NPB101 lectures 38-41
1/103
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
104 Terms
What is the general function of respiration?
Obtain O2 for use by the body’s cells and to eliminate CO2 the body cells produce
What does respiraiton encompass?
External repsitation and internal (cellular) respiration
Why do we have 2 passages to breathe?
IN case one does not work or we cannot breathe through one
What encompasses the repsiratory system?
The airways leading to the lungs, lungs, and the structures of the thorax involved in producing movement of air though the airways into and out of the lungs
What are the respiratory airways?
Trachea and larger bronchi
Describe the trachea and bronchi.
Fairly rigid, non-muscular tubes composed of rings of cartilage to prevent collapse
Why is there smooth muscle surrounding the bronchi?
TO constrict and relax the airways
(T/F) The bronchioles contain cartilage to hold them open.
False, their walls contain smooth muscle innervated by autonomic nervous system
What does the autonomic nervous system do to the bronchiole’s walls.
Parasympathetic stim. constricts while sympathetic (weakly) relaxes
What do they type 2 alveolar cells produce?
Pulmonary surfactant that keeps the cell open
Why is the alveolus so much larger than the erythrocyte?
TO have efficient exchange of O2 and CO2
What are the alveoli?
Thin-walled inflatable sacs that function in gas exchange
What do the walls of the alveoli contian?
Single layer of flattened Type I alveolar cells
What do Type II alveolar cells secrete?
Pulmonary surfactant
What do alveolar macrophages do?
Guard the lumen
(T/F) pulmonary capillaries encircle each alveolus and they are all interconnected.
True
What does the surfactant produced by type II alveolar cells do?
Disrupts hydrogen bonding of water lining the alveolar wall and decreases siurface tension
Why is water dangerous in the alveolar wall?
Can cause collapse of the alveola
Why do the Type II alveolar cells need to decrease surface tension?
So large groups of small bubbles don’t collapse into a smaller number of larger ones
What induces the surfactant secreted by type II alveolar cells at birth?
Cortisol, just prior to birth
What do premature babies need to ensure they have proper lung function?
Synthetic glucocorticoid
What are the lungs suspended in?
A pleural sac that surrounds it
What is the pleural sac?
A double-walled, closed sac that separates each lung from the thoracic wall
What is the pleural cavity?
Interior of the pleural sac
What is the lubricant that is secreted by the surfaces of the pleura?
Intrapleural fluid
What is the purpose of the Intrapleural fluid?
To reduce friction from the lungs
What are the 3 important pressures for ventilation?
Atmospheric, intra-alveolar, and intrapleural pressure
What is atmospheric pressure (commonly)?
760 mm Hg
What is the intra-alveolar pressure?
760 mm Hg
What is the intrapleural pressure?
756 mm Hg
What produces the flow of air into and out of the lung?
Changes in intra-alveolar pressure
If intra-alveolar pressure is less than atmospheric, then air….
enters the lungs
If intra-alveolar pressure is greater than atmospheric pressure…
Air leaves the lungs
What pressure NEEDS to drop for air to enter?
intra-alveolar pressure
What NEEDS to increase for air to leave the lungs?
intra-alveolar pressure
What muscle help in bretahing?
Diaphragm and external intercostal muscle
(T/F) Lungs have elastic recoil
True
What other muscle is recruited when we are actively forcing air and in out of our lungs?
Abdominal muscles
Why do lungs have elastic recoil?
Highly elastic connective tissue in the lungs
Alveolar surface tension
What is tidal volume?
The average volume taken in when relaxed (~500mL)
What is the inspiratory reserve volume?
Air we can take in when needed (~3000mL)
What is the inspiratory capacity?
The max amount of air a person can take in (~3500mL)
What is residual volume?
The amount of air present in the lungs even after the max amount of air is forced out, present to prevent collapse (~1200mL)
What is the expiratory reserve volume?
The max amount of air a person can force out of their lungs (~1000mL)
What is the pulmonary ventilation (mL/min)?
The tidal volume (mL/breath) * respiratory rate (breath/min)
What is dead space?
The amount of “old” air that is in our lungs that has exchanges O2 and CO2
(T/F) Everyone has the same Tidal volume.
False, it changes from person to person, with larger lungs having more space
What is the: tidal volume, respiratory rate, dead space, pulmonary ventilation, and alveolar ventilation in Quiet breathing at rest?
TV: 500
RR: 12
Dead space: 150
Pulmonary ventilation: 6000
Alveolar ventilation: 4200
What is the: tidal volume, respiratory rate, dead space, pulmonary ventilation, and alveolar ventilation in Deep, slow breathing?
TV: 1200
RR: 5
Dead space: 150
Pulmonary ventilation: 6000
Alveolar ventilation: 5250
What is the: tidal volume, respiratory rate, dead space, pulmonary ventilation, and alveolar ventilation in Shallow, rapid breathing?
TV: 150
RR: 40
Dead space: 150
Pulmonary ventilation: 6000
Alveolar ventilation: 0
(T/F) Large blood flow helps balance small airflow, and vice versa.
True
What happens when there is small airflow and large blood flow?
Increase CO2, decrease O2
Relaxation of local airway smooth muscle, increase in constriction of pulmonary arteriolar smooth muscle
Dilation of local airways, constriction of blood vessels
Decrease airway resistance, increase vascular resistance
Increase airflow, decrease blood flow
What happens when there is large airflow and small blood flow?
decrease CO2, increase O2
Contraction of local airway smooth muscle, relaxation of pulmonary arteriolar smooth muscle
constriction of local airways, dilation of blood vessels
increase airway resistance, decrease vascular resistance
decrease airflow, increase blood flow
Why is the the diffusion constant of CO2 so high compared to O2?
Helps to offset the small partial pressure of CO2
(T/F) At pulmonary and tissue capillary levels, gas exchange involves simple diffusion.
True
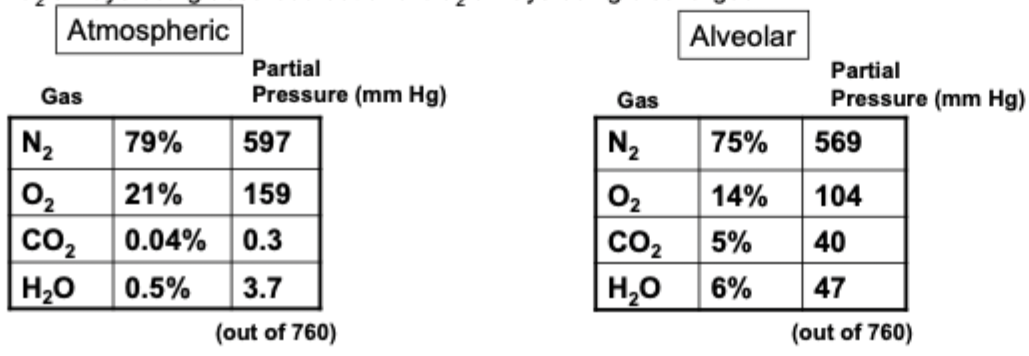
What does the partial pressure exerted by each gas in a mixture equal to?
Total pressure * fractional composition of gas in mixture
Why is alveolar air composition different than atmospheric air?
Increased water vapor as air travels thru respiratory system
Dead space and residual volume not all air in alveoli is fresh, higher CO2 and lower O2\
O2 always being absorbed out and CO2 always being discharged in
How do O2 and CO2 exchange across the pulmonary and system capillaries?
Partial pressure gradients

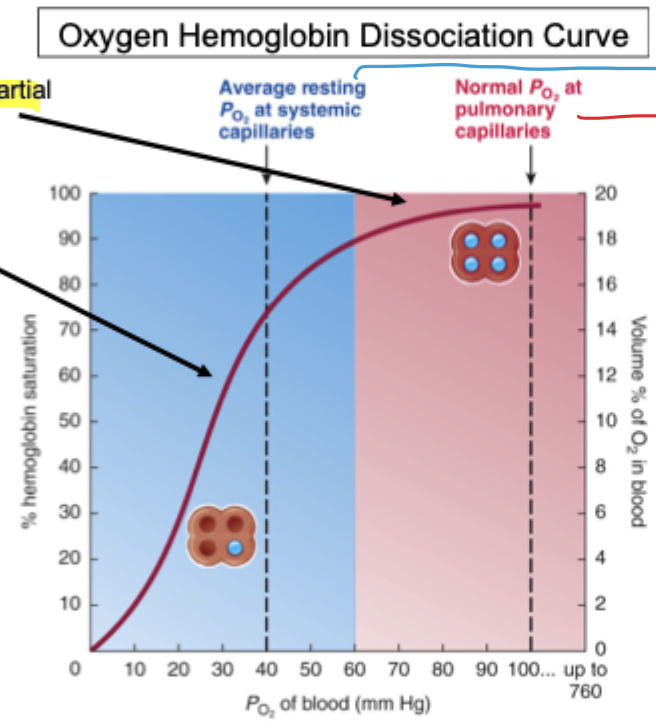
How is most oxygen transported?
Bound to hemoglobin in erythrocytes (RBCs)
What is main factor determining the % of hemoglobin saturation?
Partial pressure of O2
The percent saturation (of heme) is high where the pO2 is _____. and vice versa.
high
The percent saturation(of heme) is _____ where pO2 is high and vice versa.
high
Where is the pO2 high?
lungs
Where is the pO2 low?
tissues
What does O2 do at the tissue cells?
Dissociate from hemeoglobin
When O2 binds to hemoglobin, the affinity for O2 goes (up/down).
up
Why does the steep part of the Oxygen-hemoglobin dissociation curve exist?
This is where hemoglobin unloads O2 to the tissue cells
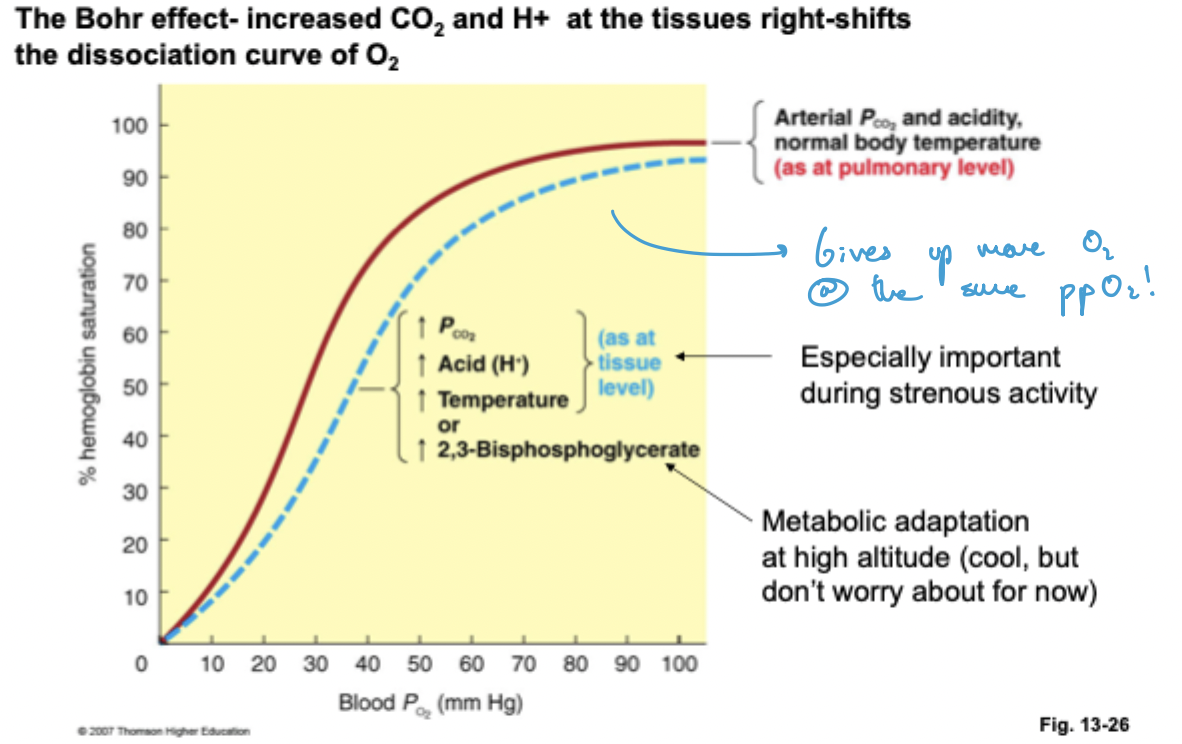
What does the Bohr effect mean?
Increased CO2 and H+ at the tissue level shifts the dissociation curve (i.e. O2 is unloaded more readily at the same pO2)
WHat is the Haldane effect?
Reduced O2 in the tissues facilitates the loading of Hb with CO2 and H+ while increase O2 in the lungs promotes the dissociation of CO2 form Hb
What is the Chloride shift?
The inward shift of Cl- in exchange to the efflux of HCO3- from RBCs
What is primary form CO2 is moved as?
HCO3-
What does carbonic anhydrase do?
Facilitates the reaction of CO2 and H2O into HCO3- and H+, dependent on concentration
(T/F) In sickle cell anemia, only a single point mutation in the b-chain causes a defective Hb.
True
How does sickle cell anemia affect gas exchange?
Reduces it
What is the problem with hypoventilation?
Underventilation, increasing pCO2 and respiratory acidosis (increase pH)
What is the problem with hyperventilation?
INcreased pulmonary ventilation, decreased pCO2 and respiratory alkalosis
What are the nueral networks that control rhythmic firing of motor neurons to diaphragm?
Medullary respiratory centers
Dorsal respiratory group (DRG)
Ventral respiratory group (VRG)
Pons respiratory centers
Modulate activity of medullary centers to promote smooth breathing rhythms
What is the dorsal respiratory group?
Inspiratory neurons that are active in normal, quiet breathing
What is the ventral respiratory group?
Inspiratory and expiratory neurons that are activated on demand (exercise)
What is the pro-botzinger complex?
A region rostral from the VRG where respiratory rhythm is generated
What is the Hering Breuer reflex?
Stretch receptors in smooth muscles of the bronchioles that prevents the over-inflation of the lungs
As CO2 increases, ventilation ______.
increases
As O2 increases, ventilation _______.
Decreases
(T/F) Low pH is initially beneficial, but can become dangerous.
True
Where are the carotid bodies located?
Carotid sinus
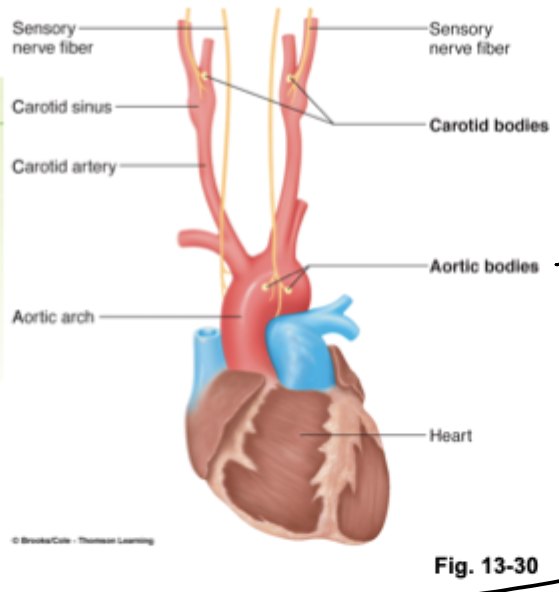
Where are the aortic bodies located?
Aortic arch
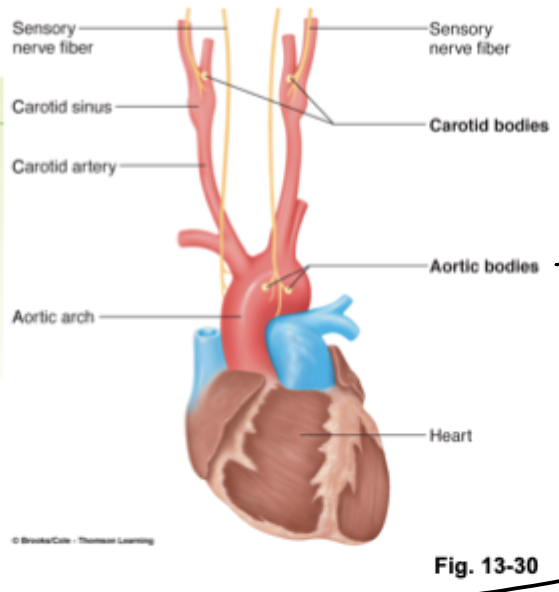
The carotid bodies and aortic bodies are ____-receptors.
Chemo
WHat happens if there is low pO2 in arterial blood (peripheral)?
Stimulates the carotid and aortic bodies when it has fallen to the point of being LIFE-THREATENING.
What happens if there is an increase in pCO2 in arterial blood (peripheral)?
Weakly stimulates carotid and aortic bodies.
What happens if there is an increase in the H+ in arterial blood (peripheral)?
Stimulates the carotid and aortic bodies, important in acid-base balance.
Why is hemoglobin always partially saturated?
High altitude and suffocation response
Explain what happens when there is a decrease in inspired pO2.
leads to: decrease in alveolar pO2, which leads to decreased arterial pO2, which increases the peripheral chemoreceptors firing, which increases contraction of respiratory muscles, which increases ventilation which returns the alveolar and arterial pO2 towards normal.
What are the peripheral chemoreceptors?
Carotid and aortic bodies
In the central chemoreceptors, what happens when there is a decrease in pO2 in arterial blood?
Directly depresses the central chemoreceptors and the respiratory center itself when lower than 60mmHg
In the central chemoreceptors, what happens when there is an increase in pCO2 in the arterial blood and increase in brain H+?
STRONGLY stimulates, dominant control of ventilation
In the central chemoreceptors, what happens when there is an increase in H+ in arterial blood?
Nothing, it cannot pass the blood-brain barrier
(T/F) There is NO H+ in the brain.
False, while arterial H+ cannot pass the blood-brain barrier, H+ can be present in the brain ECF if it is brain derived (i.e. from CO2 forming HCO3- and H+).
Why do the central chemoreceptors weakly stimulate the peripheral chemoreceptors?
Keeps the medullary respiratory center in check so it does NOT hypoventilate
Why is CO dangerous?
CO binds to hemoglobin irreversibly and with much more affinity
(T/F) The diaphragm is the main muscle we use during quiet (resting) inspiration.
True