Pathophysiology II - Exam 2/CBL 1 - Peptic Ulcer Disease 💊
1/52
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
53 Terms
why is understanding the incidence and prevalence of peptic ulcer disease (PUD) so difficult?
due to variability in...
- H. pylori infection
- NSAID use (occurs in 15-30% of chronic NSAID users)
- cigarette smoking
*there is also varying sensitivity and specificity of Sx and diagnostic tests used to detect ulcers
PUD is one of the most common GI diseases, resulting in...?
- impaired quality of life
- work loss
- high-costs
how do gender, age, and race/ethnicity impact the epidemiology of PUD?
gender
- similar prevalence, but mortality rates are higher in MALES
age
- prevalence and mortality rates increase with age (especially >65 yo)
- gastric ulcers are most common in the ELDERLY, while duodenal ulcers are most common in MIDDLE-AGED patients
race/ethnicity
- African Americans and Hispanics continue to see disparities in H. pylori infection
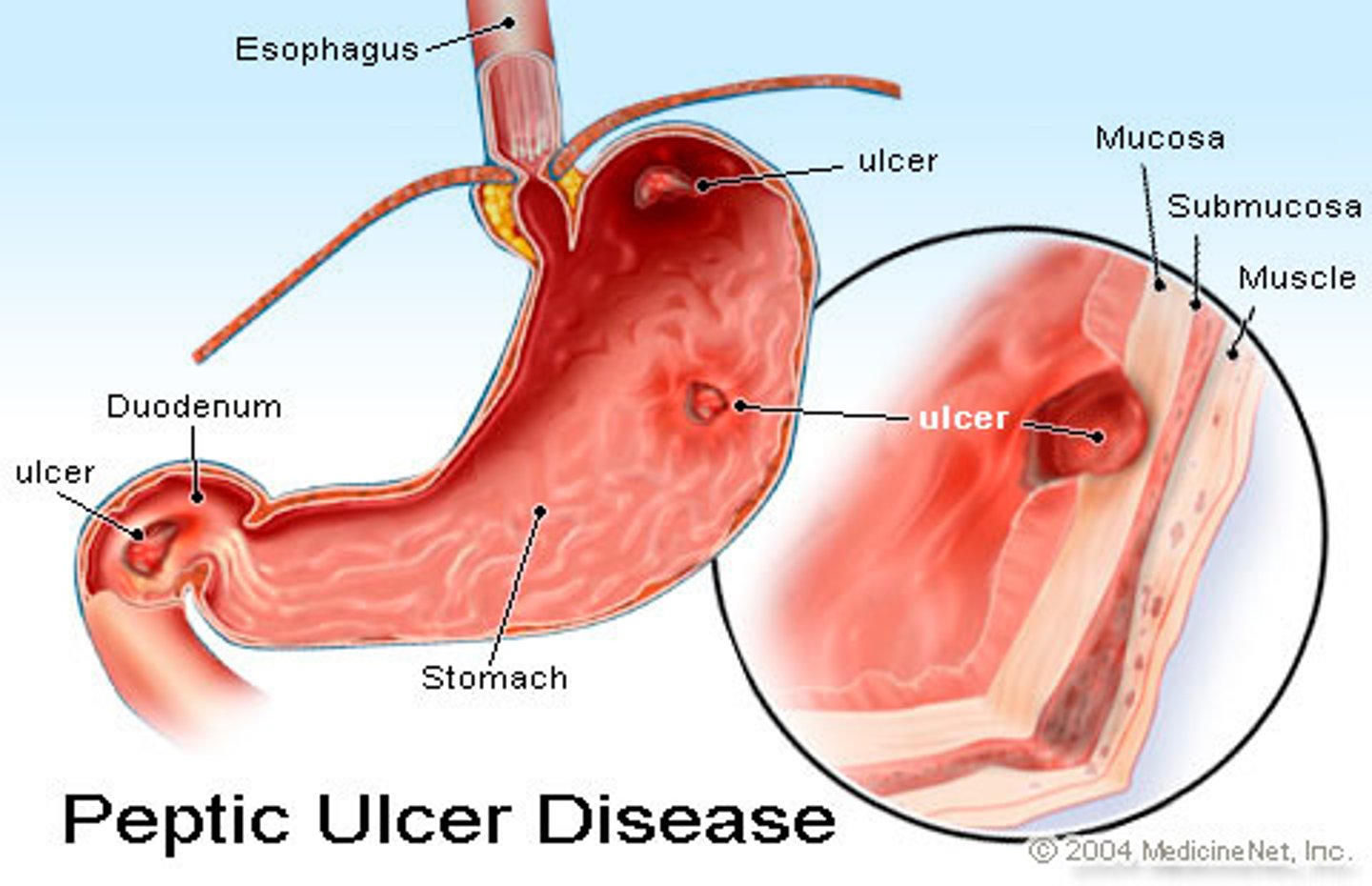
what is PUD? how big do ulcers tend to be?
damage to gastric or duodenal mucosa caused by impaired mucosal defense and/or increased acidic gastric contents; erosion of the GI tract
- ulcers 5+ mm in size
- can extend into the muscularis mucosa
what characterizes chronic PUD?
frequent ulcer recurrence
- exacerbations and remissions
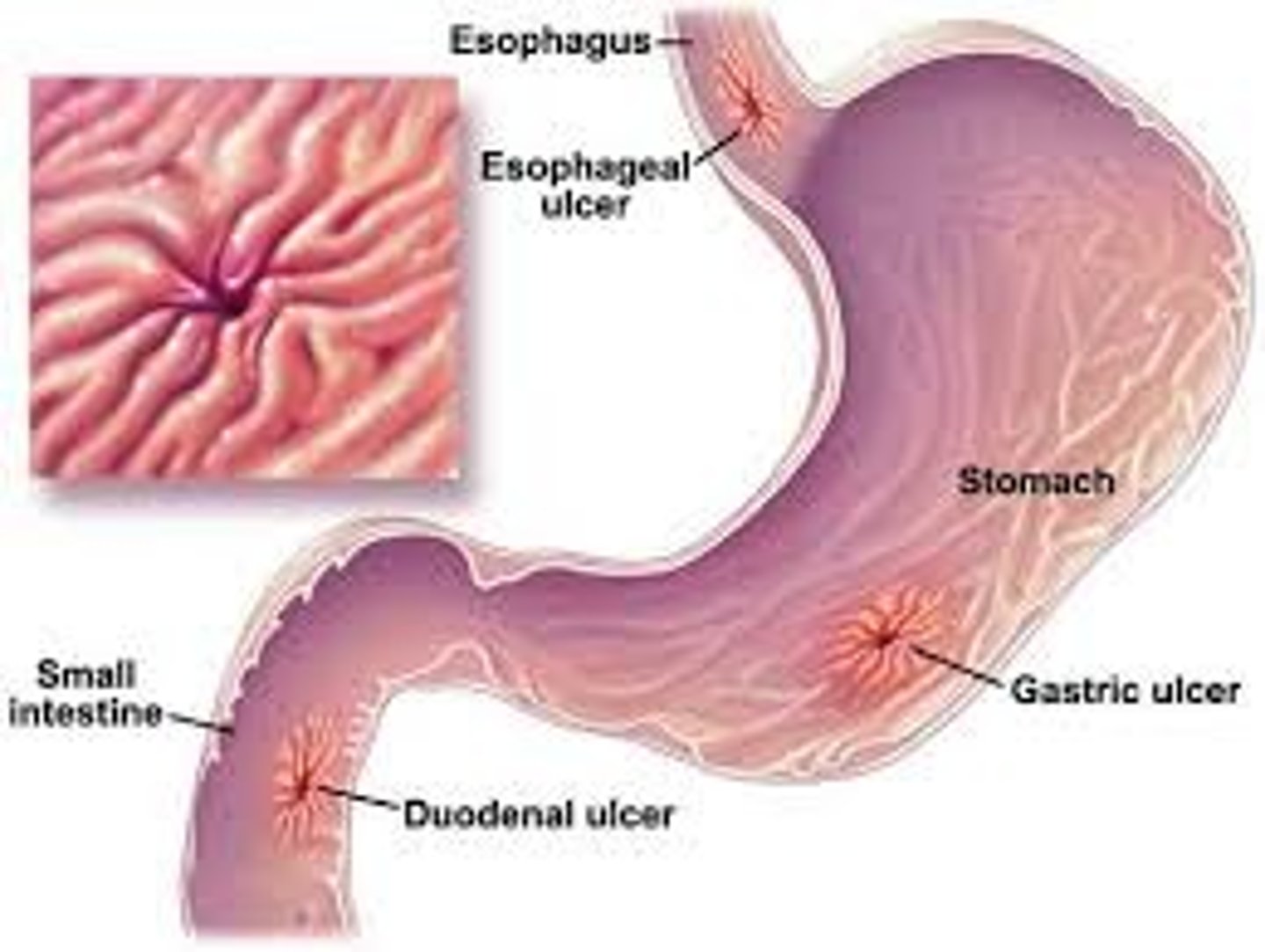
what are the most common locations of PUD?
- duodenal (duodenum)
- gastric (stomach)
- less commonly: esophagus, colon, ileum, jejunum
what are the common causes of PUD?
- H. pylori infection
- NSAIDs
- stress-related mucosal damage (SRMD) → associated with critical illness
what are the uncommon causes of PUD?
- hypersecretion of gastric acid (ex: Zollinger-Ellison syndrome {ZES})
- viral infections (ex: cytomegalovirus)
- Chron's disease (infiltrating disease)
- vascular insufficiency
- radiation
- chemotherapy
- idiopathic (unknown) causes
in addition to the common causes, what are the most prevalent risk factors of PUD?
- cigarette smoking
- alcohol use
- gastric acid hypersecretion
- medication non-adherence
- *stress/diet → controversial; may be indirectly related to PUD development
what is the pathophysiology of PUD? list the key players
physiologic imbalance between acid secretion and protective factors; key players:
- pepsin
- gastric acid
list the producing cell type, activation mechanism, and resulting action of pepsin in the context of PUD
- produced by: chief cells (produce pepsinogen, which is the inactive precursor of pepsin)
- activation: acidic environment (optimal pH of 1.8-3.5)
- resulting action: proteolytic activity involved in ulcer formation
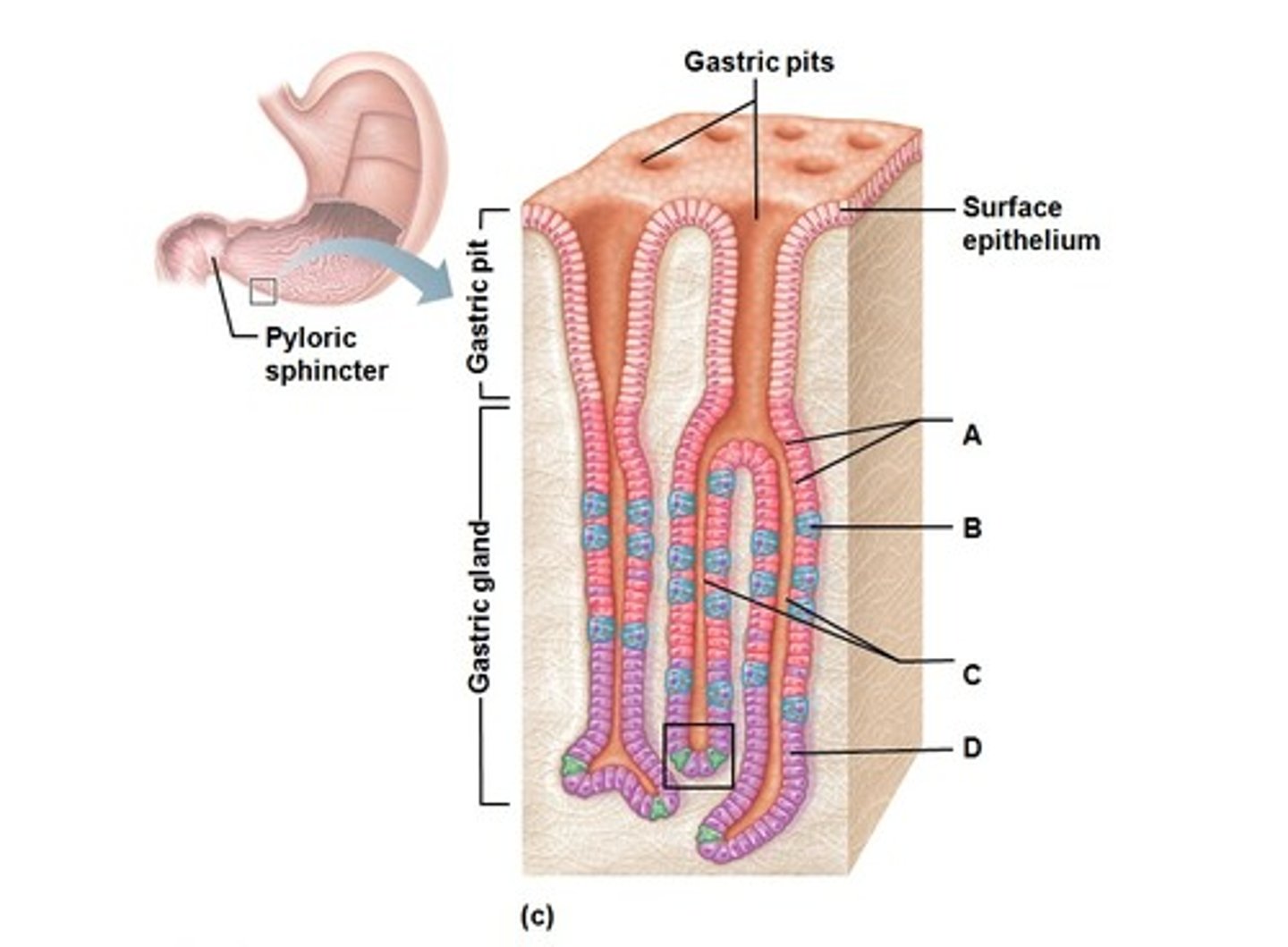
list the producing cell type, activation mechanism, and resulting action of gastric acid in the context of PUD
- produced by: parietal cells
- activation: histamine, gastric acid, and ACh R's
- resulting action: disruption of mucosal integrity
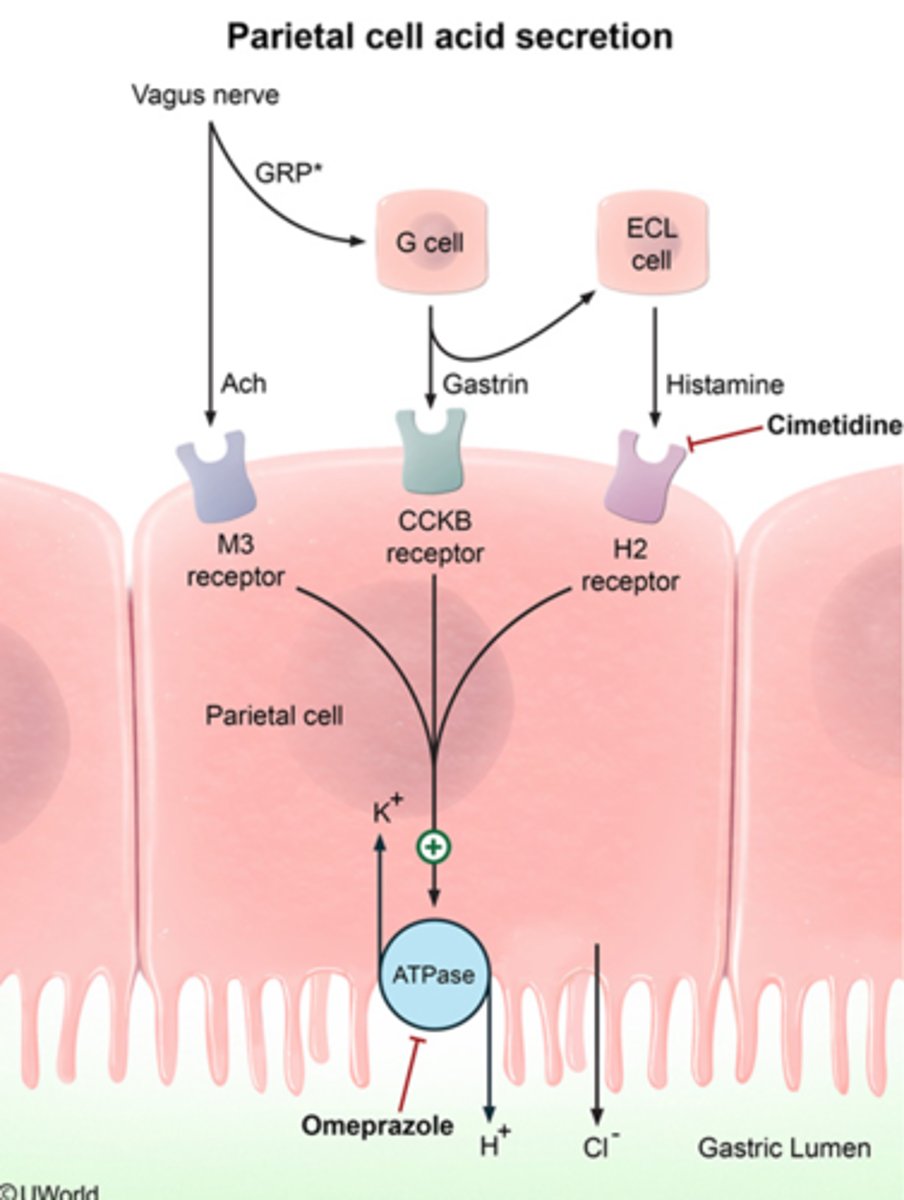
what are basal and maximal acid outputs? these values vary based on...?
- basal acid output (BAO): amount of acid secreted under FASTING conditions; follows the circadian rhythm (highest at night, low in the morning)
- maximal acid output (MAO): amount of acid secreted after maximal stimulation
vary based on...
- time of day
- physiological/health status
- age/gender
a high BAO:MAO ration = ____________
basal hypersecretory state
list the 6 main protective mechanisms against PUD and the related pathogenic factors
- mucosal defense ← H. pylori, reflux (bile, pancreatic)
- mucous bicarbonate layer ← excess pepsin and gastric acid
- prostaglandins ← meds.
- epithelial resistance ← meds.
- epithelial cell renewal ← alcohol
- preservation of vascular flow ← smoking
what are the 3 layers of the mucosal defense system?
pre-epithelial, epithelial, and sub-epithelial
describe the pre-epithelial layer of the mucosal defense system
mucus-bicarbonate-phospholipid layer
- viscous physiochemical barrier
- gastroduodenal surface epithelial cells secrete...
--- mucus: prevents diffusion of acidic H+ ions and gastric contents
--- bicarbonate: produces neutral pH at the epithelial surface (pH 6-7)
describe the epithelial layer of the mucosal defense system
surface epithelial cells
- mucus production
- ionic transporters → maintain pH, bicarbonate production
- heat shock protein production → prevent denaturation
- cell surface protection and regeneration
what happens in the epithelial layer when the pre-epithelial barrier is damaged?
restitution (restoration of damaged cells)
- alkaline pH and continuous blood flow are needed to incorporate GFs for the modulation of this process → epidermal GF (EGF), transforming GF α (TGF), fibroblast GF (FGF)
what happens if restitution in the epithelial layer is inadequate?
- cell proliferation (regeneration): regenerated by prostaglandins and GFs (EGF, TGF)
- angiogenesis: formation of new blood vessels regulated by FGF and vascular endothelial GF (VEGF)
describe the sub-epithelial layer of the mucosal defense system
microvascular system
- neutralizes acid through bicarbonate production
- provides micronutrients and O2
- removes toxic metabolic byproducts
what are the primary characteristics of gastric and duodenal ulcers?
gastric
- normal or decreased acid secretion
- inflammation causes breakdown of mucosal defense mechanisms
duodenal
- increased acid secretion and gastric emptying
- decreased bicarbonate secretion
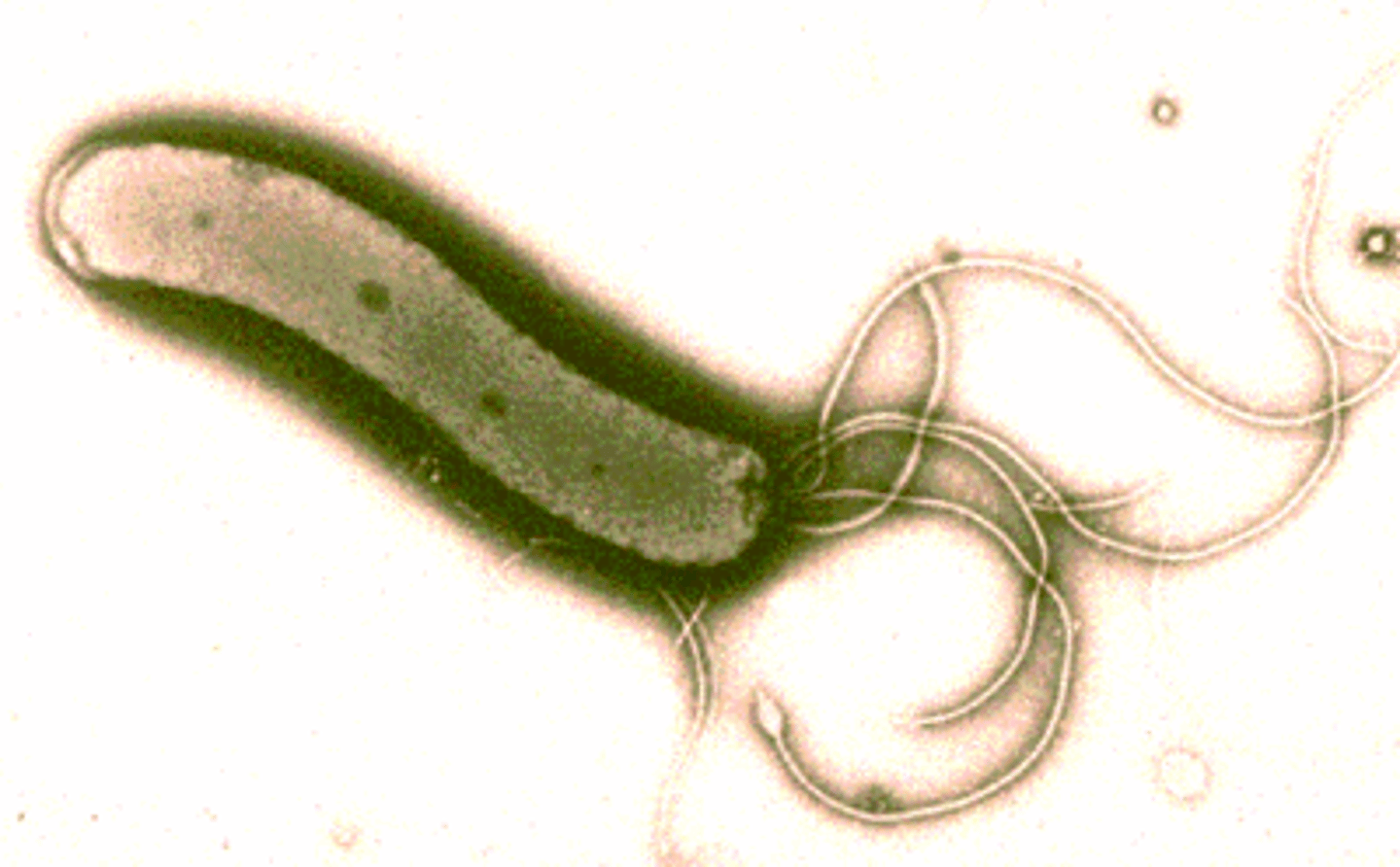
describe the 3 primary survival mechanisms of H. pylori
gram-(-), pH-sensitive bacteria
- spiral shape and flagellum allows it to move into the mucus layer (pH neutral)
- urease production → hydrolyzes urea in the gastric secretions and converts it to ammonia and CO2
- acid inhibitory protein production
how does H. pylori affect the GI tract? what is the resulting condition?
produces toxins that cause direct mucosal damage and alter the host's immune/inflammatory responses
- bacterial enzymes (urease, protease, lipase) degrade gastric mucus
- adherence enhances the uptake of toxins into gastric cells
- H. pylori virulence factors (vary by strain)
results in chronic gastritis
T/F: being (+) for H. pylori infection automatically indicates PUD
FALSE
- LINKED to PUD, but does not automatically indicate PUD
- linked to 10-15% of PUD cases, 1% of gastric cancer cases, and MALT lymphoma
how is H. pylori transmitted?
usually acquired in childhood; transmission:
- person to person → gastro-oral (vomitus), fecal-oral (diarrhea)
- unsterilized endoscopes
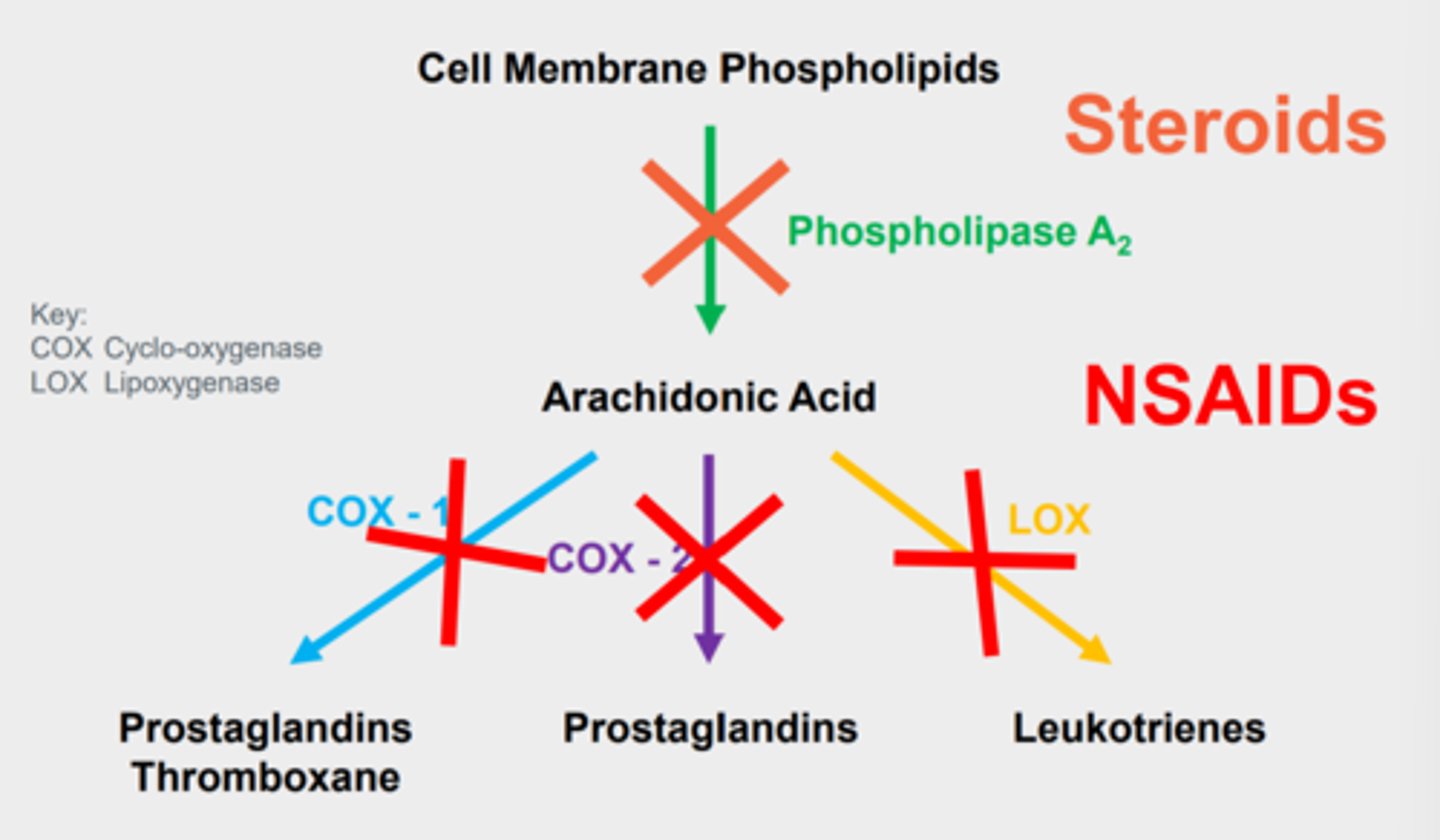
how do NSAIDs cause PUD?
- systemic inhibition of prostaglandins → prostaglandins normally have a cytoprotective effect on the GI tract
- direct irritation of the gastric epithelium → acidic properties of NSAIDs cause irritation of the GI tract
what is the rate-limiting step of prostaglandin (PG) synthesis?
cyclooxygenase
- converts arachidonic acid into PGs and thromboxanes
T/F: NSAIDs activate cyclooxygenase (COX)
FALSE
- NSAIDs inhibit COX
what are the main differences between COX-1 and COX-2?
COX-1
- constitutively active
- synthesizes cytoprotective PGs in the GI tract
- forms thromboxane A2, causing platelet aggregation and hemostasis
COX-2
- inducible
- upregulated by inflammatory responses
what are some of the risk factors associated with NSAID-induced ulcers and complications?
- age >65 yo
- previous peptic ulcers/ulcer-related complications
- high-dose NSAIDs, multiple NSAID use, and type of NSAID used
- NSAID-related dyspepsia
- ASA
- NSAID + (ASA, antiplatelets, oral bisphosphonates, corticosteroids, anticoagulants/coagulopathy, OR SSRIs)
- chronic debilitating disorders (CVD, RA)
- cigarette smoking, alcohol use
- H. pylori infection
what are the signs/Sx of PUD?
- epigastric pain → "gnawing", "burning", vague fullness/cramping
- dyspepsia
- pyrosis
- N/V, loss of appetite (most common with gastric ulcers)
describe the pain characteristics of duodenal ulcers
located in the duodenal bulb
- food may relieve pain initially, but often worsens 1-3 hours after a meal
- nocturnal pain is MORE common
describe the pain characteristics of gastric ulcers
located in the lesser curvature
- food may worsen pain
- nocturnal pain is LESS common
- other: N/V/D more common
what are the alarm Sx associated with PUD?
- age >55 yo with NEW-ONSET dyspepsia
- bleeding
- anemia
- early satiety
- unexplained weight loss
- progressive dysphagia
- odynophagia
- FH of upper GI cancer
- recurrent vomiting
- previous esophagogastric malignancy
if evaluating a patient with ulcer-like Sx, what are the next steps if there are NO alarm Sx?
are they on NSAIDs?
- if yes → stop the NSAIDs if possible; if not possible, decrease the dose
- if no → have they been treated for H. pylori before?
--- if yes → endoscopy to assess ulcer status
--- if no → perform serology
if evaluating a patient with ulcer-like Sx, what are the next steps if there ARE alarm Sx?
perform an endoscopy to assess ulcer status
- if ulcers are present → test for H. pylori
- if ulcers are absent → consider other etiologies (GERD, NUD)
H. pylori is often diagnosed using endoscopy-related methods, like biopsy (rapid) urease; describe its mechanism, advantages, disadvantages, and use
- mechanism: detects the presence of ammonia
- advantages: inexpensive, easy, rapid
- disadvantages: false-negatives
- use: test of choice at endoscopy
H. pylori is often diagnosed using endoscopy-related methods, like histology; describe its mechanism, advantages, disadvantages, and use
- mechanism: microbiologic examination using stains
- advantages: sensitive and specific (>95%), gold standard
- disadvantages: expensive, requires trained personnel, no immediate results
- use: NOT recommended for initial Dx
H. pylori is often diagnosed using endoscopy-related methods, like cultures; describe its mechanism, advantages, disadvantages, and use
- mechanism: biopsy
- advantages: 100% specific, ABX sensitivity
- disadvantages: expensive, lack of availability, no immediate results
- use: used AFTER failure of 2nd line treatment
H. pylori can also be diagnosed using less invasive methods, like Ab testing; describe its mechanism, advantages, and disadvantages
- mechanism: detects IgG Abs
- advantages: inexpensive, widely available
- disadvantages: can't distinguish between current and previous infection
H. pylori can also be diagnosed using less invasive methods, like urea breath tests (UBTs); describe its mechanism, advantages, and disadvantages
- mechanism: detect exhaled radioactive CO2 after ingestion of C-urea
- advantages: test for active infection, most accurate non-invasive option
- disadvantages: lack of availability/reimbursement, false-negatives, must stop PPIs/H2RAs (1-2 weeks) and bismuth or ABX (4 weeks) before testing
*recommended test to CONFIRM post-treatment eradication
H. pylori can also be diagnosed using less invasive methods, like fecal Ag tests; describe its mechanism, advantages, and disadvantages
- mechanism: identify Ag in stool
- advantages: tests for active infection only
- disadvantages: must collect stool samples
what are potential complications associated with PUD?
- upper GI bleeding → hematemesis, hematochezia, melena
- perforation (7%) → presents as severe, sharp pain that radiates to the back
- obstruction (2%) → presents as early satiety, weight loss, loss of appetite
- cancer → MALT lymphoma
what is Zollinger-Ellison syndrome? describe its clinical presentation
ulceration due to hypersecretion of gastric acid; presentation:
- abdominal pain
- N/V/D
- heartburn
- GI bleeding
- weight loss
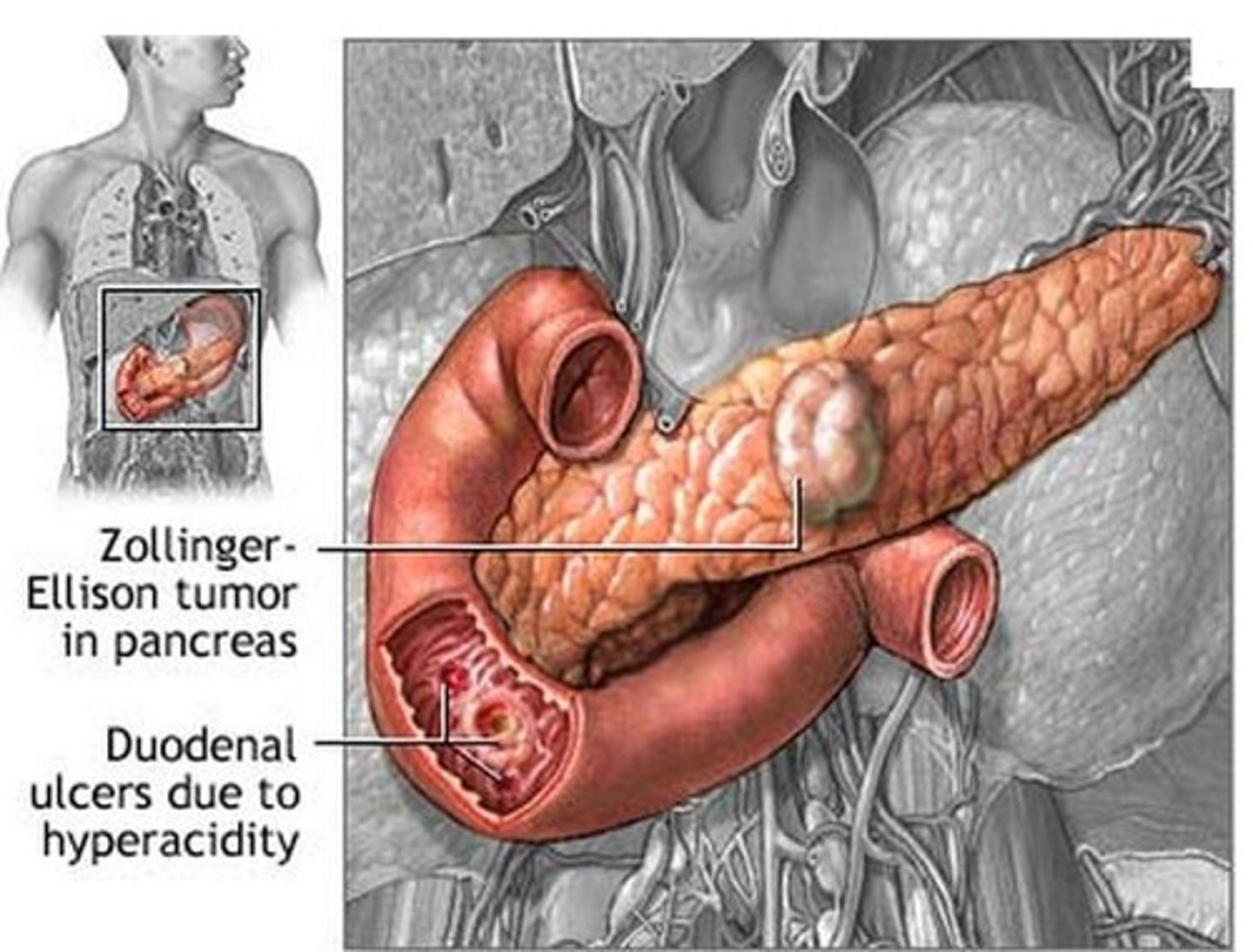
how is Zollinger-Ellison syndrome diagnosed?
- fasting serum gastrin levels
- gastric acid secretory tests
patients with what pre-existing conditions are most at-risk for developing stress-related mucosal damage (SRMD)?
critically ill patients
- respiratory failure (mechanical ventilation for >48 hours)
- coagulopathy (INR >1.5, platelet <50,000 mm³)
- burns (>35% BSA)
- traumatic spinal cord injury
- major surgery
- prolonged ICU admission (>7 days)
- hypotension
- sepsis
- acute renal failure, hepatic failure
- high-dose corticosteroid therapy (>250 mg/day hydrocortisone or equivalent)
- head injury
- multiple trauma
what is SRMD? describe its clinical presentation
stress-related mucosal disease; characterized by decreased GI motility; presentation:
- usually asymptomatic!
- associated with upper GI bleeding
T/F: the majority of critically ill patients (75%+) develop SRMD within 24-48 hours
TRUE
what is SRMB?
overt bleeding with hemodynamic instability, requiring blood products
- occurs in 1-6% of critically ill patients
list the condition, location, intragastric pH dependency, Sx, ulcer depth, and GI bleeding status of H. pylori-induced PUD
- condition: chronic
- location: duodenum > stomach
- intragastric pH: more dependent
- Sx: usually epigastric pain
- ulcer depth: superficial
- GI bleeding: less severe
list the condition, location, intragastric pH dependency, Sx, ulcer depth, and GI bleeding status of NSAID-induced PUD
- condition: chronic
- location: stomach > duodenum
- intragastric pH: less dependent
- Sx: often asymptomatic
- ulcer depth: deep
- GI bleeding: more severe
list the condition, location, intragastric pH dependency, Sx, ulcer depth, and GI bleeding status of SRMD-induced PUD
- condition: acute
- location: stomach > duodenum
- intragastric pH: less dependent
- Sx: asymptomatic
- ulcer depth: most superficial
- GI bleeding: more severe