Dermatology Medicine Exam 2
1/43
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
44 Terms

Rosacea
Causes
Chronic inflammatory skin disorder
Unknown etiology
Manifestation
Gradual onset with flares and remission
Cardinal features
Flushing/edema
Chronic centrofacial redness
Papules and pustules with absence of comedones
Telangiectasis
Phymatous changes: disfiguring tissue hypertrophy of the face, sebaceous glands, and nose (usually have rhinophyma in males)
Ocular involvement
Location: face (most commonly nose and cheeks)
Triggers (cause a temporary increase in redness)
Spicy foods
Hot beverages
Alcohol
Sun and wind exposure
Extreme temperatures
Exercise
Emotion/stress
Drugs: vasodilators, topical steroids
Associated diseases: GI diseases (celiac), autoimmune, HTN, CAD, some malignancies
Diagnosis
Clinical
May do blood work to make sure it is not Lupus
Treatment
No cure
Treatment goal → suppression
Avoid triggers and irritating topical products
Emollients
Mild-moderate → metronidazole, azelaic acid, ivermectin (has potent anti-inflammatory properties)
Moderate-severe or refractory → Doxycycline or Minocycline
Triple cream
No topical steroids or oral steroids → can cause steroid acne
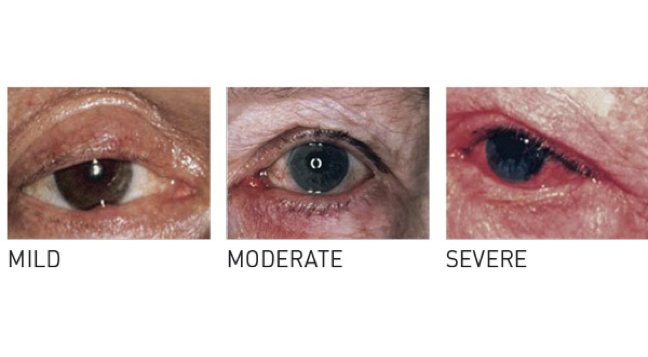
Ocular Rosacea
Causes
Seen in >50% of patients with rosacea (may precede skin lesions in 20%)
Manifestation
Ocular manifestation
Conjunctivitis with soreness, foreign body sensation, burning, or grittiness
Decreased lacrimation
Telangiectasis of lids, blepharitis, and chalazion
Treatment
Topical metronidazole to lids
Oral doxycycline
Warm compresses
Artificial tears

Perioral Dermatitis
Causes
Etiology unknown
Can follow long term topical steroids
Manifestation
Papulopustular eruption: have inflammatory papules and pustules on a red scaling base that can be confluent
Pinpoint lesions next to the nostrils common
Zone of clearance around vermillion border
Seen perioral, perinasal, and periocular patterns (particularly chin and nasolabial folds)
Asymptomatic or some pruritis or burning
Triggers: moisturizers, cosmetics, fluorinated compounds, SLS (seen in toothpaste)
Diagnosis
Clinical
Treatment
Topical steroids cause temporary improvement but then cause rebound effect → relapse common
D/C steroids and skin irritants
Brush their teeth first and then wash their face
Topical treatment
Metronidazole or erythromycin
Alternative: pimecrolimus
Oral antibiotics if refractory or moderate-severe (4-8 weeks)
Doxycycline or Minocycline
Alternative: erythromycin

Acne Vulgaris
Causes
Blockage and inflammation of pilosebaceous units
Is a multifactorial disorder
May have a genetic predisposition
Pathogenesis
Follicular hyperkeratinization is the primary defect → subsequent plugging of the follicle
Relative excess androgen production → leads to increased sebum production
Cutibacterium acnes proliferation → normal flora but increased, which leads to development of inflammatory lesion
Inflammation → produced by chemotactic factors released by the bacteria
Manifestation
Seen on the face, neck, chest, and upper back
Comedones (hyperkeratotic plug): non-inflammatory
Open → blackhead due to oxidation
Closed → white head (can become open or stay closed)
Inflammatory papules, pustules, and nodules (cysts) that commonly scar (can have pitted scarring or post-inflammatory hyperpigmentation and scarring)
Mild → superficial with few to several papules/pustules and no nodules
Moderate → several to many papules/pustules that are tender and few-several nodules
Severe → have tender lesions because it invades deep into the dermis with many nodular lesions (> 5mm), numerous-extensive papules/pustules, and scarring
Predisposing and aggravating factors
Genetics
Endocrine (PCOS)
Medications (steroids)
Cosmetics
Heat/humidity
Mechanical skin trauma (friction, pressure, vigorous washing, occlusion)
Diet (high glycemic diets and milk)
Variants
Neonatal
Steroid acne
Occupational acne (chloracne)
Acne mechanica → triggered by excess heat, pressure, friction, rubbing, or occlusion
Acne cosmetica
Acne excoriae → picker’s acne
Acne conglobata (severe nodular scarring)
Treatment
Goals
Resolution of symptoms
Prevent development of new lesions and scarring
Treat/prevent post-inflammatory pigmentation changes
Minimize the physiological impact from acne
No topical agent by itself will address all four goals
Therapies must be a minimum of 2 months
May need systemic therapy if topical fails
Mainstay: benzoyl peroxide, topical retinoid (warn females to not wax), topical antibiotic
Reduce C. acne → Benzoyl peroxide (bacteriocidal), topical and oral antibiotics (clindamycin, erythromycin), azelaic acid, oral isotretinoin
Promote exfoliation → topical and oral retinoids, salicylic acid, azelaic acid, benzoyl peroxide
Reduce inflammation → topical and oral retinoids, salicylic acid, oral antibiotics (tetracyclines), azelaic acid
Reduce sebum production → hormonal therapies, oral isotretinoin, spirolactone (potent anti-androgen only used in females)
Severe acne with scarring → isotretinoin

Hidradenitis Suppurativa
Causes
Hormonal influence (onset after puberty)
Genetic predisposition
More common in obesity
Manifestation
Chronic inflammation of the follicular unit → very painful
Have deep seated inflamed nodules and abscesses → skin tunnels (sinus tracts) and scarring
Hallmark: double heads or multi-headed comedones (tombstone comedones)
Seen in apocrine gland areas: axilla, groin, anogenital, inframammary (intertrigous areas)
Exacerbating factors: areas of mechanical stress, menstruation, smoking
Diagnosis
Clinical → typical lesions, typical locations, chronicity and relapses
Treatment
Local hygiene
Weight loss, d/c smoking, screen for comorbid obesity
Education and support
NSAIDs for pain
Long term antibiotics mainstay of treatment
Mild disease → topical clindamycin (oral tetracyclines if fail) and/or antiandrogenic medications and metformin
Moderate-severe disease: combination therapy
Oral antibiotics (tetracycline, doxycycline)
Antiandrogenic medications and metformin as adjuncts
Surgical: punch debridement/unroofing
Biologics
Large fluctuant abscess → incise and drain
Intralesional steroids for acute symptomatic lesions

Lyme Disease
Causes
Multisystem infection transmitted by tick (Ixodes scapularis) → spirochete Borrelia burgdorferi
In most cases need tick attachment for a minimum of 36 hours for infection
Manifestation
Early disease → erythema migrans rash with flu-like symptoms (may have absence of rash)
3-30 days (typically 7-14) after the tick bite
Have bulls eye at the site of the tick bite (usually a single lesion): starts as small papule → slowly increasing erythema ring → erythematous patch but border may be slightly raised
Blanches to palpation
Usually asymptomatic: fades 2-3 weeks
If there are multiple lesions → hematogenous dissemination
Early disseminated → carditis (AV block), facial nerve palsy, meningitis, neuritis
Late/chronic → arthritis
Diagnosis
Clinical diagnosis
Serologic testing: ELISA and confirm with Western blot
Treatment
Doxycycline
Alternative: amoxicillin, cefuroxime
Prevention: avoidance of tick infested areas, skin protection, rapid removal of tick, can start doxycycline if there is a tick that is engorged
Benzoyl Peroxide
Topical oxidizing agent: antibacterial that reduces C. acnes
Mildy keratolyic and comedolytic
Side effects: skin irritation
Retinoids
Any medications that are a derivative of Vitamin A
Effective for inflammatory and non-inflammatory acne: helps to turn over skin cells on the top layer of the skin faster
Reduces comedone production
Normalize follicular hyperkeratosis
Anti-inflammatory properties
Improve acne induced post-inflammatory hyperpigmentation
Side effects → dry skin, redness burning, scaling, increased sun sensitivity
Warn female patients to not wax
Topical Retinoids
Decreases amount of keratinization
May get worse before it gets better: need at least 6 weeks with maximal improvement at 3-4 months
Tretinoin (Retin A)
Best if don’t apply at same time as benzoyl peroxide
Avoid sun exposure (apply at night)
Adapalene (Differin)
Tazarotene (Tazorac)
Pregnancy category X
Antibiotics
Suppress C. acnes production and reduces inflammation
Don’t use as mono therapy
Topical
Clindamycin
Erythromycin (decreased due to resistance)
Oral
Doxycycline or Minocycline (can cause SLE)
Sub-microbial antibiotics and low dose extended release: lower risk side effects and decreases antibiotic resistance
Azelaic Acid
Effective for non-inflammatory and inflammatory acne
Mildly comedolytic, antibacterial, and anti-inflammatory
Helps with post-inflammatory hyperpigmentation
Can be used as monotherapy for mild disease: alternative to retinoids
No photosensitivity and no bacterial resistance
Salicylic Acid and Topical Combination
Salicylic acid
Alternative to retinoids
Comedolytic
Mild anti-inflammatory
Can be combined with Benzoyl peroxide
Topical combination therapy
Clindamycin/Benzoyl peroxide
Clindamycin/Tretinoin
Adapalene/Benzoyl peroxide
Oral Treatments
Oral contraceptives
Anti-androgen effect
Decreases sebum production
Not first line
Used for moderate-severe acne in post-menarchal females
Spironolactone
Androgen receptor blocker: suppresses sebum production
Not first line
Good for adult female acne (not first line for teenage acne)
Distribution is in lower third of face and jawline with cystic lesions that become worse around the menstrual cycle
Isotretinoin → only true treatment for acne
Oral vitamin A derivative → decreases sebum, which decreases C. acne activity and reduces inflammation
Inhibits comedogenesis and normalizes desquamation
Used for severe, recalcitrant nodular acne
Not a first line
Associated with severe side effects → spontaneous abortions, severe congenital malformations (Vitamin A can cross the placental barrier and cause anencephaly), IBD, depression, suicide, SJS and TEN, increased LFTs and cholesterol, visual changes, hepatitis and pancreatitis, idiopathic intracranial HTN, pseudotumor cerebri
iPLEDGE program is required
Need lab testing (pregnancy)

Syphilis
Causes
STI from the spirochete Treponema pallidum
Manifestation: is the great imitator (need high index of suspicion)
Stages
Primary infectious
Starts as papule or nodule → ischemia necrosis → erodes and ulcerates (chancre → cutaneous ulcer that is firm and raised and has well-defined borders) and is painless
Usually one lesion but multiple can occur
May develop lymphadenopathy
Most untreated lesions resolve in 3-6 weeks, but the spirochetes remain in the host
Secondary
Around 6 weeks after chancre: have hematogenous and lymphatic spread
Secondary lesions are highly contagious with direct contact
Lesions are asymptomatic: pink, scaly, macular papular rash → patches in variety of shapes → generalized distribution
Palms and soles: symmetrical hyper-pigmented oval papules with white scales
Associated with flu like symptoms, HA, fever, malaise, generalized lymphadenopathy, and weight loss
Irregular moth eaten alopesia
Mucosa erosions and condyloma lata (moist wart like papules: cauliflower)
Latent
Asymptomatic
+ serologic testing without evidence of active disease
Early latent → < 1 year from onset of primary disease
Late latent → > 1 year from onset primary disease
Tertiary
25% of untreated cases: 1-30 years after initial infection
Small number of organisms elicit an increased cellular response
Have cutaneous gummas or granulomas → grow and ulcerate → chronic inflammatory state
Associated with cardiovascular and CNS symptoms
Transmission: direct contact with infectious lesions
Complications
Late → affect aorta, brain, eyes, and bones, can be fatal (test for HIV)
Congenital → risk to fetus is highest if infection
Diagnosis
VDRL and RPR (reactive by 7th day) → associated with false positives
If screening is positive → confirm with fluorescent treponemal antibody absorption test (FTA-ABS)
Dark microscopy
Neurosyphilis → diagnosis by CSF
Treatment
Primary, secondary, latent (1 year) → Benzathine Penicillin G IM
Late disease (>1 year) → same treatment but 1x/week x 3 weeks
Neurosyphilis → IV Penicillin G x 10-14 days
Follow RPR titers

Bullous Pemphigoid
Causes
Autoimmune sub-epidermal blistering disease: have IgG autoantibodies directed against basement membrane
Trigger is unknown
Association with drugs (furosemide, captopril, NSAIDs)
Affected patients often have multiple/significant comorbidities (neurological disease)
Often in elderly
Manifestation
May have a prodromal/pre-blistering stage
Have generalized eruption with lesions that have tense bullae (1-3 cm) that may be on an erythematous or urticarial base
Bullae rupture in around 1 week, resulting in an eroded base → crusts and heals
Most common sites: trunk, lower abdomen, groin (skin folds and flexural areas)
Have moderate-severe pruritis
Recurrences may occur, but less severe than 1st episode
May be fatal (based on patient medications and comorbidities)
Diagnosis
Skin biopsy
Negative Nikolsky’s sign
Treatment
If untreated, can persist for months-years
Goals
Decrease blister formation and itching
Itching → antihistamine (hydroxyzine/Atarax: have to be careful in older patients because it can cause them to become drowsy and fall)
Anti-inflammatories for mild-limited disease → high potency topical steroids, doxycycline
Anti-inflammatories for extensive disease → prednisone until blistering stops or immunosuppressive therapy
Maintain skin barrier/promote healing
Prevent secondary infection

Pemphigus Vulgaris
Causes
Autoimmune intra-epidermal blistering disease: have autoantibodies against keratinocyte cell surface (rare and potentially life threatening)
Increased prevalence malignancy with neurological disorders and autoimmune diseases
Manifestation
Have involvement of the skin and mucous membranes
Mucosal membranes always affected → most commonly have painful oral lesions
Affected skin most commonly trunk and thighs
First lesion → flaccid blister with clear fluid +/- erythematous base
Bullae are 1-3 cm and rupture easily
Painful oral erosions typically precede blisters by weeks-months → can also occur in non-oral mucosa
Pruritis usually absent
Start localized and becomes generalized if untreated
Erosions for weeks can heal with brown hyperpigmentation
Susceptible to secondary infection
Diagnosis
Skin biopsy
+ Nikolsky sign
Treatment
Goals
Decrease blister formation
Promote healing blisters/erosions
Prevent infection
First line → systemic glucocorticoids and immunosuppressive adjuvant (rituximab)
Alternate: systemic glucocorticoids with azathioprine

Pemphigus Foliaceous
Causes
Associated with drugs (captopril): usually spontaneous recovery once the drug is removed
Increased incidence of associated thymoma, myasthenia gravis, and other autoimmune conditions
Manifestation
Blister is more superficial in epidermis vs pemphigus
Face, middle of chest, back of ears (seborrheic distribution)
Well demarcated lesions
Associated with pain/burning > itch
Intact blisters usually not seen
Usually do not see lesions on the mucosa
Treatment
Steroids

Dermatitis Herpetiformis
Causes
Autoimmune chronic vesicular and bullous skin condition associated with glucose sensitivity
Most patient’s have GI involvement and are more likely to have thyroid disease and lymphoma
Usually chronic and recurrent
Manifestation
Extremely itchy and burning
Have groupings of vesicles/excoriations that tend to be symmetrical → herpetiform
On extensors of elbows and back of neck
Usually do not see lesions that are intact → scratching removes them and leaves crusted papules and erosions
Can have oral lesions/bullae
Diagnosis
Direct immunoflourescene biopsy (will see IgA in the dermis)
Treatment
Gluten free diet
Oral dapsone (lab monitoring is required because it can cause hemolysis: G6PD, LFTs, CBC)

Bullosis Diabeticorum
Causes
Bullous disease of diabetics: spontaneous and non-inflammatory blistering condition
Associated with sub-optimal glycemic control
Tend to have other diabetic manifestations
Tends to be trauma related
Manifestation
Tense, non-tender, non-inflammatory blisters that are painless with mild burning
Often large, ranging from 0.5-1.7 cm
Most common on feet and lower legs and tend to recur in the same area
Diagnosis
Biopsy
Treatment
Generally self-limiting (lesions usually heal in 2-6 weeks)
Leave the blister intact
Antibiotics for secondary infection

Dyshidrotic Eczema
Causes
Unknown etiology
Inflammatory
Tends to be in patients with a history of atopic dermatitis
Potential triggers: contact dermatitis, fungal infection, overuse of soaps
Increased sweating can intensify the condition
Manifestations
Vesicular dermatitis
Tend to have sudden onset of eruption of vesicles that are very itchy
Deep seeded Tapioca like vesicles → filled with clear yellow fluid
Get red fissured cracked skin base with brown spots if opened
Can be on both hands (sides of fingers) and feet
Can see chronic eczematous changes such as erythema, scaling, and lichenification
Diagnosis
Clinical
Consider patch testing
Treatment
Usually resolves over 1-3 weeks
First line
Avoid irritants and triggers
Initial: cold wet dressings/Burrow’s solution
Followed by high potency topical steroids
Other options
Tacrolimus ointment can alternate topical steroids
Prednisone tapered 1-2 weeks if needed

Insect Bites
Manifestation
Red papules
Urticarial lesions
Anaphylaxis
Treatment
Symptomatic treatment for local reactions
Ice packs, cool compresses, topical anesthetics, antihistamines, steroids
Flea bites
Manifestation
Typically on the ankles and legs: have small red dots or puncta → clustered red papules
Very pruritic
Urticaria in patients who are allergic
Treatment
Topical antipruritic (Sarna)
Topical steroids
Animals, bedding, and carpets need to be treated
Watch for signs of secondary infection
Bee and Wasp Stings
Manifestation
Initially sharp pain/sting followed by burning
Initially have elevated pink wheal with central pinpoint red punctum → angioedema (localized tissue swelling)
Severe reactions more common in adults (can be localized or systemic)
If previously sensitized → local reactions with swelling that forms within hours
Can become secondarily infected 2-3 days later
Treatment
Remove stinger
Localized allergic: antihistamines

Brown Recluse Spider Bite
Causes
Lives in dark areas
Bites often not noticed
Manifestation
Early on may show local hive like reaction with minimal erythema/swelling
6-8 hours: pain, burning, stinging, followed by vasospasm and tissue ischemia
12-24 hours: joint and muscle pain, weakness, nausea and vomiting, fever and chills
Necrosis can be deep, resulting in an ulcer
Do worry about airway obstruction with neck bites
Cyanosis followed skin necrosis within days
Most severe reaction in fatty areas (abdomen, thigh)
Diagnosis
Biopsy
Early on → neutrophils
Later on → coagulative necrosis of epidermis and dermis
Treatment
Mild reactions → cold packs/wet dressings, analgesics
Necrotic lesions → wound and local care
+/- dapsone (can help to prevent necrosis)
Tetanus prophylaxis

Cutaneous Drug Reaction
Causes
Immunologic/hypersensitivity
Non-immunologic (most common)
Many drugs can cause it → antibiotics, anticonvulsants, psychotropic, NSAIDs, chemotherapeutic
Manifestation
Morbilliform maculo-papular rash that becomes confluent the longer it persists
Usually the face is spared: involved trunk and extremities (generalized distribution)
Itching common
Mucous membranes may be involved
Hard to distinguish from viral exanthems
Diagnosis
Biopsy
Treatment
Antihistamines
Cold compresses
D/C the drug

Urticarial Drug Eruption
Causes
Anaphylactic IgE mediated within minutes-hours of the drug
Most frequently due to aspirin, PCN, blood products, radioactive due
Treatment
Depends on severity of the reaction
Antihistamines, cool compresses, epinephrine, oral or IV corticosteroids, hospitalization

Fixed Drug Eruptions
Causes
Most commonly after tetracycline, NSAIDs, sulfamethoxazole/trimethoprim
Manifestation
Skin or mucous membrane that is localized
Have single or multiple well demarcated, dusky red plaques soon after drug exposure
Often form blisters → erosions → desquamation or crusting
Associated with itch and burning before/during the rash
Brown pigment with healing
Most common site → glans penis
Can see recurrence in the area of the skin

Seborrheic Dermatitis
Causes
Chronic inflammatory papulosquamous disorder: tend to have chronic course with remissions and exacerbations (stress, fatigue, climate)
Etiology unknown → associated with Malassezia (Pityrosporum yeast)
Manifestations
Papules that are pink-yellow, greasy, and scaling with areas of coalescing erythematous plaques and patches in areas with the most sebaceous glands (scalp, central face, pre-sternal areas) → scales are oil flakes
Face: eyebrows, base of eyelashes, nasolabial folds, para-nasal area, external ear canal
Flexural areas: post-auricular, inguinal, inframammary folds, anogenital area
Diagnosis
Clinical
Treatment
Cannot cure: will manage the symptoms
Difficult to treat in patient’s with neurological disorders (PD)
Adult (non-scalp) treatment
Topical antifungals (ketoconazole)
Moderate-severe cases → add low potency topical corticosteroids (one exception to using steroids with fungal/yeast infection)
Scalp treatment
Thick adherent scale → mineral or olive oil then gentle removal of scale
Antidandruff shampoo → ketoconazole, zinc pyrithione, selenium sulfide
Topical corticosteroid (high potency)
Make sure to educate the patient that it is not because they have dry skin → over moisturizing could make the symptoms worse

Infantile Seborrheic Dermatitis
Manifestations
Have thick, adherent, yellow (will look different in melanin rich skin), greasy scales on the vertex of the scalp with minimal redness
Diaper area and axilla may be involved (redness more prominent)
Minimal itch
Secondary bacterial and candida infections possible
May have hypo/hyperpigmentation changes
Treatment
Usually self limiting
Can use emollients or oil (gentle removal of scale)
Extensive/persistent cases → low dose topical steroid

Pityriasis Rosea
Causes
Etiology unknown (possibly viral)
Papulosquamous eruption
Manifestation
Have fine pink scales that can itch
Typically asymptomatic: can have mild prodrome or URI within 1 month prior to eruption
First lesion: Herald’s patch (typically the largest) usually on the trunk → 1-2 cm oval plaque that is a thin collarette scale (scale does not go to the edge of the lesion and concentrated in the center) inside a lesion border
Smaller lesions erupt days to 1-2 weeks later: initially papules and then develop to thin scales on a plaque that are salmon colored on Caucasians or dark brown on colored individuals
Usually on the trunk and back (lower abdomen/pubic area) and proximal extremities → drooping pine branches or Christmas tree pattern
Do not see it on the lower thighs/legs and the face
Treatment
Usually self limiting
Treat any itching as needed (topical steroids/oral antihistamines)
UVB can help speed up the treatment progress

Psoriasis
Causes
Etiology is unknown → have abnormal T cell dysfunction
Multiple genetic defects → hyper proliferative keratinocytes in basal layer of the epidermis
Triggered by unknown antigens → activate T cells → TNF, interleukins → hyper proliferation → physical, infectious and pharmacological agents can aggravate
See genetic disposition
Chronic remitting and relapsing disease (most common in white people)
Bimodal: peak in 20-30s and peak again in 50-60s
Manifestation
Seen in elbows, gluteal cleft, scalp, knees, fingers, toenails, tips of penis, and behind the ears
Chronic Plaque
Most common subtype → papulosquamous lesions that are well demarcated, red, and round-oval plaques
See thick adherent silvery scales: pinpoint bleeding after removal of the scale (Auspitz sign)
Have pruritis and symmetrical distribution
Guttate
Drop like, discrete papules and small plaques usually on the trunk and extremities
Strong association with infections (Strep) (seen in younger patients)
Usually have no history of psoriasis
Pustular
Erythema, scaling, pustules (painful and filled with non-infectious fluid and WBCs) → coalesce and forms lakes of pus
Generalized (von Zumbush): total body (including palms/soles) in ill patients (fever and potentially life threatening complications, such as renal, pulmonary, hepatic, and sepsis)
Erythodermic
Generalized erythema and scaling with desquamation of the skin → potentially life threatening due to loss of the skin barrier
Palmoplantar
Erythematous hyper-keratotic plaques with associated features on the palms and soles
Inverse (Intertrigous)
Inflamed lesions on intertriginous surfaces (could be confused for candidiasis): smooth, shiny plaques with minimal to no scale
Seen in gluteal cleft, breasts, peri-anal, and axillae
Nail psoriasis
Usually occurs with cutaneous lesions
Have pitting, leuokonychia, lunular red spots, onycholysis, crumbling, subungal hyperkeratosis, tan-brown color (oil drop), splinter hemorrhages
Psoriatic arthritis
Inflammatory arthritis (usually polyarthritis): have pain, swelling, stiffness in 1 or more joints often with nail abnormalities
Usually becomes better at the end of the day
Ocular involvement → blepharitis (most common), conjunctivitis, uveitis, corneal lesions
Exacerbating factors
Cold weather
Stress
Physical trauma/minor trauma → scratches, tattoo applications, surgical incisions (Koebner phenomenon)
Infections (Beta hemolytic strep, HIV)
Postpartum
Medications → beta blockers, lithium, antimalarials, NSAIDs, tetracycline, steroid with drawl, prednisone
Alcohol and smoking
Have increased prevalence of comorbid disorders: CVD, DM, HTN, obesity, depression, autoimmune, malignancy, metabolic syndrome
Treatment
Limited disease
1st line → potent topical corticosteroids and emollients
Ointments most effective: create occlusive barrier to increase hydration and penetration
Alternative: topical retinoids, tar, topical Vitamin D analogs
Tazarotene (topical retinoid): modifies keratinocyte hyper- proliferation and reduces inflammation (can be combined with high potency steroid) → avoid in pregnant women
Vitamin D (calcipotriene/calcitriol): anti-proliferative and immunomodulating effect on keratinocytes → inhibit keratinocyte proliferation and T cell activation (refrigerate if causes burning)
Facial/intertriginous areas: steroid-sparing (tacrolimus)
Localized phototherapy (narrowband UVB)
Combination topical therapy
Enhances efficacy, decreases side effects, and longer remission
Taclonex (calcipotriene and betamethasone)
Moderate-severe disease (> 5% BSA)
Topical therapies (with other treatments)
Super high potency: Clobetasol, Betamethasone
Phototherapy → highly effective (does increase risk of skin cancer)
Systemic treatment: methotrexate (first line treatment for moderate-severe: can cause long-term liver abnormalities and liver failure), cyclosporine (immunosuppressive drug but could have nephrotoxicity), systemic retinoids, and biologics (Risankizumab: should do Quantiferon gold test because of their immunosuppression)
Otezla (apremilast) → inhibits PDE4 to reduce inflammation but tend to have nausea, diarrhea, weight loss of 10 lbs, and depression
Sotyktu recently approved by FDA
Scalp psoriasis → anthralins (keratinolytic agent)

Lichen Planus
Causes
Autoimmune papulosquamous disorder of the skin and mucous membranes
Exact etiology unknown: has an immune-mediated pathogenesis
Usually idiopathic: can be drug induced (ACEI, beta blockers, quinidine, thiazide diuretics, antimalarials), hepatitis C
Can have family history
Manifestations
Acute or chronic (oral tends to be chronic)
Have various types
Papular (most common)
Hypertrophic, follicular, erosive, ulcerative, bullous, atrophic, nails
Six P’s
Planar (flat topped)
Purple
Polygonal (polyangular)
Pruritic
Papules
Plaques (milky white papules in the mouth: painful ulceration in the mouth, penis, and vulva)
Seen in the flexor surfaces (wrist, forearm, legs and shins), oral mucosa, genital mucosa, scalp (may have permanent hair loss), and nails (grooved, thinning, longitudinal fissure, onycholysis, dystrophy)
Wickham’s Striae → fine reticular pattern of white lines that criss cross in a lace like pattern
Do see Koebner phenomenon
Diagnosis
Clinical
Punch/shave biopsy
Treatment
First line
High potency topical steroids
Thicker lesions → intra-lesional steroids
Generalized or resistance cases
Phototherapy
Oral retinoids (Acitretin)
Oral steroids (short course)
Other → oral antihistamine for itch
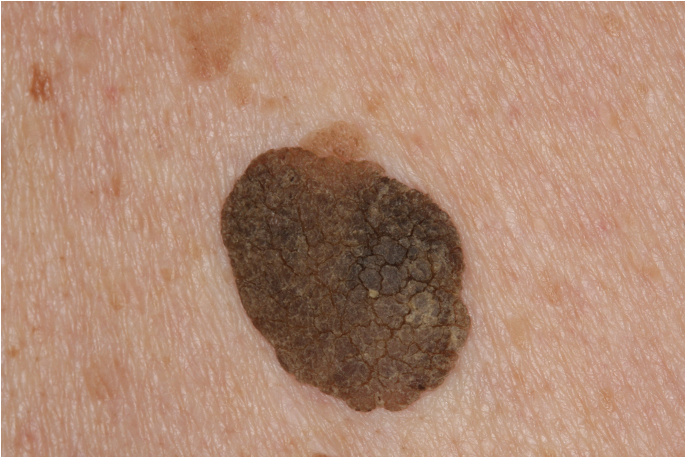
Seborrheic Keratosis
Causes
Epidermal lesion that is the most common benign tumor in older people
Multiple SebK: AD
Manifestations
Usually asymptomatic: location could cause irritation, inflammation, and bleeding
Often seen on pre-sternal areas, back, and under the breasts
Do not see on lips, palms, and soles
Uneven, dull, well demarcated, waxy, warty (can be smooth or velvety) with a stuck on appearance: can be flat or raised
Color variable: brown, black, white, pink
Usually 0.2-2 cm
Appearance may mimic other skin tumors (especially more pigmented lesions that mimic melanoma)
Dermatosis papulosa nigra: dark pigmented SebK on the face (more common in African Americans)
Stucco keratoses: smaller white firm SebK primarily on the lower legs/ankles in older Caucasians
Lesler-Trelat sign: abrupt explosive onset of numerous SebK associated with internal malignancy
Diagnosis
If in doubt, biopsy
Treatment
If not treated → persists and is slow growing
Cryosurgery for flat or slightly raised lesions
Thicker lesions: cautery and curettage under local anesthesia (does cause scarring)
Excision (usually not done)

Skin Tags (Acrochordons)
Causes
Benign growths more common in obese patients and DM
Familial tendency
Manifestation
Skin-colored brown papule that is 1-5 mm → most commonly fleshy and soft, pedunculated on a thin stalk
Occasionally flat or filiform
Black or red if thrombosed
Common locations: axilla and neck (also seen in eyelids, intertriginous areas, skin creases)
Usually asymptomatic
May become irritated by rubbing or painful if twisted or thrombosed
Diagnosis
Clinical
Treatment
Not required
Can excise tag, cryotherapy, or electrocautery
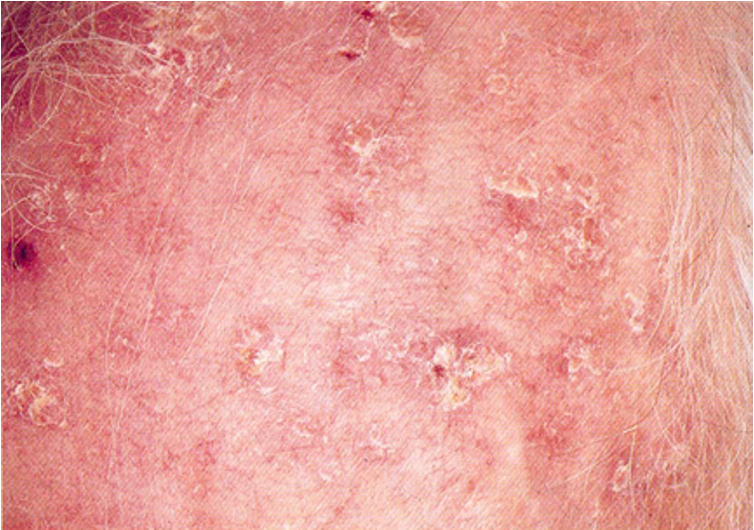
Actinic Keratosis
Causes
Solar keratosis from cumulative sun exposure
Premalignant lesion for SCC and BCC
Have a variable course: small % progress to SCC
Manifestation
Can have one or multiple lesions
Gritty papule on a erythematous base with rough adherent yellow scale
Found on the face, head, ears, neck, dorsum of hands and forearms
Can be hypertrophic: thick adherent scale on erythematous base
Can have a cutaneous horn → horn like projection on a lesion that has accumulated a thick scale (differential for AK, SCC, SebK, and wart)
Can have actinic chelitis (typically on the lower lips): rough, scaly papules that are persistent
Differential: SCC, BCC, inflamed SebK
Diagnosis
Treatment
1-few isolated lesions
Cryotherapy
Excision
Multiple lesions
Topical 0.5% fluorouracil cream (causes inflammation and sloughing)
Imiquimod
Photodynamic therapy
UVB/UVA sunscreens for prevention

BCC
Causes
Most common form of skin cancer
Seen in > 40 y/o, fair skinned, and prolonged sun exposure
Slow growing and low risk of metastasis
Manifestation
Nodular
Most common
Translucent, pearly, white-pink, dome shaped papule or nodule with telangiectasia over the surface
Have rolled border → periphery higher then center
Frequently ulcerates (rodent ulcer)
Superficial
Thinnest and least aggressive
Oval, red, scaling plaque with a raised border
Differential: eczema, psoriasis, premalignant or other malignant skin lesions
Pigmented → brown, black, or bluish
Morpheaform/sclerosing
Least common
Infiltrative BCC: more aggressive and recur more
Resemble scar tissue: have indistinct margins with firm, flat or raised whitish/yellow and waxy (can have telangiectasia)
Commonly seen on the head and neck, with 70% on the face
Can cause severe disfigurement
Diagnosis
Biopsy is essential
Treatment
High cure rate in early disease
Surgical excision
MOHS
Micrographic procedure where skin cancer is excised according to microscopically identified controlled surgical margins (conserves more tissue but takes longer)
Indicated for recurrent tumors, tumors with ill defined margins, tumors in young adults, aggressive tumors, and near cosmetic structures
Curettage and electrodessication
Secondary
Imiquimod, fluorouracil topically
Photodynamic therapy
Radiation (for treatment of high risk BCC for poor surgical candidate)
Risk factors for BCC and SCC
Incidence increases with age (> 50 y/o)
Fair, freckled, ruddy complexion
Light colored hair or eyes
Tendency to sunburn easily
Blistering sunburns as a child
Geographic location near equator or high altitudes
Cumulative sun exposure/UV light
Exposure to arsenic/hydrocarbons
Overexposure to radioisotopes or ionizing radiation
Chronic skin inflammation and/or repeated skin trauma
Precancerous dermatomes

SCC
Causes
2nd most common skin cancer
Seen in ages > 50
Immunosuppression increases risk
Often preceded by actinic keratosis
Low risk of metastasis but higher risk than BCC (grow weeks to months: higher risk with lips/ears)
Manifestation
Have a pink-dull red, poorly defined dome shaped nodule (papule/plaque) with adherent yellow-white scale (may have warty appearance): can develop necrotic, crusted center that may ulcerate
Hyperkeratosis associated with highly differentiated lesions
Often asymptomatic (can be painful or pruritic)
Commonly on the head, scalp, ear, lower lip (think about smoking history), neck, hands, forearms, lower legs, shoulders, upper trunk, and the back (not commonly on the back of the hands)
In dark skin patients: most in non-sun exposed areas
Bowen’s Disease
SCC (in epidermis only) in situ → slow growing, asymptomatic, erythematous, well demarcated, scaly plaque/patch
Differential: nummular eczema, psoriasis, BCC, inflamed SebK
Invasive/poorly differentiated → fleshy granulomatous nodules that lack hyperkeratosis and may have ulceration/hemorrhage/necrosis
Can have cutaneous horn (differential is actinic keratosis, SCC, and wart)
Diagnosis
Biopsy
Treatment
Low risk lesions
Surgical excision/MOSH
Curettage and electrodessication
Cryotherapy
High risk lesions
Surgical excision/MOSH
Radiation
Chemotherapy

Merkel Cell Carcinoma
Causes
Aggressive primary skin cancer (neuroendocrine)
Seen in the elderly and fair-skin tones
Increased incidence with immunosuppression
Malignant cells develop on or just beneath the skin and follicles → have a tendency to recur
Manifestation
Typically solitary: rapidly growing, painless, firm, shiny, non-tender, flesh-colored or bluish-red intracutaneous nodule
Regional lymph node metastasis is common
Most often on the head or neck
Do see systemic disease develop
Treatment
Overall 2 year survival rate is 50-70%
Surgery: wide and local excision
Radiation

Melanoma
Causes
Tumor of epidermal melanocytes (from melanocytic nevi or normal skin)
Associated with intense, intermittent sun exposure and sunburns in childhood
High risk of metastasis → once metastatic, 15-20% 5 year survival
Manifestation
Varies in color: red, white, blue, brown, black
Have aggressive local growth
Scalp, head and neck have higher death rate
Men → seen on back/trunk
Women → lower legs and back
Superficial spreading melanoma
Most common
Seen in upper back in men and legs in women
Red/white/blue/brown/black papule, nodule, or plaque: have typical ABCDE
Associated with precursor melanocytic nevi
Nodular melanoma
2nd most common type
Dome shaped polypoid papule/nodule that is blue-black (can be non-pigmented or pink-red with scale and ulceration): may have symmetrical border and smaller diameter (harder to diagnose)
Grows rapidly and thicker
Lentigo maligna melanoma
Related to sun exposure: arises from precursor lesion lentigo maligna (melanoma in situ)
Usually seen on face/scalp
Brown patch with irregular edges and pigmentation: slow growing
Acral lentiginous melanoma
Least common (most frequent in African Americans and Asians)
Seen in palms/soles, phalanges, and nail bed (may present as diffuse nail discoloration or a longitudinal pigmented band: Hutchinson’s sign is when the pigment spreads from the nail bed to the surrounding tissues)
Dark brown-black irregularly pigmented flat/slightly raised lesions with potential ulceration/bleeding
Tend to metastasize
Usually confused with junctional nevus or subungal hematoma
Subungal melanoma: A (age), B (brown-black band), C (change in nail band), D (digit most commonly affected is great toe and thumb), E (extension of pigment onto proximal and/or lateral nail folds), F (family or personal history)
Amelanotic melanoma
Can be of any subtype: on palms, soles, subungal
Non-pigmented melanoma: pink-red macule, papule, or plaque
Often misdiagnosed
Poor prognosis
Treatment: excision (assess sentinel nodes and work up for metastatic disease)
Diagnosis
Excisional biopsy
Have no formal guidelines for screening: remain alert
Clinical prediction rules
ABCDE
Asymmetry
Border irregularity
Color variegation
Diameter: >6 mm
Evolving lesion (elevation/enlargement)
Ugly duckling sign → pigmented lesion clearly different from the other nevi
Glasgow revised 7-point checklist
Major: change in size/new lesion, change in shape/irregular border, change in color/irregular pigmentation
Minor: diameter >= 7 mm, inflammation, crusting or bleeding, sensory change/itch
Suspicion if any major criteria +1 minor or 3 or > minor criteria
Staging
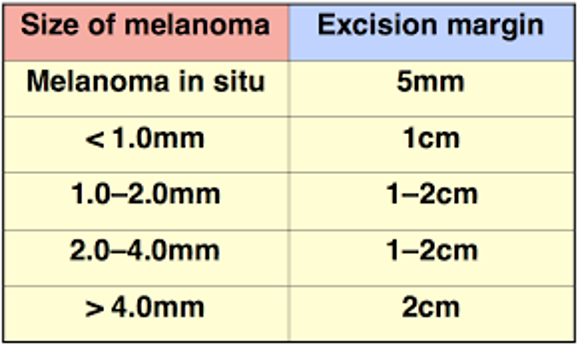
Berswlow thickness depth (determines surgical margins)
Clark levels (tissue depth)
I: in situ, confined to epidermis
II: in papillary dermis
III: filling papillary dermis
IV: in reticular dermis
V: in subcutaneous fat
+/ ulcerations
Mitotic rate
Regional lymph node involvement
Distant metastases
Differential
Nevus (maybe traumatized)
Atypical/dysplastic nevi
Blue nevi
Solar lentigo
Pigmented/irritated seborrheic keratosis
Pigmented BCC
SCC
Dermatofibroma
Hemangioma
Treatment
Mortality higher in men than women
Surgical removal (wide local excision: if not deep enough it can be a false negative)
Advanced disease, unresectable, or recurrent → chemotherapy, radiotherapy, immunotherapy (biologics)
Prognosis
Thickness of tumor (thicker → poor)
Ulceration (2nd most important factor)
Gender
Age
Regional or distant spread (involving extremities have better prognosis than trunk/head, and scalp has worst prognosis)
Grade of melanoma (I-V)
Risks for Melanoma
Advanced age
Sun exposure
Nevi that are numerous, changing, or atypical (dysplastic)
Clark’s nevi (dysplastic nevi) → acquired nevi larger then 6 mm (genetic predisposition to melanoma)
Inherited conditions (xeroderma pigmentosum, basal cell nevus syndrome)
Personal history of BCC or SCC
Personal history of melanoma or atypical nevi ***
Family history
Light complexion/inability to tan (freckling, red or light colored hair, light eyes)
History of blistering sunburn
Immunosuppression
Prevention of skin cancer
Minimize UV radiation exposure
Avoid peak hours and artificial UV
Use UVA protective coating to tint home, office, car windows
Seek shade and be aware of radiation from snow, sand, and water
Sunscreen with SPF 30 or reapply Q2 hours/after swimming and sweating
Wear photo protective fabrics
Wear UV protective sunglasses and hat
Monitor skin for suspicious lesions
Melanoma Prognosis 5-year Survival
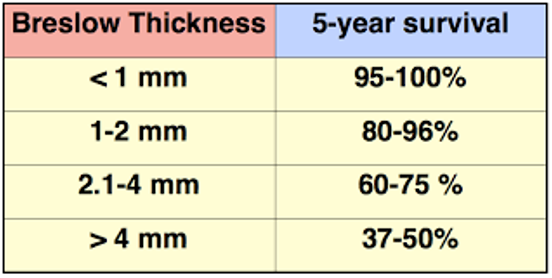
Melanoma size of melanoma and excision margin