Ch 38: Regulation of ECF Composition & Volume
1/25
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
26 Terms
What transporter in the ALOH is on the apical side and is responsible for solute reabsorption?
The Na/2Cl/K transporter allows for the reabsorption of those ions.
What is reabsorbed in the early distal tubule?
chloride and sodium ions
Is the early DCT permeable to water?
No, the DCT is impermeable to water.
What hormone alters the permeability of the late DCT and collecting duct?
ADH can increase the permeability of the late DCT and collecting duct to water by increasing aquaporin number.
What is the role of principial cells in the collecting tubules?
These cells secrete potassium into the filtrate and absorb sodium and chloride ions into the interstitial fluid.
aldosterone increases the activity of the Na/K ATPase, increasing K+ secretion and Na+ retention.
Where does the majority of sodium reabsorption occur?
~65% occurs in the proximal convoluted tubule
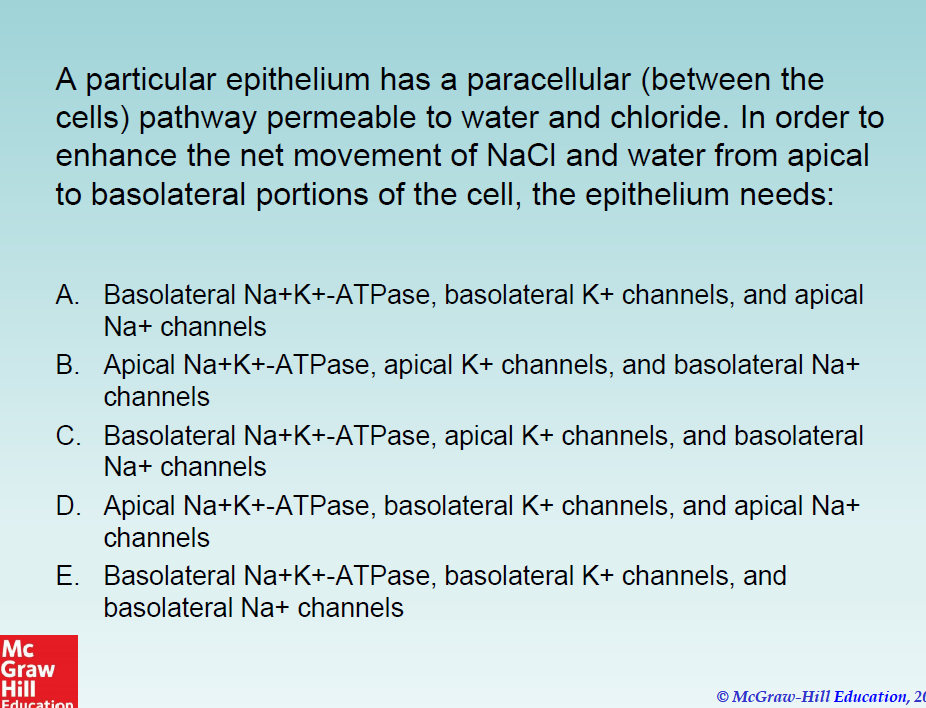
What is the answer to this question?
A is the correct answer.
Na/K ATP-ases on the basolateral side would allow Na to be removed from the cell, K+ channels on the same side would maintain the K+ gradient needed to remove more sodium.
Sodium channels on the apical side will allow sodium to be absorbed from the filtrate down the concentration gradient established by the Na/K pump.
What is the feedback mechanism for osmolarity regulation that is controlled by ADH release?
Osmolarity increases are detected by hypothalamus
ADH is released
The DCT and collecting duct have increased H2O permeability
More water is reabsorbed, diluting interstitial fluid
Less water is secreted
overall osmolarity of the blood is reduced.
What factors increase ADH secretion?
decreased ECF volume (hypovolemia)
nausea/vomiting (fluid loss)
standing
Angiotensin II (increased retention of sodium, increased retention of water)
What is the effect of angiotensin II on renal tubules?
Angiotensin II increases sodium reabsorption
What mechanisms does Angiotensin II utilize to increase blood volume?
stimulation of aldosterone secretion
Direct increase of sodium reabsorption
What factors increase aldosterone secretion?
increased angiotensin II
Increased K+ levels
aldosterone results in secreted K+
ACTH (permissive relationship)
What factors decrease aldosterone secretion?
ANP (atrial natriuretic peptide)
increased sodium concentration
enough Na in blood
What effect does ANP have on the body?
inhibits Na+ reabsorption, increasing water excretion
inhibits the release of renin and aldosterone
increases GFR
What stimuli trigger release of ANP?
ANP is released from the atria of the heart in response to stretching (increased blood volume)
What is BNP?
B-type natriuertic peptide
What stimulates secretion of BNP?
stretching of ventricular walls, perhaps due to increased ventricular volume or pressure.
What are the affects of BNP?
vasodilation
promotion of Na/H2O secretion in the kidneys
inhibition of ANG II and aldosterone
What do high levels of BNP indicate?
high BNP levels are indicative of cardiac dysfunction
What produces CNP?
CNP is produced by endothelial cells lining blood vessels
What is the function of CNP?
CNP acts locally to regulate vascular tone and flow
What is the risk of high levels of CNP?
elevated CNP levels are associated with high risk of MI
A patient is found collapsed. His body temperature is 40 Celsius, his skin and mucus membranes are dry, and his blood pressure is low. Which of the following lab results would you expect to find?
elevated aldosterone
decreased renin level
elevated urine Na+ concentration
decreased ADH level
low urine osmolarity
The correct answer is A. His body would be trying to retain as much fluid as possible, which would result in increased aldosterone levels. Aldosterone retains sodium, which in turn retains water.
Where is erythrooietin produced?
In fibroblasts located near the PCT and peritubular capillaries. produced in response to low blood oxygen.
What is the target of EPO?
bone marrow to increase hematopoiesis
What is required for the production of pro-erythroblasts?
iron stimulates the maturation of CFU-E cells into pro-erythroblasts.