Intracranial pressure
1/34
Earn XP
Description and Tags
Test 4 - sem 3
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
35 Terms
What is in the brain?
Brain tissue, blood cerebrospinal fluid (CSF)
*When one component increases, the others must decrease to maintain equilibrium
Risk factors for increased ICP
Head injury
Brain tumors
Hydrocephalus
Intracranial hemorrhage
Toxic/viral encephalopathies
Early signs of increased ICP
Decreased LOC
Altered mental status
Headache
Late signs of increased ICP
Unilateral fixed and dilated pupil
ipsilateral (same side) to cranial nerve compression
motor paresis contralateral (opposite side) to herniation
Cushing’s triad
widened pulse pressure (space between diastolic and systolic)
bradycardia
irregular resp pattern
How is increased ICP detected?
Performing serial neurological assessments
elements of wakefulness
arousal
cranial nerve
motor function
***Most sensitive indicator = decrease in LOC
Diagnostics for increased ICP
X-ray
CT
MRI
EEG
Serum osmolality
Serum sodium
Ultrasound
Lumbar puncture (last resort)
Factors the influence ICP
Intra-abdominal & intra-thoracic pressure
coughing
sneezing
Valsalva maneuver
Temperature
hypothermia – decreased metabolism
hyperthermia – increased metabolism
Arterial and venous pressure
autoregulation
Blood gasses
elevated CO2
Position
turning
sitting up/laying down
Normal ICP
Infant: 1-5.6 mm/Hg
Child: 3-7 mm/Hg
Adult: < 15 mm/Hg
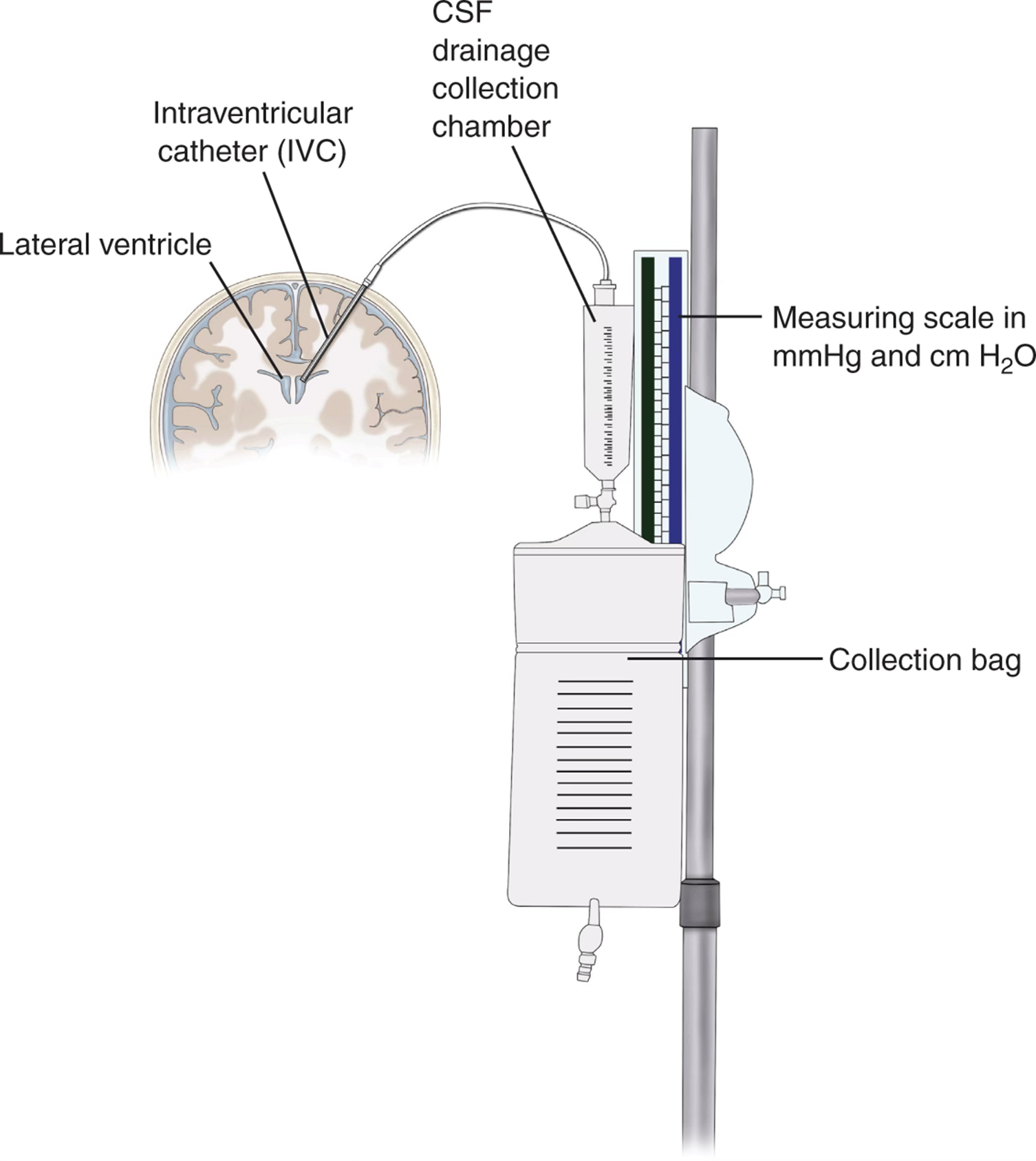
Intraventricular Catheter - Ventriculostomy/external ventricular drain
Most common
Increased risk for infection
Can drain CSF
*Can be done at the bedside
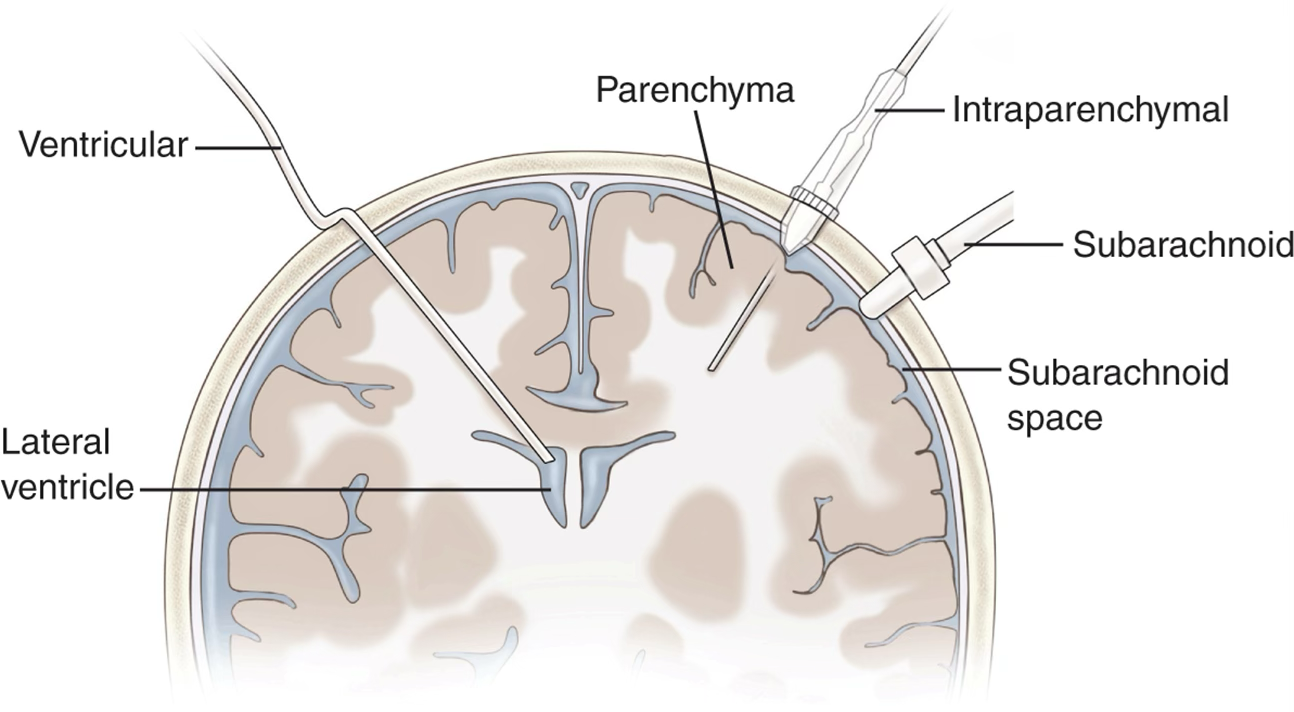
Intraparenchymal sensor/probe
Micro-strain gauge attached to tip of catheter
Fiberoptic technology
Does not drain CSF
Subarachnoid Bolt (SAB)
Bolt or screw connected to a fluid filled transducer system
Inability to drain CSF
Inaccuracy of Measurement due to drift
Nursing management for ICP procedures
Keep dressing over catheter dry and change as prescribed
Monitor insertion site for CSF leakage, drainage or infection
Maintain proper device height
Monitor for manifestations of infection
Use strict aseptic technique when
ICP management - Mannitol
Drug class: osmotic diuretic
Route: IV
Mechanism of action: increase plasma osmolality → draws water out of swollen brain tissue
diuresis → increase urine output
Effect on ICP: rapid reduction; lasts 4-6 hours; rebound risk if BBB disrupted
Effect on circulation: osmotic diuresis → decrease intravascular volume; may decrease BP and CPP
Best use case: normotensive/hypertensive with good renal function
Risks/side effects: hypotension, hypovolemia, renal injury, electrolyte loss, rebound cerebral edema
Contraindications: hypotension, renal failure, disrupted BBB
ICP management - 3% Hypertonic Saline (NaCl)
Drug class: hyperosmolar crystalloid
Route: IV
Mechanism of action: increase serum Na+ (increase osmolality) draws water out of the brain tissue and into intravascular space
vascular expansion → fluid comes out of the brain and goes back into the system/vessels
Effect on ICP: rapid reduction; more sustained effect
Effect on circulation: expands intravascular volume; increase BP and CPP
Best use case: hypotensive, hypovolemic, or renal-impaired patients
Risks/side effects: hypernatremia, fluid overload, pulmonary edema, osmotic demyelination
Contraindications: severe hypernatremia, heart failure, uncontrolled fluid overload
ICP management - surgical
hemicraniectomy and durotomy
hematoma evacuation
ICP management - sedative use
MSO4
Versed (midazolam)
Fentanyl (sublimaze)
Propofol (diprivan)
ICP management - physical interventions
↑HOB at least 30° (45-90)
Neck in neutral position
Minimized hip flexion
ICP management - hyperventilation
↑ RR → ↓ CO2 and cerebral blood vessel constriction
Maintain CO2 of 30 – 35 mmHG with hyperventilation
ICP management - external CSF drainage
Ventriculostomy
Nursing inventions for ICP
Assessment:
Serial neurological assessments every 1 to 2 hours in the critical phase, decreasing in frequency as the risk of cerebral edema and secondary brain injury decreases
Vital signs and oxygen saturation (SpO2) every 1 to 2 hours
Temperature every 1 to 2 hours
Intracranial pressure and CPP every 1 to 2 hours or more frequently if the patient is experiencing an increase in ICP and/or a deterioration of neurological assessment
Cardiac rhythm; serum markers of myocardial injury (creatinine kinase, creatinine kinase specific to cardiac muscle, and troponin)
Intake and output every 1 to 2 hours
Serum sodium and/or serum osmolality
Serum electrolytes
Blood urea nitrogen (BUN) and creatinine
Arterial blood gas samples
End-tidal carbon dioxide (EtCO2) continuously to guide hyperventilation therapy during treatment of increased ICP
Actions:
The head of the bed should be maintained at greater than 30 degrees, with the patient’s head in midline. Avoid sharp hip flexion.
Avoid placing the patient in a position that allows pressure directly on the operative side after craniectomy.
Perform endotracheal suction only as necessary; preoxygenate with 100% oxygen for 1 to 2 minutes prior to suctioning.
Administer sedative medications as prescribed.
Administer osmotic agents (mannitol and hypertonic saline).
Ensure continuous drainage of CSF through the external ventricular drainage system when applicable.
Administer antipyretics and/or implement cooling measures.
Teaching:
Devices used during the course of treating increased ICP
Medications used to treat increased ICP
Complications of increased ICP
Rationale for helmet after craniectomy
Importance of allowing the patient to rest
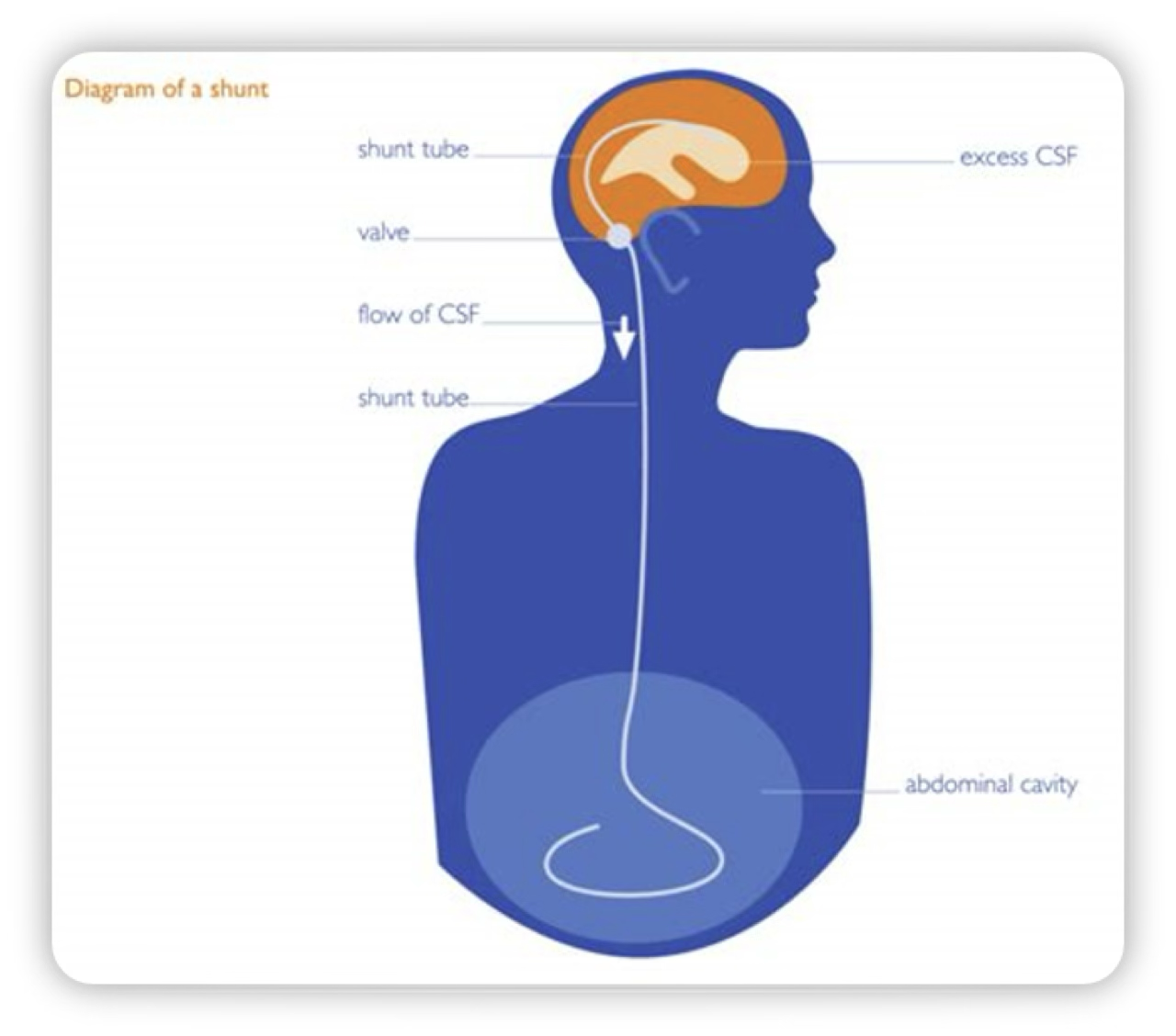
What is hydrocephalus?
The build up of CSF in the brain
Congenital hydrocphalus
Present at brith
Acquired hydrocepgalus
Developed overtime
Hydrocephalus increases risk for…
Developmental disabilities
Visual problems
Abnormalities in memory
Reduced intelligence
Therapeutic management for hydrocephalus
Shunt = most common
Complications:
Infection
Obstruction
Revision with growth
Nursing assessment for hydrocephalus
Health History
Physical Examination
Inspection
Palpation
Diagnostic tests
Nursing management for hydrocephalus
Maintain cerebral perfusion
Prevent/recognize shunt infection and complications
Minimize neurologic complications
Promote growth and development
Maintain adequate nutrition
Support and educate child and family
What is meningitis?
The inflammation of the menages
Causes of meningitis
Bacterial infection
Viral infection
Fungal infection
Aseptic meningitis
Symptoms of meningitis
Headache
Altered mental status
Phonophobia
Fatigue
Severe muscle pain
Dislike of bright lights
N/V
Paleness
Spots/rash
Blotchy
High fever
Seizures
Stiff neck
Sleepiness or difficulty waking
Medical management for meningitis
Diagnostics:
CSF exam with lumbar puncture (glucose, protein, WBC,gram stain, culture)
CT/MRI of head
Lab: urine, throat, and blood cultures; CBC
Cardiac testing
Medications:
Broad-spectrum antibiotics, ceftriaxone, vancomycin
Tx for 14-21 days
Nursing management for meningitis
Assessments:
Neurologic exam
Vital signs (↑ temperature)
Fluid balance
Cranial nerves
Renal function
Vascular assessments
Actions:
IV fluids
Antibiotic administration
↓ stimuli
HOB at 30°
Pain management
Standard precautions
Prevention of meningitis
Haemophilus influenzae type b (Hib) vaccine
Pneumococcal polysaccharide vaccine (PPSV)
Meningococcal vaccine (MCV4)