Chapter 7: Blood Calcium Levels, PTH and Vitamin D, Bones Fracture and Repiar, etc
1/13
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
14 Terms
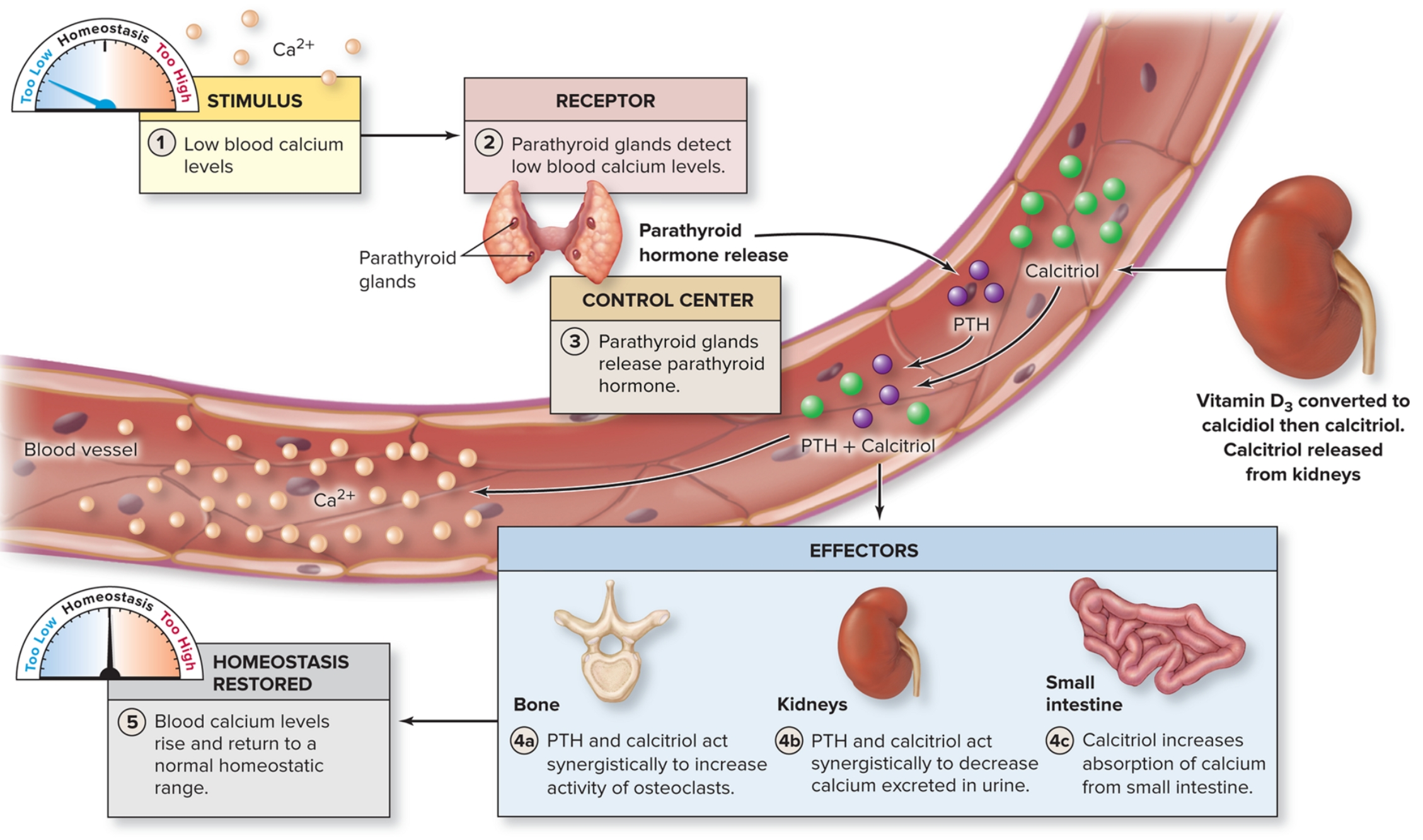
Regulating blood calcium levels
Calcium is required for initiation of muscle contraction, exocytosis of molecules from cells, including neurons, stimulation of the heart by pacemaker cells, blood clotting.
Parathyroid hormone (PTH): Secreted and released by parathyroid glands in response to reduced blood calcium levels. Accelerates conversion to calcitriol by kidney
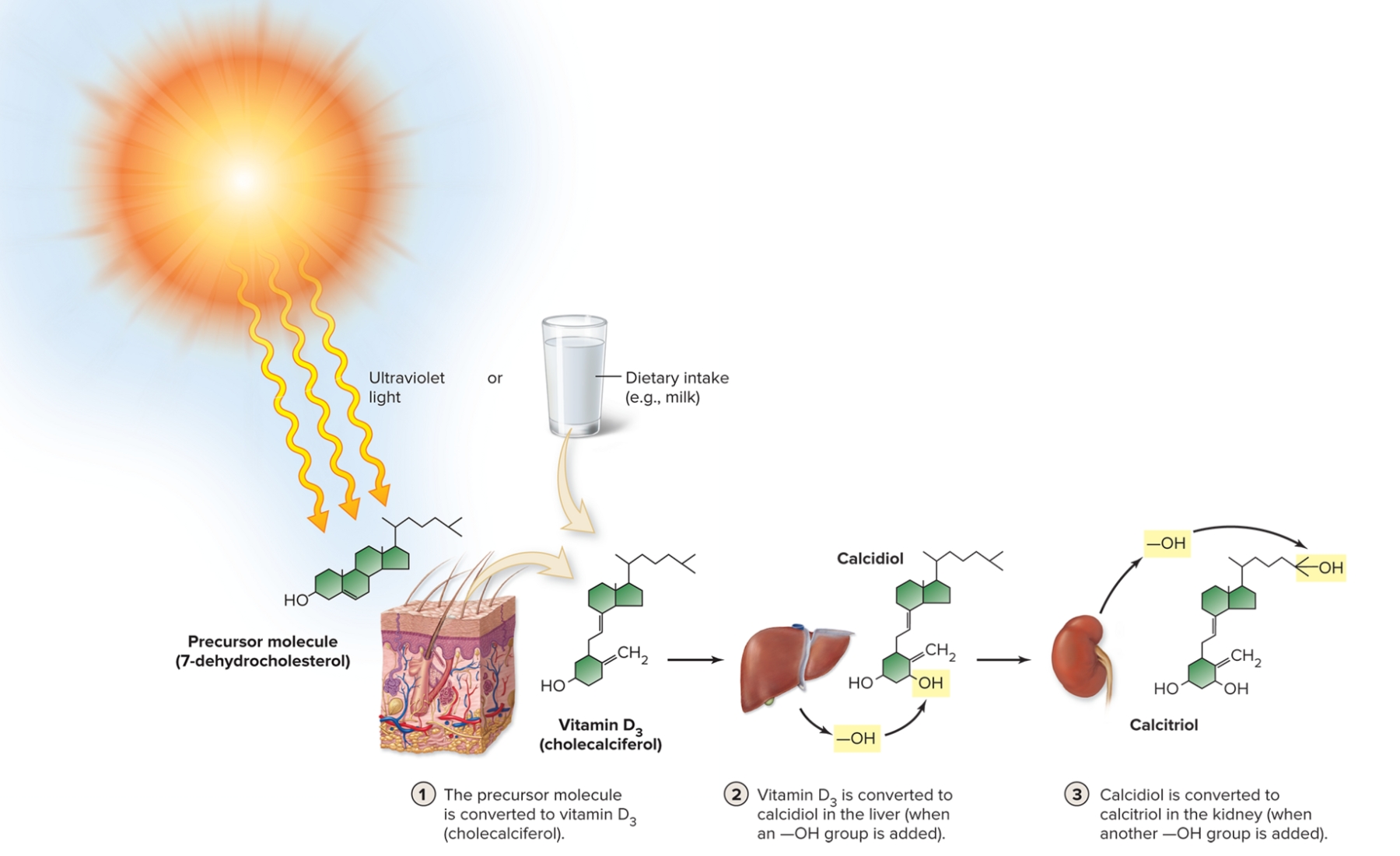
What is the interactions between PTH and active vitamin D3 and major organs?
Bone: Act synergistically to increase release of calcium from the bone into the blood by increasing osteoclast activity
Kidneys: Stimulate the kidney to excrete less calcium in urine and increase calcium reabsorption
Small intestine: Only calcitriol increases absorption of calcium from small intestine into the blood
What is calcitonin?
Aids in regulating blood calcium levels.
Less significant role than PTH or calcitriol.
Released from the thyroid gland in response to high blood calcium levels. Also secreted in response to exercise.
Inhibits osteoclast activity.
Stimulates kidneys to increase loss of calcium in the urine, therefore reducing blood calcium levels.
Greatest effect during greatest bone turnover, for example, growing children
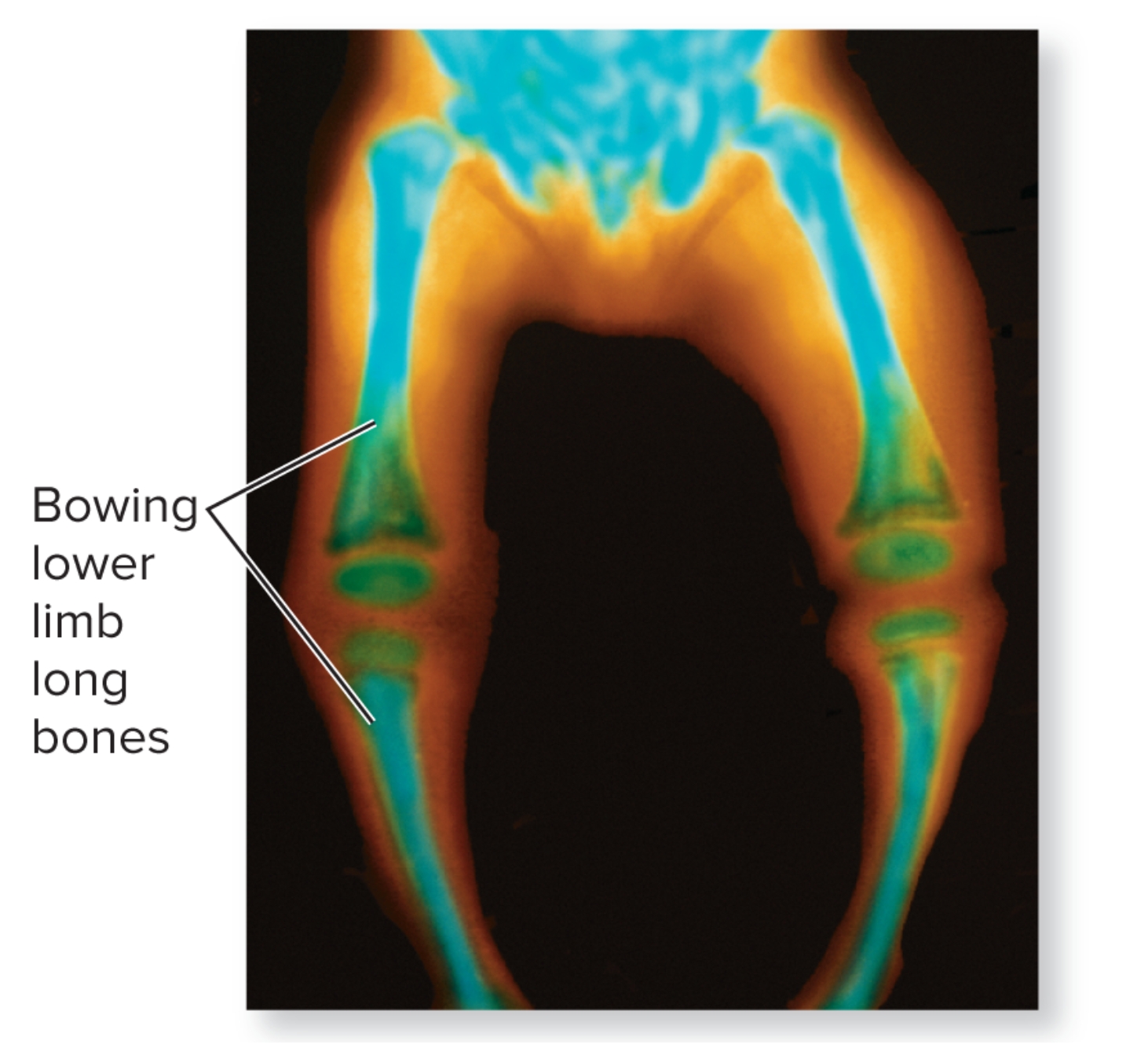
What is rickets?
Disease caused by vitamin D deficiency in childhood> Characterized by deficient calcification of osteoid tissue
Bowlegged appearance, Disturbances in growth, hypocalcemia, and tetany (cramps and twitches) caused by low blood calcium
Occurs in some developing nations but incidence increasing in urban U.S. children
What are the two ways aging affects bones?
Decreased tensile strength of bone: less protein/collagen in bones, inorganic material increases (calcium). Becomes brittle and susceptible to fracture
Bone loss of calcium and other minerals: Bones thinner and weaker. Insufficient ossification = osteopenia
What is osteopenia?
Occurs slightly in all people with age.
Begins age 35 to 40.
Osteoblast activity declines; osteoclast activity at previous levels.
Vertebrae, jaw bones, epiphyses lose large amount of mass.
Women lose more of their skeletal mass every decade than men
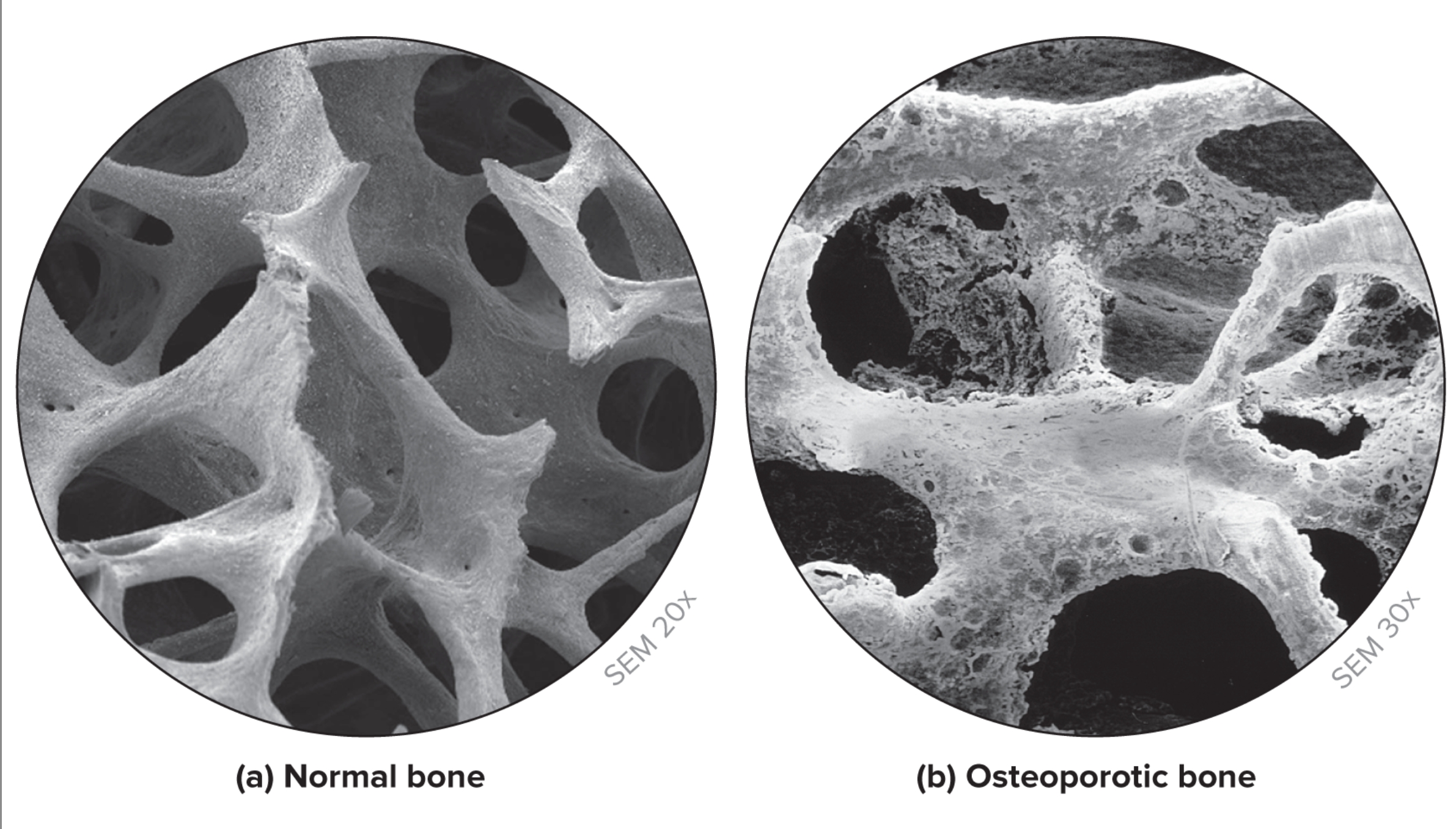
What is osteoporosis?
Reduced bone mass sufficient to compromise normal function. Occurs in a significant percentage of older individual.
Reduced hormones with age (Vitamin D, growth hormone, estrogen, and testosterone).
Results in decreased bone mass, weakened bones prone to fracture.
Linked to age, onset of menopause, Caucasian race, smoking, family history, and sedentary lifestyle. Postmenopausal women at most risk.
Increased incidence of fracture, especially at wrist, hip, vertebral column.
Best treatment is prevention with diet and physical activity in young adults.
Medical treatments involve slowing rate of bone loss and attempting to stimulate new bone growth.

What is a comminuted bone fracture?
3 or more pieces (aged)

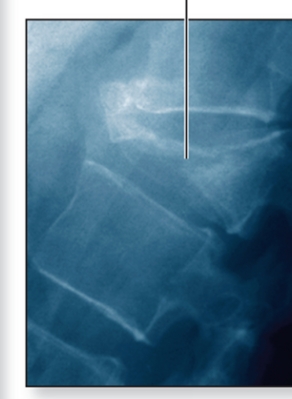
What is a spiral bone fracture?
ragged, twisting break (sports)
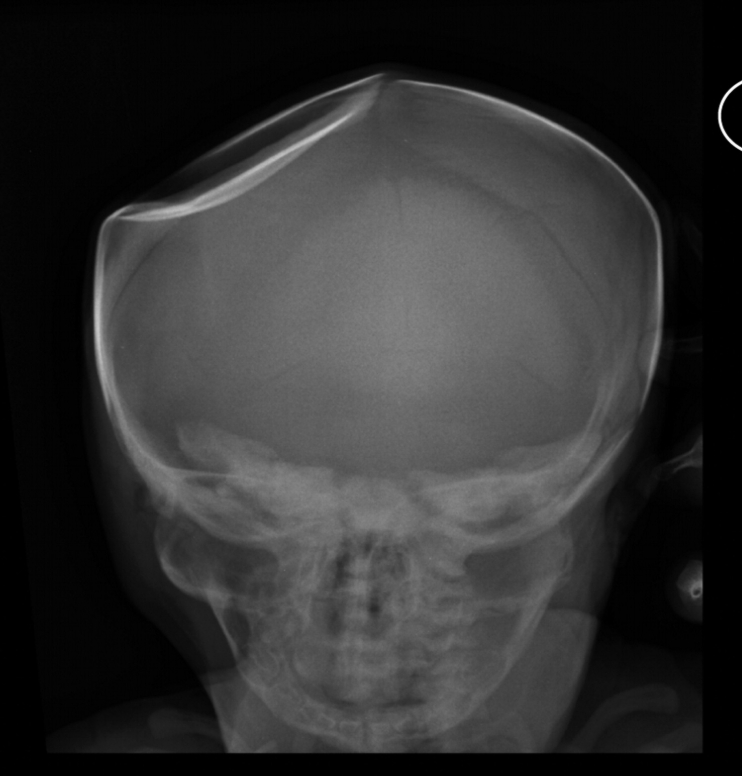
What is a depression bone fracture?
pressed inward (skull fracture)
What is a compression bone fracture?
crushed (osteoporosis)
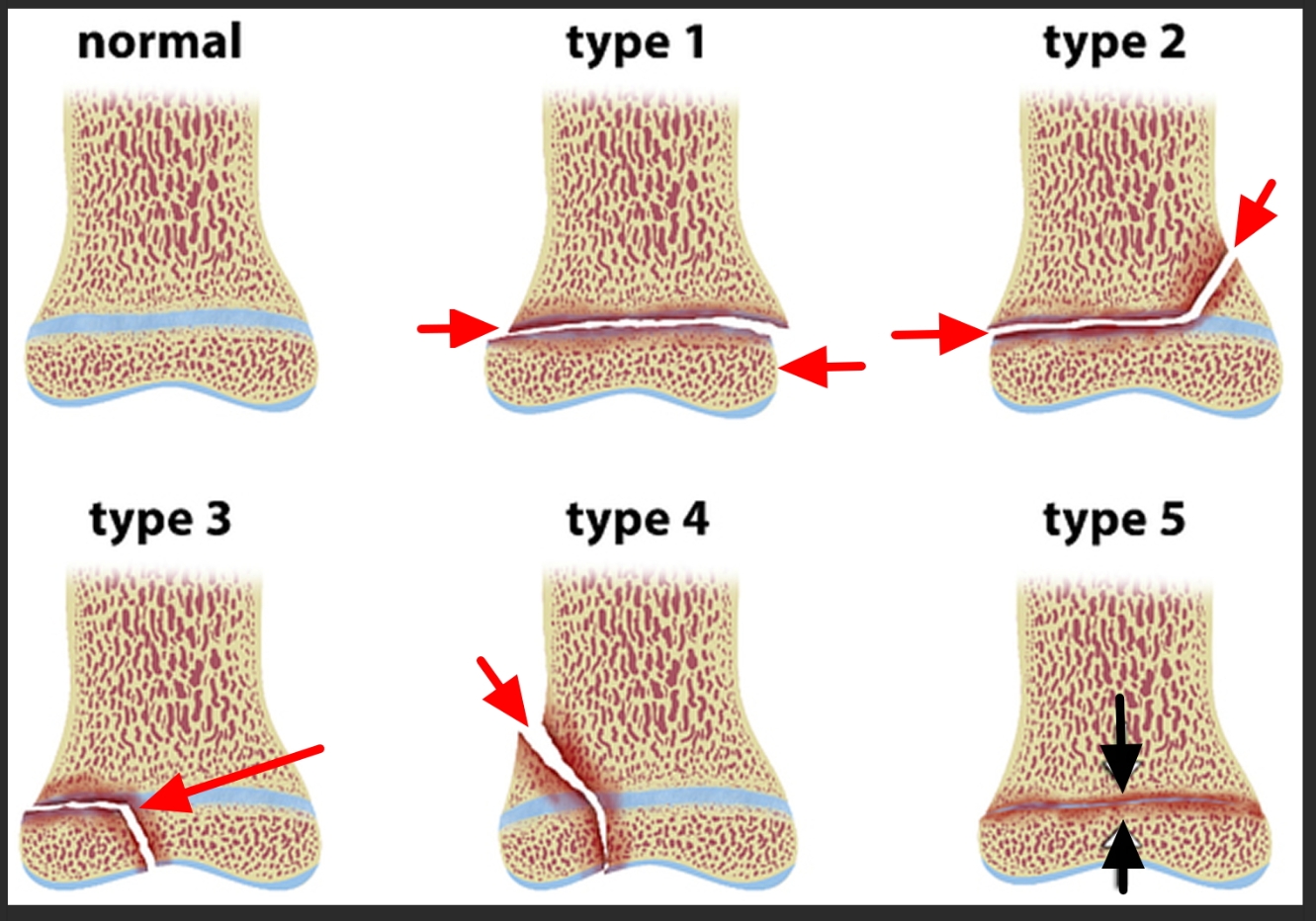
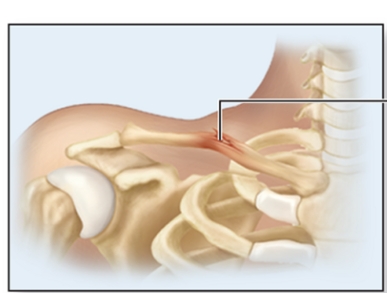
What is an epiphyseal bone fracture?
separation at plate (children)
What is a greenstick fracture?
only one side breaks (children)
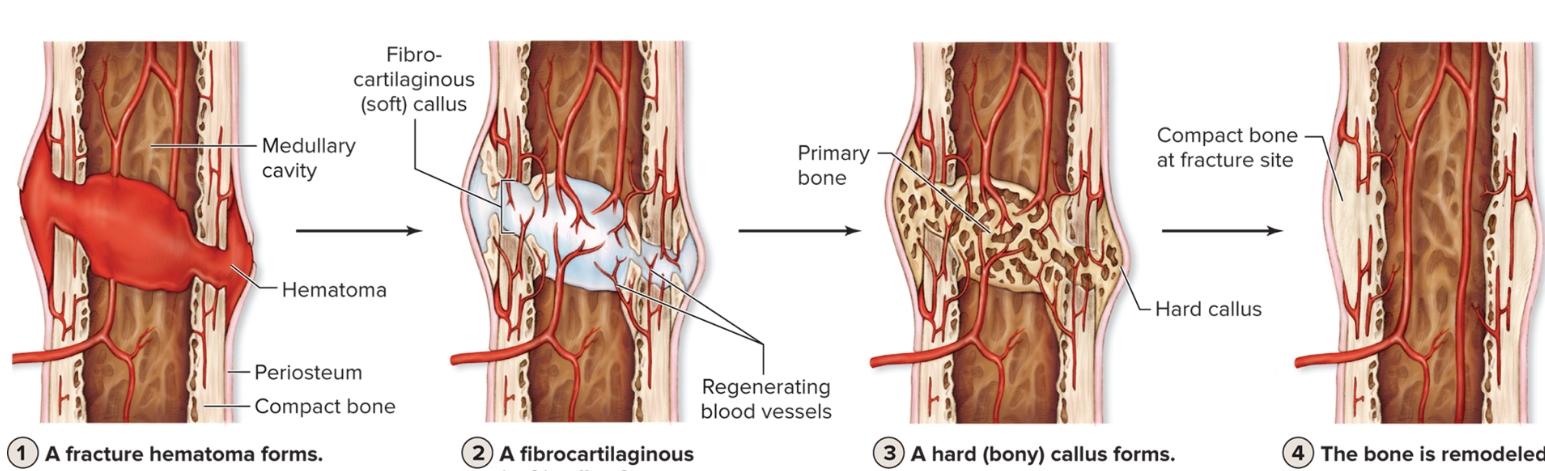
What are the four steps of fracture repair?
Fracture hematoma forms: Blood vessels torn within periosteum
Fibrocartilaginous (soft) callus forms: Fibroblasts produce collagen fibers, chondroblasts form dense regular CT
Hard (bony) callus forms: Osteoblasts adjacent to callus produce trabeculae, replaces callus, forms a hard (bony) callus, continues to grow and thicken.
Bone is remodeled: Final phase of fracture repair, osteoclasts remove excess bony material, compact bone replaces primary bone. Usually leaves a slight thickening of bone