Week 8 surgical oncology
1/60
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
61 Terms
what is the importance of knowing which disease you are dealing with for surgical oncology?
if you dont know which disease you are dealing with, inadequate, inappropriate, or erroneous treatments may be administered
What options do you have to know what the disease is with surgical oncology?
Fine Needle Aspirate (FNA)
Biopsy - Incisional unless strongly suspected to be benign
needle-core
wedge #11 or #15 blade
punch
what is cytoreductive surgery?
planned incomplete excision of a tumor (not debulking - leaving a lot of tissue behind)
generally means downstaging to microscopic disease
when is cytoreductive surgery for tumors indicated?
when complete excision carries an unacceptable consequence for the individual
must yield some P benefit by reducing tumor burden/improving QOL
downstaging to microscopic disease
what is the goal of palliative surgery?
improve QOL without trying to prolong survival
may not involve adjuvant therapies (chemo or radiation)
how are decisions to perform palliative surgery made?
must carefully weight the inflicted morbidity vs the anticipated gains
e.g. hospitalization and surgery involve pain/stress/etc
e.g. splenectomy for hemoperitoneum in a dog with metastatic hemangiosarcoma
what is the goal of curative intent surgery?
to remove the entire tumor and any local extensions or surrounding microscopic disease
aka 'definitive' surgery or to obtain 'local control' of disease
which treatment modality cures more cancer than any other single treatment modality?
surgery
how are the benefits of surgery for oncologic patients maximized?
the surgeon must understand the biology of the tumor and be knowledgeable of other tx modalities to offer best tx regimen
what does TLC refer to for tumor staging?
tumor: obtain accurate diagnosis
location: stage the patient (know how far dz has advanced, know where it mets frequently)
condition: overall health status (co-morbidities) and client desires/input
how are treatment regimens for oncologic surgery planned?
-minimize morbidity
-maximize quality and duration of life
-must involve owners expectations/situation
-remember the 1st surgery is the best chance for a cure
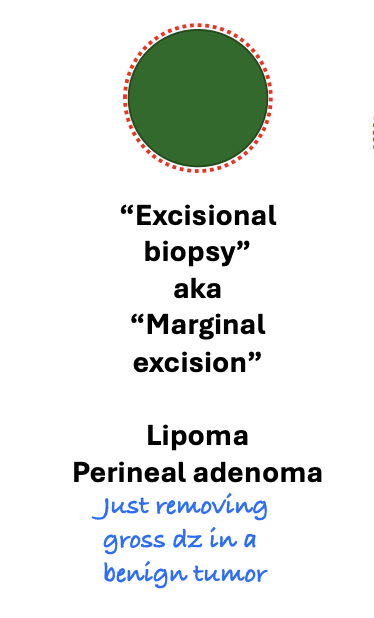
which tumor types are excisional biopsies/marginal excisions used for?
any benign tumors (lipoma, perineal adenomas)
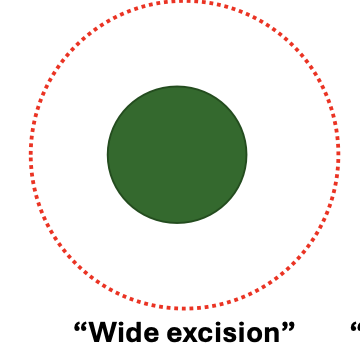
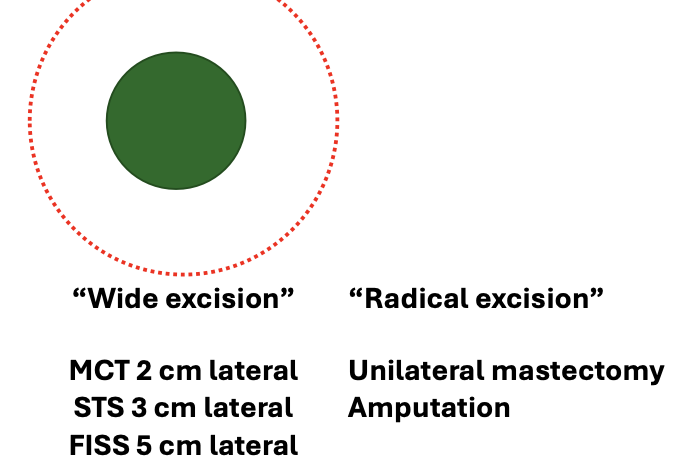
what are the lateral margins used for wide excision of MCTs, STSs, and FISSs?
MCT: 2cm lateral
STS: 3cm lateral
FISS: 5cm lateral
what is the goal of incisional excisions?
debulking if large gross disease is left
do incisional excisions remove macroscopic disease? microscopic disease?
macroscopic disease: no
microscopic disease: no
do marginal excisions (excisional biopsy) remove macroscopic disease? microscopic disease?
macroscopic disease: yes
microscopic disease: no
do wide marginal excisions (excisional biopsy) remove macroscopic disease? microscopic disease?
macroscopic disease: yes
microscopic disease: yes
does radical excision remove macroscopic disease? microscopic disease?
macroscopic disease: yes
microscopic disease: yes
which surgeries are aimed at local curative intent?
wide marginal excision and radical excision
if benign: marginal excision
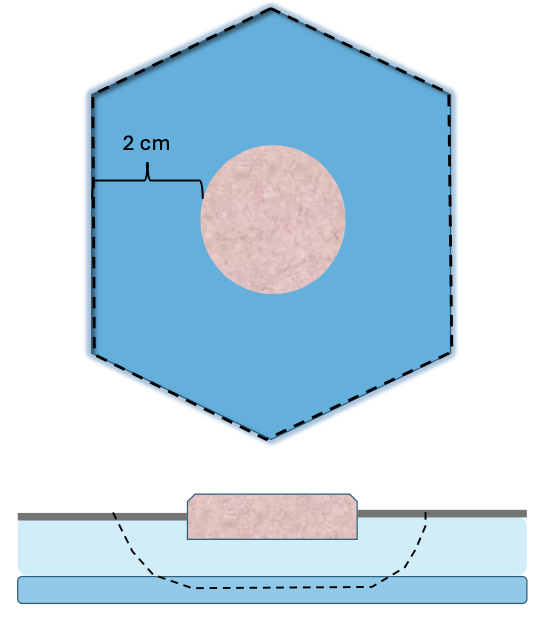
Mass removals require what lateral margins for MCT and STS? Fascial planes?
MCT: 2 cm
STS: 3 cm
Deep margins - 1 fascial plane
how should tumors be handled during curative-intent surgery?
treat the tumor as if it were an abscess and the tumor cells are bacteria--> potential to seed anywhere in the tissue once you've exposed your instruments/gloves to them

what are principles of curative-intent surgeries?
-dont puncture/rupture tumor
-ligate vessels
-remove previous drainage/biopsy tracks
-sharp dissection/cautery
-use monofilament suture
-irrigate to keep remaining tissues healthy
-dont touch ulcerated areas (infection)
-remove tumor w/ adequate margins
-avoid drains
-mark/paint margins
-excision is only as good as 'worst' margin
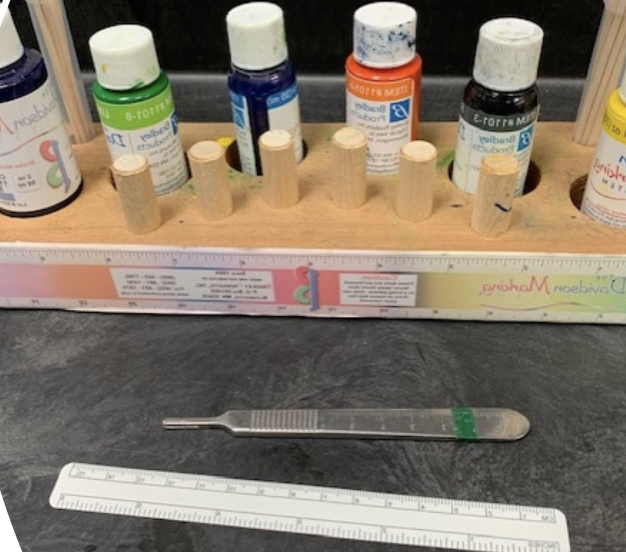
what is the purpose of marking surgical margins?
aids in orientation and identification of surgical margins
Ink vs suture - commercial inking kits, prevent running of ink, air dry ~15 min
ink will bleed into surrounding tissue, take pic right after labeling
how should neoplastic masses be submitted for pathology?
10% neutral buffered formalin
use 1:10 ratio of tissue to formalin

how is deformation of tumor prevented when putting in formalin to submit for pathology?
suture edges of mass, or can suture to formalin-soaked cardboard
anticipate tissue shrinkage

__ help locate margins if we need to follow up with radiation therapy.
hemo clips
what is the relative risk for mammary neoplasia in dogs if spayed prior to first estrus?
0.5%
after 1st estrus but before 2nd estrus= 8%
after second estrus= 26%
what is the risk of mammary tumors in female cats if spayed by the time of puberty?
risk of mammary tumors are reduced by 7-fold
does castration in male dogs/cats eliminate the risk of developing prostatic cancer?
no
does eliminate risk of testicular cancer (duh)
what are indications for a mastectomy?
mammary neoplasia

are canine mammary tumors more likely to be malignant or benign?
50% chance of being malignant, 50% chance of being benign

are feline mammary tumors more likely to be malignant or benign?
majority of mammary tumors in cats are malignant
80% malignant, 20% benign
So in cats ALWAYS remove
when is it okay to do a lumpectomy (excisional biopsy) for canine mammary tumors?
for dogs with 1+ small masses
change gloves/instruments between masses
how large should the skin incision be for lumpectomies in dogs?
skin incision=mass diameter (no larger)
usually linear skin incision but may be elliptical if mass associated with a nipple
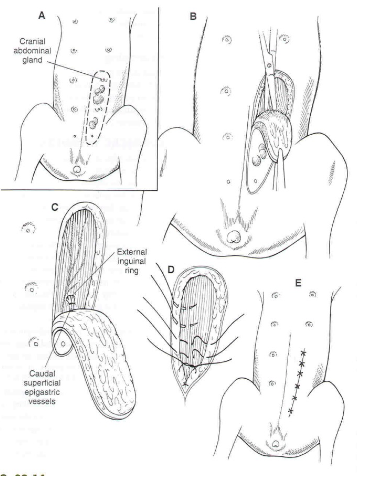
what are indications for a cranial regional mastectomy?
cranial regional if mammary mass is affecting mammary glands 1, 2, or 3
what are indications for a caudal regional mastectomy?
caudal regional if mammary mass is affecting mammary glands 3, 4, or 5
what mammary gland will always be removed with either a cranial or caudal regional mastectomy?
3
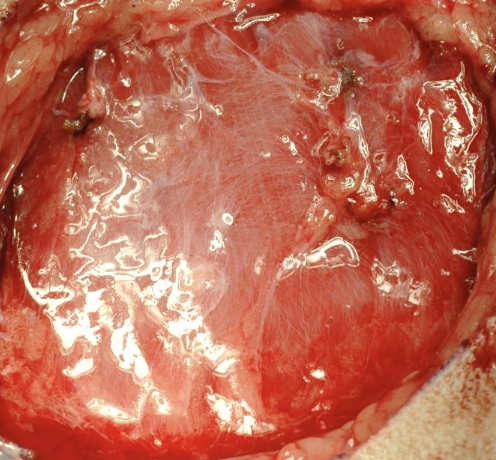
how are mastectomies (wide excisions) performed?
either cranial or caudal regional, as well as en bloc regional LN removal
'deep' margin is usually level of external fascial sheath of external abdominal oblique (rarely invades into body wall)
True or False? Mastectomy typically does not invade the body wall so the deep margin is usually the level of the external fascial sheath.
True. In RARE cases of invasion into body wall, will necessitate body wall resection
what is a chain mastectomy?
'radical excision', can be unilateral or bilateral
include lymph nodes in resection
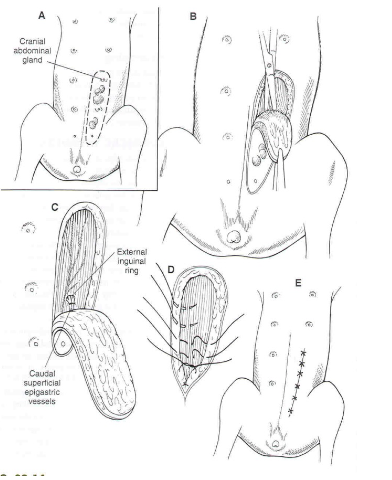
which lymph nodes drain the mammary glands?
glands 1 and 2: drain into axillary LN
glands 4 and 5: drain into inguinal LN
gland 3: drains into either LN (inguinal or axillary)
what is the gold standard surgery for cats with mammary tumors?
staged bilateral chain mastectomy (single session not recommended)
what are complications of performing bilateral chain mastectomies in one surgery in cats?
there is high tension--> greater chance of dehiscence
what should be done pre/peri-operatively for animals with multiple mammary tumors?
1. stage patient (chest rads, AUS, LN aspirates)
2. client communication
3. peri-op abx (cefazolin)
4. analgesia (opioids, +/- NSAID)

what are potential complications of removing multiple mammary tumors?
-dehiscence
-incisional infection
-tumor regrowth/spread
-hemorrhage (cranial and caudal superficial epigastric vessels)
-hematoma/seroma

what are the general considerations for amputation?
-QOL of animal (generally very well tolerated)
-co-morbidities may affect outcome
-owner education
what co-morbidities may affect outcome of amputation?
neurologic disease
orthopedic disease
obesity (ideally have weight loss prior)
what are the goals of amputation?
1. remove limb whole providing appropriate and secure hemostasis
2. minimize morbidity (includes proper tissue handling, proper anesthesia/analgesia, minimize dead space and proper wound closure)
3. consider margins and surgical oncology principles
what techniques are used for amputations?
-many variations
-skin incision varies depending on tumor presence/location
-major arteries and veins are ligated separately (double ligate, consider transfix for distal ligature)
-transection of muscles may vary
-local nerve blocks prior to nerve transection
what are complications of amputation?
-closure is as important as removal of limb; prevent dead space, appropriate apposition of tissue layers, adhere to aseptic techniques
-phantom limb pain
what are 2 methods for thoracic limb amputations? which is the most common/appropriate?
forequarter amputation or scapulo-humeral disarticulation
most common/appropriate= forequarter amputation as it better if no stump for P to try to use
what does a forequarter amputation of the thoracic limb involve?
removal of scapula and entire limb (chest wall protected even w/o presence of scapula)
tumors of proximal humerus are more safely/completely removed by this method
what are disadvantages of scapulo-humeral disarticulation amputations?
scapular muscles atrophy post-op, leaving bony prominences that can result in chronic skin ulcers
what are 3 methods of pelvic limb amputations? which is the preferred method?
1. coxofemoral disarticulation (preferred method)
2. proximal third femoral osteotomy
3. acetabulectomy/hemipelvectomy
what are advantages of a proximal third femoral osteotomy over disarticulation for pelvic limb amputations?
technically easier/faster than disarticulation
when is a acetabulectomy/hemipelvectomy indicated?
needed if a proximal femoral lesion dictates wider margins
what does the post-op care for amputations consist of?
-hospitalization (1-2 nights, 2 is always better)
-analgesia (opioid, NSAID, gaba)
-harness to help with ambulation
-cold compressing first 3 days, warm compressing after (prevents seroma formation, which is common)
-yoga mats, rugs, etc.
what is the most common reason for digit amputations?
neoplasia
if a tumor is present at the metacarpo/metatarso-phalangeal joint, where should amputation occur?
distal ostectomy of metacarpal/metatarsal to remove hyaline cap
can place tourniquet intra-op (no longer than 20mins) to ensure hemostasis
True or False? You can remove multiple digits on one foot.
True. Still OK to remove both weight bearing digits 3&4
what is the post op care for digit amputations?
soft padded bandage for 1-2 weeks
