Lecture 6: Health Inequalities
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
30 Terms
health (WHO definition)
-a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity
biopsychosocial model of health
-brings together three areas that contribute to health:
biomedical → genetics, viruses, bacteria
psychological → beliefs, behaviour, stress
social → status, ethnicity, friendship groups
-recognises that these elements interact and impact on our health
-the person and the context in which they live is taken into account as well as the influence of biology
life expectancy variation
-Japan is highest → 84.3 years
-Lesotho is lowest → 50.7 years
social determinants of health
-circumstances in which people are born, grow up, live, work and age
-the systems put in place to deal with illness
-shaped by economics, social policies and politics
equality
-everyone gets the same resources
equity
-everyone gets the same outcomes, with resources distributed according to need
equal outcomes
-achieved through the removal of structural barriers
covid inequalities
-found factors other than underlying health status might mean you are more likely to get seriously ill from coronavirus:
age
being a man
living in poorer areas
BAME
being born outside UK or Ireland
living in a care home or having certain jobs
HPV
-human papillomavirus
-sexual transmitted infection
-more than 200 types
low risk types → cause genital warts
high risk types → cause cervical and other cancers
impact of HPV on health
-genital warts
-implicated in 5% of all cancers
-incidence of head and neck cancers is attributable to HPV 16/18 is five-fold higher in men
-90% of anal cancers
-cervical cancer
90-70-90 targets (WHO)
-defines cervical cancer elimination as <4 cases per 100,000 women and has set 90-70-90 targets for countries to reach
vaccination against HPV which is responsible for 90% of cervical cancers
70% of women have cervical cancer screening which aims to detect and treat pre-cancerous cells before they develop into cancer
treatment for cancerous cells for 90% of women
cervical screening in Uganda
-not routinely offered but is available through obstetric and HIV clinics
-main approach used is visual inspection with VIA, treated with cryotherapy at the same appointment
-major barrier is access in remote or rural areas
-screening rate is between 5-30% and most women are diagnosed with advanced disease
Black - barriers to cervical screening
-embarrassment, fear of procedure or outcome
-residing in a remote or rural area
-limited resources/health infrastructure
-most frequent facilitator was having a recommendation to attend screening
cervical screening in UK
-saves >2000 lives per year
-HPV primary screening:
replaces cytology-based screening
sample tested for HPV, if positive then sent to cytology
opportunity for self-testing
dimensions of inequity
-ethnicity socioeconomic status, sexual minorities, age, sexual trauma, disability
-less likely to attend cervical screening
-at risk of worse adverse emotional responses to testing positive
-colposcopy attendance → more likely when older and wealthier
disability and health inequality
-women with disabilities often have difficulty with physical access to health services
-at risk of delayed diagnosis and cancer mortality, partly due to lower screening
medical model of disability
-problem is the disabled person
-medically focussed on condition/symptoms and person
social model of disability
-problem is the disabling world, rather than the person’s condition
-oppression and exclusion people with impairments face is caused by the way society is run and organised
-key disabling barriers:
attitudinal barriers
physical barriers
information/communication barriers
Edwards (cervical screening and physical disability)
-systematic review of barriers and facilitators to cancer care
only 5 studies between 1997 and 2015 explores cervical screening for physically disabled women
all reported a decrease in screening attendance associated with disability
Chan (cervical screening and physical disability)
-systematic review of factors influencing screening uptake
lack of knowledge of cervical cancer screening and how it can be accessed
difficulties and inconveniences in accessing cancer screening providers and undergoing the screening procedures
uncomfortable experiences during the screening procedures
UK report 2019 (cervical screening and physical disability)
-88% said it is harder for disabled women to attend or access cervical screening
-63% had been unable to undergo cervical screening because of their condition
-49% had chosen not to attend cervical screening for reasons such as previous bad experiences related to their disability
-20% reported they were assumed not to be sexually active
Sherman - method (cervical screening and physical disability)
-cross-sectional online survey
-eligible for cervical screening
-identified as having a physical disability, condition, impairment or difference
-rated statements developed with patient and public involvement stakeholders:
included screening-related problems and solutions, questions about self sampling and preferences for future screening
Sherman - results (cervical screening and physical disability)
Problem | % endorsed Sherman et al 2024 | % endorsed Waller et al 2009 |
I worry that a cervical screening test will be painful | 83 | 14 |
Cervical screening tests are embarrassing | 70 | 28 |
I’m scared of what a cervical screening test might find | 69 | 12 |
The examination table is uncomfortable | 66 | N/A |
I’ve had a bad experience of cervical screening in the past | 63 | 9 |
Having to lie on my back with my legs apart is a problem | 61 | N/A |
I worry about having a male doctor or nurse do the test | 60 | N/A |
I intend to go when I’m due, but don’t always get round to it | 52 | 21 |
Doctors and nurses lack understanding of disability | 46 | N/A |
It is difficult to get an appointment to fit in with work/childcare commitments | 46 | 7 |
-Waller looked at non-disabled women
-Sherman looked at disabled women
-shows disabled people have the same issues but these are highly exacerbated in a disabled community
Sherman - endorsed facilitators (cervical screening and physical disability)
Solution | % endorsed |
A doctor or nurse who discusses my specific needs | 86 |
A doctor or nurse who is willing to try different solutions | 85 |
A doctor or nurse who understands my physical disability | 82 |
A smaller speculum | 80 |
A cervical screening passport | 74 |
Being invited by email or text | 69 |
An examination couch that can be lowered | 69 |
Having a conversation with the doctor or nurse before the appointment | 69 |
Being offered medication that prevents muscle cramps and spasms (antispasmodic) | 62 |
Being offered the left lateral position for the screening test | 55 |
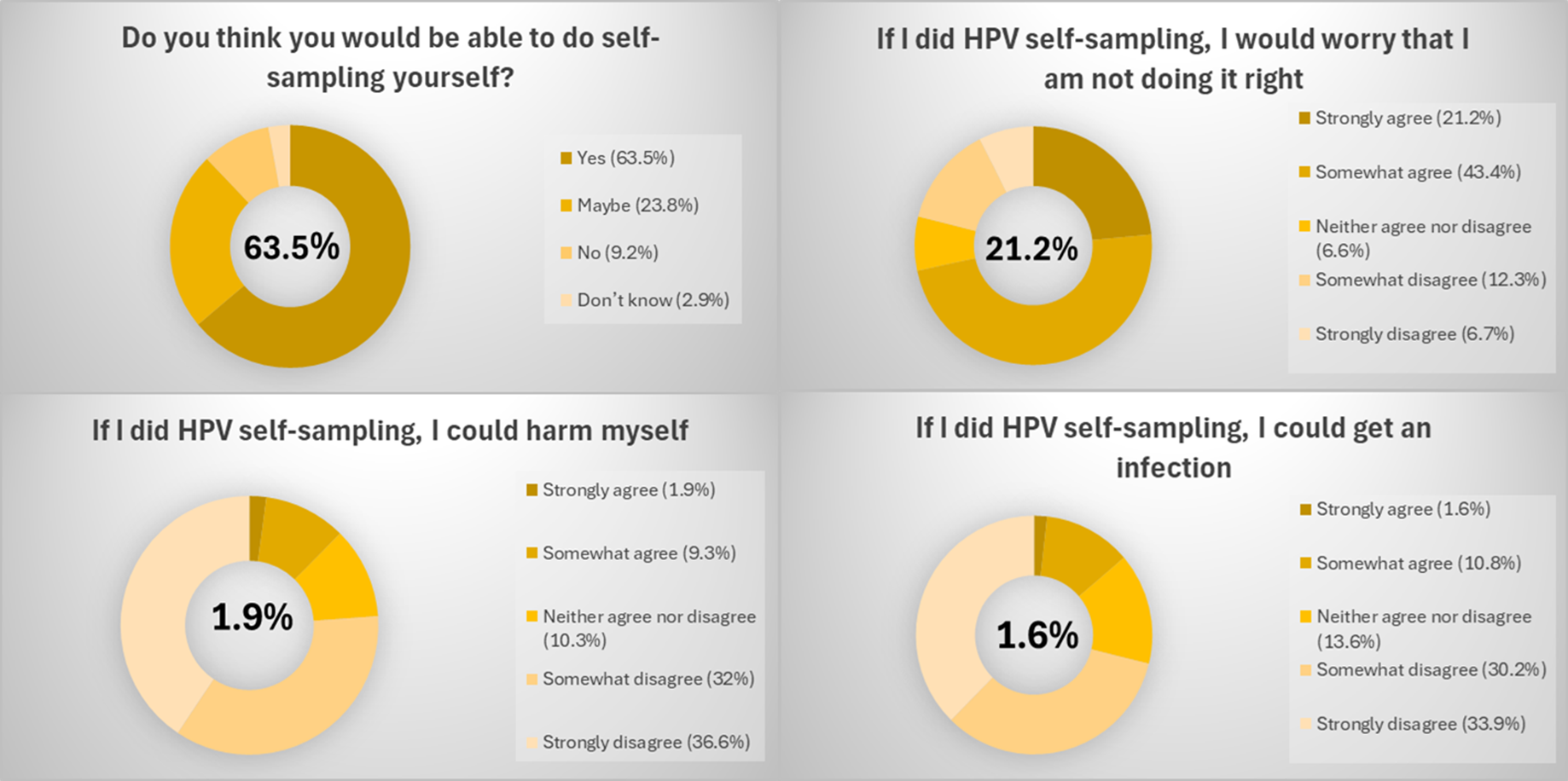
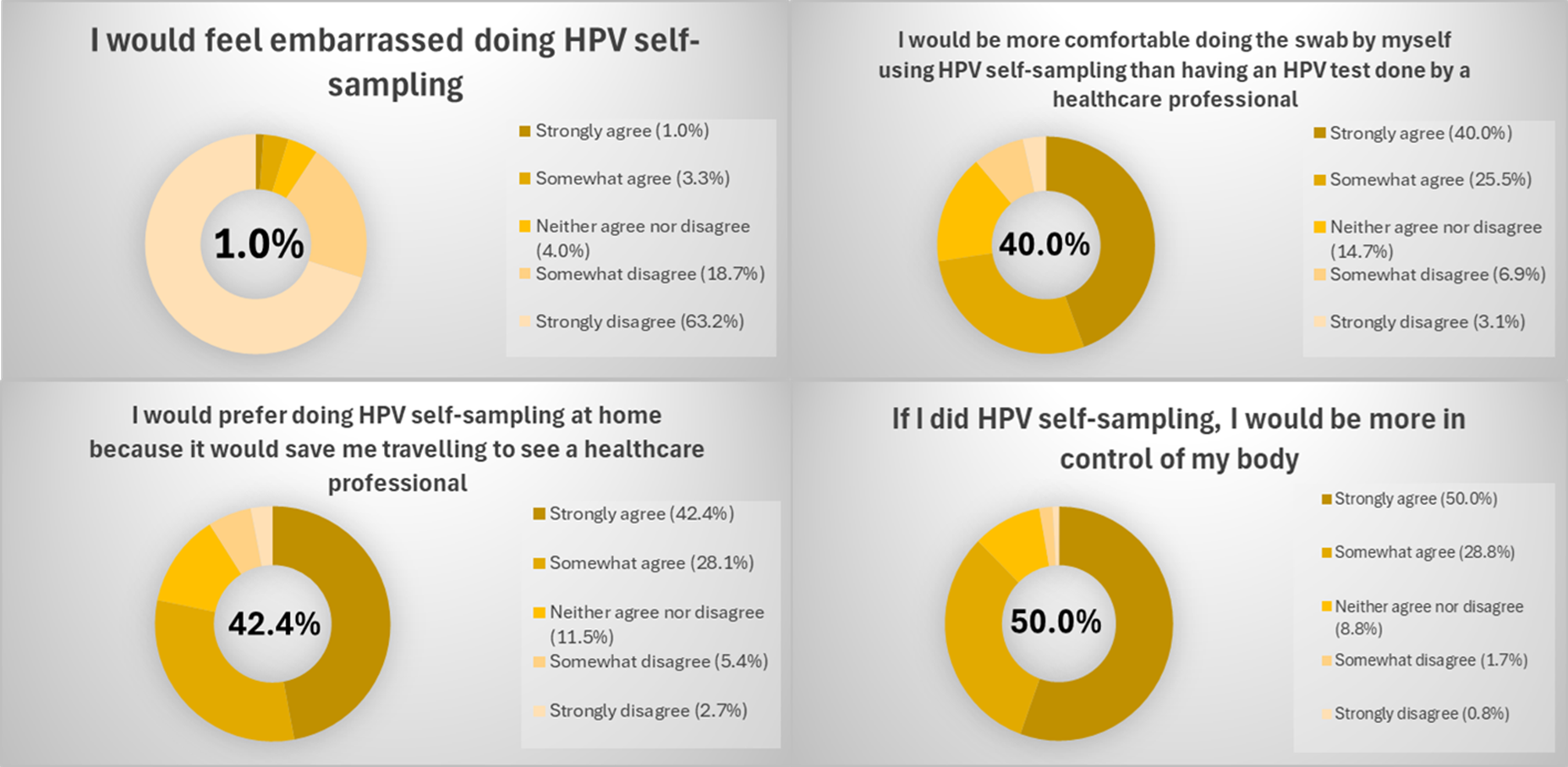
self sampling results (self-screening and disability)
HPV vaccination in UK
-school based vaccination programme introduced for girls aged 12-13
-boys later added to programme
-has led to 88% reduction in CIN grade 2 or worse in young women
-a substantial reduction in cervical cancer and incidence of CIN3
HPVC and men
-vaccinating boys:
protects female partners
protects themselves
-incidence of anal cancer is similar to estimated rate of cervical cancer without a screening programme
head and neck cancer
-risk factors:
excessive alcohol consumption
smoking
HPV
-does not include brain
oropharyngeal cancers
-rising incidence
-in UK + USA, incidence of HPV oropharyngeal cancer in men has surpassed that of cervical cancer in women
social ecological model (screening and vaccination)
-inner to outer circle:
individual → knowledge, attitudes, behaviours
interpersonal → perceived norms among family/friends
community → cultural values, religion, public transport
health systems → screening accessibility, school-based vaccination, cultural safety
politics → national or regional screening + vaccination policies