Acquired Optic Nerve Disorders
1/103
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
104 Terms
What is optic nerve head drusen?
Globular, hyaline bodies of degenerative axonal byproducts containing calcium located within the optic nerve head (anterior optic nerve)
What happens when optic nerve head drusen progresses?
Progressive: calcification and growth, migration anteriorly
+/- Compression of RNFL leading to glaucoma-like damage
What causes optic nerve head drusen?
Unknown or hereditary

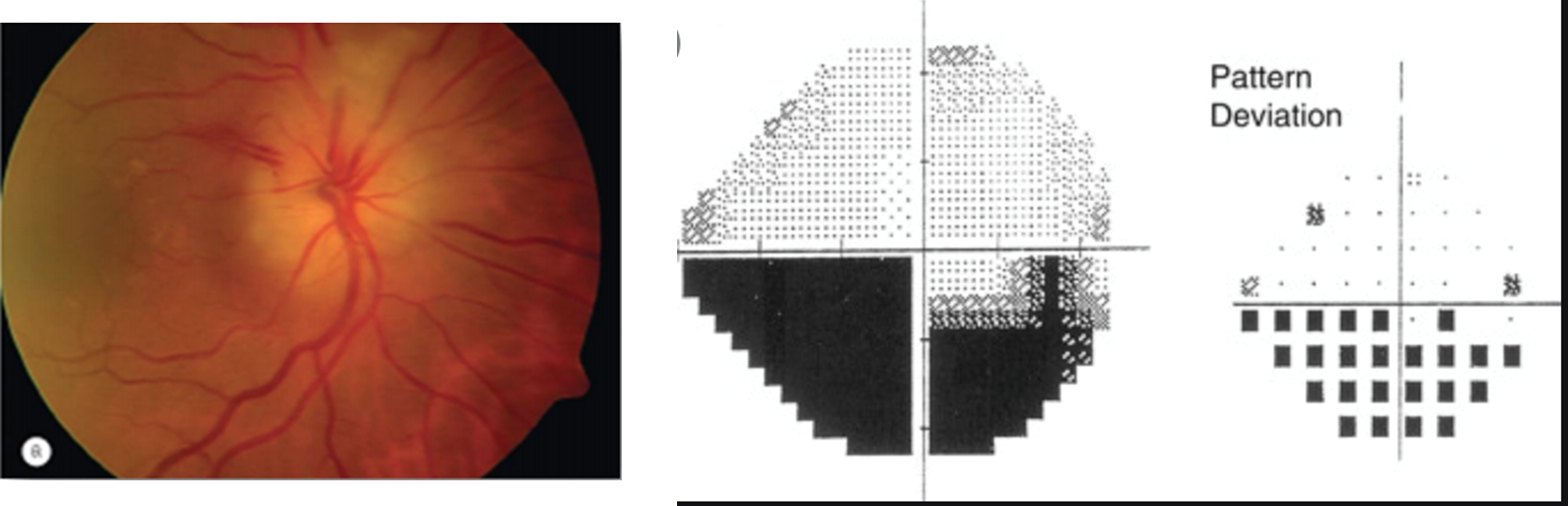
What are the signs of optic nerve head drusen?
Bilateral 75%, asymmetric
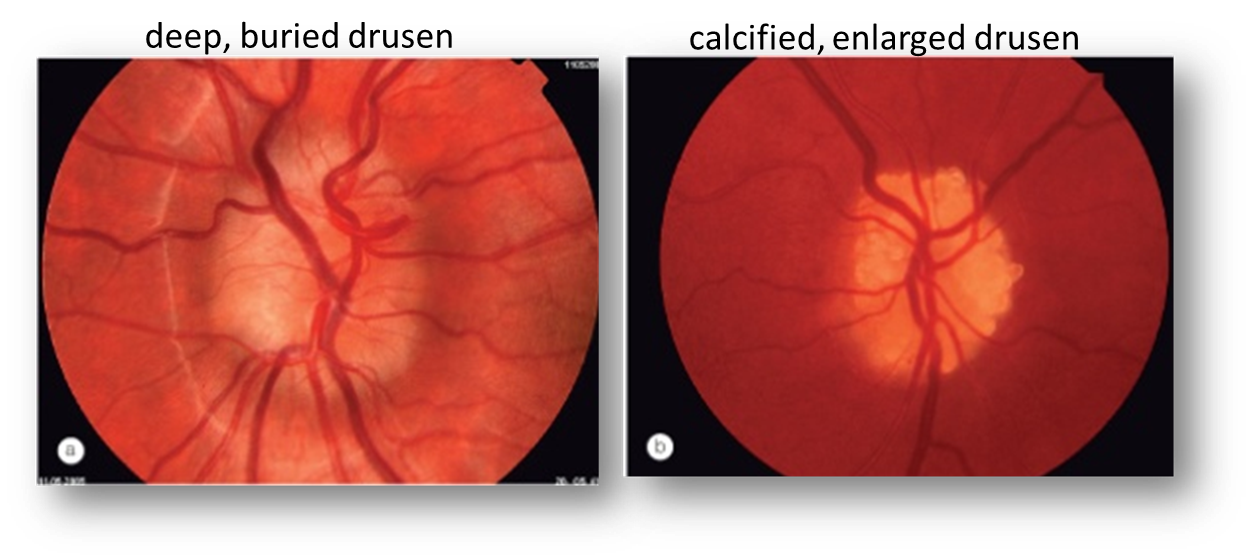
Overt (superficial, calcified, enlarged) vs. Covert (deep, buried)
Scalloped, "lumpy-bumpy" appearance at disc margin
Obscuration of cup (crowded disc)
Pseudopapilledema (blurred, elevated disc margins)
+/- angioid streaks
+/- disc hemorrhages, ischemic optic neuropathy
What are the symptoms of ONH drusen?
Asymptomatic (especially with deep, buried drusen)
Transient visual obscurations (TVO) or dimming of vision (due to compression of RNFL
Visual field defects (subjectively still may be asymptomatic; enlarged blindspot, generalized constriction, less commonly arcuate defects)
What is the management of ONH drusen?
No treatment currently
Patient education and routine testing
What testing should be done to evaluate ONH drusen?
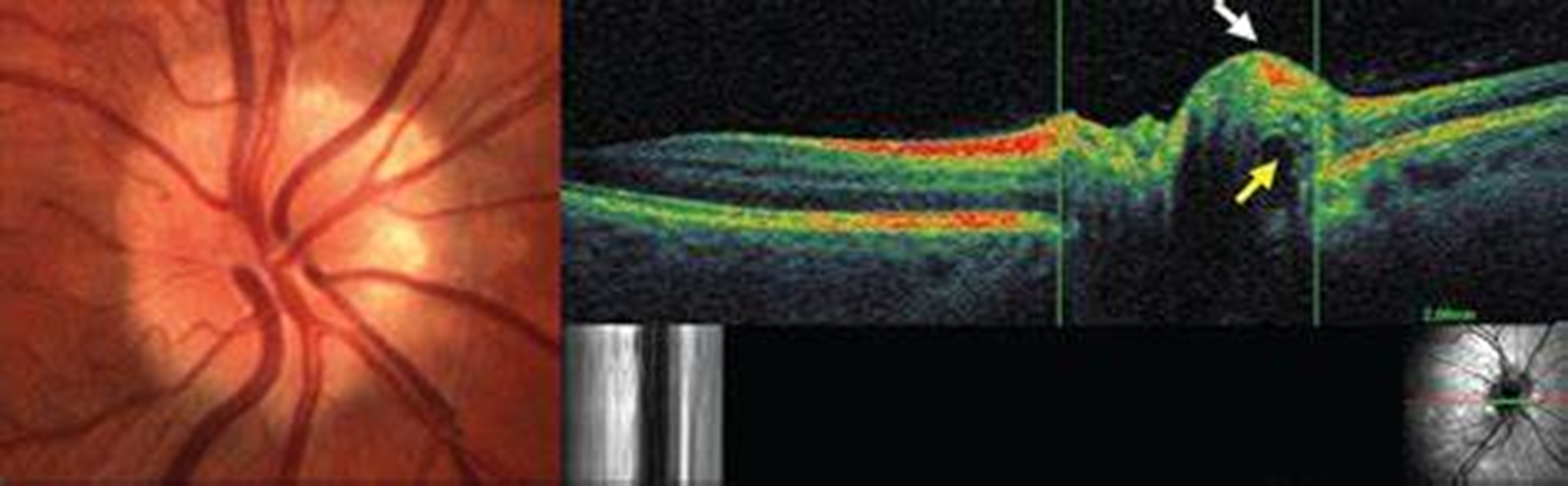
OCT
What to Order
EDI (enhanced depth imaging)
ONH radial
Neuroretinal rim RNFL
Peripapillary RNFL
Macular GCL
FAF
B-scan ultrasound
IVFA (rarely ordered)
CT
Why is it important to use EDI to observe ONH drusen?
Allows you to focus behind dense structures setting otherwise will be unable to differentiate from blood vessels
What do you expect to see on OCT with ONH drusen?
Hyperreflective, spherical/irregular anterior border with internal hyporeflective core
Adjacent NRR RNFL and cpRNFL scan can detect RNFL loss/changes
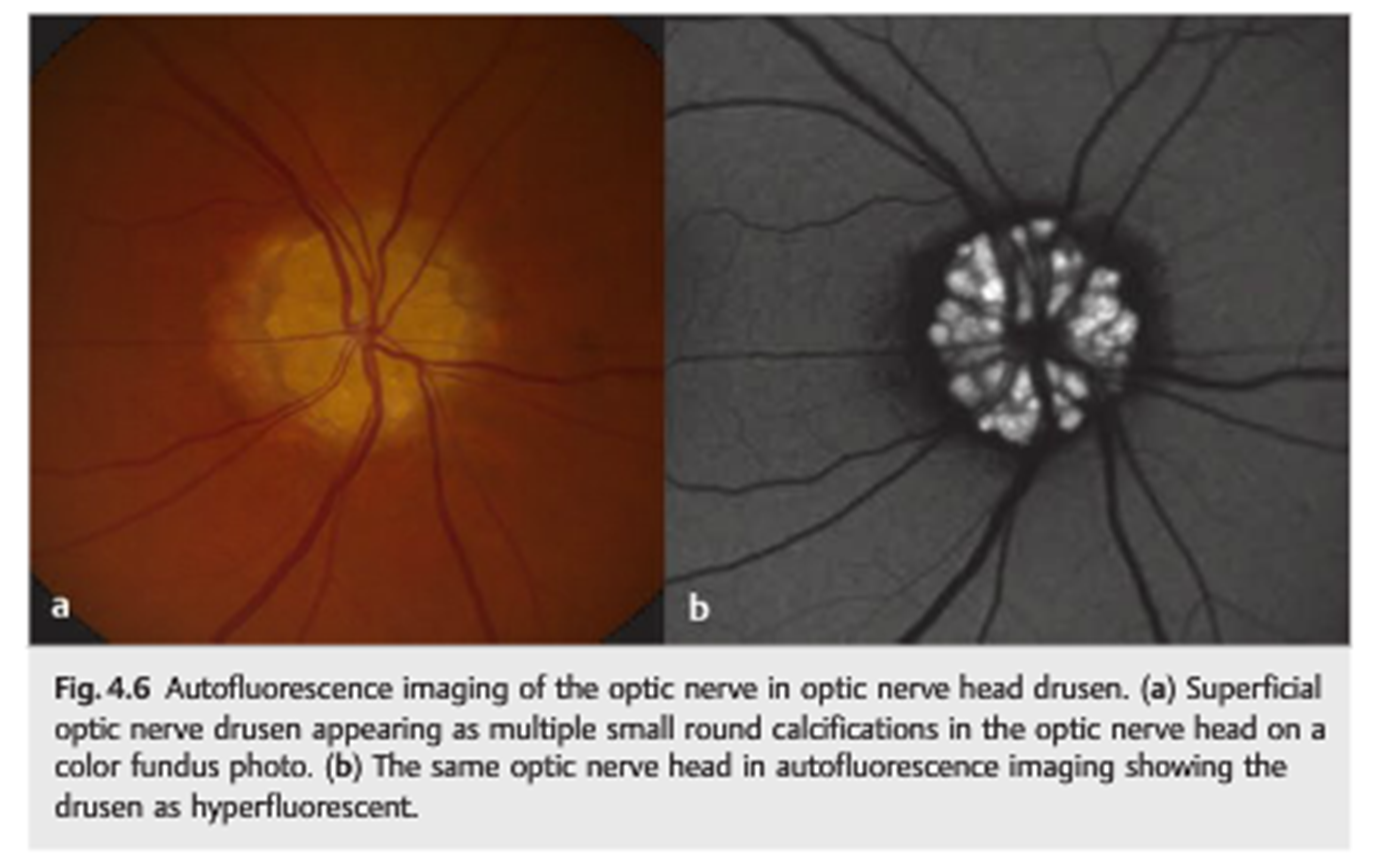
What do you expect to see on FAF with ONH drusen?
Only superficial/overt calcified drusen will hyperautofluoresce
If too deep, you will not be able to view on FAF
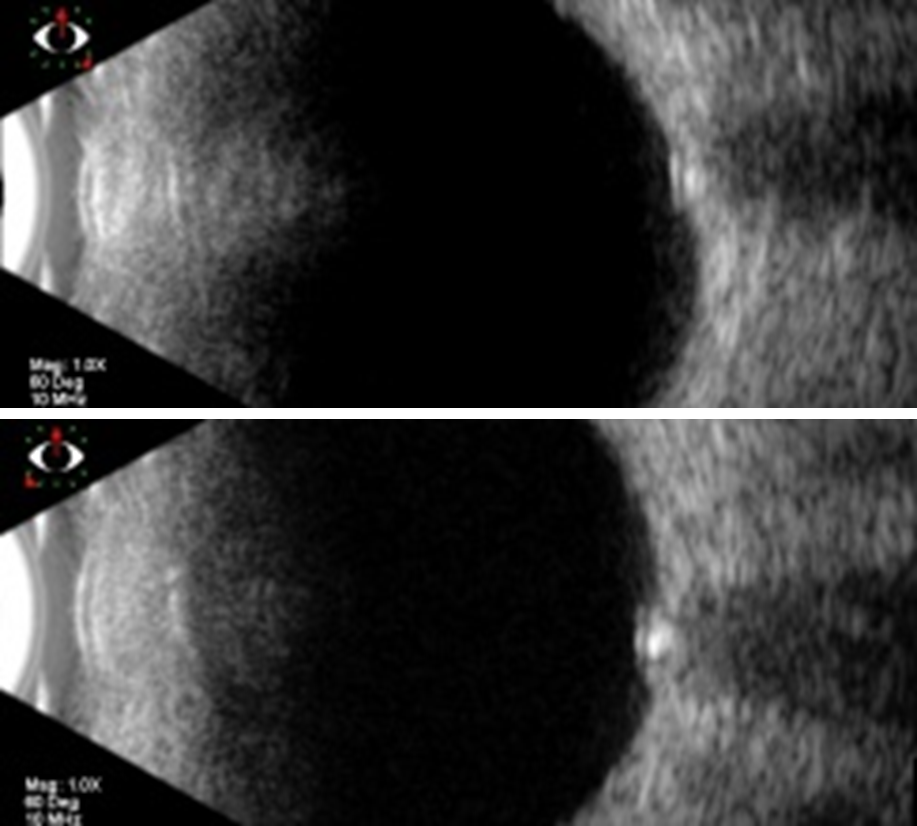
What do you expect to see on B scan with ONH drusen?
Only calcified drusen will be observable
Must be on low gain setting to see the intense signal of the calcified drusen at the ONH
What would you expect to see on IVFA with drusen?
Would not typically order for ONHD
Early diffuse hyperfluorescence, NO late leakage like seen with ONH edema
What would you expect to see on CT with ONH drusen?
Would not typically order for ONHD
Will be hyperreflective if calcified
What is optic nerve edema?
Swelling of the optic nerve
What are the 2 types of optic nerve edema?
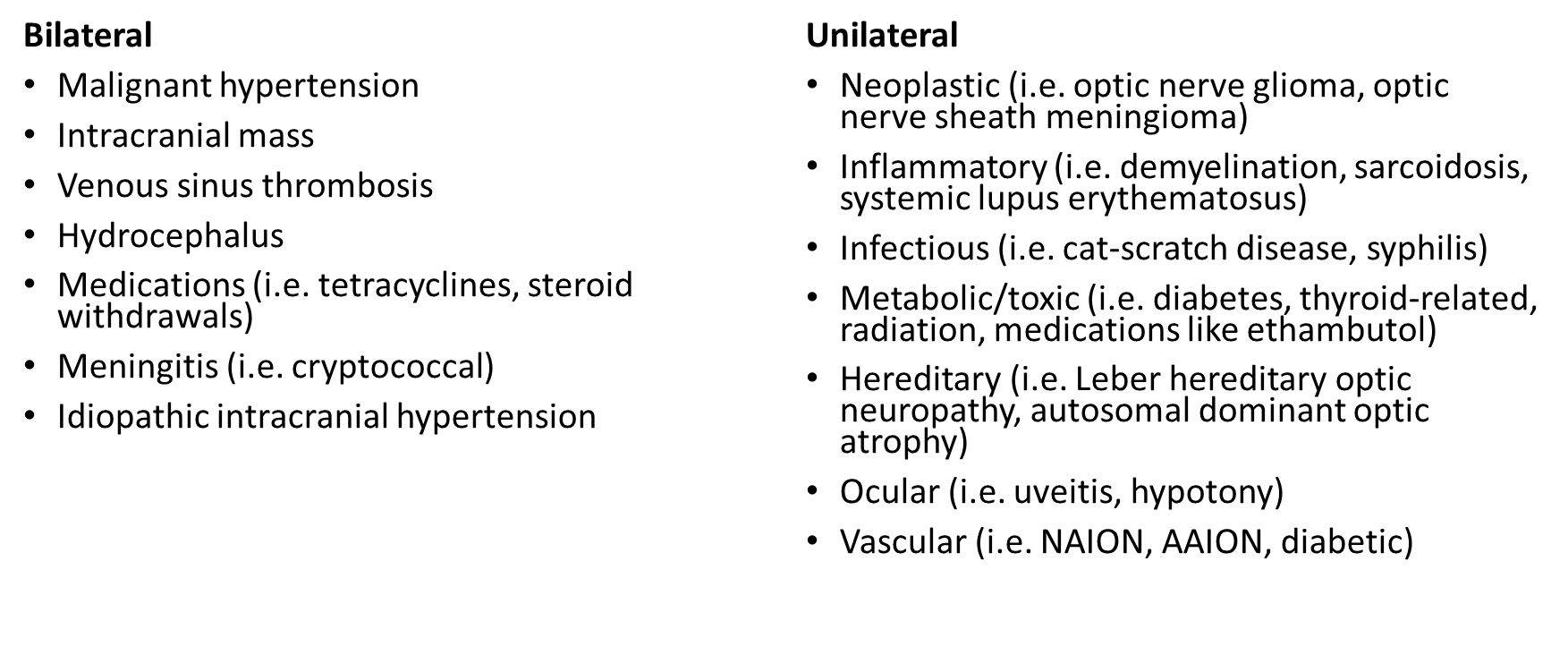
Papillitis (unilateral) and papilledema (bilateral)
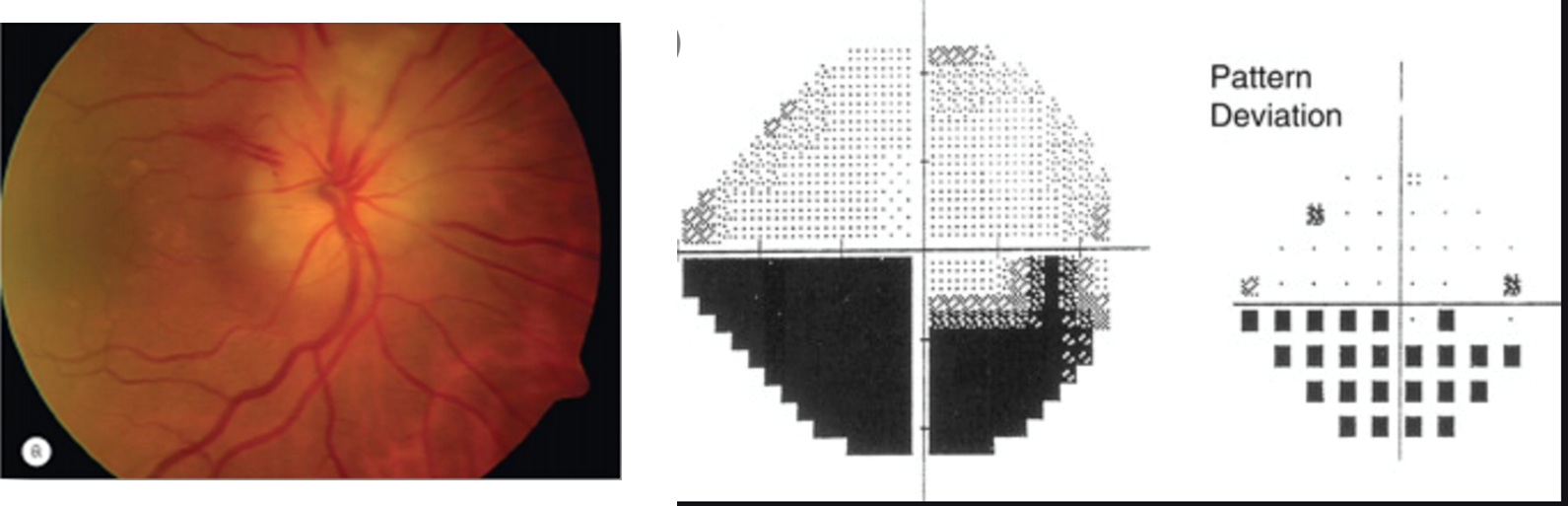
What are the causes of optic nerve edema (bilateral and unilateral?
What are the workup considerations for optic nerve edema?
Vital signs
Blood pressure
Pulse
Height
Weight
BMI
Complaint
Transient visual obscurations (especially with Valsalva or postural changes)
Health history
Current or new medications
Review of systems (When we see nerve edema, don't just refer straight to neuro - take these other conditions into considerations to manage/refer appropriately)
Recent headaches
Recent weight gain
Infectious concern: recent tick bites, rashes, upper respiratory symptoms, gastroenteritis symptoms, new exposure to cats, sexually transmitted diseases
Inflammatory concern: jaw claudication, scalp tenderness, weight loss, arthralgias, myalgias, malaise
Demyelinating concern: numbness, tingling, daytime somnolence, intractable nausea, vomiting, hiccups
Entrance tests
See optic nerve disease diagnostic testing (page 1)
Fundoscopy
Diagnostic testing - OCT, Visual Field, Fundus photos, FAF, IVFA
OCT
Consider ONH radial, NRR RNFL thickness, cp RNFL thickness, m GCL thickness
Consider 30-2, 24-2, 24-2C, or 10-2
May observe: full field, enlarged blindspot, nasal step, arcuate defect, constriction 360, or paracentral defect
Lab testing
Brain imaging
What type of lab testing would you consider with optic nerve edema?
CBC
Heavy metals
B12
Folate
FTA-ABS
VDRL
ANA
Homocysteine
ACE
Antiphospholipid antibodies
TORCH panel
What type of brain imaging would you order for optic nerve edema?
CT
MRI
MRV
What is papilledema?
Bilateral disc swelling secondary to increased ICP (intracranial pressure) or CSF (cerebrospinal fluid) pressure - differentiates from optic nerve edema
What is the cause of papilledema?
Increased ICP (intracranial pressure) or CSF (cerebrospinal fluid) pressure
What is normal ICP?
Normal ICP: <250mm H2O in adults, <280mm H2O in children
What are causes of increased ICP?
Brain tumor (compressive lesion)
CNS inflammation (hydrocephalus, meningitis, etc.)
Ventricular obstruction
Cerebral venous thrombosis (blood clot in the brain's venous sinuses)
Idiopathic intracranial hypertension/ IIH (most common cause of papilledema)
Mostly an ocular finding - neurology typically relies on this finding to help them diagnose
What are the signs of papilledema?
Bilateral (can be asymmetric)
Loss of SVP (ties back to earlier lecture) - increased ICP or OPP
Optic nerve head
RNFL opacification
Elevation of margins
Hyperemia
Obliteration of cup
Obscuration of small blood vessels at disc margin
Vascular congestion
Venous dilation
Vascular tortuosity
Hemorrhages
Cotton wool spots
Exudates
Mechanical features
Retinal folds (Paton's lines: peripapillary RNFL ripples)
Choroidal folds (posterior globe deformation, extreme)
Chronic papilledema
Rim pallor
Gliosis (greying of RNFL due to scarring)
Optociliary shunts
Refractile bodies
What is 0 on the Frisen scale for grading papilledema?
Normal Optic Disc or Pseudopapilledema
Prominence of the RNFL
Possibly some nasal blurring from smaller discs
What is Grade 1 on Frisen scale?
C shaped halo (typically nasal first)
What is Grade 2 on Frisen scale?
Circumferential blurred margins
What is Grade 3 on Frisen scale?
Obscuration of blood vessels (big difference between Stage 2) due to axon edema surrounding vessel in at least one segment
What is Grade 4 on Frisen scale?
Marked Degree of Edema
Elevation of entire nerve and inability to see margins
What is Grade 5 on Frisen scale?
Obscuration of al vessels of the disc and obvious protrusing of dome shape
What is IIH?
Increased ICP of unknown cause that predominantly affects obese females of childbearing age
What are medication associations with IIH?
Tetracyclines, vitamin A, lithium, anabolic steroids, oral contraceptive pills, nalidixic acid, cyclosporine
What are some systemic illness associations with IIH?
Obstructive sleep apnea, hypothyroidism, anemia, Addison disease, systemic lupus erythematosus, Behcet's syndrome, polycystic ovary syndrome, coagulation disorders, uremia
What are symptoms of IIH?
HA (most common): diffuse, non-specific; may be associated with vomiting; +/- retrobulbar pain/pressure
Also worse with Valsalva maneuver or postural changes
Transient episodes of vision loss/blurring out: lasts seconds, associated with Valsalva maneuver or postural changes
Pulsatile tinnitus: unilateral 'whooshing' sound exacerbated with postural change
Turbulent venous system pulsations from increased ICP
Visual disturbance: peripheral field defects
Horizontal diplopia: associated with unilateral or bilateral 6th cranial nerve palsy
What is the management for IIH?
Diagnostic LP may provide transient symptomatic relief
Weight loss (goal of 5-10% of body weight) provides long-term relief
Oral CAIs provide short-term relief - reduce rate of CSF production
Acetazolamide (Diamox) 500mg BID, less dose can be considered
topiramate (Topamax), weaker effect
Surgery for refractory cases
Optic nerve sheath fenestration
CSF shunt (LP or VP)
What is the prognosis for IIH?
Can last weeks to years with variable outcomes
Optic atrophy (permanent vision and field loss) especially without treatment
What testing should be done for IIH?
OCT
OCT ONH- radial with enhanced depth imaging (R/O disc drusen)
OCT ONH - rim RNFL and CP RNFL thickness
OCT Mac - GCL thickness
HVF - 24-2C or 30-2 and/or 10-2
Photo - posterior pole (baseline)
MRI (Magnetic Resonance Imaging) - ordered once you've determined cause is not drusen-related or pseudo-papilledema
Preferably gadolinium-enhanced (contrast medium/metal solution), fat-suppressed
MRV (Magnetic Resonance Venography)
Absence of venous sinus thrombosis
Best way to diagnose Cerebral venous thrombosis
Lumbar puncture/spinal tap
Detects opening pressure of CSF + retrieval of sample of CSF to send to lab for analysis (inflammation/infection/tumor cells)
What is the best way to diagnose cerebral venous thrombosis?
MRV
When is a lumbar puncture typically ordered?
Ordered if MRI and MRV is unremarkable to get CSF sample
Why is it important to order MRI before LP?
Procedure is contraindicated if risk of herniation (i.e. Chiari malformation seen on MRI - brain extends lower than usual)
Important to run MRI before performing LP
Slight release of pressure from LP can drop the brain and crush the spinal cord
Ordered if the MRI and MRV comes back unremarkable
What opening pressure is diagnostic for IIH?
Opening pressure > 25 cm
T or F: IIH patients will have normal CSF composition
True
What the 5 criteria in Modified Dandy criteria?
Signs and symptoms of increased ICP (papilledema, headaches, TVOs)
Normal neurological exam except for cranial nerve abnormalities
Normal neuroimaging (no evidence of hydrocephalus, mass, structural or vascular lesion and no abnormal meningeal enhancement on MRI)
Normal CSF composition
Elevated lumbar puncture opening pressure (>25 cm H2O adults)
What is definite IIH?
All Dandy criteria met
What is probable IIH?
At least 4 criteria met (with papilledema being one of them)
What is optic neuritis?
Inflammation of the optic nerve
What are the etiologies of optic neuritis?
Demyelinating (most common)
Para-infectious (resolved infection)
Infectious (active)
Non-infectious (autoimmune)
T or F: Once ICP returns to normal, horizontal diplopia will resolve
True
What are the locations of optic neuritis?
Retrobulbar
ONH appears normal (although pallor can appear later)
Commonly associated with multiple sclerosis (demyelinating)
Papillitis
Swollen, hyperemic appearing ONH
Neuroretinitis
Papillitis with retinal inflammation (i.e. circinate exudates)
Often has circinate exudates
What are the signs and symptoms of optic neuritis?
Acute, painful unilateral (although can be bilateral) vision loss
Periorbital pain, worsened with eye movements
+/- RAPD (if severe unilateral or highly asymmetric)
+/- decreased VA, VF, color vision
+/- optic nerve swelling (may be retrobulbar)
What is demyelinating optic neuritis?
Immune-mediated inflammatory demyelination of the optic nerve
What is the most common type of optic neuritis?
Demyelinating
What is demyelinating optic neuritis often associated with?
MS
What are the signs of demyelinating optic neuritis?
Acute, painful unilateral (although can be bilateral) vision loss
Periorbital pain, worsened with eye movements
+/- RAPD (if severe unilateral or highly asymmetric)
+/- decreased VA, VF, color vision
+/- optic nerve swelling (may be retrobulbar)
What are the symptoms of demyelinating optic neuritis?
Prodromal viral illness
Photopsias/phosphenes
Uhthoff phenomenon 🌡: blurry vision when body temperature rises (I.e. exercise or bathing)
Pulfrich phenomenon: altered perception of motion/2D images appear 3D due to delayed impulse from one affected optic nerve
What is used to diagnose demyelinating optic neuritis?
OCT (signs of optic nerve edema unless retrobulbar)
Serologic testing and CSF analysis (to rule out other causes)
MRI of brain and orbit with gadolinium (may eliminate other causes and high prognostic value for MS)
What is the study ONTT tell us?
Comparing treatments: oral prednisone vs. IV methylprednisolone followed by oral prednisone vs. Placebo
Faster recovery - IV methylprednisolone followed by oral prednisone sped recovery by two weeks and delayed neurological signs/symptoms of MS by 2 years
At 6 months, visual recover was the same for all 3 groups (87% 20/25 or better)
What is the percentage of MS patients that have asymptomatic white matter lesions?
72%
What are the causes of para-infectious optic neuritis?
Viral
After immunization/vaccines (1-3 weeks)
What are the causes of infectious optic neuritis?
Sinus-related
Cat-scratch disease
Untreated syphilis
Lyme disease
Cryptococcal meningitis
Varicella zoster virus
What is neuroretinitis?
Inflammation of neural retina and optic nerve, commonly involving circinate exudates and optic nerve edema
Neuroretinitis
What are the etiologies of neuroretinitis?
Infectious or para-infectious
Hypertension grade 4 retinopathy
Idiopathic (5%)
What is the prognosis of neuroretinitis?
Typically resolves spontaneously
Cause needs to be addressed
What are the etiologies of autoimmune optic neuritis?
Sarcoid disease (granulomatous inflammatory disease)
Sjogren syndrome
Systemic lupus erythematosus (SLE)
Rheumatoid arthritis (RA)
Inflammatory bowel disease (IBD)
Neuromyelitis optica
What is diabetic papillitis?
Rare ocular manifestation of diabetes
What are the etiologies of diabetic papillitis?
Potentially due to rapid glycemic control
Questionable if this is a form of NAION or malignant hypertension if other vascular issues exist
Diagnosis of exclusion (rule out other causes)
What is the laterality of diabetic papillitis?
Unilateral optic nerve edema
What is the presentation of diabetic papillitis?
Unilateral, painless vision loss with DR and DME typically present
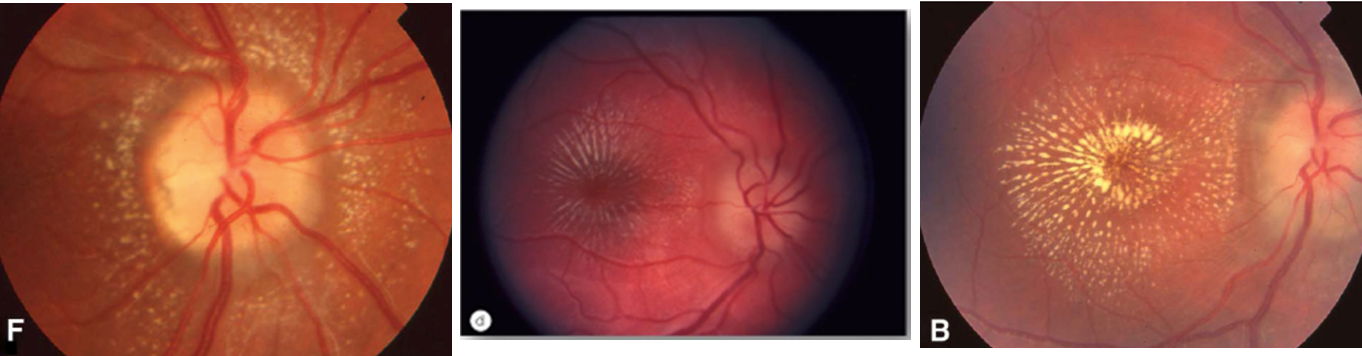
What is NAION?
Non-arteritic anterior ischemic optic neuropathy
Occlusion of short posterior ciliary arterials (partial or total)
What is the average age of onset of NAION?
40-60 YOA
What are the risk factors of NAION?
Poorly controlled vascular disease (hypertension, diabetes, hypercholesteremia)
Hypotensive event (typically during nocturnal hypotension)
Sleep apnea
Medications (I.e. amiodarone, PDE-5 inhibitors)
"disc at risk": small-sized optic disc with crowded rim tissue and minimal cup
What are the signs and symptoms?
Unilateral (rarely bilateral)
Painless (8-12% report headache or periocular pain)
Visual acuity varies (typically better than 20/200)
>2/3 of patients notice it upon wakening
Blurred margins or elevated margins/disc (diffuse or segmental)
Hyperemic appearance (rarely pale) - nerve looks more reddish in color NOT typically pale
Splinter hemorrhages (75% of patients) - superficial hemorrhages
Altitudinal field loss (common, especially inferior; 25% central scotomas) - either the top or bottom half
What is the Management for NAION?
No effective treatment
Discuss modifiable vascular risk factors
What is the prognosis for NAION?
Vision can worsen the first 2 weeks
Vision stabilizes by 2 months
50% of patients had VA 20/30 or better
Visual field defects can be permanent
Pallor (total or sectoral), cpRNFL/mGCL loss on OCT (total or sectoral)
Fellow eye involvement
15-24% in >5 years
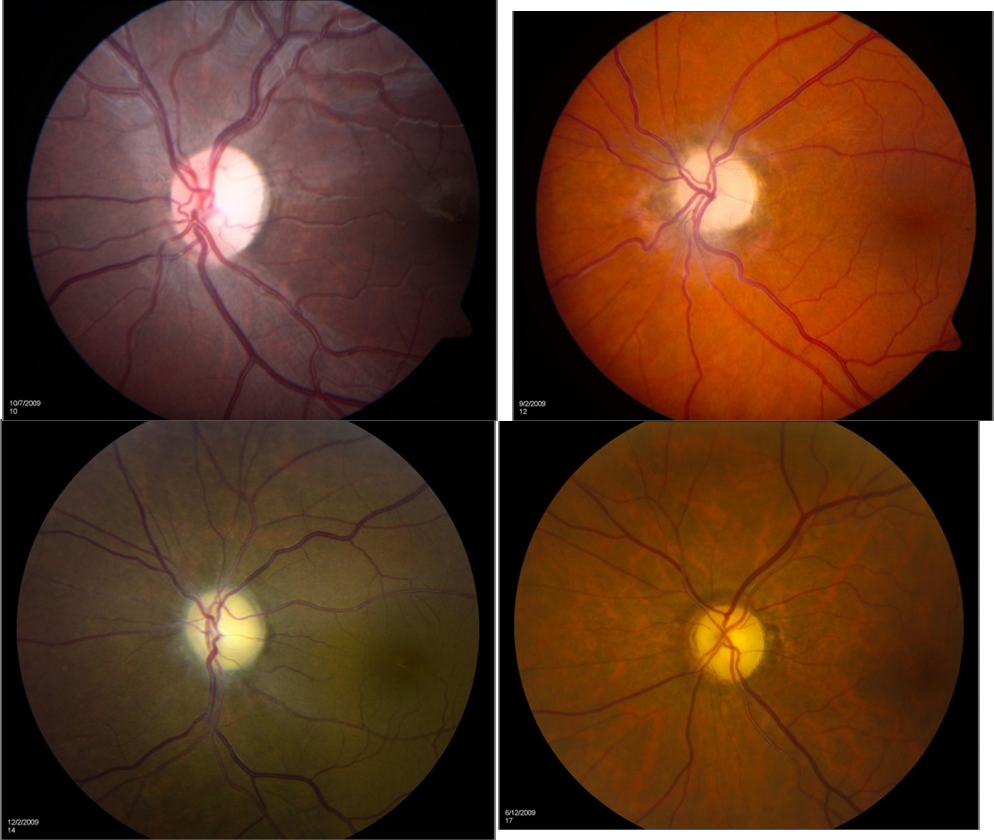
NAION
Margins are blurred with hyperemia (reddish) of rim | Inferior altitudinal defect on 24-2 with paracentral defect |
What is AAION?
Arteritic anterior ischemic optic neuropathy
Inflammation and thrombosis of short posterior ciliary arteries
What is the age group of AAION
> 50 YOA
Increasing incidence each decade
What are the most common causes of AAION?
Most commonly caused by giant cell arteritis (GCA), which is a form of vasculitis that most commonly affects the medium- to large-sized arteries in the temple (temporal arteritis)
1/3 to 1/2 of patients with GCA have polymyalgia rheumatica (PMR)
What are the signs and symptoms of AAION?
Acute, often painful, severe vision loss
BCVA typically worse than 20/200
Visual field defects, most commonly altitudinal
Headache (most common), tenderness of scalp/temple, jaw claudication - pain or fatigue when chewing (specific to GCA), malaise, loss of appetite, weight loss, fever, joint and muscle pain, ear pain
Chalky-white appearance of optic nerve, typically
+/- APD
Narrowed appearance of arteries around the nerve
What lab testing should be ordered for AAION?
Erythrocyte sedimentation rate (ESR) - general inflammation
Westergren method
Normal: males ≤ age / 2 females ≤ (age+10) / 2
C reactive protein (CRP) - acute inflammation
Normal < 5mg/L (studies vary)
*97% specificity for temporal arteritis when ESR and CRP are both elevated
Platelets (within CBC)
Normal: 150,000 – 400,000 /µL
Leukocytes?
Hemoglobin levels?
Normal: males: 13-17g/dL females: 11.5-15.5g/dL
What is normal for ESR?
Normal: males ≤ age / 2 females ≤ (age+10) / 2
What is normal for CRP?
Normal < 5mg/L (studies vary)
What is normal for platelet count?
Normal: 150,000 – 400,000 /µL
What diagnostic testing should be ordered for AAION?
Biopsy
Superficial temporal artery biopsy (TAB) (gold standard, although negative biopsy could still mean "skip lesions" are present)
Temporal artery ultrasound (superior alternative to biopsy but not widely available)
Dark wall swelling ("halo") and acute occlusions in active AAION
MRI?
During acute stage, optic nerve head enhancement with AAION but not NAION
What is the treatment for AAION?
IV methylprednisolone 1g/day for first three days, followed by oral prednisone 60-100mg/day; taper after several months or years
No long-term definitive studies to determine if this is the best line of treatment
Tocilizumab (FDA approved 2017 for GCA)
Monoclonal antibody
What is the prognosis for AAION?
Without treatment, 54-95% permanent vision loss within four months
With steroid treatment, 13% permanent vision loss
Untreated, other eye becomes involved in up to 50% of cases
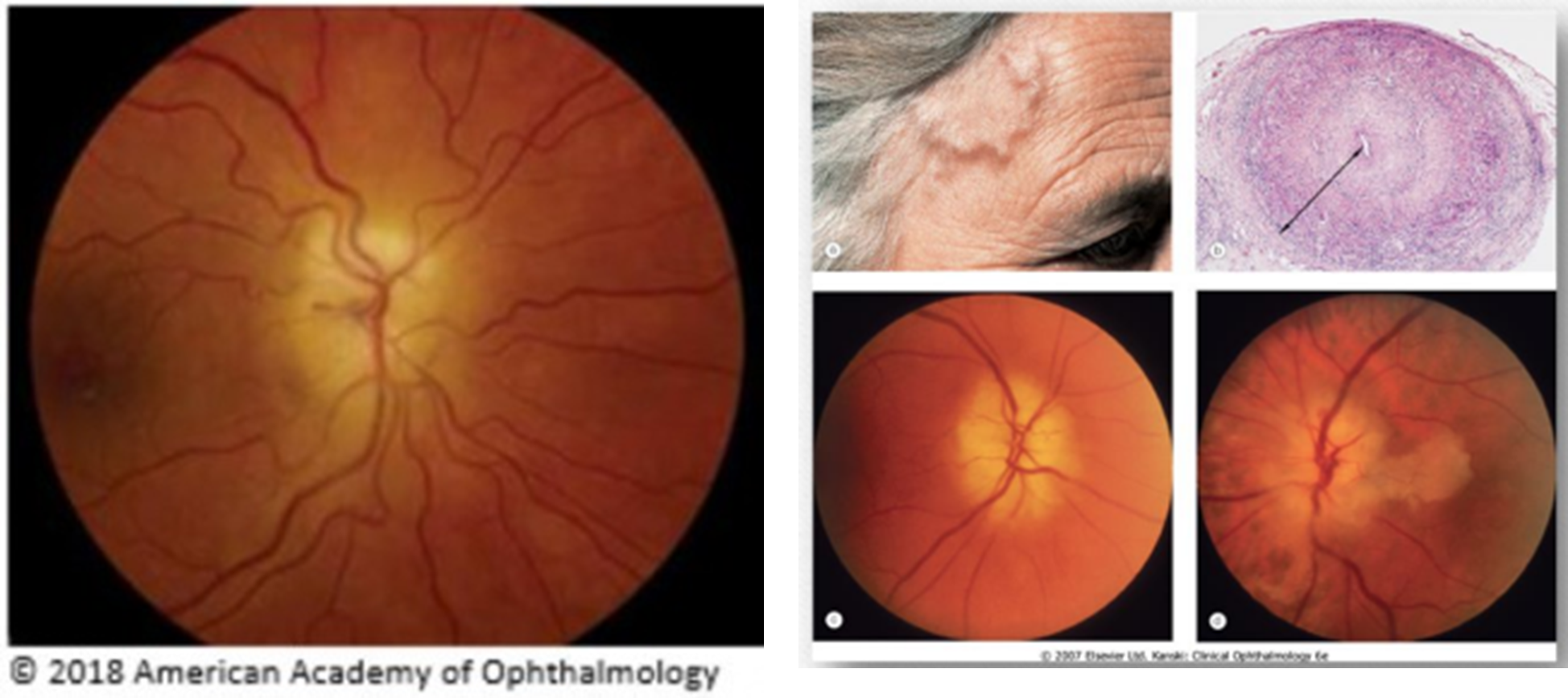
AAION
Optic Atrophy
Atrophy of the optic nerve
Possible end point for any of the optic nerve edematous conditions we've discussed
What is the presentation of optic atrophy?
Can be diffuse or sectoral, from insult
What are the findings of optic atrophy?
+/- Optic nerve pallor
Total
Sectoral
Altitudinal
OCT correlation
NRR RNFL thinning
cp RNFL thinning
mGCL atrophy
What are the symptoms of optic nerve atrophy?
VA and VF correlation
Possibly APD (if asymmetric damage)
What are the etiologies of optic atrophy?
Chronic papilledema/optic nerve edema
Optic neuropathy
Optic neuritis
Tumor (compressive)
Trauma
Cerebrovascular events/Strokes
CVA that affects any part of the visual pathway can cause visual field defects that correspond to thinning on the OCT (RNFL or GCL)
Neurodegenerative disorder
Studies on Alzheimers shows thinning of RNFL on OCT
Toxic or nutritional
I.e. alcohol overuse or vitamin B complex deficiency can lead to bitemporal pallor of the optic nerve head, leading to loss of visual acuity and/or a centrocecal scotoma
Congenital (mitochondrial)/childhood disorder
Leber Hereditary Optic Neuropathy
Autosomal Dominant Optic Atrophy
Optic Atrophy
What two conditions can cause painful vision loss?
Optic neuritis and AAION
How would you describe the typically visual field defects you would see with NAION and AAION
Altitudinal