Gallbladder and Pancreas
1/74
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
75 Terms
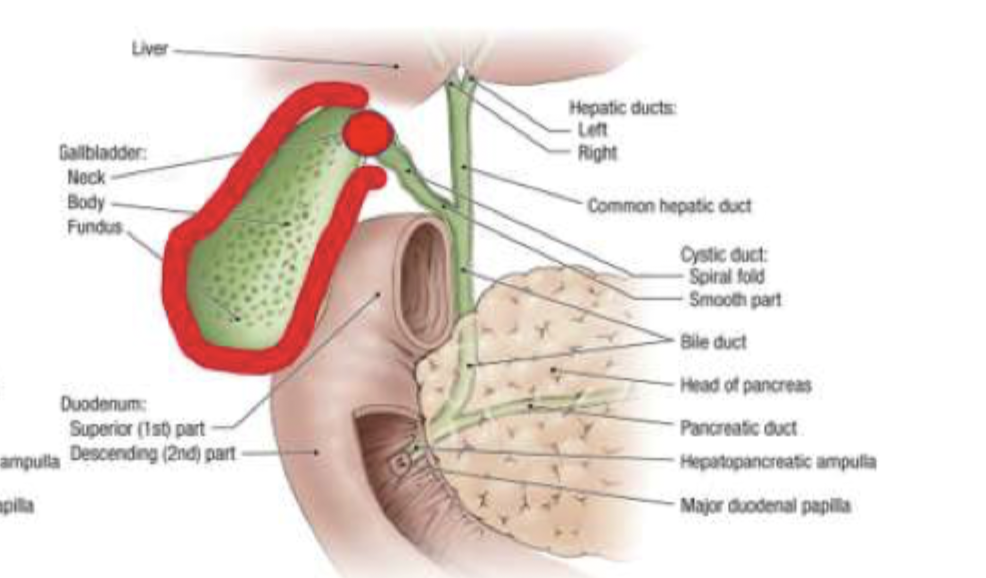
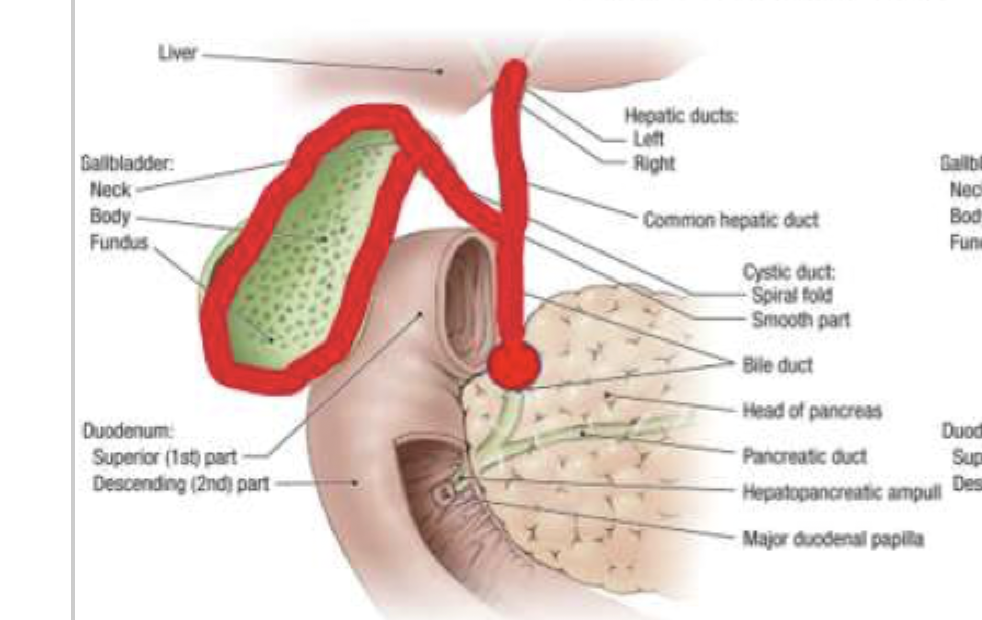
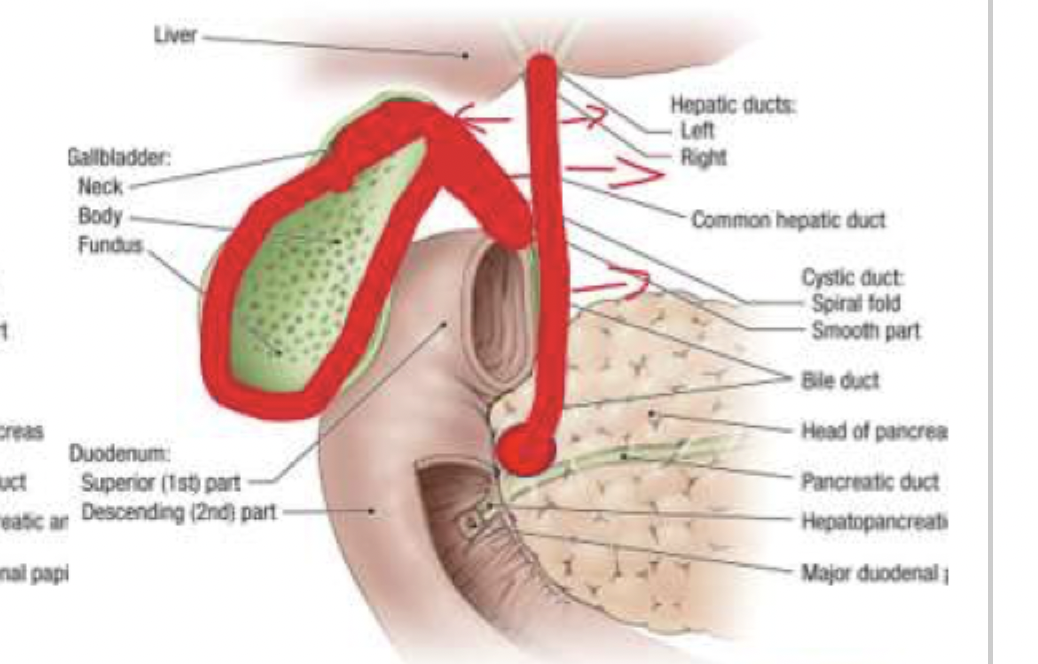
Produced in the liver, stored and concentrated in the gallbladder, secretion is triggered by CCK, cystic duct, common bile duct, duodenum
Give me the path of bile
Cholesterol (80%), Calcium bilirubinate (pigment - 20%)
What are gallstones (cholelithiasis) composed of?
Women, age, LITH gene, obesity, rapid weight loss (mobilization of cholesterol), DM, insulin resistance, high carb/glycemic intake, hypertriglyceridemia, pregnancy, Cirrhosis, Hep C, Crohn disease
Risk factors for Gallstones
Estrogen increases cholesterol secretion, progesterone slows gallbladder emptying
Why is pregnancy a risk factor for cholelithiasis
increased circulating cholesterol, bile over concentration
Pathogenesis of cholelithiasis
Biliary colic
Cholelithiasis can be asymptomatic, but when it does have symptoms it is known as
NSAIDs and anticholingerics (diclyclomine) for pain, Cholecystectomy (Treatment of choice) for symptomatic patients, UDCA (dissolves gallstones in 2 years), extracorpeal shock wave lithotripsy (use with oral dissolution)
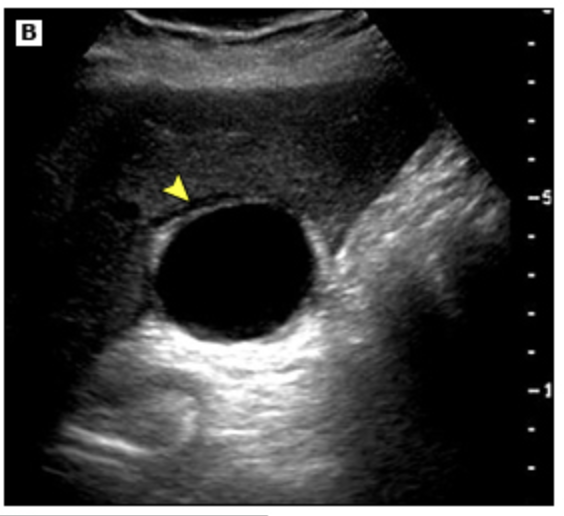
36 y/o female presents to the ER for epigastric pain that radiates to the shoulder. She states that it worsens after greasy meals and usually peaks 30 minutes after eating. On a physical exam you note RUQ tenderness and a positive murphy sign. Labs are normal. See ultrasound. What is your treatment plan?

calcified gallbladder, gallstones 3cm+, LITH gene, bariatric/cardiac transplant candidates
What are the indications for prophylactic cholecystectomy?
Gastritis, GERD, acute hepatitis, pancreatitis, viral gastroenteritis, cardiac, cholecystitis
DDX for cholelithiasis
Acute Cholecystitis
Infection and inflammation within the gallbladder most often caused by cholelithiasis (90%), opportunistic infections, and vasculitis.
Known cholelithiasis, Family Hx of gallstones, immune compromise
Risk factors for acute cholecystitis
NPO, NSAIDs/Morphine for pain control, IV 2nd or 3rd gen CPH + metronidazole, Laparoscopic cholecystectomy with in 24 hrs of admission (treatment of choice)
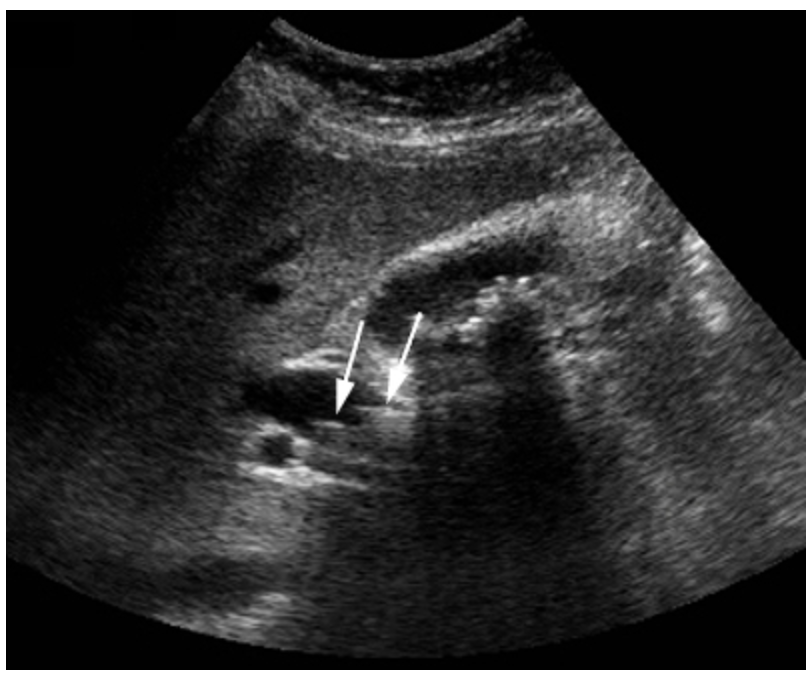
Patient presents to the ER for severe epigastric pain. She notes that the pain is constant, she can’t find a position of comfort, and the pain is worst after meals. Vitals are stable with the exception of 123 bpm and 102.3 temp. On a physical exam you note RUQ tenderness with guarding, rebound tenderness and a positive murphy’s sign. See U/S. What is your treatment plan?
Leukocytosis, elevated AST/ALT, Elevated ALP/Bili if obstructive
Describe the labs for acute Cholecystitis
gallbladder wall thickening with edema (double wall), pericholecystic fluid, sonographic murphy’s sign
What are the U/S red flags for acute cholecystitis?
HIDA (good for acalculosis cholecystitis), CT with contrast
If U/s is neg for acute cholecystitis what can we do?
Chronic cholecystitis, cholangitis, gallbladder gangrene (tissue ischemia which can lead to peritonitis)
Complications of acute cholecystitis
Chronic cholecystitis
Chronic inflammation of the gallbladder due to repeated episodes of acute cholecystitis or irritation of the gallbladder by stones
Strawberry gallbladder, hydrops, fistula formation to the bowel, pancreatitis, porcelain gallbladder, carcinoma of the gallbladder
Complications of Chronic Cholecystitis
Cholecystectomy (may end up being open due to chronic complications)
Gameplan for Chronic cholecystitis
gastritis, GERD, acute hepatitis, pancreatitism
DDX for cholecystitis
choledocholithiasis
A stone obstructing flow within the common bile duct (proximal or distal)
gallstone passage, bile stasis, bile duct dilation, age
Risk factors of choledocholithiasis
ERCP (endoscopic retrograde cholangiopancreatography)
Patient presents to the ER for RUQ pain. He also notes N/V/D and that his stools are pale. On a physical exam you note jaundice, RUQ and MEQ tenderness as well as guarding and rebound tenderness. Labs are as follows elevated ALT/AST, elevated direct bilirubin, elevated ALP, elevated amylase and lipase. U/S reveals a dilated common bile duct. What can you use to confirm your diagnosis and treat the patient?
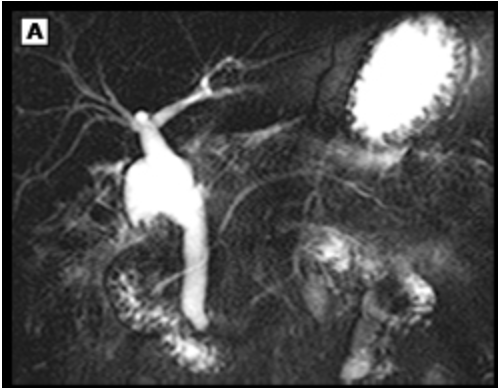
MRCP (magnetic resonance cholangiopancreatography)
What imaging modality can confirm your diagnosis of choledocholithiasis but not treat the patient?
cholecystitis, gastritis, GERD, acute hepatitis, pancreatitis, post-hepatic jaundice, cardiac
DDX choledocholithiasis
Acute cholangitis
Bacterial infection of the biliary tract that can cause severe illness and death most commonly caused by organisms ascending from the duodenum during an episode on biliary obstruction
choledocholithiasis, bilary stents, duct stenosis (benign/malignant)
Risk factors of acute cholangitis
Abd U/s (first line), CT with contrast, ERCP (relieve obstruction), MRCP (we have all the time in the world)
Patient presents with severe RUQ that comes and goes with the 1st episode starting 5 hours ago. Vitals are stable with the exception of 90/54 and 103.4 temp. On physical exam you note jaundice. Labs are as followed Elevated ALP, AST, Conjugated bilirubin, ALP, marked leukocytosis. What imaging do you want?
Severe, episodic RUQ pain persisting for at least 3 hours, fever, jaundice
Charcot’s triad - cholangitis
Severe, episodic RUQ pain persisting for at least 3 hours, fever, jaundice, AMS, hypotension
Reynolds Pentad - suppurative cholangitis
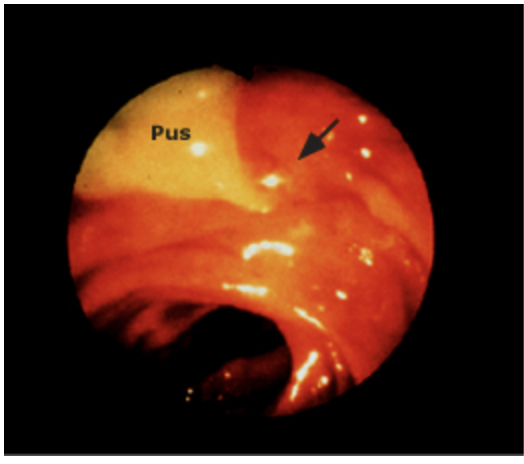
IV fluids, analgesics, Cipro + metronidazole OR Pip-Tazo
Patient presents with severe RUQ that comes and goes with the 1st episode starting 5 hours ago. Vitals are stable with the exception of 90/54 and 103.4 temp. On physical exam you note jaundice. Labs are as followed Elevated ALP, AST, Conjugated bilirubin, ALP, marked leukocytosis. U/S shows a dilated bile duct and stones. What’s your treatment plan?
Urgent biliary drainage (endoscopic, percutaneous, open), Cholecystectomy when stable
Patient presents with severe RUQ that comes and goes with the 1st episode starting 5 hours ago. Vitals are stable with the exception of 90/54 and 103.4 temp. On physical exam you note jaundice. Labs are as followed Elevated ALP, AST, Conjugated bilirubin, ALP, marked leukocytosis. U/S shows a dilated bile duct and stones. Patient IS NOT RESPONDING to initial treatment measures. What you doing?
cholecystitis, choledocholithiasis, gastritis, GERD, acute hep, pancreatitis, Post-hepatic jaundice, obstructive neoplasm, cardiac
DDX for cholangitis
endocrine secretion of glucagon, insulin, somatostatin, pancreatic polypeptide; exocrine secretion of digestive enzymes and alkaline bicarb ions
What is the role of the pancreas?
Biliary tract disease (most common), Heavy alcohol intake, Hypercalcemia, hyperlipidemia, recent abdominal trauma/surgery (ERCP), meds, infections (mumps, CMV), pancreatic neoplasms
What are some things that can cause acute inflammation of the pancreas (pancreatitis)
smoking, truncal obesity, age
Risk factors for acute pancreatitis
amylase, lipase, CBC, lipids, LFTs, CMP, CRP, CT with contrast (preferred), MRI, U/S
67 y/o male presents to the ER for sudden onset epigastric pain. He says the pain radiates to the back, worsens with walking, but improves with leaning forward. He also reports N/V/D. Social history is positive for 10 pack year smoking hx and daily EtOH (4 12 oz beers). Vitals are stable with the exception of 101.5 temp, 143 bpm, and 100/70. On physical exam you note panniculitis, epigastric tenderness, a distended abdomen with absent bowel sounds. What diagnostics do you want champ?
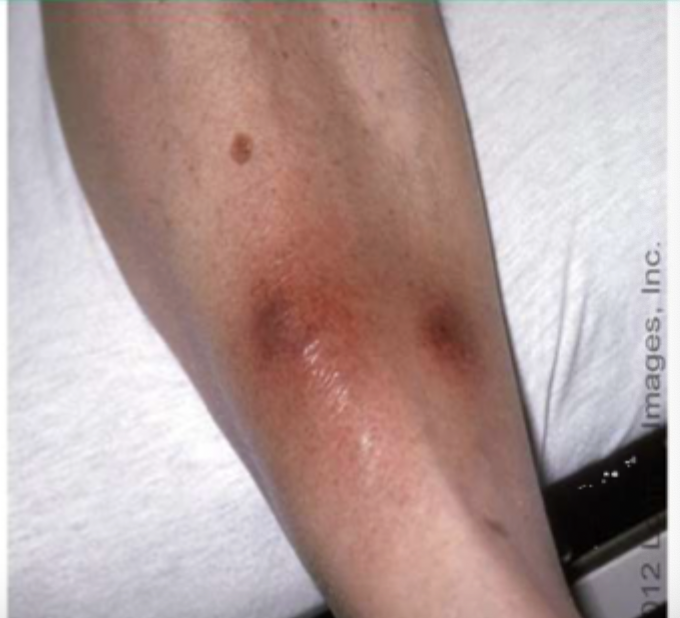
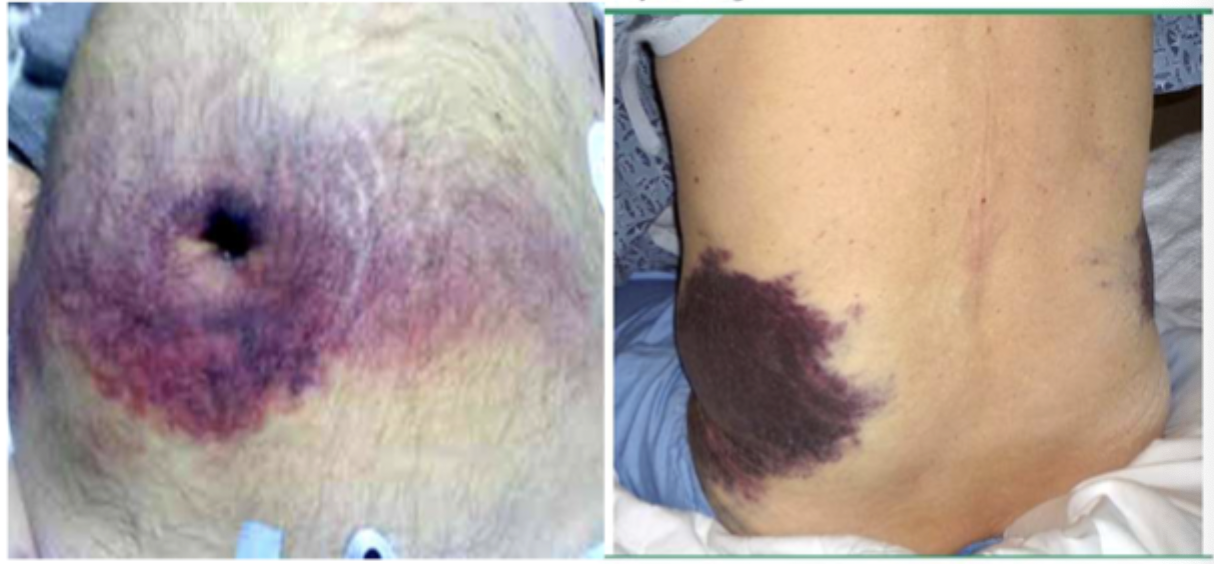
Cullen (periumbillical), Grey Turner (flank)
What signs might you see on the skin that are signs of hemorrhagic pancreatits
Elevated amylase and lipase (3x normal), leukocytosis, ALT UP (biliary etiology), TGs UP (hypertriglyceridemia etiology), ALP UP (common bile duct obstruction), AKI (elevated BUN, Creat, proteinuria, glycosuria), CRP Up or hypocalcemia is not a good sign
What labs do you expect for acute pancreatitis
Ranson Criteria (Big number BAD)
What helps predict a severe course of acute pancreatitis and the mortality based on labs
Acute onset of persistent, severe epigastric pain, Lipase/amylase 3x normal, characteristic findings on any imaging
Diagnostic criteria for acute pancreatitis (2/3 is positive)
Pseudocyst (pocket of amylase), pancreatic abscess (fever, leukocytosis, epigastric mass), Pancreatic necrosis sterile or infected (fever, leukocytosis, SHOCK), SIRS (can lead to hypovolemic shock, ARDs, cardiac failure)
Complications of pancreatitis
NPO, IV hydration, NG suction, opiates, bed rest, elective procedure to fix underlying (cholecystectomy, biliary sphincterotomy)
67 y/o male presents to the ER for sudden onset epigastric pain. He says the pain radiates to the back, worsens with walking, but improves with leaning forward. He also reports N/V/D. Social history is positive for 10 pack year smoking hx and daily EtOH (4 12 oz beers). Vitals are stable with the exception of 101.5 temp, 143 bpm, and 100/70. On physical exam you note panniculitis, epigastric tenderness, a distended abdomen with absent bowel sounds. Labs show leukocytosis, amylase and lipase are 3x normal. Whats your treatment plan (he’s fine its mild)
ICU admit, IV fluids to maintain pressure, Whole blood/albumin PRN, IV imipenem and cefuroxime, necrotic tissue debridement, If biliary ERCP, consult gen surge for exploratory laparotomy
67 y/o male presents to the ER for sudden onset epigastric pain. He says the pain radiates to the back, worsens with walking, but improves with leaning forward. He also reports N/V/D. Social history is positive for 10 pack year smoking hx and daily EtOH (4 12 oz beers). Vitals are stable with the exception of 101.5 temp, 165 bpm, and 88/48. On physical exam you note panniculitis, epigastric tenderness, a distended abdomen with absent bowel sounds. Labs show leukocytosis, amylase and lipase are 3x normal, and CT shows pancreatic necrosis. Whats your treatment plan (HE’S ABOUT TO CODE)
Perforated dudodenal ulcer, gastritis, acute cholecystitis, bowel obstruction, renal colic, acute mesenteric ischemia, ectopic pregnancy, cardiac, PE
Acute Pancreatitis DDX
EtOH use disorder (45-80%), Hyperparathyroidism, Autoimmune diseases, obstructive chronic pancreatitis, Tropical pancreatitis (malnutrition based), idiopathic
What are some common causes for chronic pancreatitis?
An initial sentinel acute pancreatitis event (SAPE) causes injury → fibrosis → chronic pain and recurrent episodes → endocrine and exocrine insufficiency
Run me through the pathogenesis of chronic pancreatitis
MRCP (1st line), ERCP (can exacerbate pancreatitis), Transabdominal U/S, endoscopic U/S, CT, MRI, X-ray (shows calcifications)
67 y/o female presents to the ER for “Pancreatitis AGAIN.” She states she gets it like once every 6 months and the pain is usually in the LUQ or epigastric region. On physical exam you note MEG tenderness with guarding. Labs reveal elevated amylase, lipase, ALP, and bili, excess fat in the stool. What imaging you want?
endoscopic therapy/open surgery (biliary), pancreatic sphincterotomy (pancreatic duct), drain persistent pseudocysts, lithotripsy/endoscopic, relieve pain, manage complications, No alcohol, low-fat diet, No opioids, Pancreatic supplements, prednisone (autoimmune pancreatitis)
Chronic pancreatitis treatment
Gastroparesis
Chronic motility disorder characterized by delayed gastric emptying in the absence of mechanical obstruction (AKA delayed gastric emptying)
Diabetes (neuropathy), viral (CMV, EBV, VZ), meds (ozempic), iatrogenic vagal nerve injury, neurological disorder, autoimmune
Gastroparesis etiologies
Xray/CT (r/o obstruction), Scintigraphic gastric emptying (Draft pick), capsule swallow study
35 y/o female presents to the clinic for “a rock in her stomach” and N/V. She reports that she gets full easily and hasn’t been eating as much but that could be due to the semaglutide. On physical exam you note epigastric tenderness without guarding or rigidity. What diagnostics you want?
Low fat and fiber diet, Glycemic control and nutrition, Prokinetics - Metaclopramide (1st line) or macrolides, antiemetics, jejunostomy
Okay so Ozempic girlie has gastroparesis what is our treatment plan?
Cavenous hemangioma (most common and associated OCPs), focal nodular hyperplasia, hepatocellular adenoma (OCPs and may cause pain)
Types of benign liver neoplasms
Multiphase CT or MRI
What is the diagnostic of choice for benign liver neoplasms
Normal LFTs, RUQ pain, possible palpable RUQ mass
Classic findings for benign liver neoplasms
Surgical resection for symptomatic lesions, tumor over 5 cm or rapidly growing, stop the OCP (tumor may regress)
Treatment plan for benign liver neoplasms
Hepatocellular carcinoma (HCC)
Malignant neoplasms that form from the liver’s normal hepatocytes
Cirrhosis (80%), viral hepatitis, drug-induced hepatitis, fatty liver, Alpha-1-Antitrypsin deficiency, radiation, FHx
Risk factors for HCC
CBC, LFTs, Alpha fetoprotein, hep screen, CT with contrast/MRI, multiphasic MRI/CT with contrast (diagnostic), U/s, Liver biopsy (definitive diagnostic)
66 y/o patient presents to the ER for failure to thrive. PMHx is positive for cirrhosis. Wife states that he was doing great 4 days ago before rapidly deteriorating after his last para which was bloody. He reports weight loss and fatigue. On a physical exam you note a bruit over the liver and palpable liver enlargement. What diagnostics you want?
Hepatic resection (56% 5 yr) and liver transplantation (75% 5 yr)
66 y/o patient presents to the ER for failure to thrive. PMHx is positive for cirrhosis. Wife states that he was doing great 4 days ago before rapidly deteriorating after his last para which was bloody. He reports weight loss and fatigue. On a physical exam you note a bruit over the liver and palpable liver enlargement. Labs show anemia, leukocytosis, and elevated AFP. Multiphasic CT with contrast reveals 3 cm HCC. What is your treatment plan?
U/S every 3 months, biopsy if it gets bigger
In liver lesions less than 1 cm what is the game plan?
radiofrequency ablation, Sorafenib
Palliative treatments for HCC
Chronic HBV peeps, Cirrhosis due to HBV, HCV, EtOH
Who is getting screened for HCC?
U/S and AFP q6months
Screening method for HCC
Vax for HBV, Treat HBV/HCV
Prevention of HCC
Pancreatic adenocarcinoma
Most common neoplasm of the pancreas - 75% head (more symptoms due to obstructions) and 25% tail
Age, tobacco use, heavy EtOH, obesity, chronic pancreatitis, prior abdominal radiation, family hx, new onset DM after 45, insulin, sitagliptin, GLP-1
Risk factors for Pancreatic adenocarcinoma
MEN1 syndrome, GEP-NETs
Islet cell tumors make up 1-5% of pancreatic cancers, what are some examples?
Cystic neoplasms
1% of pancreatic cancers but occur without hx of pancreatitis and have a better prognosis than adenocarcinoma
painless jaundice, weight loss in older patients, vague abdominal pain (MEG if head, LUQ with tail), diarrhea, migratory thrombophlebitis, early satiety, silver stools (Thomas sign - involves ampulla of Vater), Palpable non-tender gallbladder (Courvoisier sign), Hard periumbilical nodule (Sister Mary Joseph Nodule)
Red flags for Pancreatic cancer
Anemia (mild), DM, Hyperglycemia, maybe elevated amylase/lipase, elevated LFTs if biliary obstruction, Cancer antigen 19-9, plasma chromogranin A (neuroendocrine), fecal occult blood (if vater is affected)
Typical labs for Pancreatic cancer
Multi-phase thin cut CT with contrast (1st line), MRI, ERCP (if CT is ambiguous), PET, FNA
Imaging gameplan for pancreatic cancer
Radical pancreaticoduodenal resection (Whipple - treatment of choice for head tumors), Chemo (downstage to allow for resection or palliative), endoscopic stent if surgery not an option
Treatment plan for pancreatic cancer
Poor (20% 5 yr)
Prognosis of pancreatic cancer