audiology exam
1/77
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
78 Terms
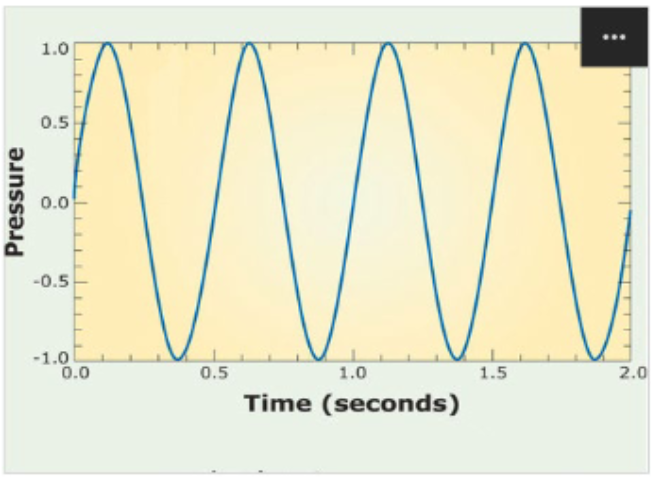
Frequency
Number of cycles (Hz) per second
Wavelength
Distance
Period
time
Amplitude
pressure
intensity
A measurement of sound energy, related to the
amplitude of the wave and the perception of loudness
db
dB SPL
Decibels Sound Pressure Level
Typically used to characterize noise levels in an
environment
• Measuring level of loud noise in a factory
• Ambient sound level in quiet spaces
dB HL
Decibels Hearing Level
Measurement scale used by audiologists to
describe hearing thresholds
dB SL
Decibels Sensation Level
Measurement scale used by audiologists
to equate audibility across patients
• Based on the
individual’s hearing threshold
Useful for testing speech recognition
10 ABOVE threshold
ranges of hearing
Normal: -10 to 15 dB HL
Slight: 16 to 25 dB HL
Mild: 26 to 40 dB HL
Moderate: 41 to 55 dB HL
Moderately Severe: 56 to 70 dB
Severe: 71 to 90 dB HL
Profound: 90+ dB HL
degree
Normal, mild, moderate, moderately-severe, severe, profound
configuration
Flat, sloping, rising, notched
type
Sensorineural, conductive, mixed
SRT
speech Recognition Threshold
• Measure of the softest word that the patient can
correctly repeat about half the time
• Use “spondee” words, two-syllables with equal
stress
• Examples: Baseball, hotdog, airplane, toothbrush
SRT agreement
“Good agreement” = PTA and SRT are within +/- 6 dB
• “Fair agreement” = PTA - SRT difference is > 6 and < 12 dB
• “Poor agreement” = ≥12 dB difference
WRS
A measure of speech recognition at a
comfortable and audible intensity level
40db SPL above SRT
Pure-Tone Average
PTA average of hearing thresholds at 500 Hz,
1000 Hz, 2000 Hz
• Add hearing thresholds at these frequencies and then dividing by 3
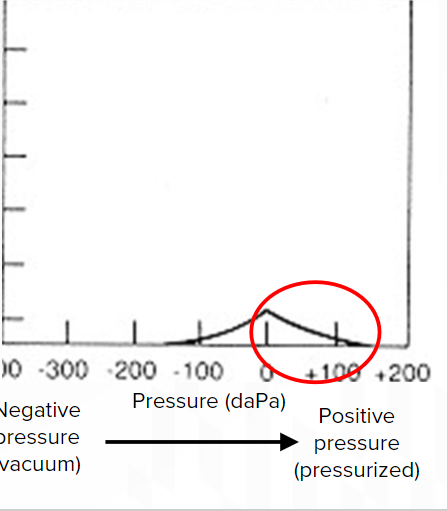
type A
observed in an individual with normal middle
ear pressure
normal hearing ,sensorineural hearing loss

Type B
patient with middle ear fluid
conductive hearing loss,big airbone gaps
Type C
patient with an obstructed Eustachian
tube
negative pressure and small conductive hearing loss
Type As
short compliance seen in patients with otosclerosis
middle ear is not conducting sound well
Otoacoustic emissions (OAEs)
measure the movement of Outer hair cells
OAEs are generated by the movement of fluid in the cochlea, creating a traveling wave that travels back through the ME and ear canal
OAEs will be absent
in patients with conductive hearing loss,
moderate sensorineural hearing loss, or hearing loss greater than moderate will have absent OAE’s (no response) or no outer hair cells
OAEs are measured within a frequency range of 1000 Hz to 4000 Hz.
If a patient has present OAEs but absent ABR
they may have an acoustic neruoma
auditory brainstem response
measures the path of electrical potentials
from the cochlea to the cortex, like an EEG
The normal latency for wave V in an ABR test is approximately 5 ms
x=time y=electrical impulses
detection brainstem tumors-are able to compare good ear to bad ear
Hearing aids
Hearing aids amplify sounds at a specific increment at specific frequencies
List three styles of hearing aids
a. In the ear (ITE)
b. Behind the ear (BTE)
c. Completely in the canal (CIC)
What do CROS hearing aids do?
Sound from the bad ear is sent through a
microphone and travels to the good ear via receiver.
hearing level technology
basic vs advanced
advanced -more features
hearing aid selection
a. Manual dexterity issues
b. Need for amplification
c. Cost considerations
d. Need for discretion
e. Bluetooth connectivity
manual controls
Bluetooth, volume, switch b/w programs
battery
powers hearing aid
amplifier
amplifies sound signals
microphone
picks up sound
sound transmission within a hearing aid
sound enters microphone ---> sounds amplified by amplifier ---> sent to receiver ---> sounds delivered to ear
receiver
sends sound to ear
hearing aid fitting and verification
Enter patients audiogram into the hearing aid software --> program HA settings/programs --> conduct real ear measurements to verify amplification --> adjust based on patient feedback
Real Ear Aided Response (R E A R)
The output of the hearing aid while it’s on the patient’s ear
Real – Ear - Measurement
Measuring the output of a hearing aid while the patient is wearing it
Unaided Response (R E U R)
The patient’s natural ear canal resonance
Insertion Gain (R E I G)
The amount of gain provided by the hearing aid
Private practice
independently owned small business
What types of patients can be treated in private practice
Patients with sensorineural hearing loss
What financial considerations are associated with starting and managing a private practice
a. Equipment costs / maintenance
b. Rent/utilities
c. Employee salaries/benefits
d. Office supplies
e. Marketing expenses
hearing aid orientation
a. Proper insertion/removal
b. Battery handling/charging
c. Volume/program controls (speech mode, restaurant mode, music,
etc.)
d. Cleaning and maintenance
e. Common troubleshooting (check battery, remove wax, ensure
properly inserted)
f. When to wear / not wear them
Don't wear hearing aids
1. While sleeping
2. In the shower or swimming
3. During excessive sweating
KEEP AWAY FROM PETS
hearing aid troubleshooting
Check if battery is dead
• Inspect for wax blockage
• Verify correct insertion
• Use a hearing aid stethoscope to listen to sound output
• Reprogram device
utricle
detects movement in the horizontal plane
saccule
detects movement in the vertical plane
semicircular canals
filled with endolymph
8. Fluid in the semicircular canals will flow through the ampulla at the base of
the canal, deflecting the hair cells and sending a signal to the brain that the
head is in motion.
9. The semicircular canals are aligned with the muscles of the eye muscles
canals
anterior (superior) canal detects movement in the sagittal plane (nodding yes)
Lateral (horizontal) canal detects movement in the transverse plane (shaking no)
Posterior (inferior) canal detects movement in the coronal plane (tilting side to side)
videonystagmography (VNG)
Patient wears VNG goggles with cameras inside to monitor eye movement
• The computer tracks the position of the pupils throughout testing
• Nystagmus looks like a saw-tooth pattern on the VNG tracing
Rotary Chair and Velocity Step Test
measures the vestibular response to different head movements -bilateral horizontal semicircular canals
caloric irrigations
1. introduce warm/cool air or water into the ear canal to stimulate the
lateral semicircular canals
2. endolymph heats or cools
3. deflects hair cell stereocilia in the ampulla
4. activates the hair cells
5. Sends signal to brain = feeling of spinning
provides ear- specific results, allowing each ear to be tested independently and compared for vestibular function assessment.
cochlear implant
A cochlear implant replaces the cochlea by directly stimulating the auditory nerve via
electrical impulse
what four parts make up the cochlear implant
a. 1. Sound processor / Microphone
b. 2. Transmitting coil
c. 3. Internal receiver
d. 4. Electrode array
tonotopic organization
aspect of cochlear physiology that a cochlear implant relys on to facilitate speech perception
Where each place of the basilar membrane is specifically tuned to a different frequency based on stiffness and mass
CI candidacy in adults
a. 1. Adults aged 18+
b. 2. Moderate to profound SNHL
c. 3. Limited benefit from amplification; <50% speech recognition (w/ hearing aids)
d. 4. Speech material used: Sentences or word tests
CI candidacy in children
a. 1. Children aged 2-17 y/o
b. 2. Severe to profound SNHL
c. 3. Limited benefit from amplification; <30% speech recognition (w/ hearing aids)
d. 4. Speech material must be age-appropriate
CI candidacy in infants/toddlers
a. 1. Infants/toddlers aged 9-24 months, earlier if cochlea may become ossified
b. 2. Profound SNHL, both ears
c. 3. Limited benefit from amplification (case dependent)
d. 4. Limited opportunity for speech-based testing
T-Level
the lowest current level required for a cochlear implant patient to perceive sound
M-Level
refers to the current level required for a cochlear implant patient to perceive a loud, but comfortable sound
list medical indicators/red flags for a medical referral
1. Sudden hearing loss
4. Ear pain/drainage
2. Sudden onset of tinnitus
5. Asymmetric hearing loss
3. New conductive HL
presentation of acoustic neuroma
Auditory/Vestib portion of the 8th CN
ABR diagnostic test that is most sensative
noncancerous
tinnitus, hearing loss, dizziness
(presses on 8th nerve)
Abnormal ABR on affected, normal ABR on unaffected
otosclerosis
Abnormal bone growth on the stapes
Type As tympanogram
carhart notch
1-3-6 rule
By 1 month: Infants should be screened for hearing loss by 1 mo.
By 3 months: Infants that failed screening should have a diagnosis evaluation by 3 mos.
By 6 months: Infants with a hearing loss dx are enrolled in early intervention
diagnostic tests that are most appropriate for diagnosing congenital hearing loss
otoscopy,tympanometry,OAE,contioned play ,visual reinforment
visual reinforcement audiometry
a. Patient age range: 6-24 mos. old
b. Briefly, how is the test performed? Audiologist plays a loud sound, and the infant will look toward the sound.
i. Once they look toward the sound, a toy will light up and dance/move to confirm that they heard the sound.
ii. The audiologist/parent will divert their attention back to the center (E.g.,toys on a table), and repeat until the child continues to turn their head
when they hear sound.
iii. Audiologists will play sound softer until they find the threshold.(Hughson-Westlake method)
conditioned play audiometry
c. Patient age range: 2-5 yo
d. Briefly, how is the test performed? Discuss with the child that if they hear a beep
in their headphones, perform an act (E.g., When you hear a beep... Put a ball in
the bucket. Stack a block on the tower. Put a ring on the peg.)
i. The audiologist will play a sound and demonstrate the game
ii. The assistant to the audiologist will instruct the child to wait and listen until they hear a beep
iii. Repeat until the child learns the rules
iv. Find the child’s thresholds
how to confirm that hearing devices are working properly?
Picture pointing & Ling-6 sounds
Ling -6 sounds
A broad range of speech sounds that can be imitated by children
i.m iv. ah
ii. oo v. sh
iii. ee vi. s
picture pointing
Speech recognition can be
assessed through picture pointing
• Speech reception threshold
• Word recognition score
nystagmus
The involuntary rhythmic movement of the eyes
fast nystagmus= more dizzy
slow nystagmus=less dizzy
vertigo
false sensation of spinning
Hughson-Westlake method of testing
Start where the patient may hear (50-70 dB) and proceed to play sound. If they respond,
decrease by 10 dB. No response, increase by 5. Repeat process after 2 out of 3 times until you fill
the audiogram at different frequencies.
“Up 5, down 10”
Symbols
1. Air conduction:
Right ear: O Left ear: X
2. Bone conduction:
Right ear: < Left ear: >
Electromotility
OHC stimulation pulls the basilar membrane closer to the tectorial membrane, causing shearing and allows for amplification of sound (Electro)
Mechanotransduction
Where IHC movement sends electrical impulses that send sound
waves to the auditory nerve in the brain... allows for sound recognition
Solve wavelength
What is the period? 1/freq = 0.5 sec
What is the frequency? 2 Hz
What is the amplitude? 1