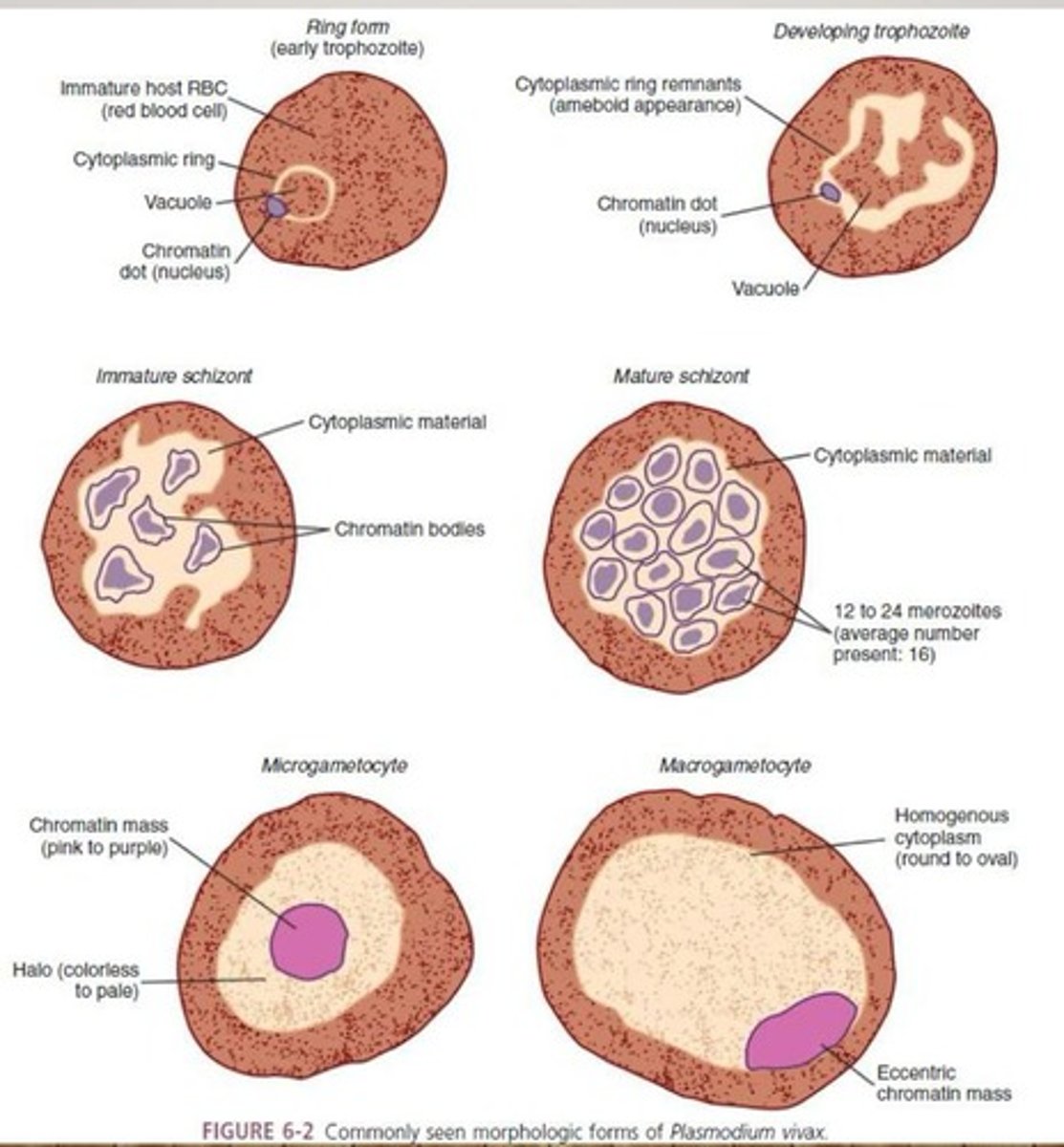
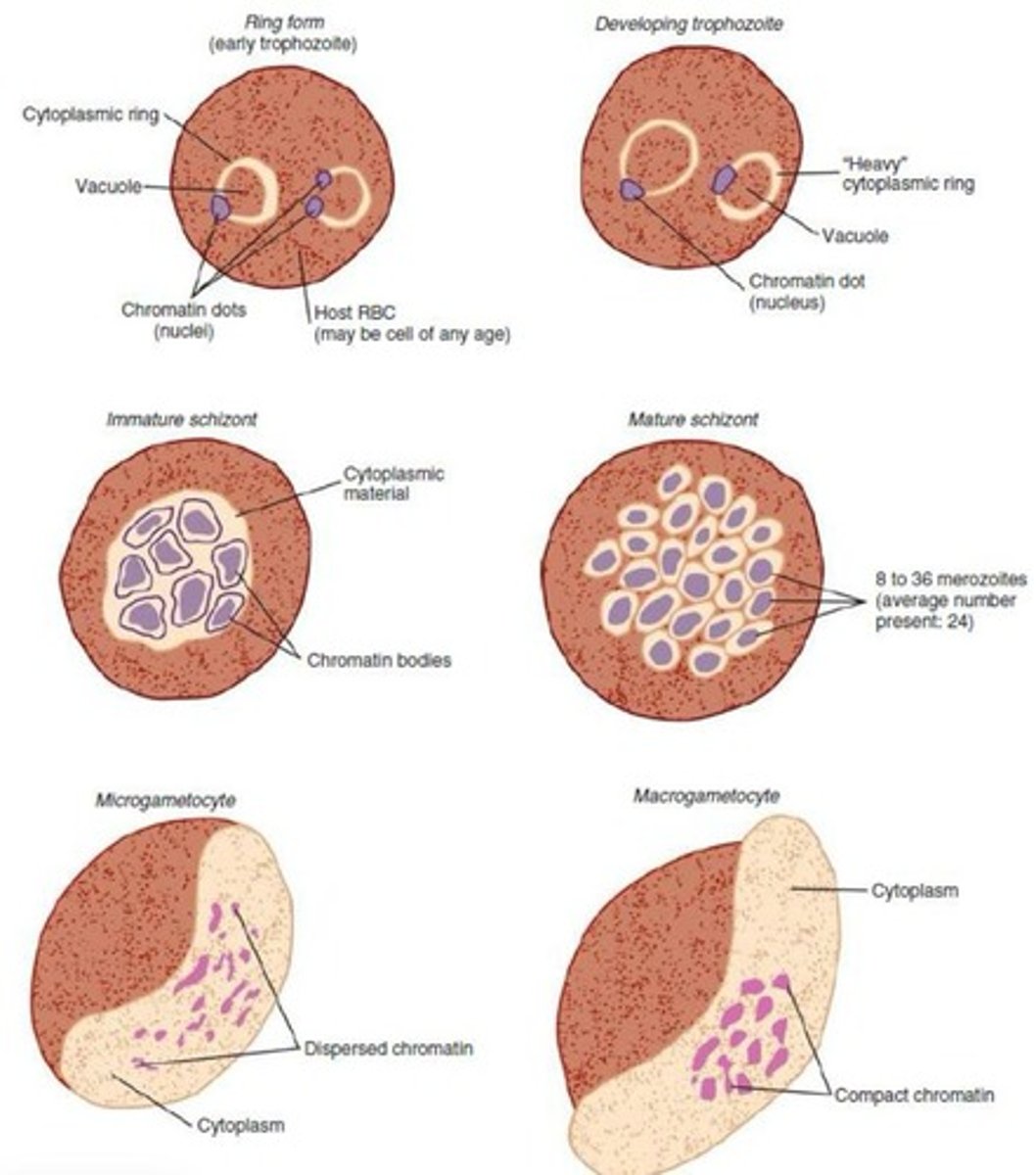
What are the morphological forms of Plasmodium spp. after RBC invasion?
Ring form/early trophozoite, developing trophozoite, immature schizont, mature schizont, microgametocytes, and macrogametocyte.
How is malaria transmitted?
Through the bite of an Anopheles mosquito, blood transfusion, or sharing of needles.
What is the life cycle of Plasmodium spp.?
Sporozoites are carried to hepatocytes, release merozoites that infect RBCs, which may develop into gametocytes ingested by mosquitoes.
What are the symptoms of benign tertian malaria?
Cold stage followed by fever, profuse sweating, extreme fatigue, headache, lethargy, and anorexia.