COMMUNITY AND DEVELOPMENT CONCEPTS, THEORIES, AND STRATEGIES
1/96
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
97 Terms
Pre-Spanish Era (before 1565)
Babaylans were considered as healer, prietess and leader
Spanish Era (1565-1898)
Hospitals were created for the welfare of spanish soldiers that succumbed to tropical diseases
Spanish Era (1565-1898)
First epidemic 1574: small pox (bolotong); smallpox vaccine was introduced
Health Care Under the Americans (1898-1918)
PGH was opened; UP College of Medicine was opened
Health Care Under the Americans (1898-1918)
Worst epidemic in Philippine History: cholera; cholera vaccine was first tried
Health Care Under the Americans (1898-1918)
Building more hospitals and formal medical education and medical benefits were given to Filipinos
Commonwealth Period (1936-1941)
Reorganization of public health laboratory with modern facilities – establishment of a unit for treatment and study of cancer
Japanese Occupation (1941-1945)
Increase incidence of TB, venereal diseases, Malaria, leprosy and malnutrition
Post Word War II (1945-1972)
Introduction of penicillin to treat gonnorhe
Post Word War II (1945-1972)
BCG (Bacille Calmette Guerin) was used for mass vaccination for prevention of tuberculosis
Post Word War II (1945-1972)
Rural Health Units)were established in municipalities under Pres. Ramon Magsaysay who introduced “Health Care for the masses”
BCG (Bacille Calmette Guerin)
was used for mass vaccination for prevention of tuberculosis
Health
"a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity."
Community Health
the health of a community's members, the health care they receive, and the factors that affect their health
Public Health
The science and art of preventing disease, prolonging life, and promoting health through organized community efforts.
Wellness
A dynamic process of becoming aware of and making choices toward a healthy and fulfilling life
Illness
A subjective state of feeling unwell or experiencing symptoms
Disease
An objectively measurable condition that impairs normal functioning
Physical health
The ability of the body to function properly, free from illness, injury, or disability
Mental health
Psychological and emotional well-being, affecting how individuals think, feel, and behave in daily life
Social health
Ability to form relationships and adapt to social situations
Spiritual health
Finding meaning and purpose in life
Environmental health
Living in harmony with one's surroundings
DETERMINANTS OF HEALTH AND DISEASE
1. Biological factors
2. Environmental factors
3. Socio-economic factors
Biological factors
inherent characteristics that influence a person's health and susceptibility to diseases
Environmental factors
external conditions that affect health of an individual
Socio-economic factors
influence health through:
a. Income
b. Education
c. Employment
d. social support, and
e. healthcare access
ASSESSMENT
involves systematically collecting, analyzing, and interpreting data to monitor the health status of the population.
POLICY DEVELOPMENT
involves creating policies, laws, and regulations that guide public health practice
ASSURANCE
involves ensuring that necessary health services are available and accessible to the population, promoting health equity
Public health achievements
refer to the significant improvements in the overall health of a population, which are typically the result of wellcoordinated interventions and policies aimed at preventing disease, promoting health, and improving well-being.
LEVELS OF PREVENTION
1. Primary prevention
2. Secondary prevention
3. Tertiary prevention
4. Quaternary prevention
Primary prevention
preventing the onset of disease or injury before it occurs
Secondary prevention
focuses on the early detection and intervention of diseases before they cause significant harm
Tertiary prevention
managing and mitigating the impact of an already established disease or injury
Quaternary prevention
prevent unnecessary or potentially harmful medical interventions
LEVELS OF CLIENTELE
1. Individual
2. Family
3. Community
3. Community
Individual
focusing on personalized healthcare needs
Family
targets the family as the primary unit of health intervention
Community
involves public health interventions that focus on populations within a specific community or locality
Population
interventions are aimed at the entire nation or large population groups
ETHICAL VALUES IN PUBLIC HEALTH
Beneficence
Justice
Respect for Autonomy
Non-maleficence
Beneficence
Promoting public good
Justice
Fair distribution of health resources
Respect for Autonomy
Individual right to make health decisions
Non-maleficence
Avoiding harm
Primary Sources
• Census (Philippine Statistics Authority)
• Civil Registration
• Sample Surveys
Secondary Sources
• Philippine Health Statistics
• Local Government Unit Records
• Hospital Records
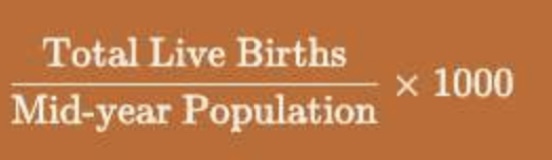
Crude Birth Rate (CBR)
number of live births per 1,000 people in a given population in a specific year
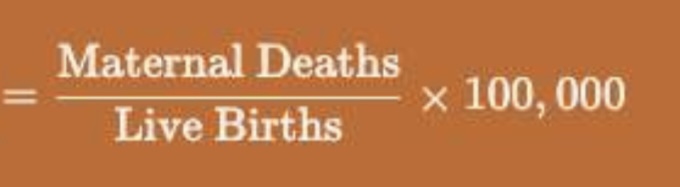
Maternal Mortality Ratio (MMR)
number of maternal deaths per 100,000 live births
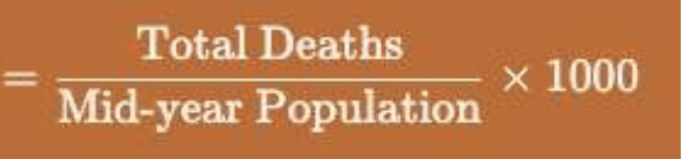
Crude Death Rate (CDR)
number of deaths per 1,000 people in a given population over a specific period (usually one year
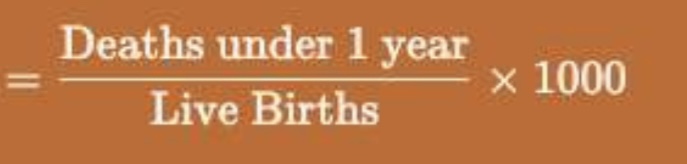
Infant Mortality Rate (IMR
number of deaths of infants under 1 year of age per 1,000 live births
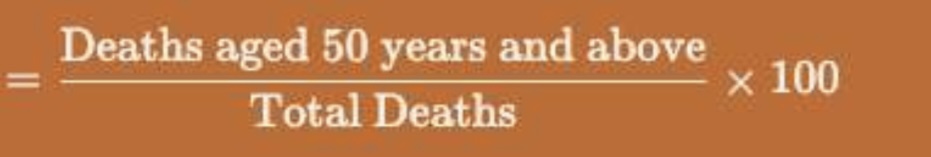
Swaroop’s Index
proportion of deaths that occur in individuals aged 50 years and above
Ludwig von Bertalanffy
General Systems Theory (GST) proponent
General Systems Theory (GST)
posits that various systems, whether biological, social, or ecological, share common principles and can be understood through their interconnections and interactions.
General Systems Theory (GST)
This theory emphasizes the holistic nature of systems, where the sum of parts is greater than the individual components.
General Systems Theory (GST)
It helps us understand how different social, economic, and environmental factors interact to influence health outcomes.
Social Learning Theory (SLT)
emphasizes the importance of observation, imitation, and modeling in learning behaviors.
Social Learning Theory (SLT)
Social Learning Theory (SLT) proponent
Social Learning Theory (SLT)
This theory suggests that individuals learn new behaviors by watching others, especially those they perceive as role models. In community development, this theory highlights the role of social networks in promoting health and well-being.
Social Learning Theory (SLT)
This theory underscores the importance of incorporating social dynamics into health promotion strategies, making it essential for developing effective community interventions.
Health Belief Model (HBM)
is a psychological framework that seeks to explain and predict health behaviors based on individuals' beliefs and attitudes.
Irwin M. Rosenstock
Health Belief Model (HBM) proponent
Health Belief Model (HBM)
It posits that people are more likely to engage in health promoting behaviors if they perceive a high level of personal susceptibility to a health issue, believe the consequences of the health issue are severe, think that taking a specific action would reduce their risk, and feel that the benefits of taking that action outweigh the barriers.
Health Belief Model (HBM)
can help community developers tailor their strategies to address specific beliefs and misconceptions that hinder health-promoting behaviors.
Milio’s Framework for Prevention
expands the understanding of health determinants by focusing on the social and environmental contexts that shape individual behavior.
Nancy Milio
Milio’s Framework for Prevention proponent
Milio’s Framework for Prevention
emphasizes the need to assess both individual choices and the broader societal factors that influence those choices.
Pender’s Health Promotion Model
emphasizes the role of individual characteristics and experiences in shaping health behaviors. It focuses on the intrinsic motivations that drive individuals to engage in health-promoting activities.
Nola J. Pender
Pender’s Health Promotion Model proponent
Pender’s Health Promotion Model
This model reinforces the idea that effective health promotion should be person-centered, taking into account individual preferences and motivations.
Transtheoretical Model
outlines a five-stage process that individuals typically follow when changing behavior.
James O. Prochaska and Carlo DiClemente
Transtheoretical Model proponents
Precontemplation
Contemplation
Preparation
Action
Maintenance
five stages of the transtheoretical model
Precontemplation stage
individuals are not yet considering change, often due to a lack of awareness of the problem.
Contemplation stage
they recognize the need for change but are ambivalent about taking action.
Preparation stage
involves planning for change, where individuals may start small efforts toward their goal.
Action
is the stage where individuals actively modify their behavior
Maintenance
involves sustaining these new behaviors over the long term.
Precede-Proceed Model
serves as a comprehensive planning framework for health promotion and education.
Lawrence W. Green and Marshall W. Kreuter
Precede-Proceed Mode proponents
PRECEDE
which focuses on assessing needs before implementing a program
Precede
The ________ phase includes several assessments: social assessment, epidemiological assessment, behavioral and environmental assessment, and educational and organizational assessment. This ensures that interventions are based on community needs and are contextually relevant
PROCEED
emphasizes the implementation and evaluation of health programs
Proceed
The __________ phase involves the actual implementation of the program and its ongoing evaluation to measure effectiveness and make necessary adjustments. This model underscores the importance of a data-driven approach to health promotion, ensuring that interventions are not only effective but also sustainable
PRIMARY HEALTH CARE
Essential health care based on practical, scientifically sound and socially acceptable methods and technology made universally accessible to individuals and families in the community through their full participation and at a cost that community and the country can afford … (Alma-Ata, 1978)
PRIMARY HEALTH CARE
is essential health care that is a socially appropriate, universally accessible, scientifically sound first level care provided by a suitably trained workforce supported by integrated referral systems and in a way that gives priority to those most in need, maximizes community and individual self-reliance and participation and involves collaboration with other sectors.
Accessibility
refers to the ease with which individuals can obtain health services, which is crucial for underserved populations.
Community participation
emphasizes involving individuals in the planning and implementation of health services, ensuring that they are culturally appropriate and effective.
Comprehensive care
indicates that PHC addresses a wide array of health issues, including preventative, curative, and rehabilitative services, thus promoting overall well-being rather than merely treating illness.
1970s
The concept of Primary Health Care emerged in the _____ as a response to the inadequacies of traditional health systems.
Declaration of Alma-Ata in 1978
The landmark ______________________________ marked a pivotal moment, recognizing that health is a fundamental human right and advocating for the need to provide primary health care as part of comprehensive health systems.
Equitable distribution of health care
according to this principle, primary care and other services to meet the main health problems in a community must be provided equally to all individuals irrespective of their gender, age, caste, color, urban/rural location and social class
Community participation
in order to make the fullest use of local, national and other available resources. Community participation was considered sustainable due to its grass roots nature and emphasis on self sufficiency, as opposed to targeted (or vertical) approaches dependent on international development assistance
Health workforce development
comprehensive healthcare relies on an adequate number and distribution of trained physicians, nurses, allied health professions, community health workers and others working as a health team and supported at the local and referral levels
Use of appropriate technology
medical technology should be provided that is accessible, affordable, feasible and culturally acceptable to the community.
Multi-sectional approach
recognition that health cannot be improved by intervention within just the formal health sector; other sectors are equally important in promoting the health and self-reliance of communities.