4. The Gonads
1/26
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
27 Terms
What are the main classes of sex hormones and their key examples?
Androgens → Testosterone
Oestrogens → 17β-Oestradiol
Progestogens → Progesterone
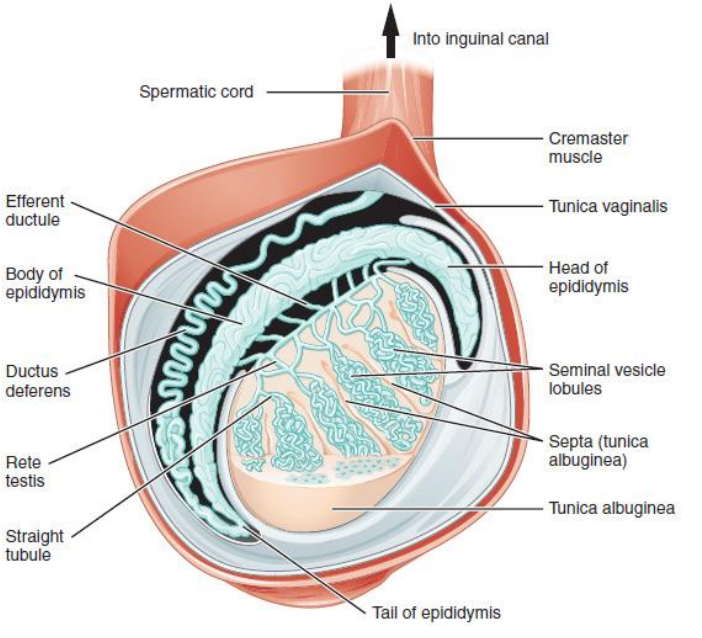
What are the functions of the testes & the pathway of sperm production?
Functions:
Spermatogenesis (sperm cell development)
Testosterone production
Sperm production pathway:
Occurs in seminiferous tubules
Spermatozoa secreted into tubule lumen → epididymis → vas deferens → expelled from testes
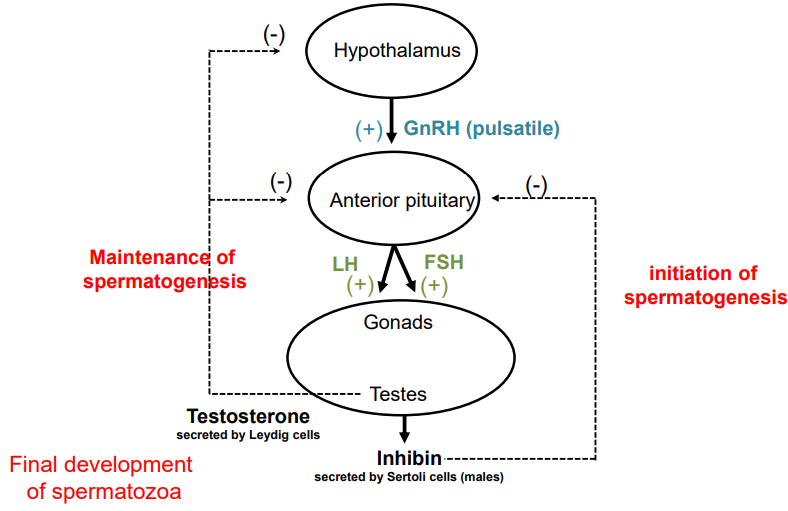
How is testosterone secretion regulated & what is its role in spermatogenesis?
Leydig cells (in testes) secrete testosterone
Stimulated by LH & FSH from anterior pituitary
LH → maintains spermatogenesis
FSH → initiates spermatogenesis
GnRH (from hypothalamus) controls LH & FSH via pulsatile release
Sertoli cells (in tubule walls) aid sperm maturation & secrete inhibin
Inhibin → negative feedback on FSH
Testosterone → essential for spermatozoa maturation
↑ Testosterone → negative feedback on:
Hypothalamus = ↓ GnRH
Anterior pituitary = ↓ LH & FSH
= ↓ testosterone from gonads
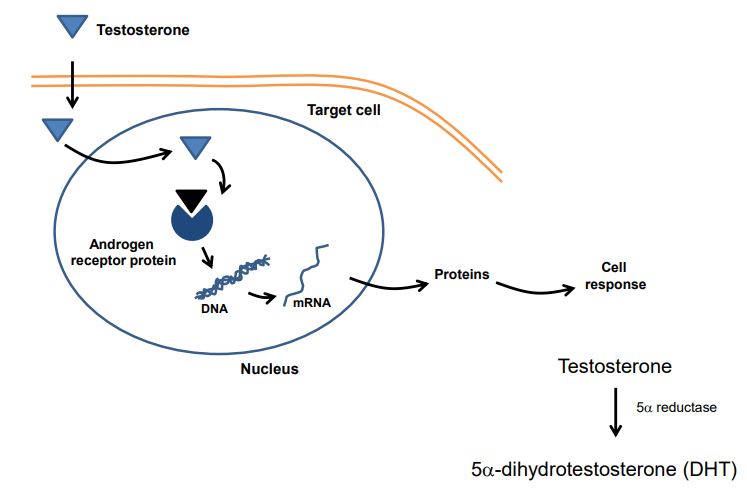
What is the mechanism of action of testosterone & the role of DHT?
Testosterone enters cell, binds androgen receptor
Complex binds DNA → protein production → cell response
In some tissues, testosterone → DHT via 5α-reductase
DHT = more potent; needed for full androgen effect
5α-reductase inhibitors ↓ DHT (used in treatment)
Enzyme dysfunction → ↓ DHT → hyposecretion effects
What are the main actions of testosterone at different life stages?
Foetus:
Male genitalia development
Testes descent
Puberty:
Growth of sex organs
Growth spurt & bone epiphysis fusion
Deep voice, body hair, acne
↑ Muscle & strength (anabolic)
Adult:
Maintains masculinity, libido, spermatogenesis
Causes scalp recession & baldness
What are the causes & treatment of testosterone hyposecretion?
Causes:
Absent testes at birth (primary hypogonadism)
Low pituitary gonadotrophins (secondary hypogonadism)
Undescended testes
Testes loss (castration/disease)
5α-reductase deficiency
Treatment:
Androgen replacement therapy
What are the methods of testosterone replacement therapy & which is most common?
Deep IM injection: testosterone enantate or propionate
Capsules (oily solution): testosterone undecanoate
Transdermal (most common): Testim, Testogel, Tostran
What causes hypersecretion of testosterone & what is its effect?
Cause: Rare, usually Leydig cell tumours in children
Effect: Precocious puberty
What are the clinical uses of androgens?
Replacement therapy for hypogonadism (testicular or pituitary disease)
↑ Muscle mass after chronic/wasting disease (e.g. nandrolone)
Treatment of oestrogen-dependent tumours (e.g. some breast & cervical cancers)
May cause masculinisation in women (facial hair, voice deepening, acne
What are the clinical uses of anti-androgen treatments?
Testosterone receptor antagonists:
Suppress excessive sexual drive
Treat acne/hirsutism (e.g. cyproterone acetate, flutamide)
Androgen-dependent prostate cancer:
Use bicalutamide
Benign prostatic hyperplasia (BPH):
Use finasteride (5α-reductase inhibitor) to reduce potent testosterone’s effect on prostate enlargement
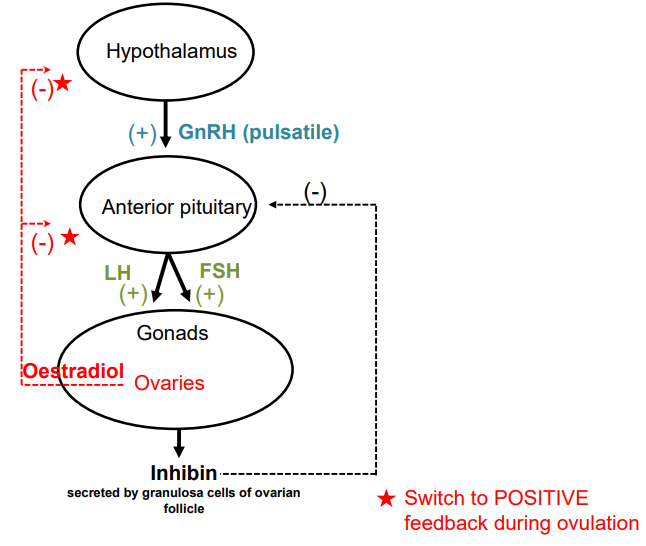
How is the secretion of female sex hormones regulated, and what is the feedback mechanism?
Ovaries secrete oestrogen (17β-estradiol) & progesterone
Oestrogen & inhibin secretion is regulated by LH & FSH from the anterior pituitary
LH & FSH are stimulated by GnRH from the hypothalamus
Granulosa cells secrete inhibin → inhibits FSH
Oestrogen exerts:
Direct negative feedback on LH
Indirect negative feedback on GnRH
High oestrogen levels → ↓ GnRH → ↓ LH & FSH
During ovulation: feedback switches to positive, causing LH/FSH surge → triggers ovulation
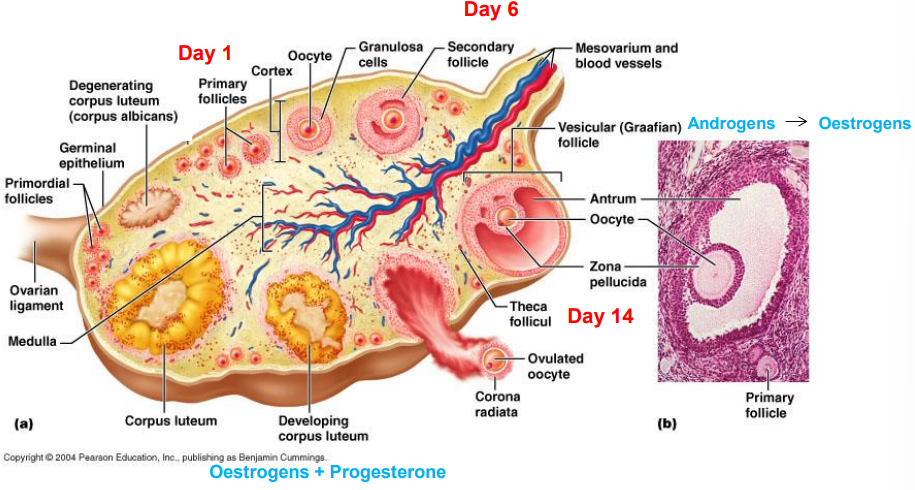
What happens during the ovarian cycle?
Day 1: 10–20 follicles grow; 1 becomes dominant by day 6
Dominant follicle matures into Graafian follicle, secretes oestrogen
Day 14: Ovulation — oocyte released into fallopian tube
Remaining cells form corpus luteum → secretes oestrogen & progesterone
If no fertilisation → corpus luteum degenerates, cycle restarts
How do hormones regulate the ovarian & menstrual cycle?
Days 1–13:
FSH ↑ → follicle maturation
Oestrogen ↑ from growing follicle → initially negative feedback
Around Day 14:
High oestrogen switches to positive feedback
LH & FSH surge → ovulation
Post-ovulation:
Follicle becomes corpus luteum → secretes oestrogen & progesterone
Progesterone ↑ → stabilises & vascularises endometrium
If no fertilisation:
Corpus luteum degenerates → hormone levels ↓
Endometrium sheds → menstruation
Cycle restarts
What hormonal changes occur during pregnancy?
hCG secreted from day 20 → basis of pregnancy tests
hCG maintains corpus luteum for ~9 weeks → prevents ovulation & menstruation
From 9 weeks, placenta secretes oestrogen, progesterone & hCG
Corpus luteum regresses after placental takeover
What happens during menopause?
Menstruation ceases (age 45–55)
Symptoms:
Hot flushes
Sweating
Palpitations
↑ Irritability, anxiety, depression
Vaginal atrophy
Osteoporosis
What are the principal actions of oestrogens?
Essential for normal development/maintenance of female genital tract & breasts
During puberty:
Stimulate growth of uterus, breast & vagina
Contribute to growth spurt & secondary sexual characteristics
What are the principal actions of oestrogens in adults?
Regulate menstrual cycle (growth of endometrial lining)
Important during pregnancy & lactation
Maintain sexual drive & female personality
What are the principal actions of progestogens?
Cause endometrial secretory changes for pregnancy
Stimulate breast development for lactation
Thicken & acidify cervical mucus (↓ sperm receptivity)
Reduce spontaneous myometrial contractions during pregnancy
What are the effects of oestrogen hyposecretion?
Primary hypogonadism: Ovarian failure (e.g. Turner’s) → no puberty, menstruation, or bone closure
Secondary hypogonadism: Pituitary/hypothalamic issues → ↓ hormone signals, delayed development
What are the effects of oestrogen hypersecretion?
Ovarian tumours → irregular endometrial bleeding
What are the clinical uses of oestrogens?
Treatment of hypogonadism
Treatment of menopausal symptoms (e.g., surgical removal of ovaries, hysterectomy, severe endometriosis)
Treatment of osteoporosis
What are the main formulations of HRT?
Oral tablets (natural oestrogen)
Transdermal patches
Implants
Vaginal cream or pessaries
What are less common clinical uses of oestrogens?
Treatment of androgen-dependent prostate cancer
Emergency contraception (now withdrawn due to side effects: nausea, vomiting, headaches)
What are less common clinical uses of oestrogens?
Treatment of androgen-dependent prostate cancer
Emergency contraception (now withdrawn due to side effects: nausea, vomiting, headaches)
What are clinical uses of oestrogens & anti-oestrogens?
Treat infertility: clomiphene (risk of hyperovulation & multiple pregnancies)
Treat oestrogen-dependent breast cancers:
Oestrogen antagonists: tamoxifen, toremifene
Aromatase inhibitors: letrozole, anastrozole
3β-HSD inhibitor: trilostane
What are clinical uses of oestrogens & anti-oestrogens?
Treat infertility: clomiphene (risk of hyperovulation & multiple pregnancies)
Treat oestrogen-dependent breast cancers:
Oestrogen antagonists: tamoxifen, toremifene
Aromatase inhibitors: letrozole, anastrozole
3β-HSD inhibitor: trilostane
What are clinical uses of progestogens?
Control uterine bleeding & menstrual disturbances
Treat endometriosis
Examples: northisterone, norgestrel, levonorgestrel, dydrogesterone, medroxyprogesterone