terms of pulmonary dysfunction - patho exam 4
1/104
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
105 Terms
a pattern seen where airflow obstruction is present, primarily impacting exhalation.
characterized by a reduced FEV1 and FVC (but to a lesser extent than FEV1) and reduced FEV1/FVC ratio (<0.7).
obstructive disease pattern
a pattern seen where lung tissue or chest wall compliance is decreased, limiting lung expansion.
characterized by a reduced FEV1 and FVC, but a normal FEV1/FVC ratio (>0.7)
restrictive disease patterns
subjective sensation of uncomfortable breathing or shortness of breath
dyspnea
a type of dyspnea that is accompanied by flaring of nostrils, use of accessory muscles of respiration, and retraction of intercostal spaces.
severe dyspnea
a type of dyspnea that is characterized by shortness of breath experienced during physical activity.
dyspnea on exertion
dyspnea that occurs when lying down, often relieved by sitting up.
orthopnea
awakening at night suddenly feeling short of breath and gasping for air, requiring the person to sit up or stand up for relief.
paroxysmal nocturnal dyspnea (PND)
a protective reflex (explosive expiration) that helps clear the upper airways by stimulating irritant receptors due to particles, mucus, inflammation, or foreign bodies.
cough
this type of cough resolves within 2-3 weeks (e.g., from URI, acute bronchitis, pneumonia, CHF).
acute cough
this type of cough lasts more than 3 weeks (or >7-8 weeks), often seen in smokers, chronic bronchitis, CA, postnasal drip, asthma, GERD.
chronic cough
coughing up bright red, frothy blood, typically with an alkaline pH.
hemoptysis
type of breathing that is present if the airway is obstructed, requiring increased effort.
labored breathing
this type of airway obstruction is characterized by a
low ventilation rate
increased effort
prolonged inspiration/expiration
stridor (high pitch)
wheezing
large airway obstruction
this type of airway obstruction is characterized by a rapid ventilation rate, small tidal volume, increased effort, prolonged expiration, wheezing, asthma/COPD
small airway obstruction
a breathing pattern characterized by smaller tidal volumes and a rapid ventilation rate, often due to conditions that decrease compliance (stiffened lungs or chest wall).
restricted breathing
inadequate alveolar ventilation relative to the body's metabolic demands causes this
hypoventilation
this type of ventilation leads to respiratory acidosis from an increase in arterial carbon dioxide (PaCO2 > 44mmHg).
hypoventilation
alveolar ventilation that exceeds the body's metabolic demands causes this
hyperventilation
this type of ventilation leads to respiratory alkalosis from a decrease in arterial carbon dioxide (PaCO2 < 36mmHg).
hyperventilation
a condition where the blood pH is less than 7.25
typically caused by hypoventilation leading to an increase in carbon dioxide.
respiratory acidosis
a condition where the blood pH is elevated (usually associated with decreased PaCO2)
typically caused by hyperventilation leading to a decrease in carbon dioxide.
respiratory alkalosis
a bluish discoloration of the skin and mucous membranes, resulting from desaturated hemoglobin.
cyanosis
a type of cyanosis caused by poor circulation, often best observed in the nail beds (e.g., Raynaud's disease).
peripheral cyanosis

a type of cyanosis caused by decreased arterial oxygenation, best observed in the buccal mucous membranes and lips (e.g., pulmonary or cardiac disease).
central cyanosis
right-to-left shunts cause decreased arterial oxygenation which is the direct cause of this type of cyanosis.
central cyanosis
this condition is due to an abnormal enlargement of the fingertips and toes
often due to chronic hypoxemia.
clubbing
a sharp or stabbing pain, usually caused by infection or inflammation of the parietal pleura (pleuritis/pleurisy)
pleural pain
a sharp or stabbing pain that can cause pain when the pleura is stretched during inspiration (e.g., pneumothorax).
pleural pain
continuous, dry grating, creaking sound caused by inflammation of pleural surfaces and loss of lubricating pleural fluid. this is accompanied with pleural pain
pleural friction rub
pain originating from the muscles or ribs, such as from a rib fracture, contusion, or costochondritis.
chest wall pain
this type of chest wall pain is characterized by an inflammation of the costochondral junction
- often caused by overuse of chest wall muscles (e.g., from severe coughing).
costochondritis
elevated levels of CO2 in the arterial blood (increased PaCO2), typically resulting from hypoventilation of the alveoli.
hypercapnia
decreased O2 levels in the arterial blood (decreased PaO2)
hypoxemia
reduced oxygen supply to cells and tissues
hypoxia
an abnormal ratio between alveolar ventilation (V) and pulmonary capillary perfusion (Q), which is the most common cause of hypoxemia.
V/Q mismatch
inadequate ventilation occurring in well-perfused areas of the lung (e.g., atelectasis, asthma, pulmonary edema, pneumonia) would result in this V/Q ratio
low V/Q ratio
poor perfusion occurring in well-ventilated portions of the lung, leading to "wasted ventilation" (e.g., pulmonary embolism) would result in this V/Q ratio
high V/Q ratio
A severe form of V/Q mismatch where blood passes through portions of the pulmonary capillary bed that receive no ventilation. this form would result in this V/Q ratio
very low V/Q (shunting)
gas exchange failure (failure of the lung tissue itself to adequately transfer gases) that is manifested by hypoxemia
respiratory failure caused by lung failure
ventilatory failure (Failure of the respiratory muscles or control center to move air effectively) that is manifested by hypercapnia
respiratory failure caused by pump failure
a life-threatening condition where gas exchange is inadequate. this is
often a mix of severe hypoxemia and/or hypercapnia, leading to a blood pH ≤ 7.25.
acute respiratory failure
respiratory failure due to poor alveolar ventilation.
pt needs ventilatory support
hypercapnic respiratory failure
respiratory failure due to poor exchange of oxygen between alveoli and capillaries
hypoxemic respiratory failure
conditions that limit the chest wall's ability to expand fully, increasing the work of breathing and compromising ventilation due to deformity, trauma, immobilization, or neuromuscular disease.
chest wall restriction
conditions such as muscular dystrophy, myasthenia gravis, or Guillain-Barré syndrome that impair respiratory muscle function due to chest wall restrictions
neuromuscular disease (affecting respiration)
the instability of a portion of the chest wall resulting from multiple rib or sternal fractures (three or more contiguous ribs broken in two or more places), causing paradoxical chest wall movement
flail chest
paradoxical chest wall movement (moving inward during inspiration, outward during expiration) is seen in this condition
flail chest
the presence of air in the pleural space, causing part or all of the lung to collapse.
pneumothorax (collapsed lung)
this type of pneumothorax occurs unexpectedly in healthy individuals (men, 20-40 years) without obvious cause.
primary (spontaneous) pneumothorax
this type of pneumothorax is caused by underlying lung disease (e.g., COPD), trauma, or injury.
secondary pneumothorax
this type of pneumothorax is caused by medical treatments or procedures (e.g., transthoracic needle aspiration).
iatrogenic pneumothorax
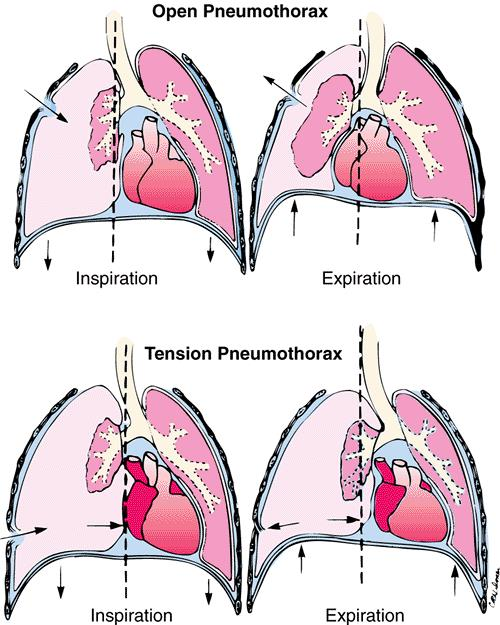
a life-threatening type of pneumothorax that leads to a rapid buildup of pressure that collapses the lung and shifts mediastinal structures, interfering with venous return to the heart.
tension pneumothorax
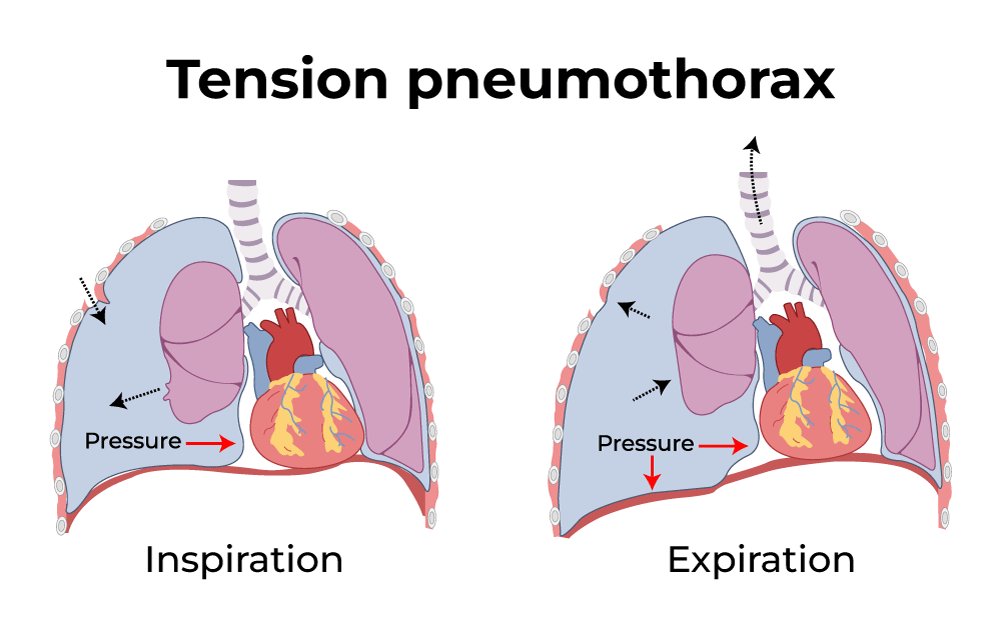
a life-threatening type of pneumothorax where a flap-valve leak allows air to enter the pleural space during inspiration but prevents its escape during expiration
tension pneumothorax
an open wound in the chest wall that allows free communication between the pleural space and the atmosphere, meaning air can move in and out of the chest wall opening, impairing effective ventilation.
open pneumothorax
the presence of abnormal fluid in the pleural space is termed a
pleural effusion
this type of pleural effusion includes watery fluid that diffuses out of capillaries (e.g., in congestive heart failure).
transudative effusion
this type of pleural effusion includes fluid with high concentrations of white blood cells and plasma proteins (e.g., from inflammation, infection, or cancer).
exudative effusion
this type of pleural effusion includes milky fluid (lymph/fat) in the pleural space, often from injury, infection, or a specific disorder.
chylothorax
the presence of blood within the pleural cavity
hemothorax
an infected pleural effusion, meaning there is pus within the pleural space.
empyema
a group of conditions characterized by decreased compliance of lung tissue, meaning the lungs are stiff and require more effort to inflate, resulting in dyspnea, increased respiratory rate, and decreased tidal volume.
restrictive lung disorders
the passage of fluid and solid particles into the lungs, most frequently affecting the right lower lobe.
aspiration
collapse of lung tissue
atelectasis
this type of atelectasis is caused by external compression on the lung (e.g., tumor, fluid, air).
compression atelectasis
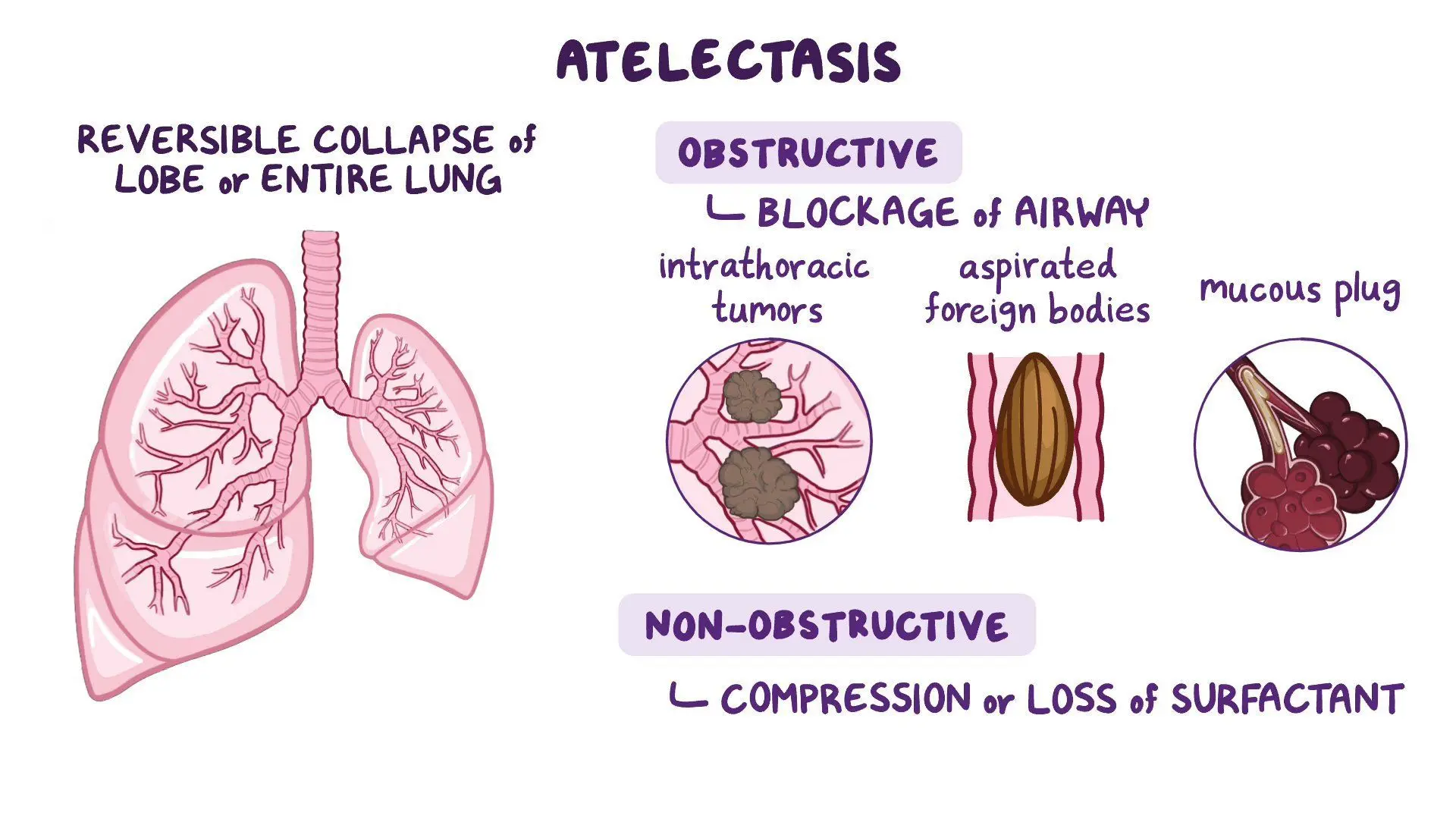
this type of atelectasis occurs due to gradual absorption of air from obstructed or hypo ventilated alveoli, or from inhalation of concentrated oxygen
absorption atelectasis
this type of atelectasis results from decreased production or inactivation of surfactant, which is necessary to reduce surface tension and prevent alveolar collapse.
surfactant impairment/contraction atelectasis
a persistent and abnormal dilation of the bronchi, caused by chronic bronchial inflammation
bronchiectasis
a diffuse inflammation of the bronchioles, most common in children, but can also occur in adults with chronic bronchitis, viral infections, or inhalation of toxic gases.
bronchiolitis
a late-stage fibrotic disease of the airways that causes permanent scarring of the lungs, often observed after lung transplantation or as a complication of bronchiolitis.
bronchiolitis obliterans
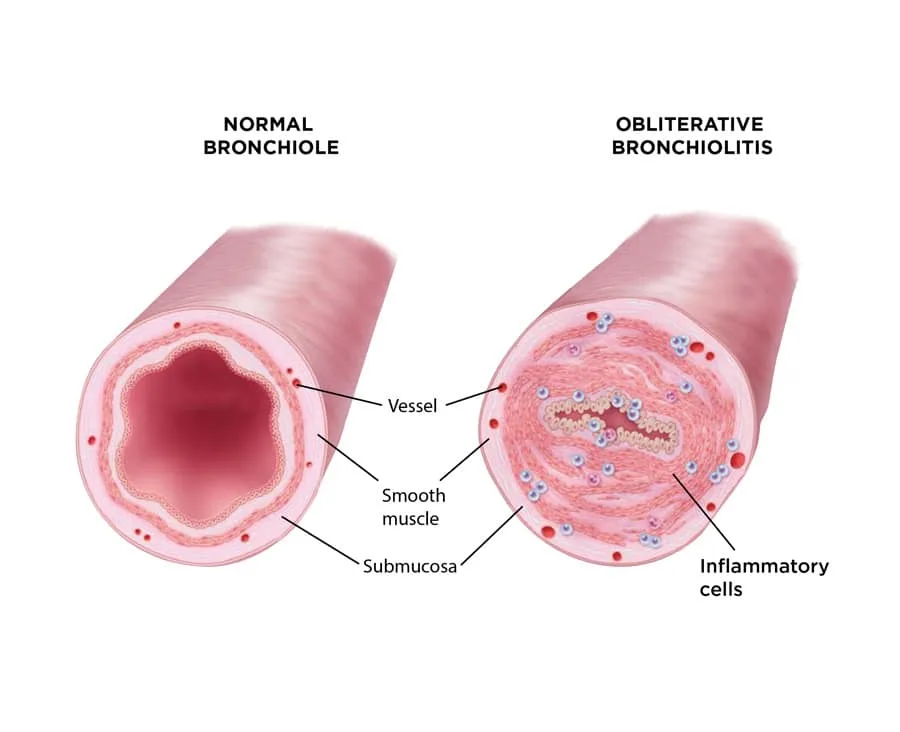
a specific type of bronchiolitis obliterans that is complicated by pneumonia
bronchiolitis obliterans organizing pneumonia (BOOP)
a condition characterized by an excessive amount of fibrous or connective tissue in the lung, making the lung stiff and poorly compliant, often due to chronic inflammation or exposure to irritants
pulmonary fibrosis
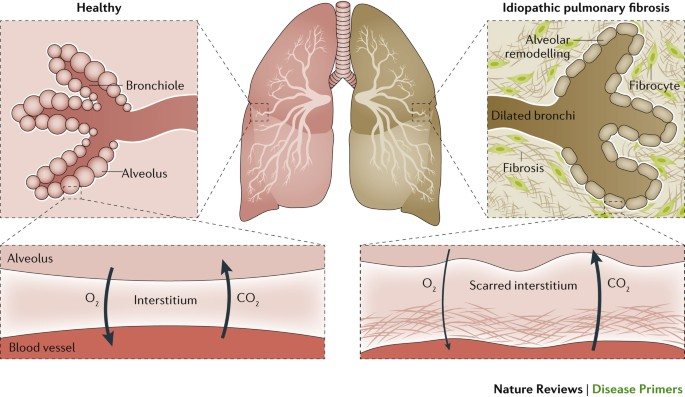
the most common idiopathic (unknown cause) lung disorder, involving chronic inflammation and fibro-proliferation of the interstitial lung tissue.
idiopathic pulmonary fibrosis (IPF)
a group of lung diseases caused by the inhalation of inorganic dust particles (e.g., silicosis, asbestosis, coal worker pneumoconiosis), leading to chronic inflammation and scarring (pulmonary fibrosis).
pneumoconiosis
an immune-mediated lung disease caused by the inhalation of organic particles or fumes (e.g., bird droppings, wood dust)
hypersensitivity pneumonitis (extrinsic allergic alveolitis)
a severe inflammatory response in the lungs caused by prolonged exposure to high concentrations of supplemental oxygen, leading to damage of alveolo-capillary membranes and surfactant disruption.
oxygen toxicity
excess water in the lung, resulting from disturbances in capillary hydrostatic pressure, oncotic pressure, or capillary permeability
pulmonary edema
severe forms of respiratory failure characterized by acute lung inflammation and diffuse alveolocapillary injury
Acute Lung Injury (ALI) / Acute Respiratory Distress Syndrome (ARDS)
a category of lung disorders characterized by airway obstruction that is worse during expiration, requiring more force and time to exhale, often presenting with dyspnea and wheezing.
obstructive pulmonary disease
a chronic inflammatory disorder of the bronchial mucosa
asthma
a severe, life-threatening asthma attack characterized by bronchospasm that is not reversed by usual measures.
status asthmaticus
a progressive and generally irreversible airflow limitation that arises from an abnormal inflammatory response of the lung to noxious particles or gases
chronic obstructive pulmonary disease (COPD)
a type of COPD defined by hypersecretion of mucus and a chronic productive cough that lasts for at least 3 months of the year for at least 2 consecutive years.
chronic bronchitis
a type of COPD characterized by abnormal, permanent enlargement of the gas-exchange airways accompanied by the destruction of the alveolar walls without obvious fibrosis, leading to a loss of elastic recoil.
emphysema
this type of emphysema is caused by an inherited deficiency of the enzyme α1-antitrypsin.
primary emphysema
this type of emphysema is primarily caused by cigarette smoke
secondary emphysema
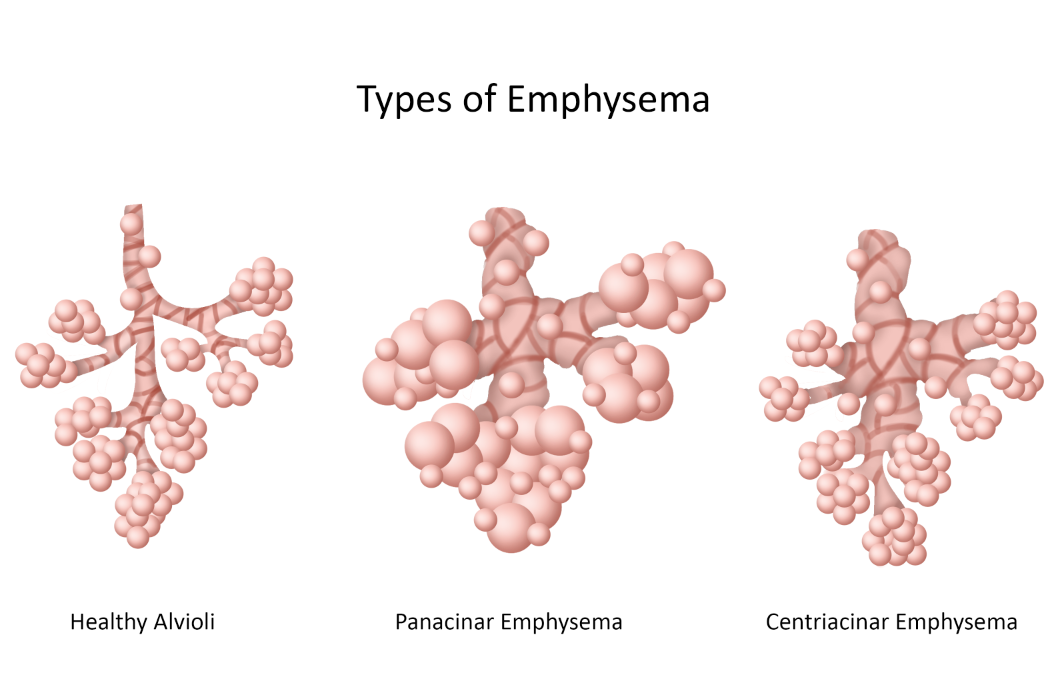
this type of emphysema affects respiratory bronchioles and alveolar ducts, typically in the upper lobes, and is often seen in smokers.
most common
centriacinar (centrilobular) emphysema
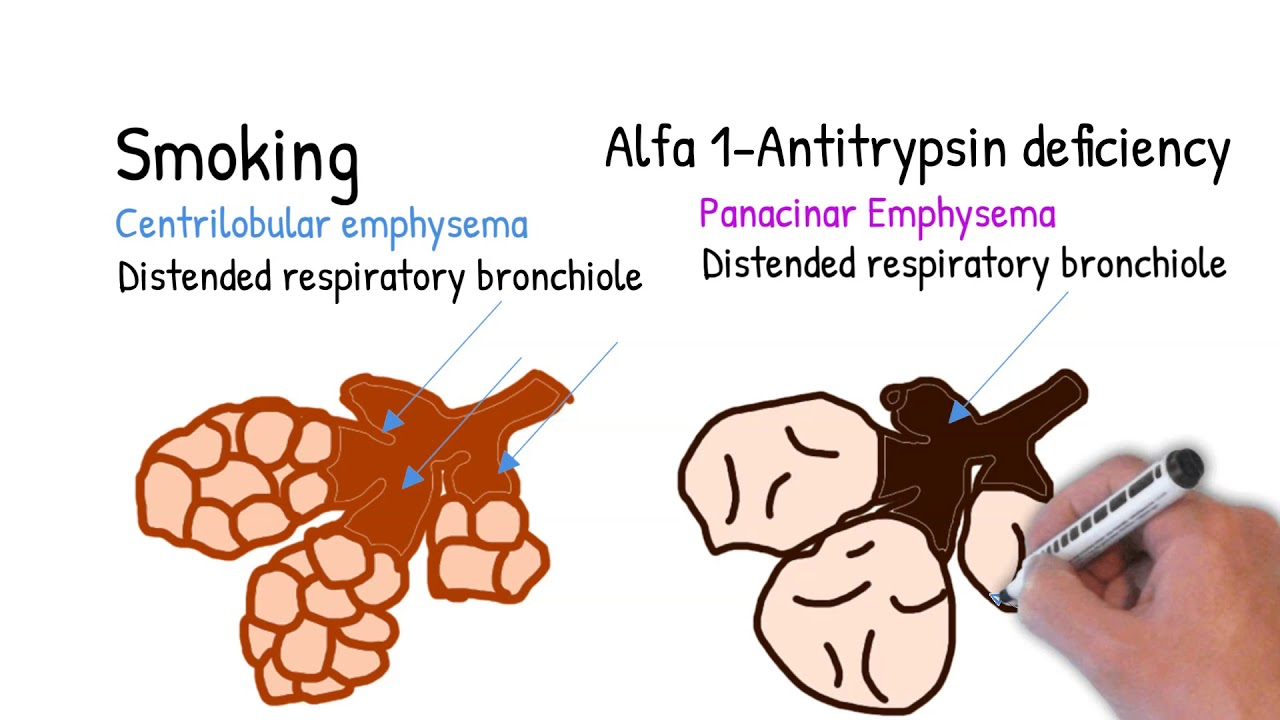
this type of emphysema Involves the entire acinus, uniformly damaged, often associated with alpha-1 antitrypsin deficiency and involves the lower lobes.
panacinar (panlobular) emphysema
a type of infection that occurs in very young, very old, or those with impaired immunity. examples: pneumonia, TB, abscess, and acute bronchitis
lower respiratory tract infections
an infection of the lower respiratory tract (bronchioles or alveoli) caused by viruses, bacteria, fungi, protozoa, or parasites, leading to an inflammatory response within the lung tissue.
pneumonia
a type of pneumonia caused by a viral infection (e.g., influenza), often seasonal and self-limiting, which can destroy ciliated epithelial cells and predispose to secondary bacterial infections.
viral pneumonia
a chronic infectious disease caused by Mycobacterium tuberculosis, an acid-fast bacillus, characterized by the formation of granulomatous lesions and caseous necrosis in the lungs.
tuberculosis
a circumscribed area of pus formation and destruction of lung parenchyma, often following consolidation of lung tissue and can form a cavity.
abscess formation (lung abscess)
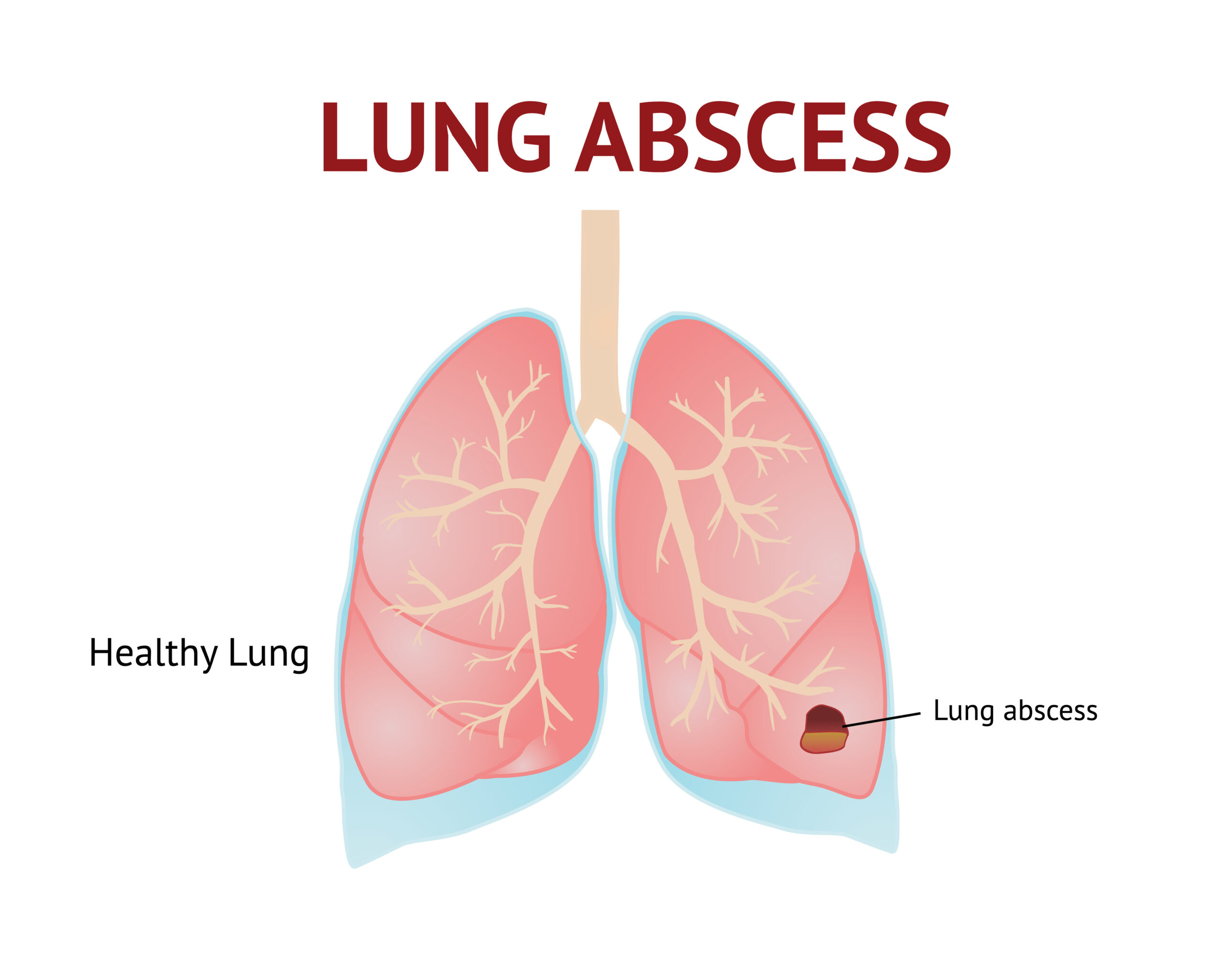
the process of a lung abscess emptying into a bronchus, leaving a cavity within the lung tissue.
cavitation (lung)
an acute infection or inflammation of the airways or bronchi, commonly following a viral illness
acute bronchitis
an acute infection presenting with symptoms similar to pneumonia but without pulmonary consolidation or chest infiltrates.
acute bronchitis
the occlusion of a portion of the pulmonary vascular bed by a thrombus, embolus, tissue fragment, lipids, or air bubble
most commonly originating from deep veins in the thigh.
pulmonary embolism (PE)
high blood pressure within the blood vessels of the lungs (pulmonary arteries), defined as a mean pulmonary artery pressure above 25 mm Hg at rest, eventually leading to right-sided heart failure.
pulmonary artery hypertension (PAH)
malignant growth affecting the larynx, with risk factors including tobacco smoke, alcohol consumption, gastroesophageal reflux disease, and human papillomavirus (HPV).
laryngeal cancer
malignant tumors originating in the bronchi or lung tissue, the most frequent cause of cancer death, with cigarette smoking being the primary risk factor.
bronchogenic carcinomas (lung cancers)
a category comprising about 85% of all lung cancers with three different types
non-small-cell lung cancer (NSCLC)