Contouring and Localization
1/28
Earn XP
Description and Tags
ONCOL 355 - Planning and Dosimetry I. University of Alberta
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
29 Terms
External Countour
Outline of the patient’s skin surface usually done through the transverse plane
Internal Contour
Outline of the body's internal structures, depicting organ shapes and relationships, through the transverse plane
three reasons contours are made
Patient shape and size
depths from surface to isocenter
Location of Organs
amount of organs in the radiation path to calculate dose to these organs
we need to have a visual of what the radiaiton beam is travelling through
Set-up data for the radiation therapists
Contours needed to assist radiation therapists in setting up the patient
Depths important for the planner, helps with MU calculations
why do we need critical organs countoured?
they are radiosensitive and dose limiting
this limits the amount of dose we can give to the tumor
Serial Structures
Structures that when damage to the organ occurs in one spot, the organ completely loses function
example: spinal cord
have max dose that can be applied (4500-5000 cGy)
Parallel Structures
structures that hen damage to the organ occurs in one spot, funcitonal impairment in that spot occurs, but the rest of the organ can keep working
example: lung and kidney
we need to know how much of that structure gets dose, is a volume relationship
how much of the lung is getting 3000 cGy
4 old methods of external contouring
Simulator
Bendable Wire
Plaster of Paris Bandages
Immobilization Shell
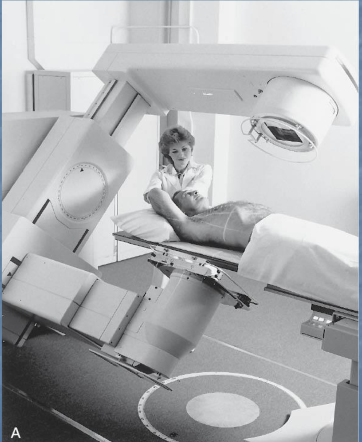
Simulator
Simulator looks like a treatment machine
Rotates around patient's isocenter 10 degrees and read the ODI's of patient surface, then can extract an external countour
Bendable wire
Put wire on patient and get crude contour, apply to digitizer
Plaster of Paris Bandages
Bandages used to create external contours by wrapping them around the patient's body, hardening to form a rigid shape for treatment planning and localization.
Immobilization Shell
a shell which reflects a patient’s shape is used and a contour is traced from inside the shell.
a jig with a pointer attached to a pencil traces the shape and applies it to paper
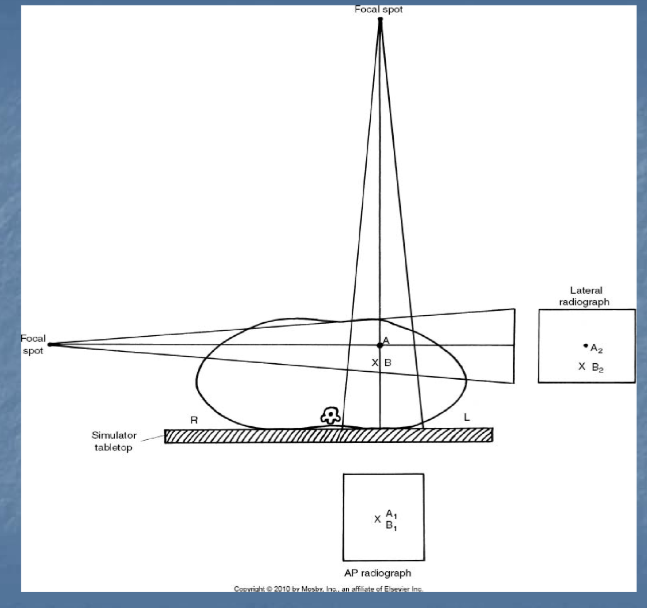
how are internal contours created alongside the 4 outdated methods of external contouring?
orthogonal x-rays images
A/P and lateral images to gain A/P, Sup/Inf and lateral information
disadvantage of 2D contouring
only reflect’s patient’s contour at one point, there is a change in organ shape within each slice that can’t be see without a CT
what machine is now used for both internal and external contour
CT images
multiple planes: 2D transverse, saggital, and coronal images are used to give a 3D view of the body/tumor
we now get multiple slices in each plane
3D CT countours give information about …
the size and shape of the patient, internal structures, and the tumor
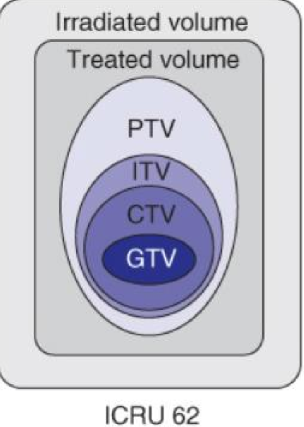
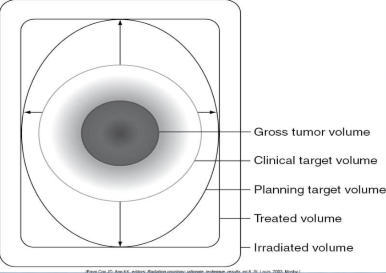
GTV
Gross Tumor Volume
visable extent of the tumor, easy to put contour line around
CTV
Clinical Target Volume
accounts for microscopic cells of the tumor, puts extra room around GTV
ITV
an additional margin (internal margin) placed to account for motion of the patient
can only do this if we have 4D CT information
Formula for ITV
ITV = CTV + IM
SM
Set-up margin
additional contour placed as a geometrical concept as patient set-up on bed will always have discrepencies
placed on top of the CTV or ITV

PTV
Planning Target Volume
is the volume that includes the ITV plus the setup margin (SM) to ensure that the prescribed dose is delivered to the CTV despite variations in patient positioning and internal motion.
PTV formula
PTV = CTV (or ITV) + SM

TV
Treated Volume
high dose region that is treated when all the beams are on, what is prescribed by the RO
IRV
total treated volume account for all areas where beams enter or exit
ITV accounts for _____, PTV accounts for _____
motion, set-up discrepancies
describe the orders of the volumes as they are created
GTV —> CTV —> ITV —> PTV
OAR
Organ at risk
normal tissues whose radiation sensitivity may significantly influence treatment planning and/or prescribed dose
PRV
Planning risk volume
additional margin around the OAR may be recommended to account for organ motion and set-up uncertainties
helps ensure sparing of OAR
PRV formula
OAR + Internal/set-up margin = PRV