Perceptual Speech Assessment
1/6
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
7 Terms
Perceptual Assessment of Motor Speech Disorders
🧠 What Is a Perceptual Assessment?
A perceptual assessment involves listening to and observing speech production to evaluate how the different components of the motor speech system are functioning.
It is the primary clinical tool used to diagnose dysarthria types and guide treatment planning.
It helps identify which subsystems are impaired and the nature of those impairments.
🎯 Aims of the Assessment
Elicit behaviours that inform both diagnosis and management.
Establish which components of speech are within normal limits, and which are disrupted.
Detect patterns of impairment across:
Respiration
Phonation
Resonance
Articulation
Prosody
👀 What Do We Observe and Listen For?
Changes in clarity, loudness, pitch, intonation, nasality, voice quality, and speech rate.
Evaluate speech characteristics in connected speech, isolated sounds, and repetitive tasks.
🧪 Common Perceptual Tasks Used
Task | Purpose |
Vowel prolongation (e.g. /a/) | Assesses phonatory control, sustained breath support, and voice quality |
Alternating Motion Rates (AMRs) (e.g. “puh-puh-puh”) | Measures speed and regularity of repetitive articulatory movements |
Sequential Motion Rates (SMRs) (e.g. “puh-tuh-kuh”) | Assesses ability to rapidly sequence different articulatory movements |
Spontaneous speech or reading aloud | Assesses natural prosody, articulatory precision, resonance, and overall intelligibility |
Sentence repetition or paragraph reading | Allows observation of connected speech features, such as stress and intonation |
🧭 Interpreting the Findings
We compare client performance to what is expected in typical motor speech.
Features like shortened vowel prolongation (<3 seconds) may indicate reduced respiratory support or glottal insufficiency.
Irregular AMRs/SMRs can suggest cerebellar dysfunction (ataxic dysarthria) or basal ganglia issues (hypo-/hyperkinetic dysarthria).
Diadochokinetic (DDK) Rates in Motor Speech Assessment
🔁 What Are DDK Rates?
DDK stands for Diadochokinetic rates—used to evaluate motor control, coordination, and speed of speech movements.
It involves rapid, repeated articulation of syllables or sequences of syllables.
Crucial for assessing articulatory precision and motor planning/execution in various dysarthrias and apraxia.
🔍 Types of DDK Tasks
🟦 Alternating Motion Rates (AMRs)
Single repeated syllables such as:
“puh-puh-puh” (labial)
“tuh-tuh-tuh” (alveolar)
“kuh-kuh-kuh” (velar)
Assesses individual articulator speed and rhythm.
🟧 Sequential Motion Rates (SMRs)
Sequenced combinations of syllables, e.g.:
“puh-tuh-kuh”
“butterfly,” “Patty cake”
Measures ability to rapidly shift between different articulatory positions—important for motor planning.
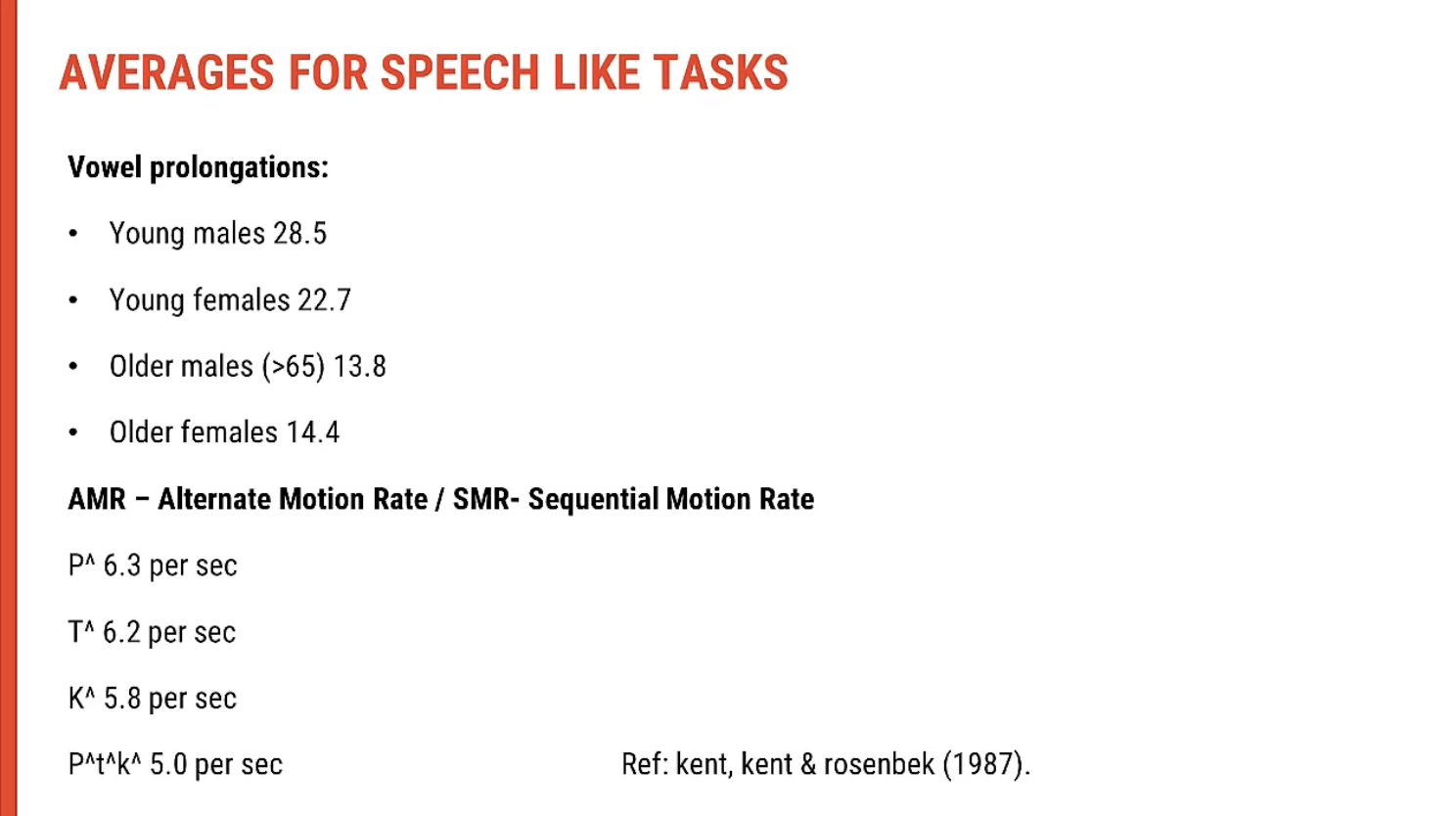
📈 Normative Data for DDK
Expected rate: approximately 5–7 repetitions per second for AMRs and SMRs.
Below normal rate may suggest:
Flaccid or spastic dysarthria (slowed, weak, or strained articulation)
Ataxic dysarthria (irregular rhythm)
Apraxia of speech (inconsistent sequencing errors)
🎤 Clinical Tips for DDK Tasks
Always seek consent before recording.
Record DDK tasks and slow them down for detailed perceptual analysis.
With experience, clinicians often develop a “tuned ear” for what falls outside the normal range.
Compare sides if relevant (e.g. unilateral weakness).
Using DDK Chains for Clinical Modelling and Visual Feedback
🎯 Purpose of Modelling DDK Tasks
When assessing alternating motion rates (AMRs) and sequential motion rates (SMRs), clinicians model productions so clients can:
Hear the correct rate, clarity, and rhythm.
Imitate the production as closely as possible.
Especially helpful in cases of dysarthria or apraxia, where motor planning or execution is impaired.
🎙 Modelling and Recording
DDK productions (e.g. "puh-puh-puh" or "puh-tuh-kuh") can be recorded on an iPhone or similar device.
The client listens to the model, then attempts to reproduce it.
These recordings allow:
Auditory comparison between clinician and client output.
Self-monitoring and feedback.
📊 Visual Feedback from Recordings
DDK recordings can be visualised using waveform displays or spectrograms to show:
Rate of syllable production
Consistency of intervals
Presence of irregularities or breakdowns
This approach is useful for:
Teaching self-monitoring
Making perceptual errors visible
Tracking progress over time
💡 Clinical Tip
The AMR should not sound like the SMR—if they do, it may indicate sequencing difficulty, particularly relevant in apraxia of speech.
Connected Speech Assessment: Incorporating Stress Testing, Intelligibility & Comprehensibility
🔍 Key Components of Connected Speech Assessment
🏋 Stress Testing (Evaluating Limits and Fatigue)
Purpose: To observe the resilience and sustainability of speech under increasing demand, which can reveal fatigue or weakness that doesn't appear in low-demand tasks.
Common Stress Tests:
Extended speech tasks (e.g. long sentences, paragraphs)
Sustained phonation or prolonged speech tasks
Rapid or complex sentence production (such as alternating complex phrases or word lists like "papa" or "peta" in rapid succession)
Conversational flow during continuous communication to see if endurance issues arise
🧠 Intelligibility (Speech Clarity and Understanding)
Purpose: To evaluate how well the client’s speech can be understood by others.
Articulation clarity: Are consonants and vowels accurately articulated?
Prosody and pacing: Does the individual use natural prosody (e.g., stress, rhythm) that helps with understanding?
Observed in Connected Speech:
Slurred articulation, imprecise consonants, or nasal emission may lower intelligibility.
Rapid speech with inconsistent stress patterns or imprecise articulation may cause speech to become less intelligible.
Stress Testing and Intelligibility:
Prolonged tasks or fatigue will often affect intelligibility. For example, during sustained speech tasks (e.g. telling a story continuously), fatigue may cause reduced articulation, leading to more unclear or indistinct speech.
💬 Comprehensibility (Overall Understanding)
Purpose: To assess how easily the message can be understood by a listener, despite potential speech clarity issues.
Verbal clarity combined with contextual cues such as gestures, facial expressions, and body language.
Observed in Connected Speech:
Gestures, facial expressions, and posture contribute significantly to comprehensibility, helping to convey meaning even if articulation is poor.
Well-structured sentences and strategies like circumlocution (explaining around unknown words) aid in comprehensibility, making the message clearer.
Intelligibility vs. Comprehensibility:
Intelligibility refers to the actual clarity of speech sounds, whereas comprehensibility involves the listener’s ability to grasp the overall message, even when speech sounds aren’t perfect.
A person with low intelligibility but high comprehensibility may struggle with clarity but can still communicate effectively through compensatory strategies like repetition, exaggerated gestures, or contextual clues.
🧩 Multimodal Communication
When assessing comprehensibility, consider how much non-verbal communication is used:
Facial expressions, gestures, posture, and eye contact all support the message.
These compensatory strategies can offset difficulties with intelligibility, enabling effective communicationeven when speech is impaired.
📽 Why Recording Helps
Recordings allow detailed analysis of both verbal and non-verbal communication.
This includes intelligibility of speech as well as how well the context (non-verbal cues) helps with comprehensibility.
For example, a client with poor intelligibility might still communicate well by using strong contextual speech, gestures, or facial expressions to clarify meaning.
🎯 Practical Application: Analyzing Speech and Communication Effectively
Stress testing will help identify how intelligibility changes under fatigue or extended speaking tasks.
Contextual speech (e.g. personal conversation or storytelling) will give you insight into how the client uses compensatory strategies to make themselves understood, regardless of the clarity of their speech.
Intelligibility and comprehensibility should be considered together, as clients with low intelligibility may still have high comprehensibility through the use of additional communication strategies.
Connected Speech Assessment and Multimodal Communication
🔍 Beyond Speech Output Alone
In connected speech, we assess more than just how speech sounds. We're also looking at how the person communicatesusing all available strategies.
🧩 Key Components of Connected Speech Assessment
Verbal Output:
Articulation clarity
Intelligibility in natural flow
Prosody (intonation, pitch, rhythm, rate)
Pause patterns and fluency
Multimodal Communication:
Facial expressions
Gestures
Body language and posture
Pointing, drawing, writing
Use of visual aids or augmentative tools
Message Effectiveness:
Does the person successfully convey ideas?
Are they understood despite speech impairment?
📽 Why Recording Helps
With permission, recordings allow for:
Later analysis of speech and non-verbal cues
Review by team members (SLT, OT, family)
Capturing spontaneous compensatory behaviours
💡 Example: A Person with Low Intelligibility but High Understandability
A client may:
Have slurred or imprecise articulation, making individual words hard to catch
But still be understood due to strong gestures, facial cues, and structured topic delivery
Demonstrate effective message formatting, even with reduced verbal clarity
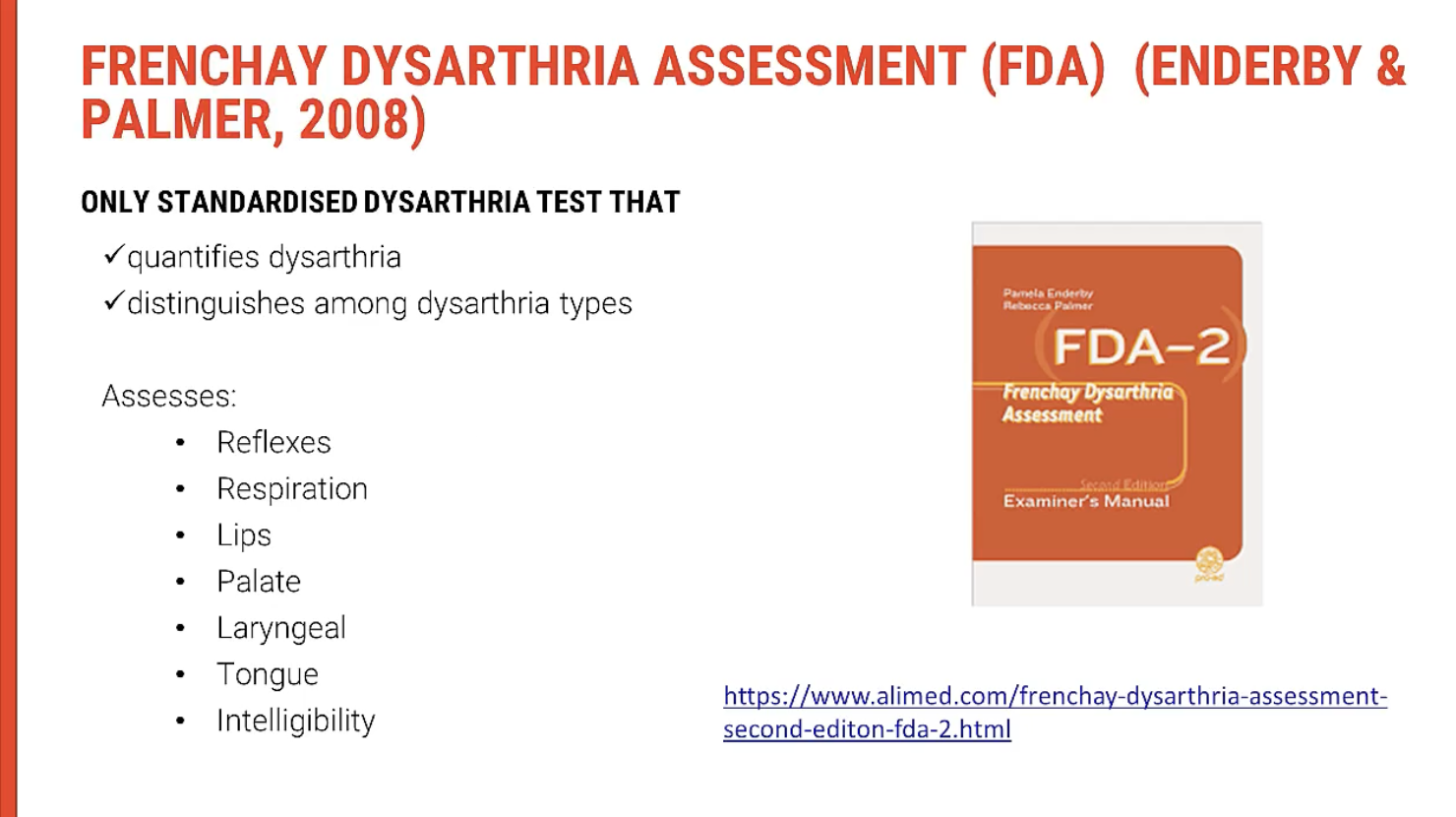
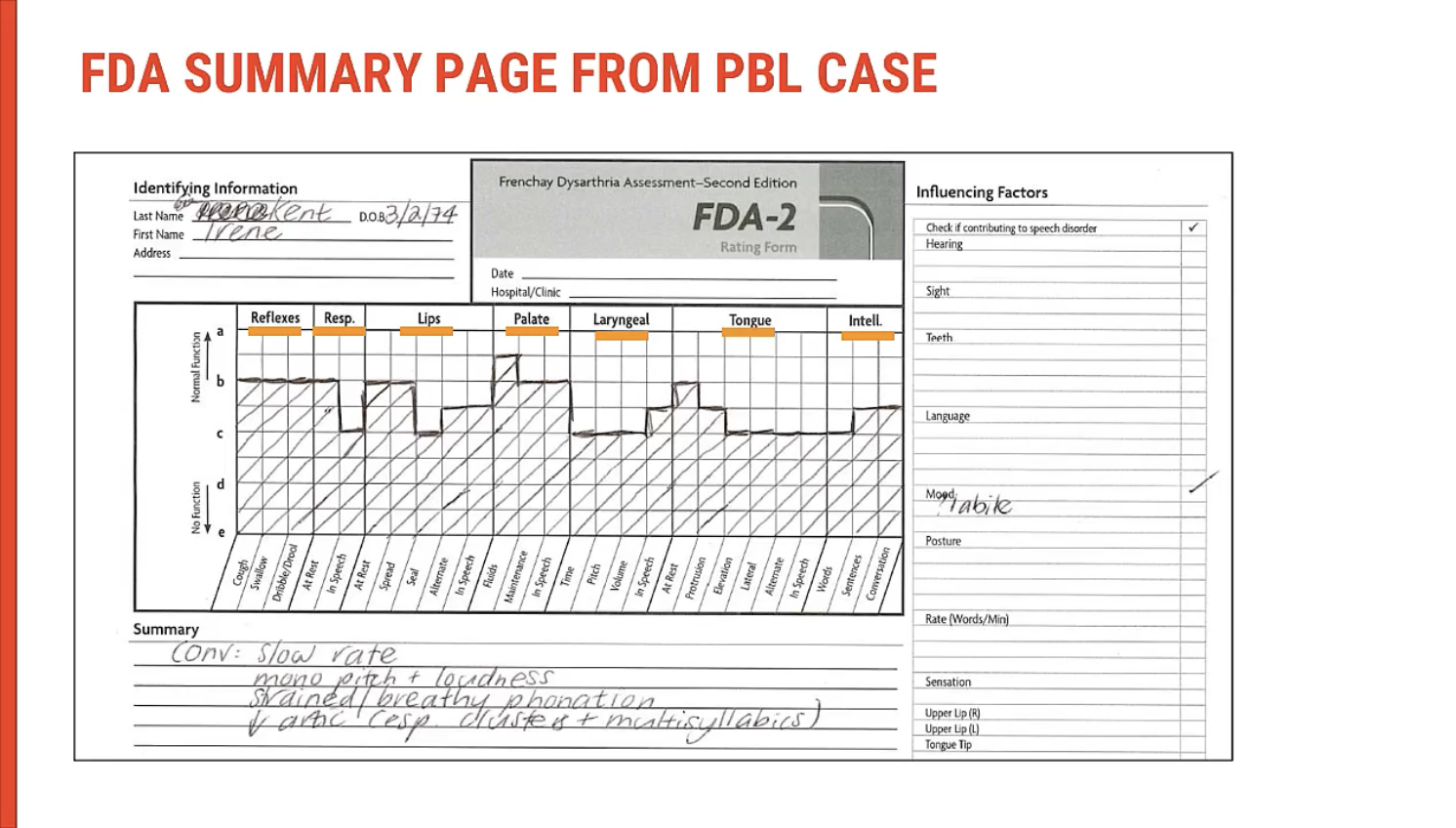
Overview of the Frenchay Test
The Franchises Offer is commonly used in Australian hospitals and community health centres for dysarthria assessment. It provides a standardised tool to evaluate speech and communication functions in a structured manner. The test incorporates extended oral examination and focuses on multiple speech subsystems, including respiration, phonation, resonance, articulation, and prosody. It also considers reflexes, such as swallowing and coughing, and the ability to perform essential movements related to speech production.
🧠 Key Components of the Franchises Offer Test
🫁 Respiration & Phonation
Respiratory Function: Evaluates breath control, ability to generate sufficient airflow for speech, and endurance.
Resting Rates & Cough Reflex: Assesses cough strength, indicating respiratory health and phonation ability.
Sustained Phonation Tasks: Measures the ability to sustain sound production, indicating lung and laryngeal health.
🎤 Articulation & Resonance
Lip Function & Sealing: Assesses the ability to form a seal with lips, important for producing certain speech sounds.
Lip Movement & Strength: Ability to protrude and retract lips for articulation.
Tongue Movement: Assesses tongue agility and range for speech production.
Lateral and Vertical Movements: Ensures proper tongue positioning for clear articulation.
🗣 Intelligibility Assessment
Word-level Intelligibility: Assesses how well individual words are understood.
Sentence-level Intelligibility: Evaluates the clarity and accuracy of full sentences.
Conversational Intelligibility: Measures the overall ability to communicate during a natural conversation.
⚖ Additional Factors Considered
Hearing: Evaluates the impact of hearing loss on speech production and intelligibility.
Vision: Assesses how visual impairments may affect communication strategies.
Dentition: Looks at how dental issues (e.g., missing teeth) may affect articulation.
Posture & Sensation: Assesses posture and how it influences speech production, particularly the movement of the head, neck, and facial muscles.
📝 Evaluation Criteria
The Franchises Offer evaluates:
Resting Speech Patterns: Resting rates and muscle control.
Intentional Movement: During voluntary actions such as swallowing, sucking, and lip protrusion.
Speech Tasks: Includes simulation of everyday conversational scenarios for real-world applicability.
🔄 Why This Assessment is Key
The Franchises Offer provides an in-depth analysis of multiple speech subsystems, enabling clinicians to understand the functional limitations and compensatory strategies a client may use.
By integrating intelligibility measures with motor assessments, this tool gives a comprehensive view of a patient's speech capabilities and limitations across several speech modalities.
Assessment Process for Dysarthria: Managing Client Fatigue
🧠 Assessment Process for Dysarthria: Managing Client Fatigue
🕰 Multiple Sessions for Comprehensive Assessment
Assessing dysarthria can be taxing for the client, especially if the presentation is more complex or involves multiple systems. To ensure accurate and manageable assessment, testing may be broken down into multiple sessions. This can help reduce fatigue and improve client cooperation, allowing for more detailed observations across speech subsystems.
🏋♂️ Strengths and Weaknesses Identification
The goal of testing is to identify strengths and weaknesses in the client's speech systems:
Stronger Areas: These will generally fall within the 80% range or higher, reflecting normal function or minimal impairment in specific subsystems.
Weaker Areas: Subsystems showing reduced function or less than 80% performance indicate areas requiring further attention or therapy focus.
🧠 Testing Components Breakdown
🎤 Speech Motor Tasks
Testing involves various speech motor tasks to assess articulation, respiration, phonation, and prosody. Clients may struggle with:
Consonant Precision: Difficulty articulating specific consonants clearly.
Breathing Coordination: Issues coordinating breath with speech production, leading to breathy or strained voice.
💡 Cognitive and Emotional Aspects
In addition to physical aspects, clinicians should consider emotional factors that may affect speech:
Emotional Lability: Difficulty controlling emotions during speech.
General Speech Fluency: Changes in pitch, loudness, or rate may be connected to underlying emotional challenges, not just motor function.
Fatigue: Clients may show inconsistent performance due to fatigue, especially during longer tasks.
📊 Documenting Client Progress
In the next sessions, document progress in strengths and weaknesses:
Resilient Areas: Can be acknowledged as areas of strength or mild difficulty.
Progress Monitoring: Track improvements over time to assess the effectiveness of therapy and adapt the treatment approach accordingly.