Embryology Midterm
1/270
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
271 Terms
Are ASD's usually symptomatic in childhood?
Rarely, except in coincidental lung disease
ASD's are more common in __________ (men/women)
women
ASD's are the ______ most common CHD.
3rd
What is potential long-term consequence of an ASD?
Eisenmenger's syndrome - when an ASD causes high blood pressure in the lungs (PHTN)
Types of ASD's
PFO (not rlly), sinus venosus (not rlly), secundum, primum, AV canal, coronary sinus (also not rlly)
What is the limbic band a remnant of?
the septum secundum
What is the most common type of ASD?
secundum ASD
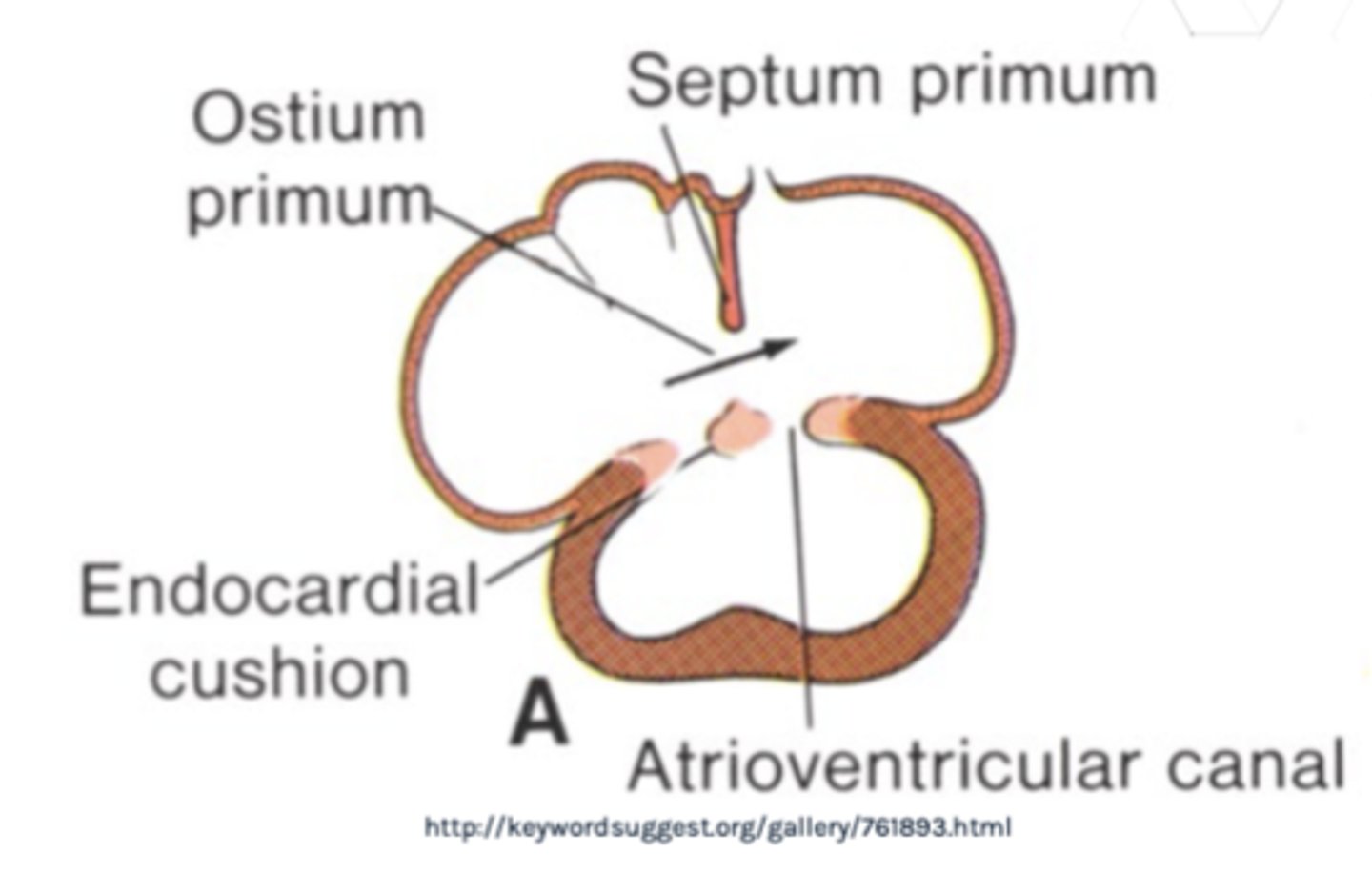
Secundum ASD
inadequate growth (or defective growth) of septum primum (fossa ovalis)

Primum ASD's are associated with...
endocardial cushion defects (partial, transitional, complete)
What is the most common type of sinus venosus defect (SVD)?
absence of tissue between the RUPV and SVC
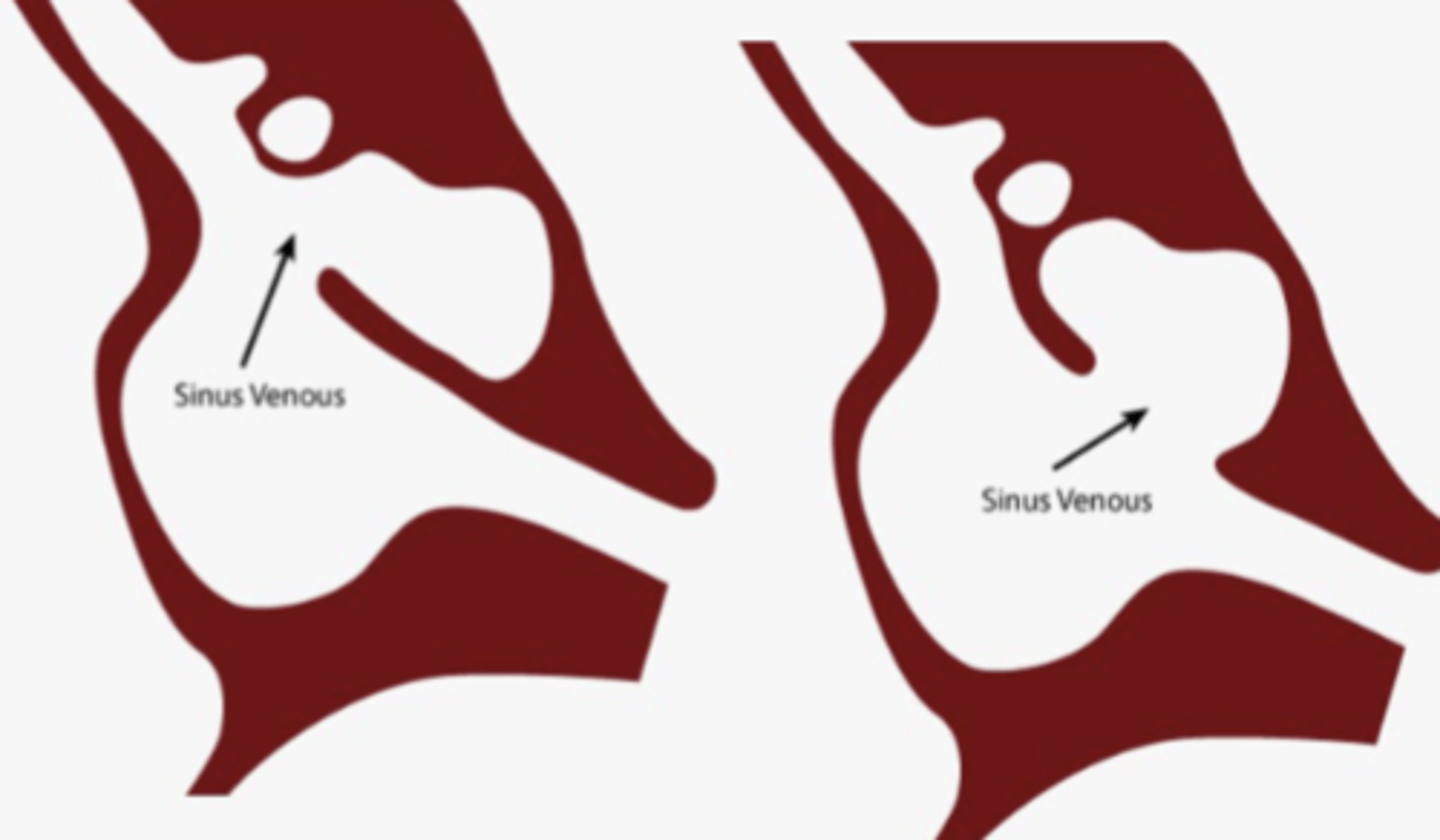
SVD ultrasound
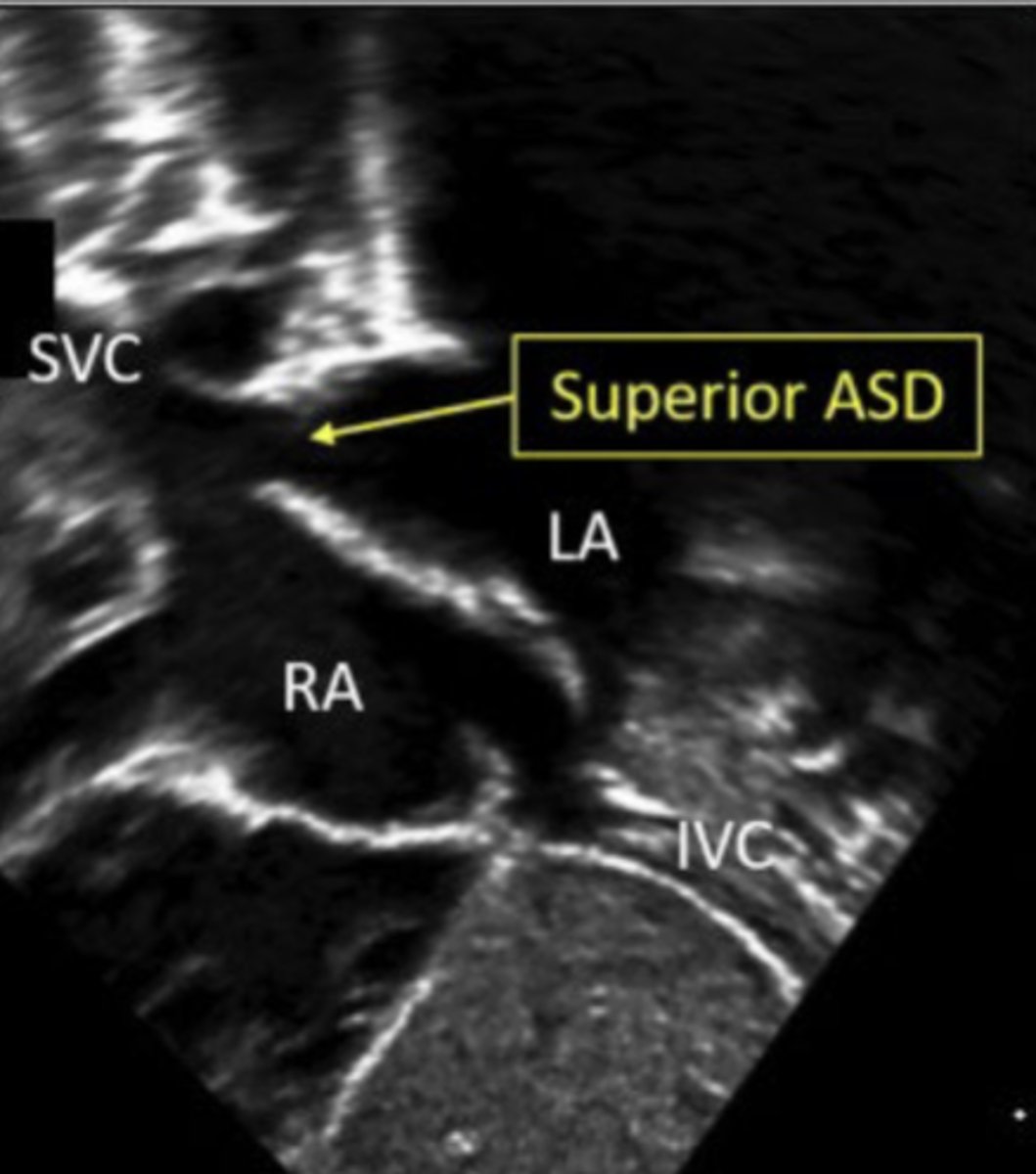
Sinus Venosus ASDs should be suspected in patients who demonstrate...
unexplained right ventricular volume overload
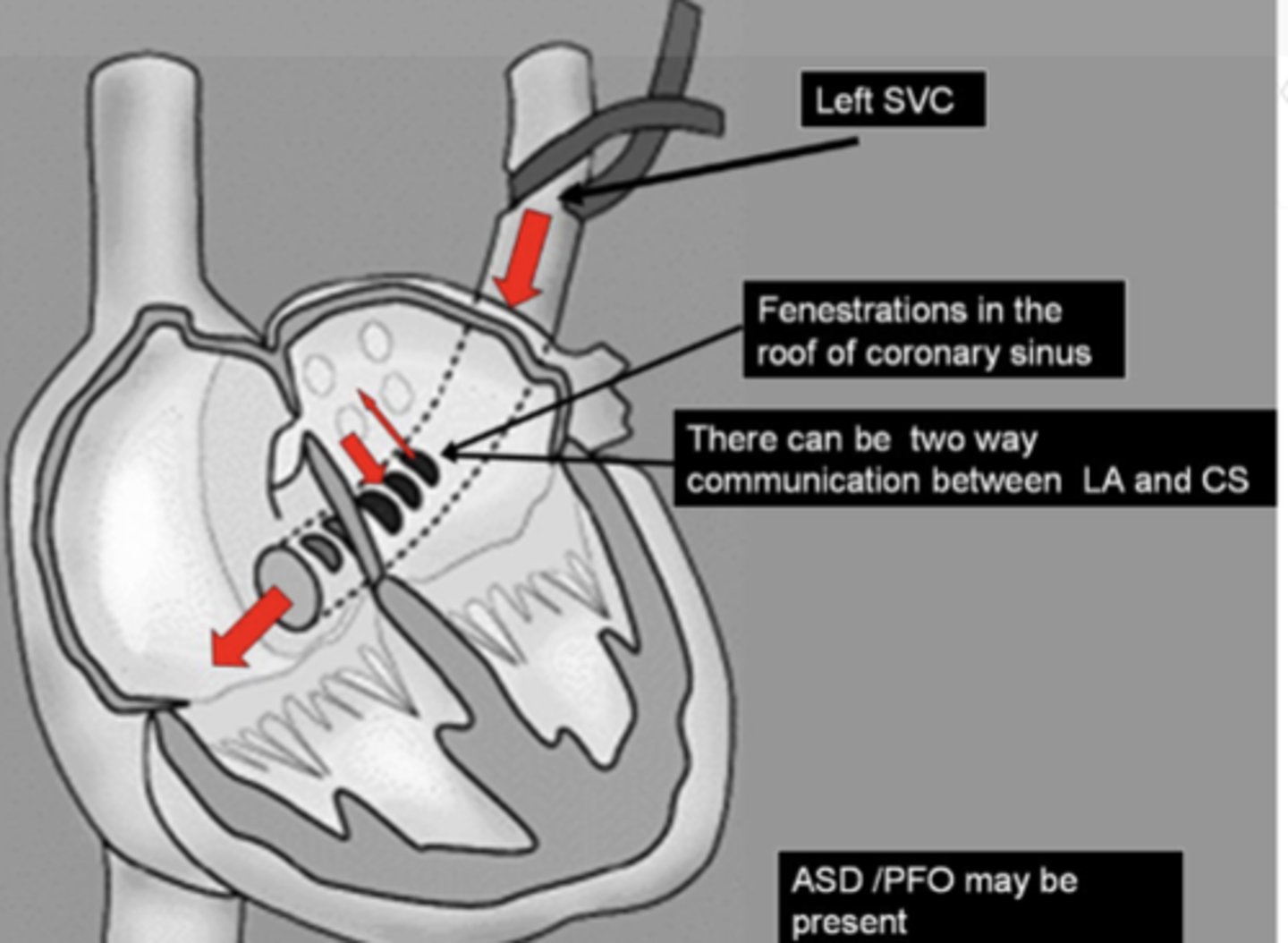
Coronary Sinus Defect
Unroofing (either complete or partial) of the coronary sinus
Raghib Syndrome
persistent LSVC that drains through the coronary sinus
What do we look for with Echo?
Size, location and number of the defects
Shunt flow direction
Measure with calipers
Multiple views - 2D & 3D
What is its relationship to neighboring structures? (next slide)
SL & AV valves/pulmonary & systemic veins
Evaluate biventricular function
Detect associated lesions
How do we evaluate hemodynamic assessment?
Flow direction (color & spectral Doppler)
Transseptal pressure gradient
How do we evaluate hemodynamic load?
RAE, RVE & MPA/branch dilation
Diastolic septal flattening (D shape MV in PSAX)
Increased pulmonary blood flow
Estimate RVSP
Biventricular systolic function
Pre-atrial level shunts:
Partial anomalous pulmonary venous return (PAPVR)
Atrial level shunts:
ASD's of all sorts
Ventricular level shunts:
VSD's, AV canal, etc.
Great Artery level shunts:
PDA, coronary fistulae, etc.
Crossing levels shunts:
various fistulae, AVM's, LV to RA shunts
Amount of shunting is determined by?
1. Defect size
2. Compliance of the LV and RV
given that there is no AV valve stenosis or hypoplasia
What is a consequence of pre-atrial or atrial left to right shunts?
right heart enlargement
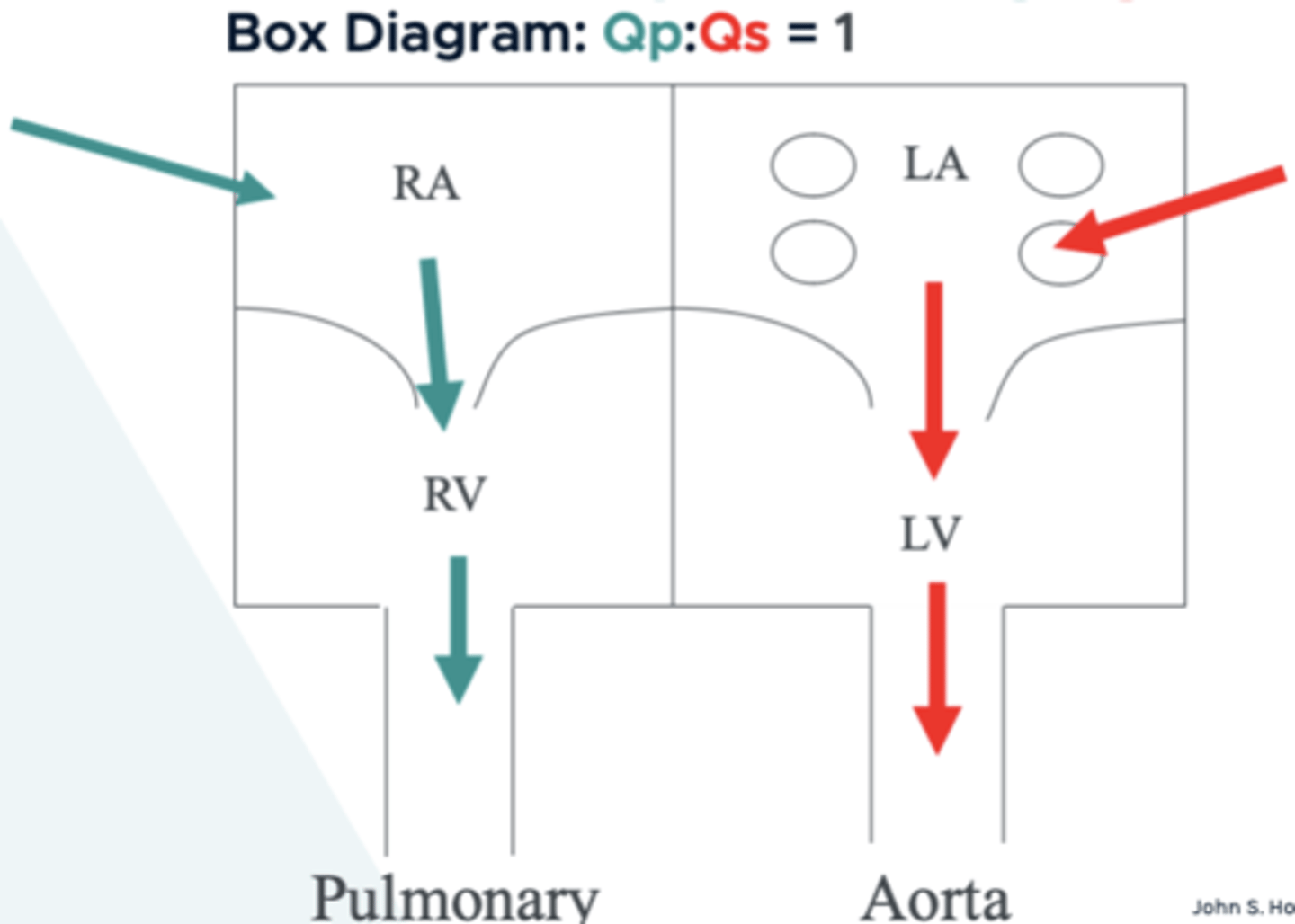
Normal flow volume ratio:
pulmonary:systemic
Qp:Qs = 1
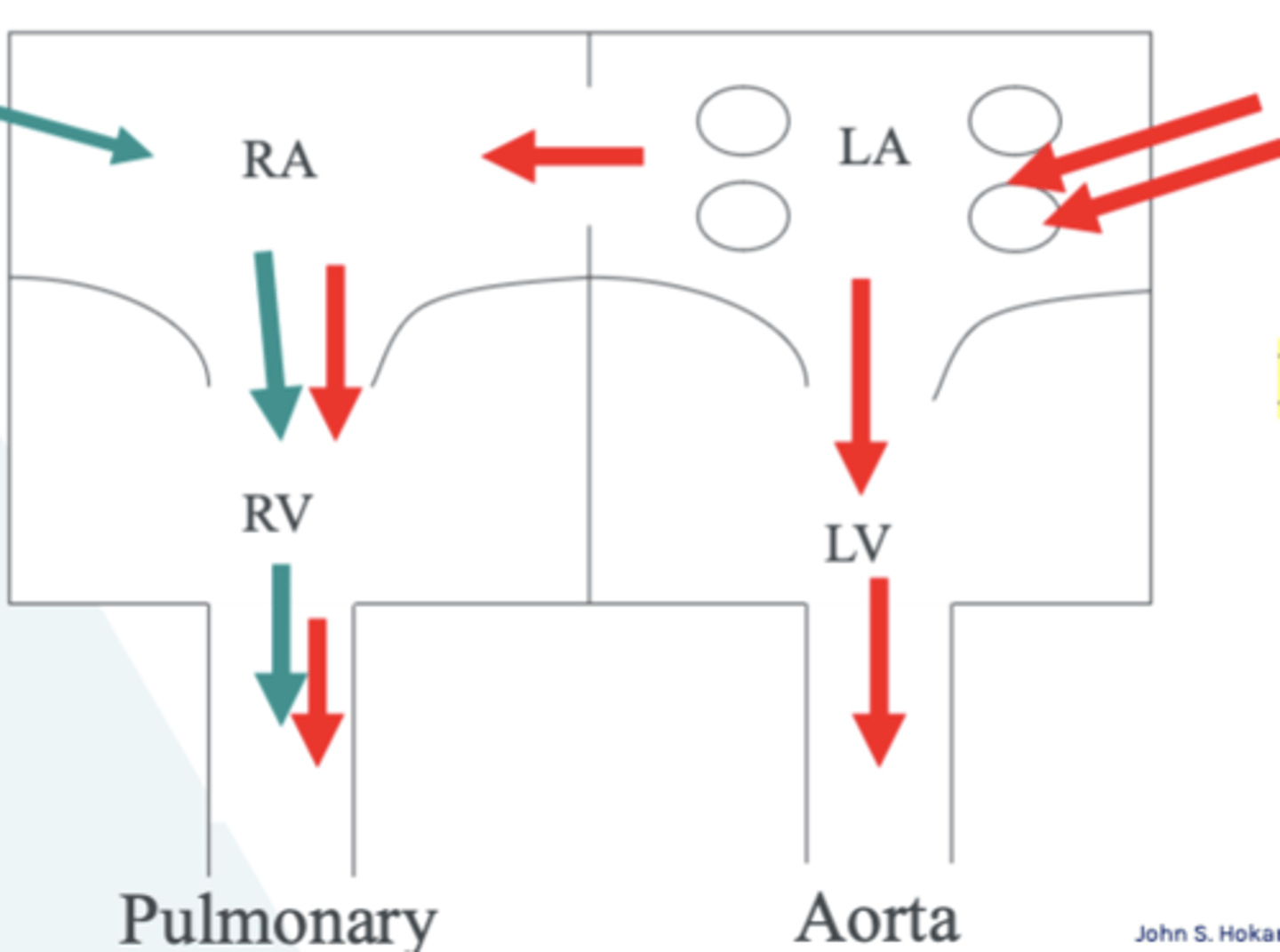
ASD - Qp:Qs = 2:1 (left to right)
Fixed split S2 and pulmonary flow murmur
RA, RV, MPA enlarged
Eisenmenger's Syndrome
ASD creates a left to right shunt
Shunt causes RA & RV enlargement
Over time, the pulmonary vascular system can't handle the extra shunt flow, which increases PA pressure
When the PA pressure exceeds the Aortic pressure, the shunt will now become right to left across the ASD
This leads to: pulmonary hypertension, cyanosis, low CO & death
ASD - Qp:Qs = <1:1 (right to left)
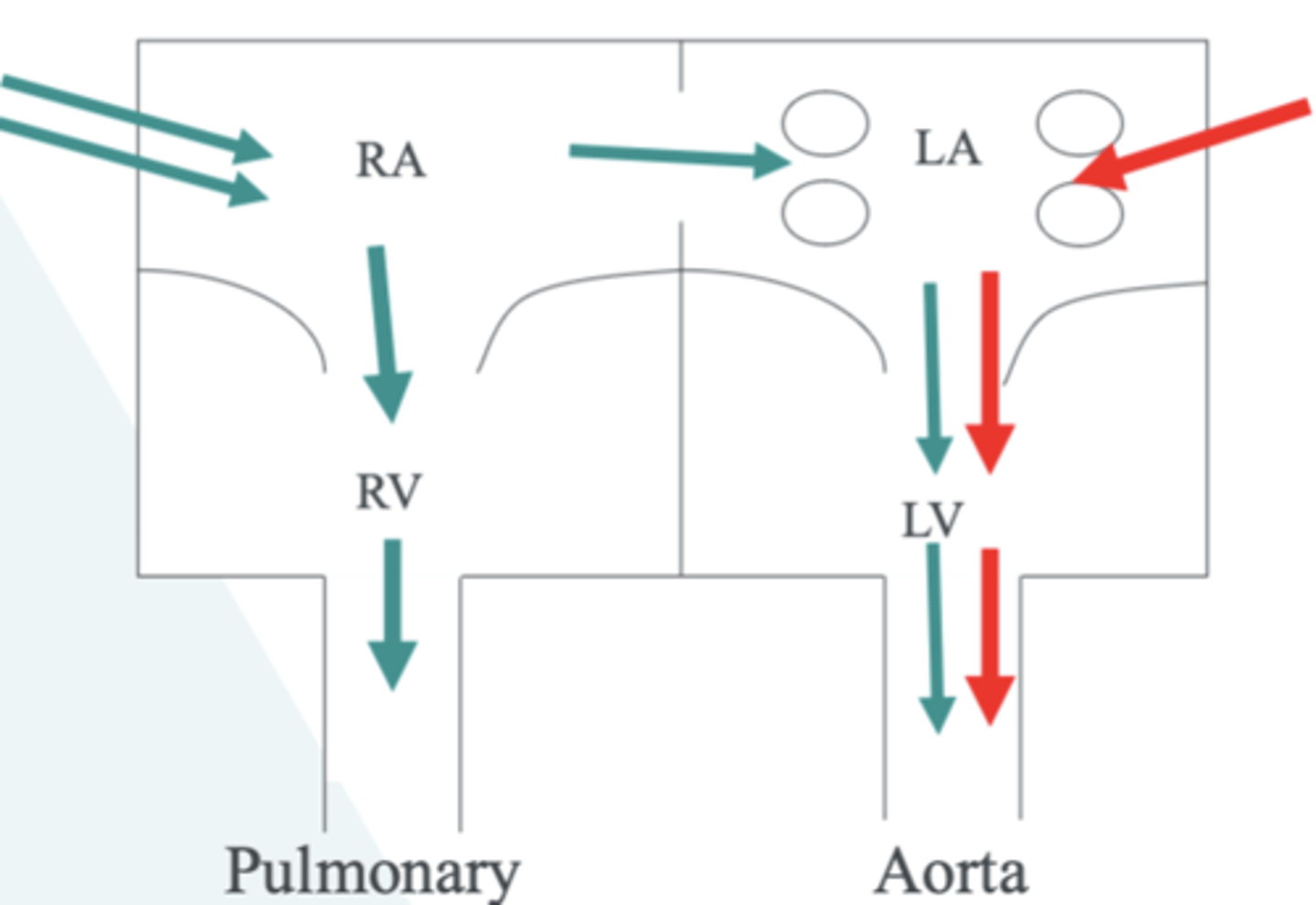
Bidirectional Shunts
Left to right AND right to left shunting at the same level
Qp=Qs
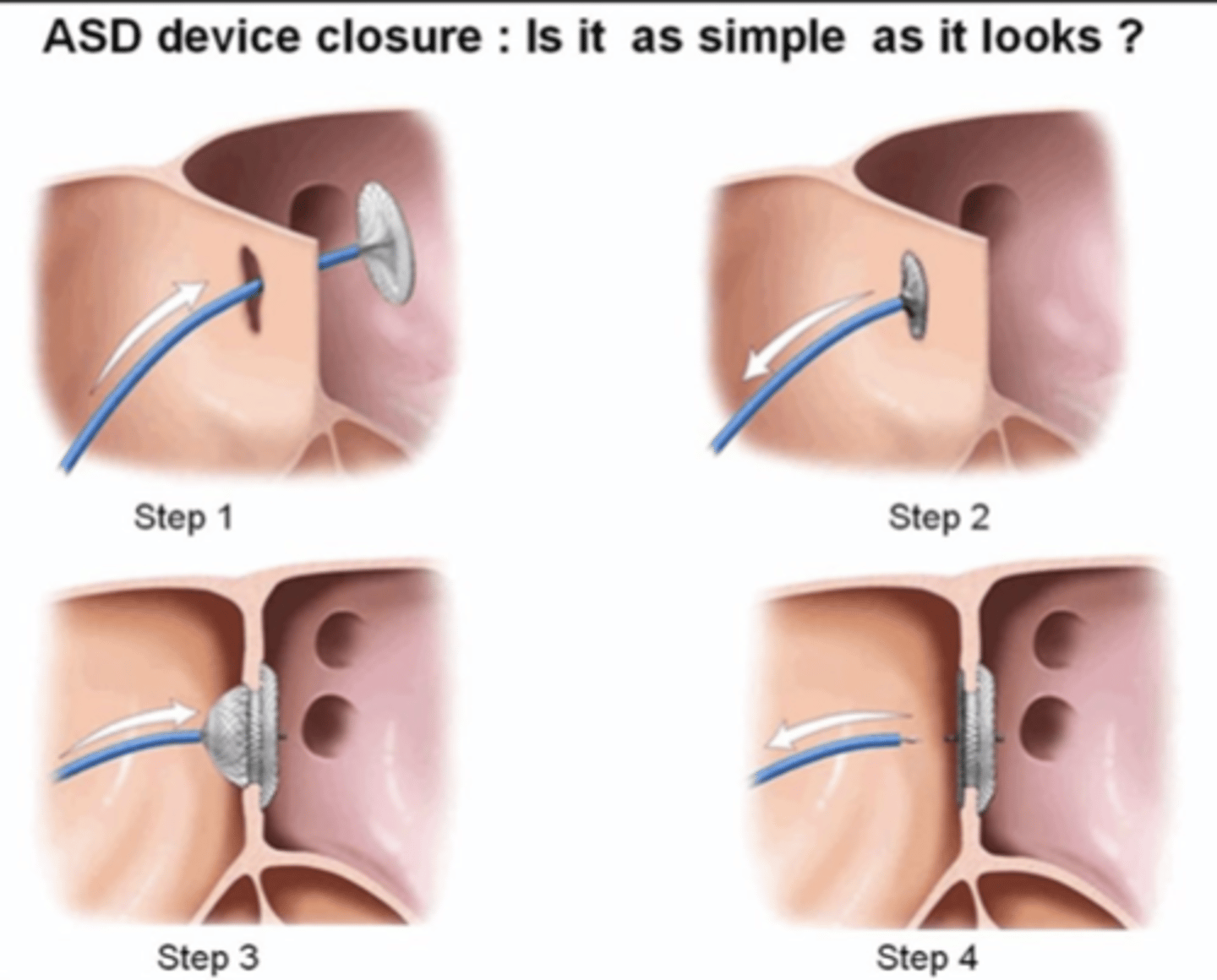
How do they fix an ASD?
Amplatzer or Helix device
What do we look for with Echo...after they fix it?
1. Multiple views of the septum - 2D & 3D
2. Color Doppler to rule out residual ASD flow
3. Evaluate device position
4. Abnormal movement: rocking, flopping or absence of the device all together
5. Impingement of the device on surrounding structures
6. Rule out thrombus or endocarditis in general, and on thedevice as well
7. Estimate RVSP
8. RV size and function - improvement?
Can PFOs cause issues later on?
No they usually won't cause problems down the line
What is a common finding of the IAS in the elderly?
thickening of the muscular septum (not the FO) - dumbbell shape
Ductal dependent lesion
the ductus is the only way the PA or Ao are getting flow (ex. atresia of PV)
What shunt would PHTN cause?
right -> left shunt
What views can you visualize a PFO?
subcostal 4C, bicaval
What do we use to evaluate a shunt?
color, PW
Will the flow through a PFO be high or low velocity?
low
What views can you visualize a sinus venosus ASD?
bicaval, right parasternal
What views can you visualize a coronary sinus ASD?
PLAX, apical 4C (w/ posterior angle)
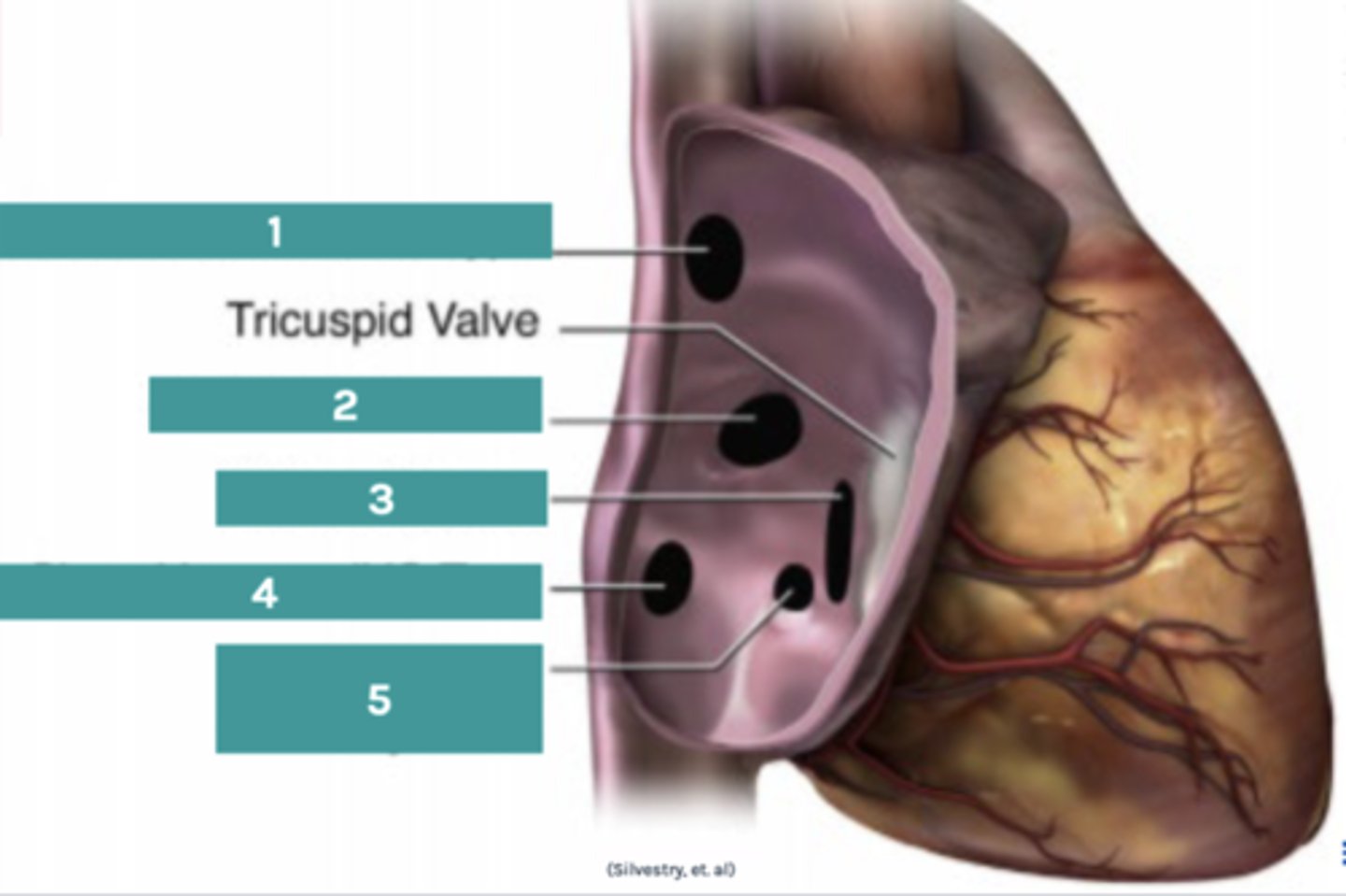
Label the image:
1. Sinus venosus ASD
2. Secundum ASD
3. Primum ASD
4. Sinus venosus ASD
5. Coronary sinus ASD
Will lungs be able to withstand a shunt that directs double the blood flow through the PA?
Yes actually, they are very compliant - but it won't last forever - PHTN
History
Maternal history of Rubella (similar to measles)
Maternal history of SLE (lupus)
Maternal diabetes
Maternal use of medications
Maternal use of alcohol
Maternal use of smoking
Maternal exposure to radiation
Low birth rate
Prematurity
Familial history
Congenital heart disease
Syndromes
Stillbirths
Spontaneous abortion
Birth history
Progress of labor
Method of delivery
APGAR score (Appearance (skin color), Pulse (heart rate), Grimace (reflex irritability), Activity (muscle tone), and Respiration (breathing effort)
Asphyxia during labor/delivery
Symptoms - Serious CHD
Cyanosis, Tachypnea, Swelling (legs, abdomen), Failure to thrive, Poor weight gain, Feeding difficulties, Colic/irritability, Lethargy, Respiratory distress, Diaphoresis, Clinically significant murmur
Symptoms - "Not-so-Serious" CHD
Shortness of breath with exercise or activity, easily tiring during exercise or activity, fainting/syncope during exercise or activity, palpitations, swelling (hands, ankles, feet), innocent murmur
Signs/Physical Exam
Squatting after exercise or activity
Syndrome identification
Down's syndrome
Skeletal abnormalities
Scoliosis
Pyrexia
Clubbing
Blood pressure
Hypertension
Differences in extremities
Pulses & pulse oximetry
Murmur(s)
Diagnostics
Fetal Echocardiogram
Echocardiogram
Electrocardiogram
Chest X-ray
Pulse Oximetry
Cardiac Catheterization
Cardiovascular Magnetic Resonance Imaging
Computed Tomography
Exercise Stress test (imaging or non-imaging)
Indications & AUC
Failure of 20-week OB/fetal echocardiogram
Failure of any antenatal exam
Abnormal EKG
Chest pain
Congestive heart failure
Cyanosis
Desaturation
Hypertension
Murmur
Syncope
Palpitations
Fatigue
Fever
Chemotherapy
Systemic disorders
Family history of CHD
Maternal history
Obtain the following before every exam:
Height/Length
Weight
Blood pressure
O2 Saturations (when clinically indicated)
When do we use EKGs?
ALL outpatients over the age of 3
Do we use high or low color scale the evaluate the coronaries? What about the valves and shunts?
low; high
Subcostal - transducer position
3 o'clock - transducer in neutral position (not looking up this time)

What is the goal of subcostal?
to establish and document thoracic-abdominal situs
What anatomy do we include in the first subcostal sweep?
Liver, stomach, IVC, abdominal aorta
What pathologies can be identified in the first subcostal sweep?
Interrupted IVC, abnormalities of abdominal visceral situs, pleural effusions
Subcostal Sagittal - transducer position
rotate probe so notch is at 12 o' clock - tilt and sweep from right to left until aorta comes into view

What is the ideal angle of insonation for PW interrogation of the abdominal aorta?
as close to less than or equal to 30 degrees as possible
Subcostal Coronal - transducer position
rotate notch to 3 o' clock and tilt transducer anteriorly (up)

What are we looking for with the posterior to anterior sweep?
Dextrolooping, atrial identity, ventricular identity, AV connections
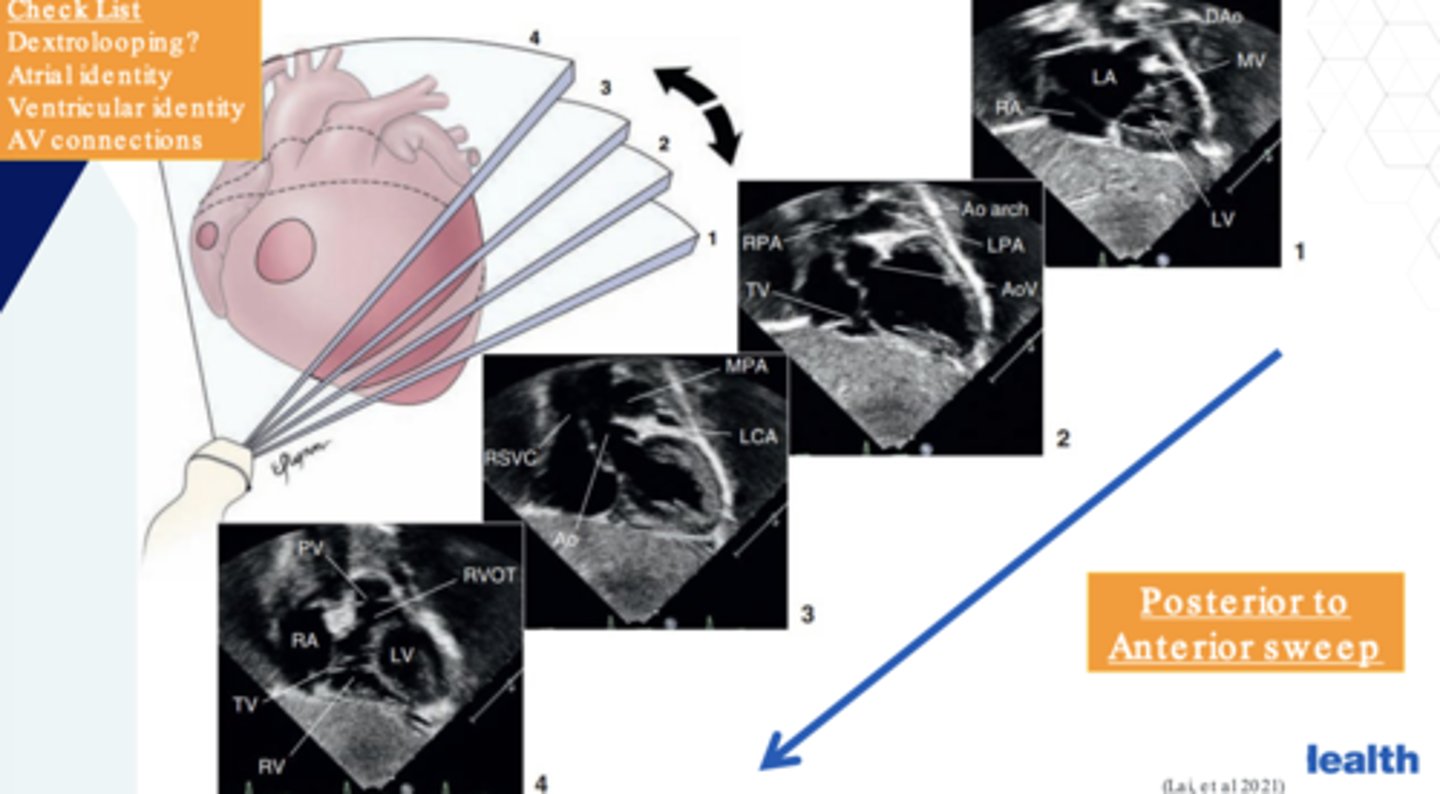
What other anatomy are we evaluating in the subcostal coronal view?
If the atrial septum and ventricular septum is intact
Left Anterior Oblique (LAO) transducer position:
Transducer is midline, notch is to 4:30
Right Anterior Oblique (RAO) transducer position:
Transducer is midline, notch is to 2 o' clock
Which veins do we focus on for venous anomalies?
SVC
IVC
Azygos vein
Hemiazygos vein
Hepatic veins
Coronary sinus
What are the 3 things we should be thinking about with venous anomalies?
Atrial situs - which systemic veins come into which atria
Prevalence - persistent left superior vena cava is most common
Embryology - which veins regress and which veins stay patent and why
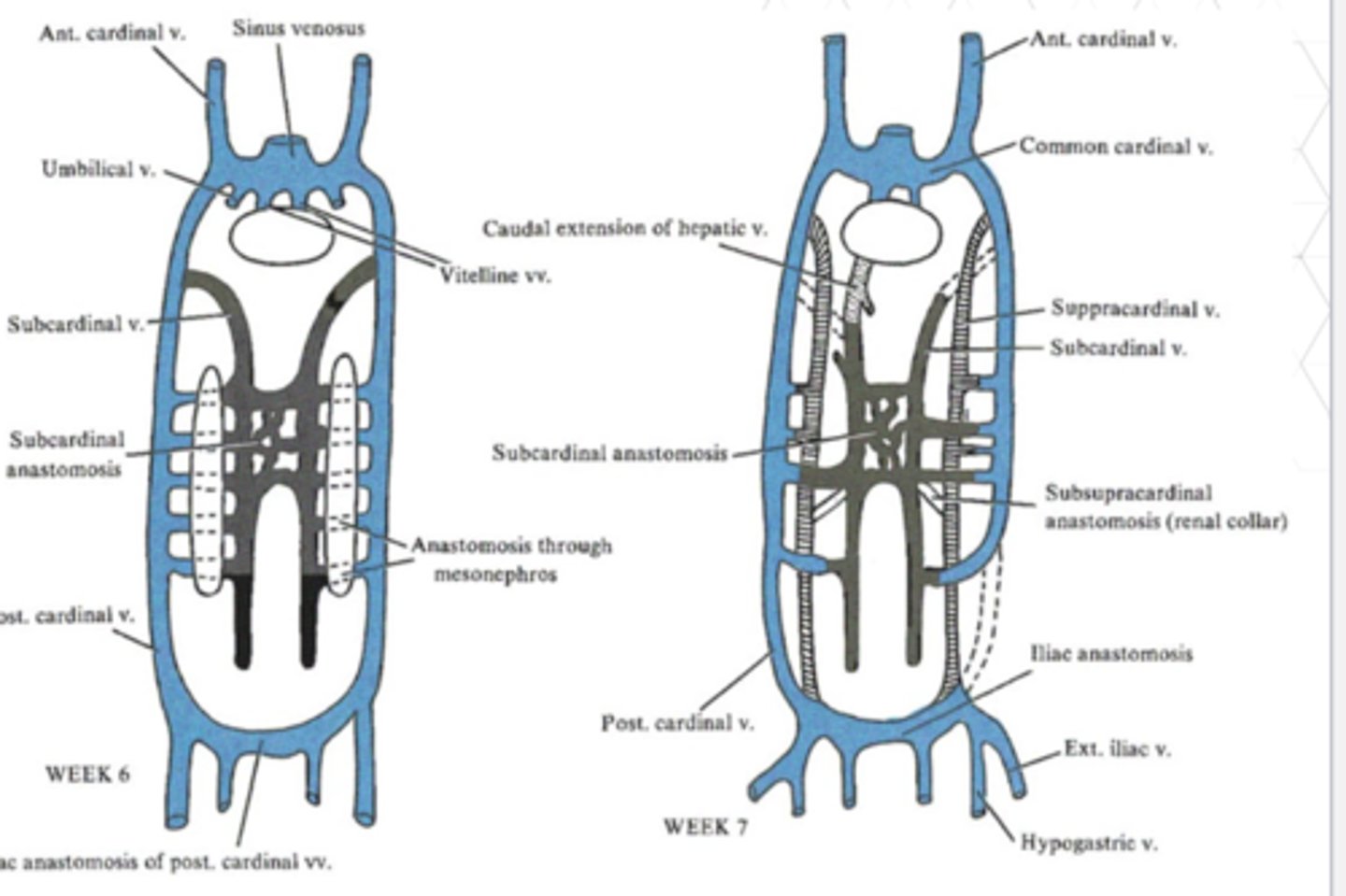
vitelline veins
carry blood, oxygen, and nutrients from the yolk sac to the sinus venosus
umbilical veins
carry oxygenated blood from placenta to fetus
cardinal veins
drain deoxygenated blood from the head and body of the embryo to the sinus venosus
anterior cardinal veins
drain cephalic part of embryo
posterior cardinal veins
drain the rest of the embryo
Which vein forms the portal system?
the vitelline vein
Which veins forms the caval system?
cardinal veins, SVC, IVC, brachiocephalic vein
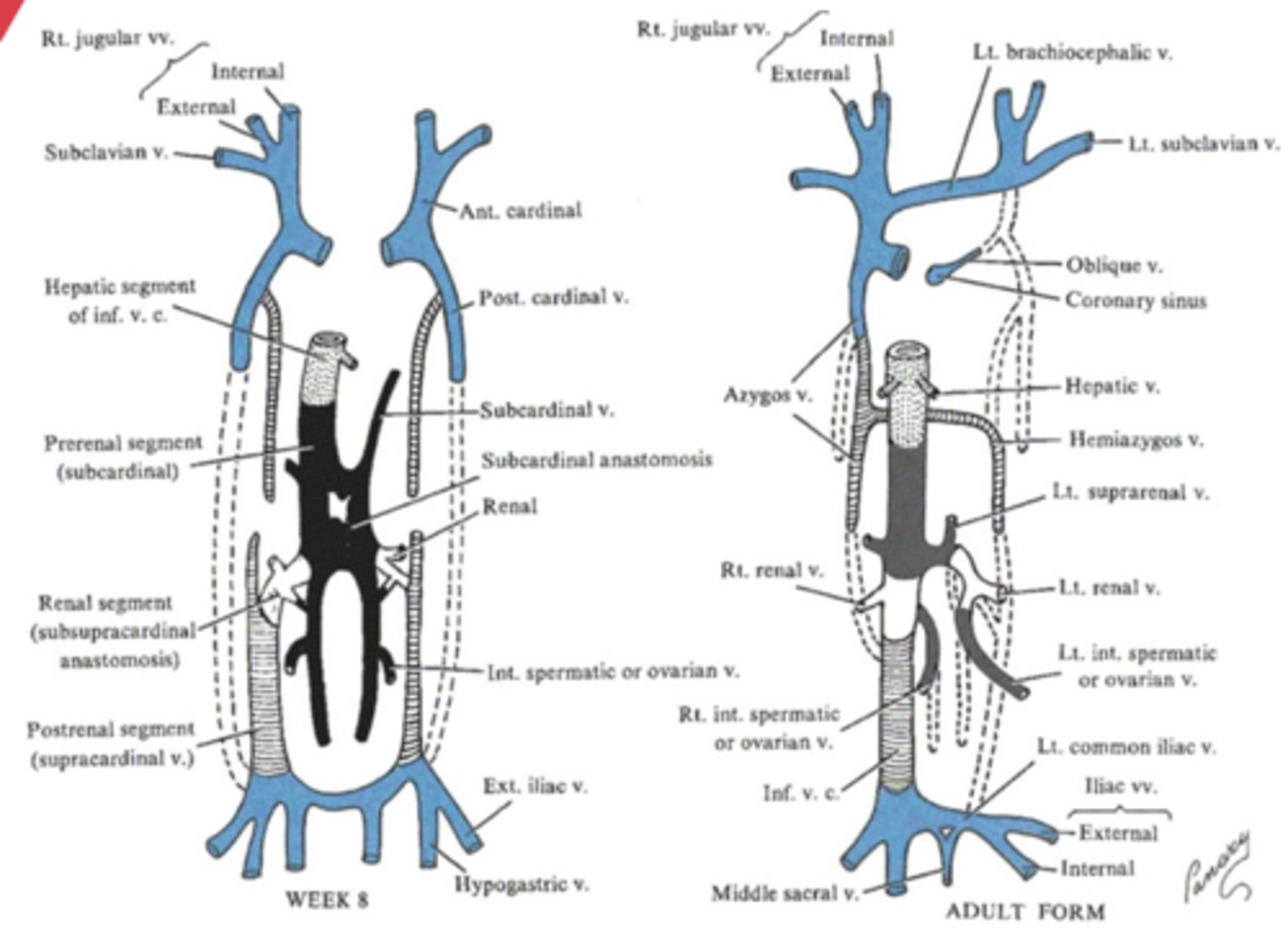
SVC embryologic origin
right anterior cardinal vein
left innominate vein embryologic origin
persistent connection between the anterior cardinal veins after regression of the left cardinal vein
coronary sinus embryologic origin
left common cardinal vein
IVC embryologic origin
right vitelline vein, right hepatocardiac vein, right sub cardinal vein
Hepatic vein embryologic origin
vitelline veins, omphalomesenteric veins
Azygos vein embryologic origin
right supracardinal vein
Hemiazygos vein embryologic origin
left supracardinal vein
Draw the embryologic venous system at Week 6 & 7:
Draw the embryologic venous system at Week 8 & 9:
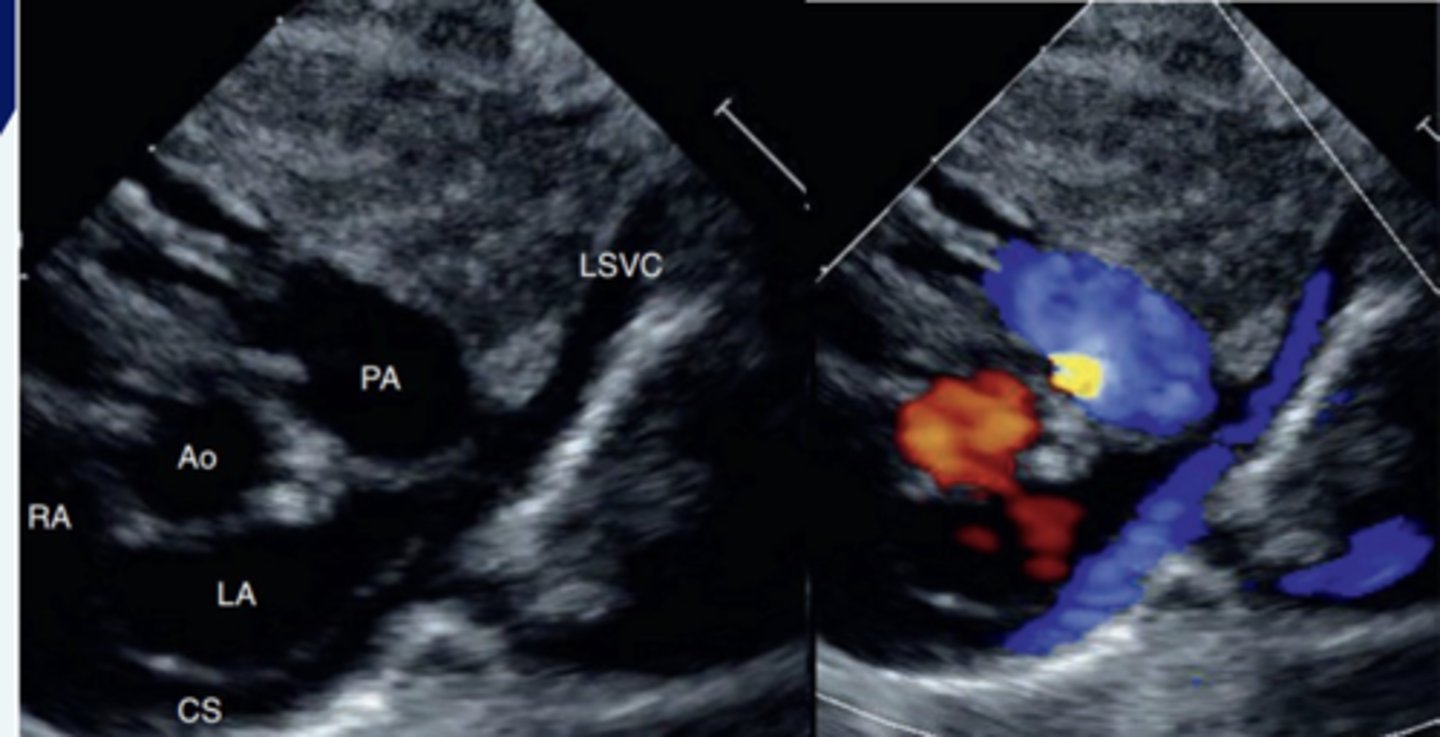
SVC anomalies
- Left SVC to the coronary sinus with normal right SVC (Bilateral SVC's)
- Left SVC to the coronary sinus with atretic (closed) right SVC
- Left SVC to the left atrium
- Levoatrial cardinal vein
How does a left SVC to the CS form?
because there is failure of regression of the left anterior cardinal and left common cardinal veins
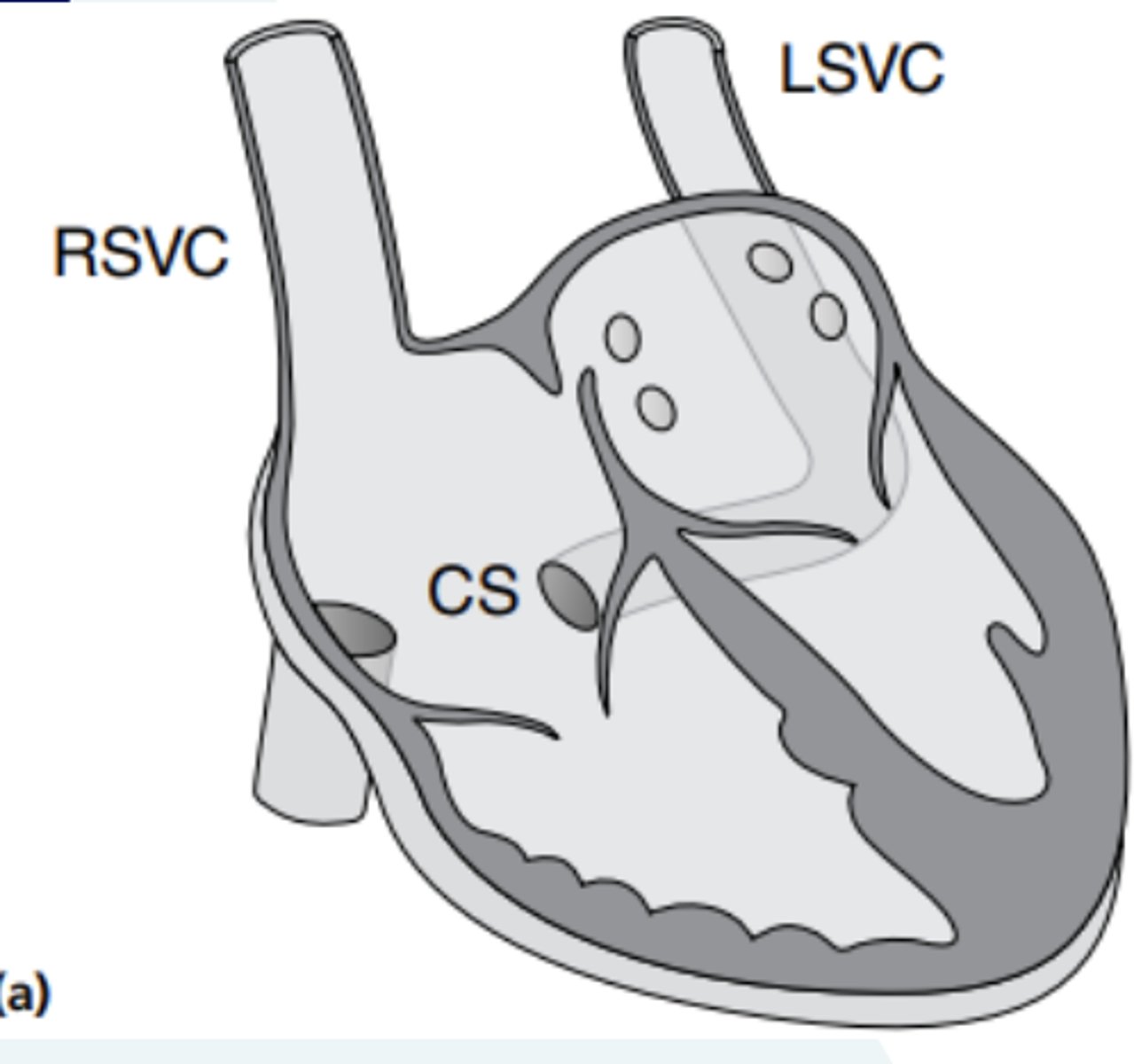
Why is a left SVC to the CS important to be identified?
due to the significant impact on the cannulation approach during cardiopulmonary bypass support if surgical intervention is required (in the setting of CHD)
Where can we view a left SVC to the CS?
in the high left parasagittal view
Ultrasound image of a left SVC to the CS:
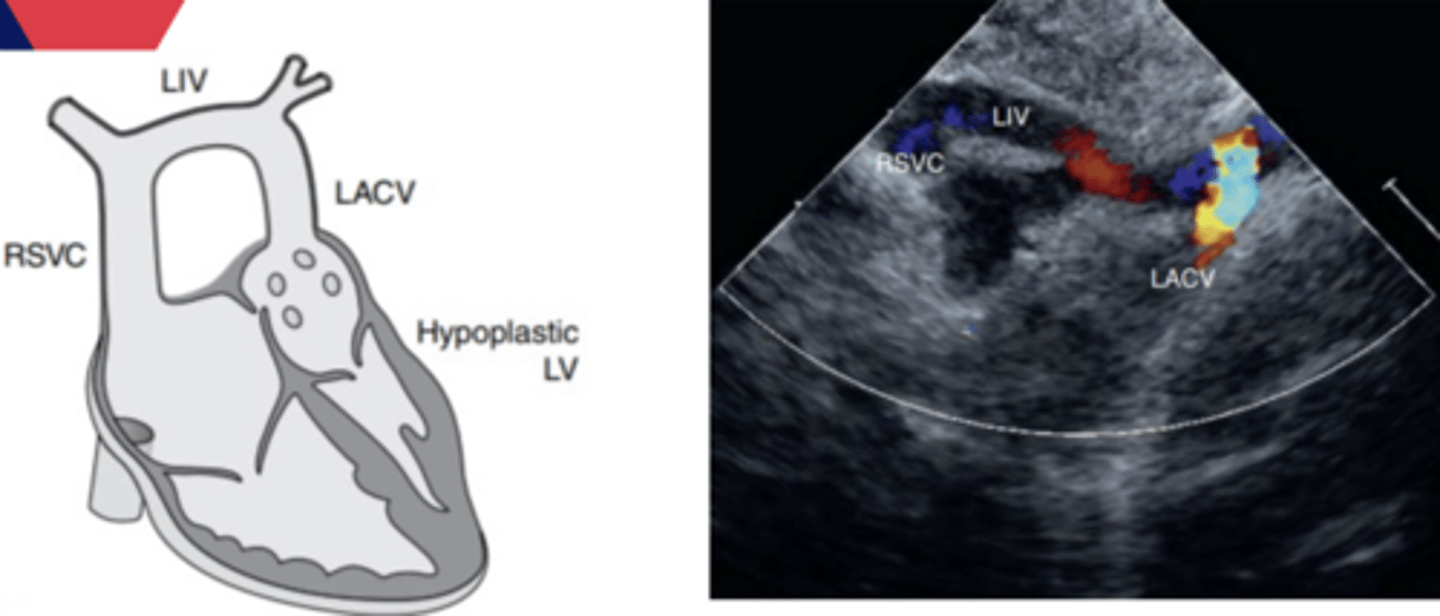
What is a levoatrial cardinal vein?
Embryonic connection between the capillary plexus of the embryonic origin of the pulmonary veins and the cardinal venous system (to dumb it down: it provides a connection between the left atrium or pulmonary veins to the systemic veins such as the innominate vein or superior vena)
Why do we think levoatrial cardinal veins occur?
Thought to occur due to the elevated pressures in patient's who have pulmonary venous obstruction.
Decompresses the pulmonary veins by connecting the LA or PVn to the lower pressure right atrium via the SVC or innominate vein
What view is a levoatrial cardinal vein obtained?
Visualized in the suprasternal SAX view
Image of a levoatrial cardinal vein:
Inferior Vena Cava Anomalies
Interrupted IVC with azygos/hemiazygos continuation
Bilateral IVC (duplicate IVC)
Left IVC to Right Atrium
Right IVC to Left Atrium
What is an interrupted IVC withazygos/hemiazygos continuation?
IVC forms from the iliac veins, stops, then blood finds a way to the RA through the azygos/hemazygos vein
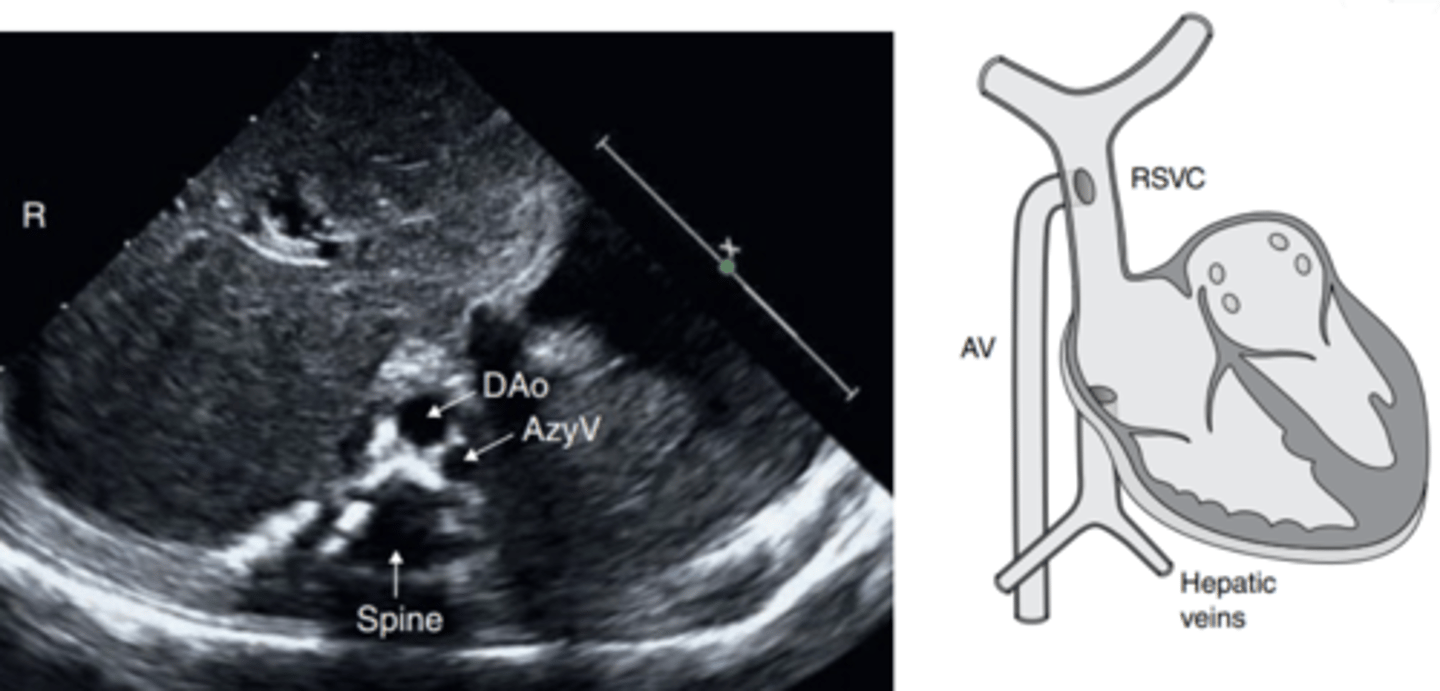
What type of patients is interrupted IVC withazygos/hemiazygos continuation most common in?
patients with Heterotaxy syndrome
What causes an interrupted IVC withazygos/hemiazygos continuation?
Due to failure of the right subcardinal vein to connect to the right vitelline and right hepatocardiac veins (absence of hepatic segment of the IVC)
In what view can we obtain an interrupted IVC withazygos/hemiazygos continuation?
Subcostal SAX and LAX with a posterior angle will demonstrate the hepatic veins draining into the RA without a connection to the IVC
Is a bilateral (duplicate) IVC rare?
yes
What causes a bilateral (duplicate) IVC?
persistence of both supracardinal veins
What type of patient is most common to have bilateral (duplicate) IVC?
Heterotaxy syndrome, but also with normal Abdominal Situs
Types of bilateral (duplicate) IVC's & confluences:
