HRM - Lecture 1: Composition of Blood and Haematopoiesis
1/81
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
82 Terms
m: 5-6L
f: 4-5L
What is the normal blood volume for an adult male and female respectively?
centipoise - 1.1-1.2
In what unit is blood viscosity measured and what is a normal value?
7.35-7.45
What is the normal blood pH range?
285/295 mOsM
What is the typical osmolarity of blood?
1/4
How much of the ECF is accounted for by blood?
8%
How much of the human body weight is accounted for by blood?
- carry nutrients around the body
- carry hormones around the body
- carry waste products to excretory organs
Name 3 transport functions of blood
- regulate temperature
- regulate fluid balance
- regulate pH
Name 3 regulatory functions of blood
Plasma - 46-63%
Formed Elements - 37-54%
What are the two main components of blood and what percentages do they account for?
Water (92%), Plasma proteins (7%), and other solutes (1%)
What makes up plasma?
Red blood cells, White blood cells, and Platelets
What are the main formed elements of blood?
Albumin (60%)
Which is the most abundant plasma protein?
Steroid hormones, lipids, fatty acids, bilirubin
Name 4 types of molecules albumin transports
< 1.0g/L
What level of albumin is considered albuminaemia?
alpha1, alpha2, beta, gamma
What are the 4 categories of globulin?
lipids, hormones, metal ions
Name 3 types of molecule transported by globulins
These are the immunoglobulins made by lymphoid tissue
What is the role of gamma globulins?
IgG, IgA, IgM, IgB, IgE
List the immunoglobulins
alpha1 antitrypsin - it protects the lungs from proteases and elastases
What is the main alpha1 globulin and its role?
Fibrinogen is a clotting factor (CF1). It makes the blood viscous and contributes to clotting.
What is the role of fibrinogen?
This is the blood pressure (approx 25mmHg) exerted by plasma proteins. It plays a role in controlling the amount of fluid exchange between capillaries and interstitial fluid, by preventing excessive plasma loss from blood.
What is the colloidal osmotic pressure?
its asymmetrical shape
What properties allow fibrinogen to create viscosity?
The erythrocyte sedimentation rate is the rate at which erythrocytes settle into a sediment in an hour. Typically higher for females than males and correlating to the amount of fibrinogen
What is the ESR?
> 8.0g/L
What is considered hyperproteinaemia?
Usually excessive fluid loss increasing protein concentration such as:
- vomiting
- diarrhoea
- diabetes insipidus
What causes hyperproteinaemia?
Dilution or loss of plasma protein such as:
- Excretory organ dysfunction such as nephrotic syndrome
- pregnancy
- extensive skin burns
- malabsorption
What causes hypoproteinaemia?
The red blood cell is essentially a concentration of haemoglobin (33% of RBC), transporting oxygen around the body
What is the role of the red blood cell?
~120 days
What is the life span of an erythrocyte?
anaerobic glycolysis
What is the main source of energy for erythrocytes?
Maximises surface area for gas exchange and enhances flexibility to pass through narrow capillaries.
What is the functional advantage of the erythrocytes bi-concave shape?
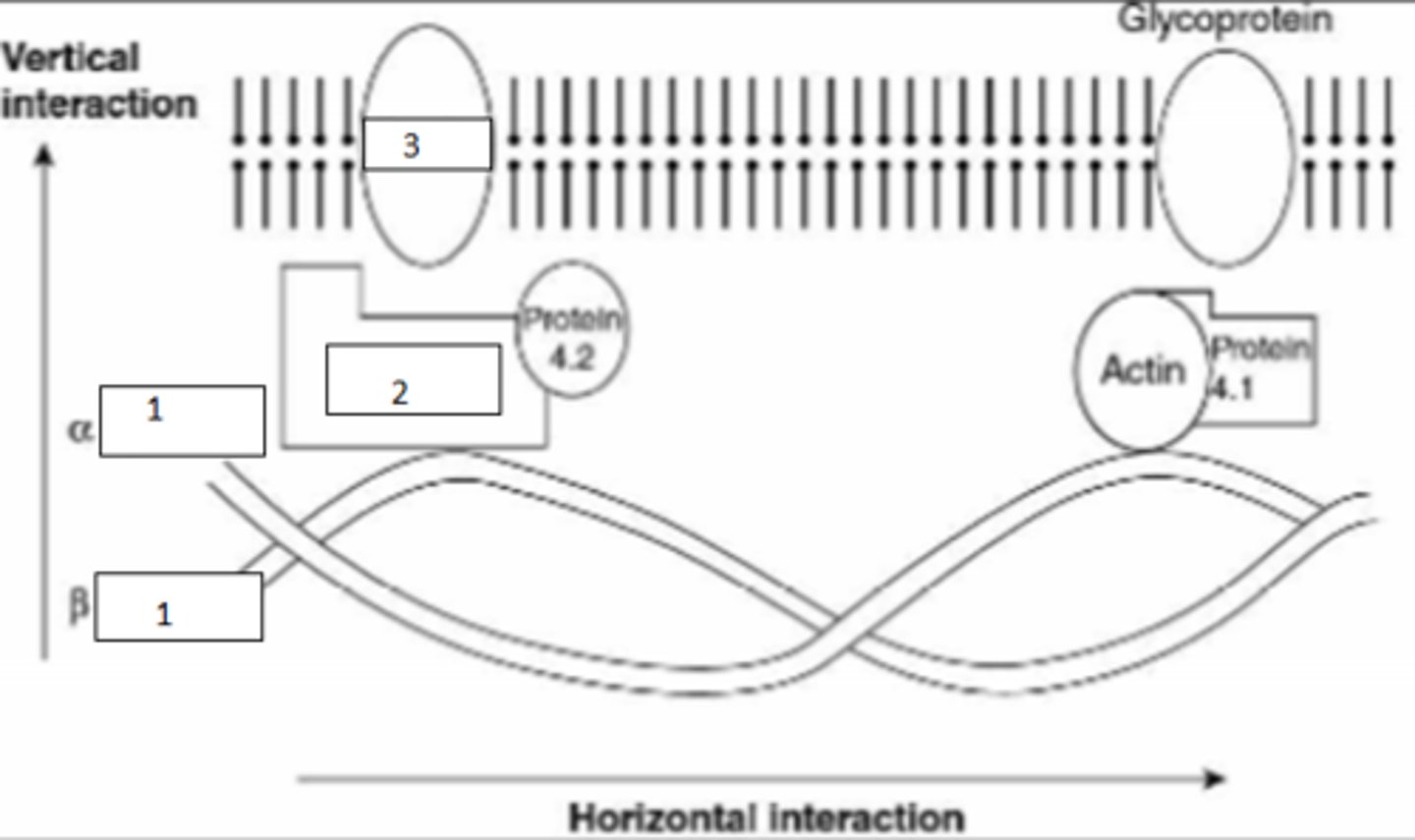
1. spectrin
2. ankyrin
3. transmembrane protein band 3
These proteins interact to form the major structural components of the red blood cell wall
Fill the blanks on this RBC and describe the role of these structures
Since the ion concentration is maintained actively via ATP, a lack thereof causes a loss of cell volume, increase of rigidity and decreased survival.
(Water leaves the cell, rather than entering, because K+ channels are leakier than Na+ channels - net ion movement out of the cell)
How will ATP production deficits affect a red blood cell?
Via an inhibition of the HMP(aka PPP)-pathway, NADPH and glutathione aren't produced to adequately deal with oxygen radicals. This increases susceptibility to haemolysis
How does Glucose-6-phosphate dehydrogenase defficiency (common defect) affect RBCs?
These are the white blood cells of the immune system
What are leukocytes?
neutrophils, eosinophils, basophils
Name the granulocytes?
lymphocytes, monocytes
Name the agranulocytes
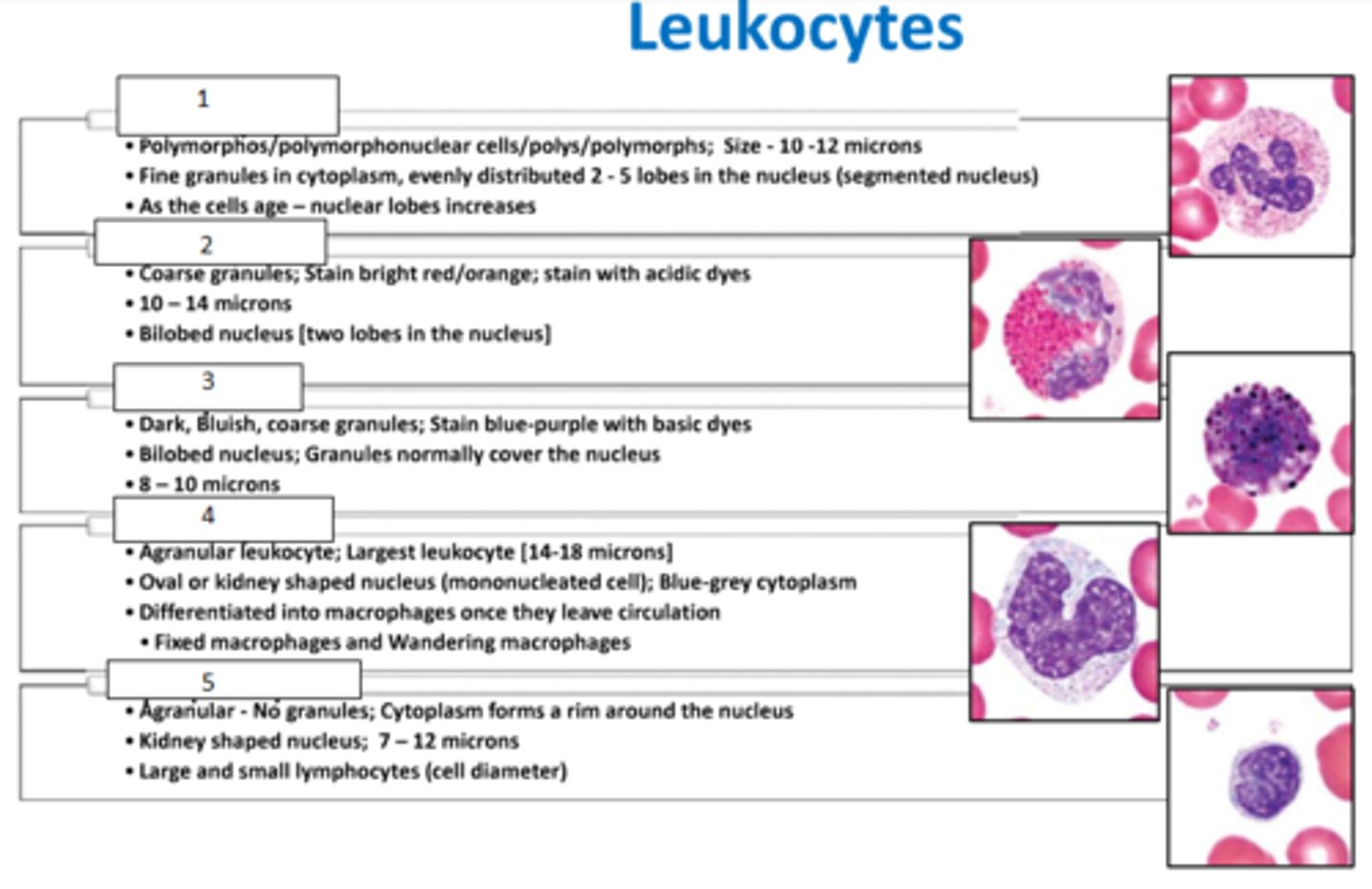
1. neutrophils
2. eosinophils
3. basophils
4. monocytes
5. lymphocytes
Fill the blanks
1. eosinophils
2. neutrophils
3. lymphocytes
4. basophils
5. monocytes
Fill the blanks
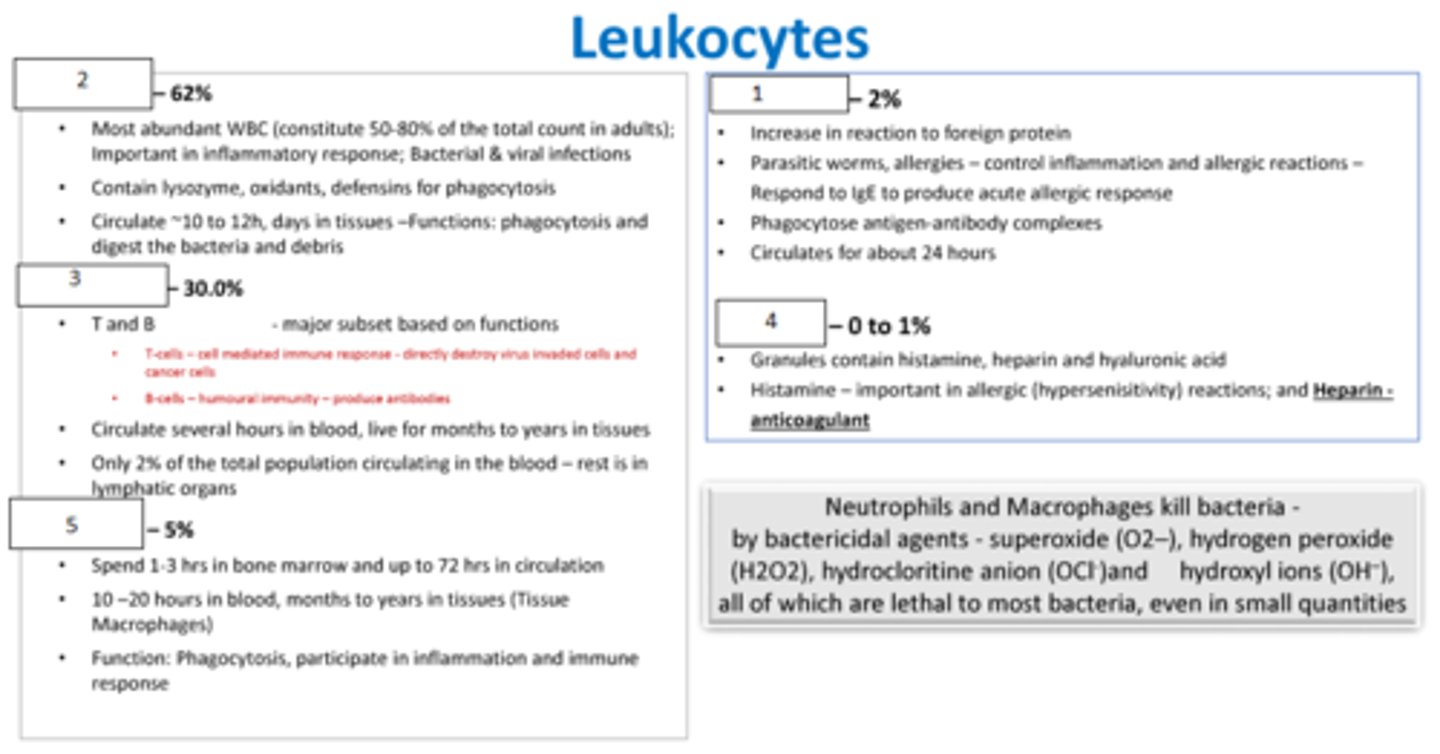
neutrophils and monocytes (macrophages)
Which leukocytes are phagocytic?
The passage of blood cells through intact capillary walls
What is diapedesis?
Movement of cells toward specific chemicals
What is chemotaxis?
Disc shaped cell fragments originating from megakaryocytes (bone marrow cells)
What are platelets?
5-9 days
What is the normal life span of platelets?
150-400 billion per litre
What is a normal platelet count?
Thrombocytosis and thrombocytopenia
What are an increased and decreased platelet count called respectively?
alpha granules and delta granules
What are the main 2 types of platelet factor?
In bone marrow - mostly red
Where does haematopoiesis occur?
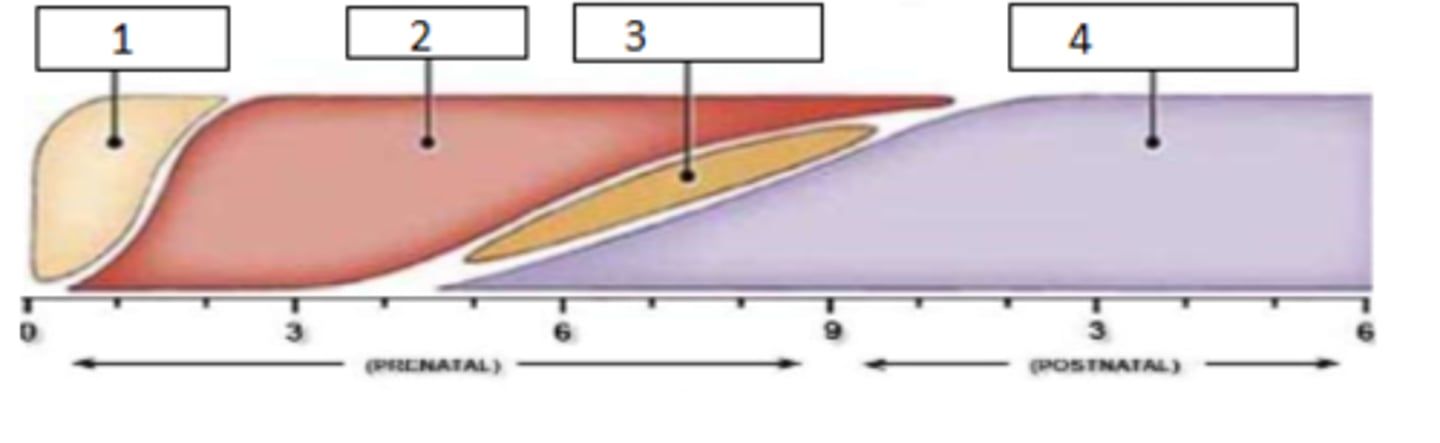
at week 3 of embryonic development in the yolk sac
At which site and when on the embryonic timeline does haematopoiesis begin?
1. yolk sack
2. liver
3. spleen
4. bone marrow
Fill the timeline of haematopoiesis during embryonic development
1. erythrocytes
2. granulocytes
3. megakaryocytes
4. lymphocytes
5. monocytes
Fill the timeline of blood cells produced during development
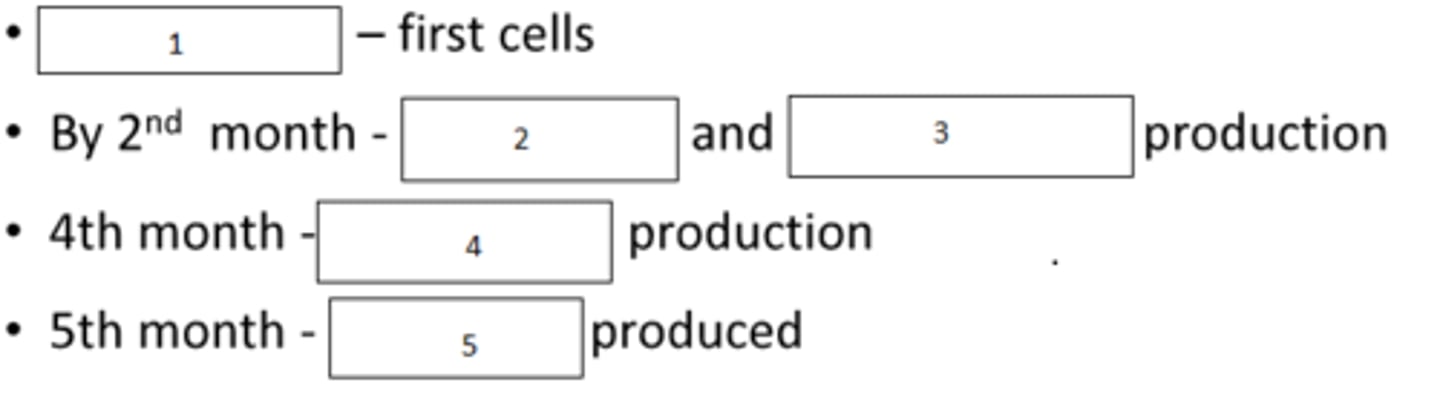
Mesoblastic stage: haematopoiesis in yolk sac
Hepatic Stage: haematopoiesis in liver and spleen
Myeloid stage: haematopoiesis in bone marrow
What are the haematopoiesis stages? (3)
4-5 years of age
At what age does yellow marrow begin to replace some of the red marrow?
- sternum
- vertebrae
- ribs
- clavicles
- skull
- pelvis
- proximal ends of long bone
What are the sites of red marrow in the adult?
pluripotent haematopoietic stem cells
What is the precursor to all blood cells?
0.5%
What portion of nucleated bone marrow cells is accounted for by pluripotent stem cells?
red cells, platelets, monocytes, neutrophils, basophils, eosinophils
Which mature cells arise from the myeloid progenitor cell?
T and B lymphocytes, NK cells
Which mature cells arise from lymphoid progenitor cells?
Colony forming units (CFU) which further differentiate to mature blood cells
What is the next step of differentiation from progenitor cells?
- decreased size
- increased cytoplasmic volume
- decrease in RNA -> decrease in basophilia
- granules appear and condense
- Chromatin thickens, becomes coarse and irregular
- relative amount of cytoplasm increases
List some changes that occur during cell maturation
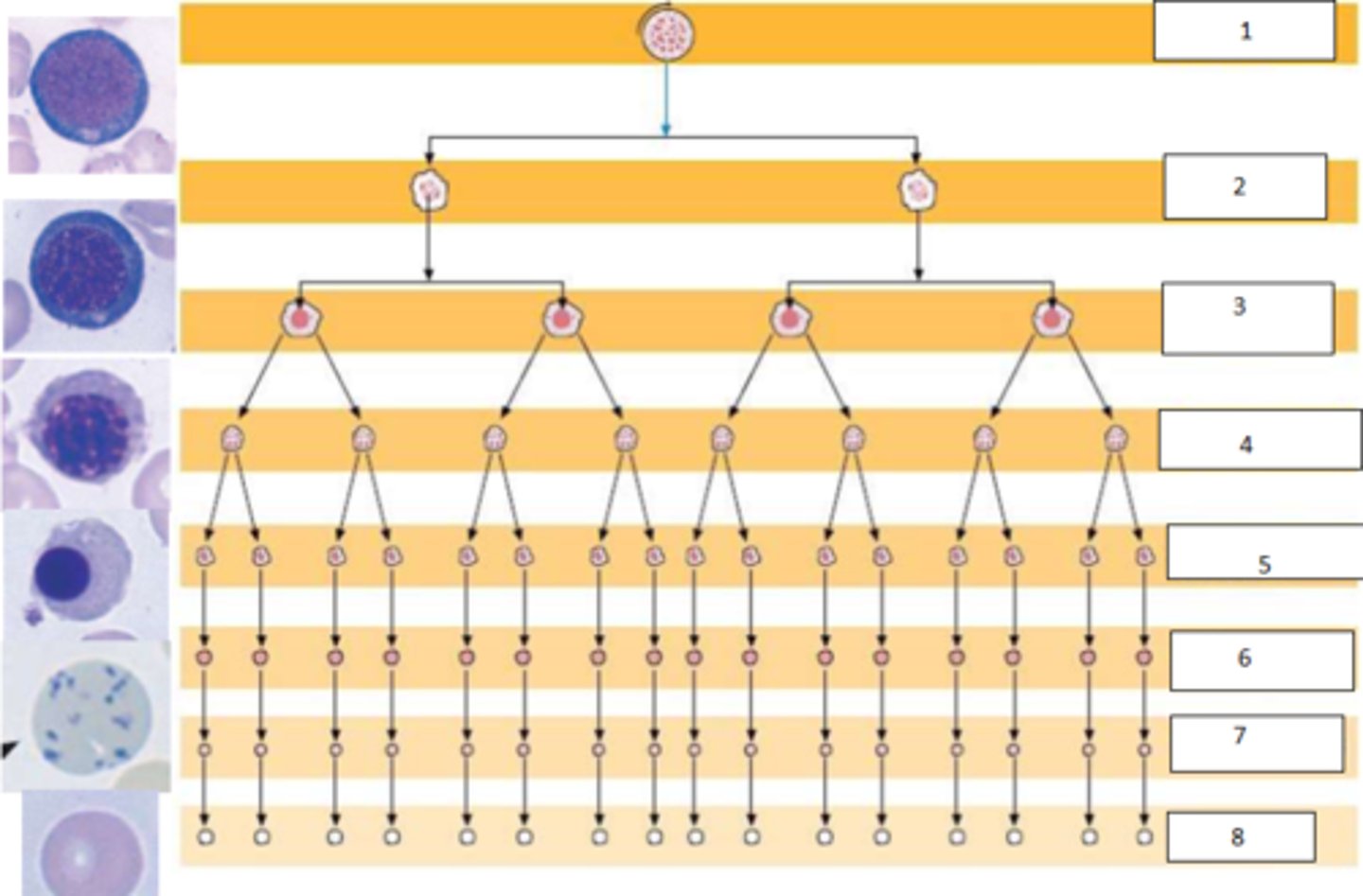
1. pluripotent stem cell
2. Pronormoblast
3. basophilic normoblast
4. polychromatophilic normoblast
5. orthochromic normoblast
6. shift reticulocyte - BM
7. reticulocyte - PB
8. erythrocyte
Name the steps of erythropoiesis
5-9 days
How long does erythropoiesis take?
in the spleen
Where does the reticulocyte undergo its final maturation?
Absence of granules (RNA) and absence of basophilia (in mature erythrocyte)
How might you tell the difference between a reticulocyte and a mature erythrocyte?
haematopoietic growth factors (such as erythropoietin and thrombopoietin among others)
Aside from environmental conditions, what else is required for maturation of blood cells?
These glycoprotein paracrine messengers are produced by many cells and act synergistically to affect the maturation of many blood cell lineages
Describe some characteristics of haematopoietic growth factors and what they do
This cytokine stimulates erythropoiesis, all steps of maturation, and release
What is the role of erythropoietin?
In the kidneys
Where is erythropoietin produced?
hypoxia and hemolysates (released during hemolysis)
What stimulates erythropoietin release?
Vitamin B12, Folic acid, Vitamin C, riboflavin (B2), pyridoxine (B6), iron, copper, manganese, cobalt, zinc, calcium, erythropoeitin, thyroxin, testosterone, ACTH, Cortisol, GH, PTH, essential amino acids, lipids
Name 10 factors important for erythropoiesis (vitamins, minerals, hormones, etc)
Folic acid is essential for DNA synthesis and thereby cell division
How does folic acid aid erythropoiesis?
2 alpha and 2 beta chains, each containing an iron-containing heme-group
What are the units of haemoglobin?
To the iron atom
To which part of haemoglobin does oxygen bind?
2,3-Bisphosphoglycerate (2,3-BPG) is derived from 1,3-bisphosphoglycerate (1,3-BPG), an intermediate of glycolysis. During hypoxia, glycolysis is upregulated, increasing the levels of 1,3-BPG. This can lead to elevated 2,3-BPG production. 2,3-BPG binds to haemoglobin and decreases its affinity for oxygen, facilitating oxygen release to tissues.
How can hemoglobin decrease its oxygen affinity and thereby oxygen supply to tissues, during hypoxia?
gamma-chain - this has a higher oxygen affinity
Which foetal haemoglobin chain precedes the beta chain? How does it differ?
Via macrophages in blood and also via the spleen, liver and bone marrow.
How are erythrocytes degraded?
Haeme is degraded to bilirubin and eventually progresses to urobilinogen. Urobilinogen is excreted via faeces
How is haeme degraded and excreted?
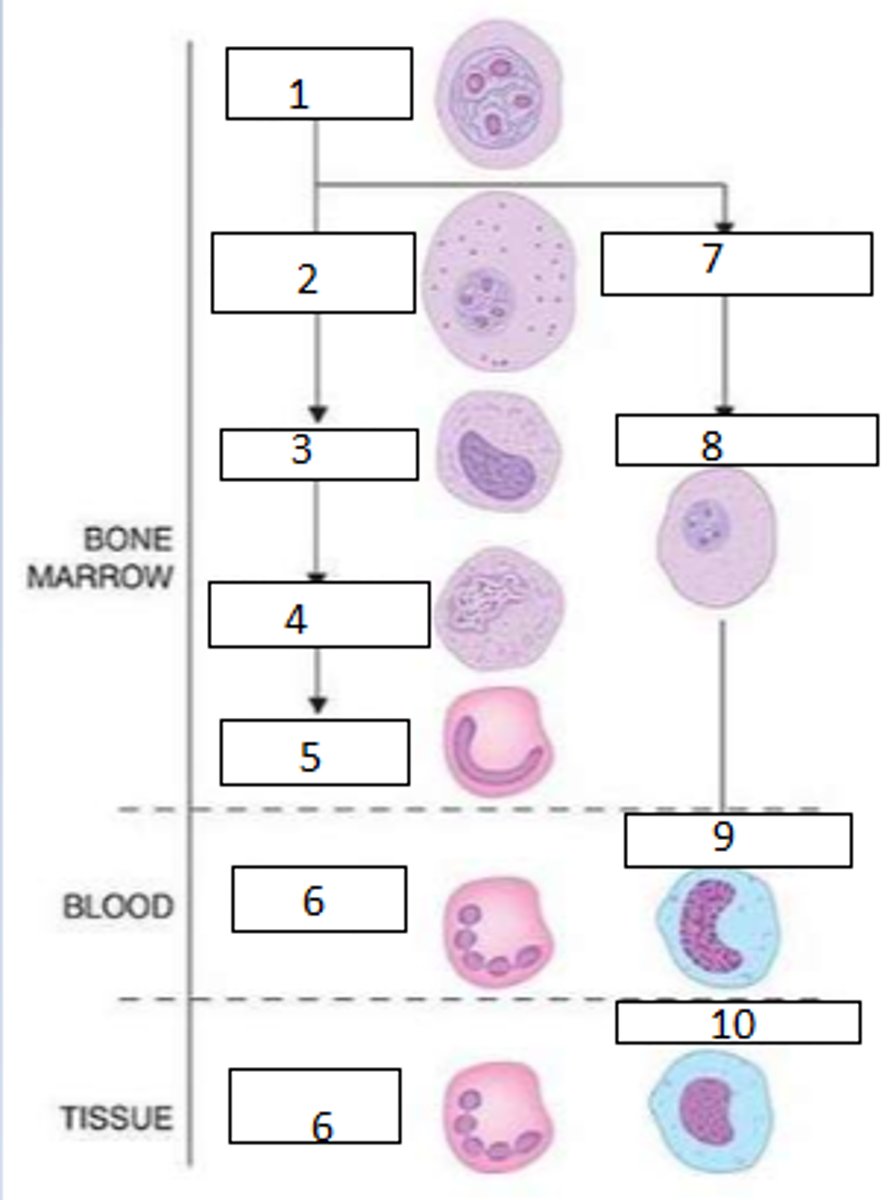
1. myeloblast
2. promyelocyte
3. myelocyte
4. metamyelocyte
5. Band form
6. neutrophil
Complete the left cascade
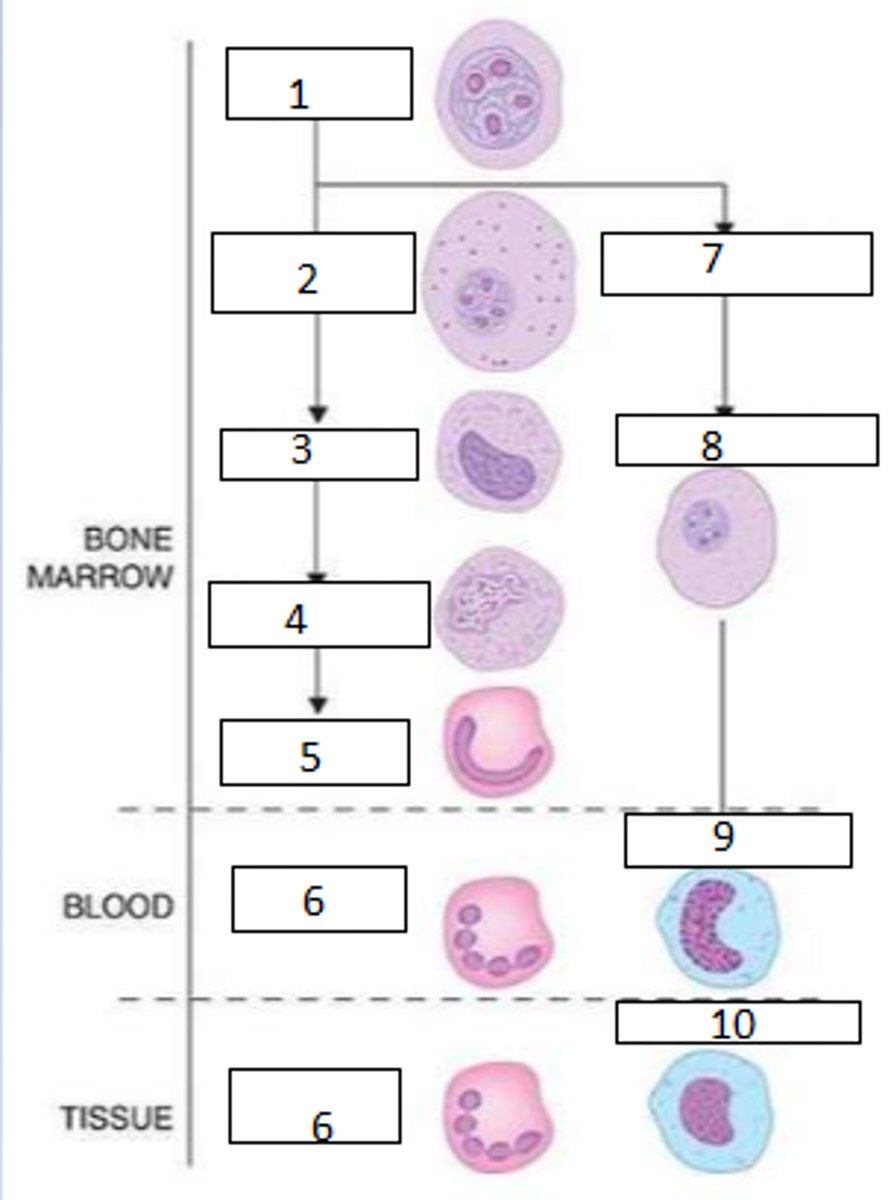
1. myeloblast
7. myelomonoblast
8. promonocyte
9. monocyte
10. macrophage
Complete the right cascade (include step 1)
G-CSF: granulocyte colony stimulation factor
Which factor is used clinically to increase neutrophil production?
Between the orthochromoblast and reticulocyte stages the nucleus is pushed to the periphery and removed.
At which stage of erythropoiesis does the nucleus disappear?
reticulocytes and mature erythrocytes
Which stages of erythrocytes can be found in the blood?
polychromatophilic normoblast
At which stage of erythropoiesis does hemoglobin appear?