Fetal Monitoring & Cardiovascular Alterations Study Set
1/81
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
82 Terms
intrapartum fetal surveillance
assessing the baby in the abdomen
Improving Placental Perfusion
-stopping oxytocin
-repositioning
-administering oxygen
-increasing rate of IV fluids
purpose of fetal surveillance
-Evaluate the fetal condition during pregnancy.
Is the baby tolerating pregnancy well?
-Identify possible hypoxic insult.
Result from low FHR
intermittent auscultation w/palpation of uterine activity (low tech)
electronic fetal monitoring (high tech)
What are two approaches to intrapartum fetal monitoring?
advantages of electronic fetal monitoring
-supplies more data about the fetus and auscultation
-provides a permanent record that may be printed or stored electronically
-gradual trends in FHR and uterine activity are apparent
helps assess labor and how well the baby is tolerating it
reduced mobility
What's a limitation of electronic fetal monitoring?
ultrasound transducer and toco transducer
What are two components of external fetal monitoring?
ultrasound transducer
-measures FHR
-found in lower abdomen
-secured on the mother's abdomen with elastic straps
-less accurate than internal devices but are noninvasive and suitable for most women in labor
toco transducer
-measures contractions
duration and frequency, not severity
-a pressure-sensitive area detects changes and abdominal contour to measure uterine activity
during the interval between uterine contractions (i.e. uterine relaxation)
When does optimal exchange of oxygen with the placenta occur?
110-160 bpm
What is normal fetal heart rate?
baseline
-average HR calculated during a 10-minute interval
-minimum of 2 minutes of data within the 10-minute period is needed to calculate the FHR
-heart rate is rounded to the closest multiple of 5 beats/min
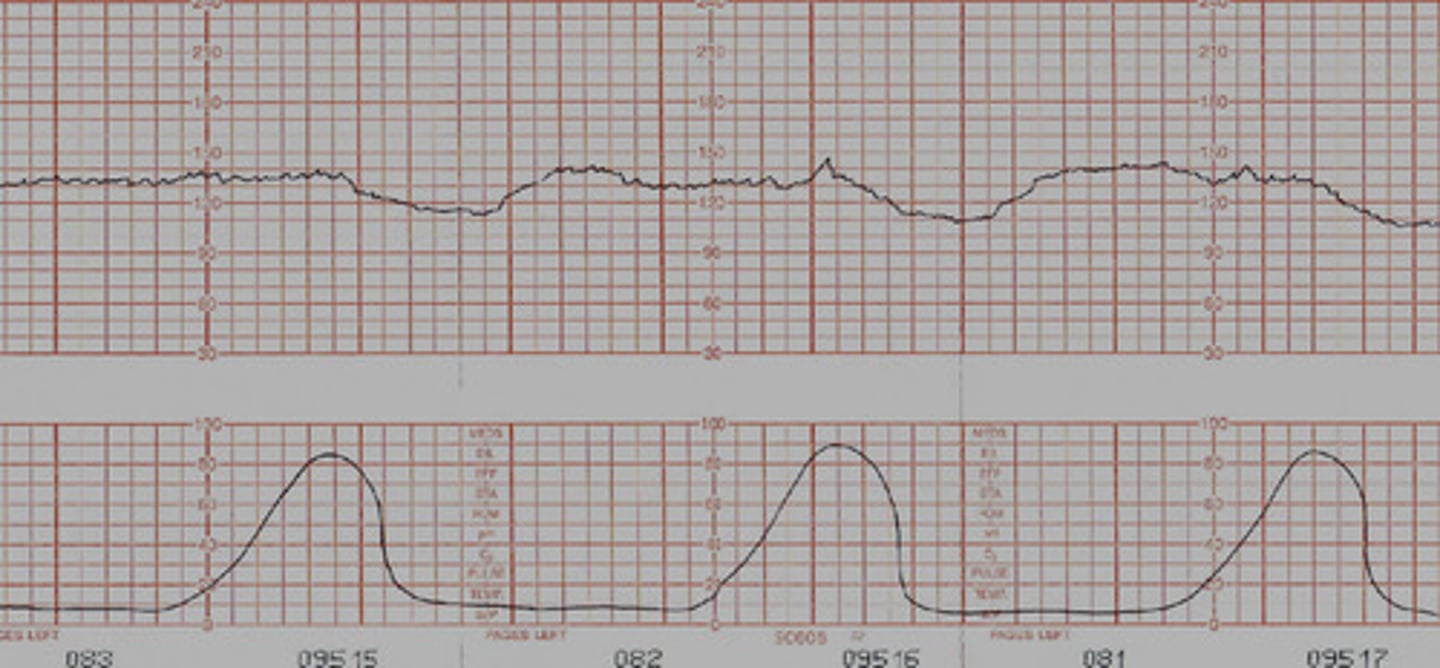
FHR Variability
-describes fluctuations in the baseline FHR that cause the line to have a wavelike appearance
-shows function of fetal autonomic NS --> how well the fetus is tolerating labor
absent FHR Variability
-undetectable
-emergency C-section
-baby hypoxic but still has heart rate
-baby not moving at all
minimal FHR variability
-Greater than undetectable but less than 5 bpm per minute
-baby isn't moving that much
-baby may be asleep
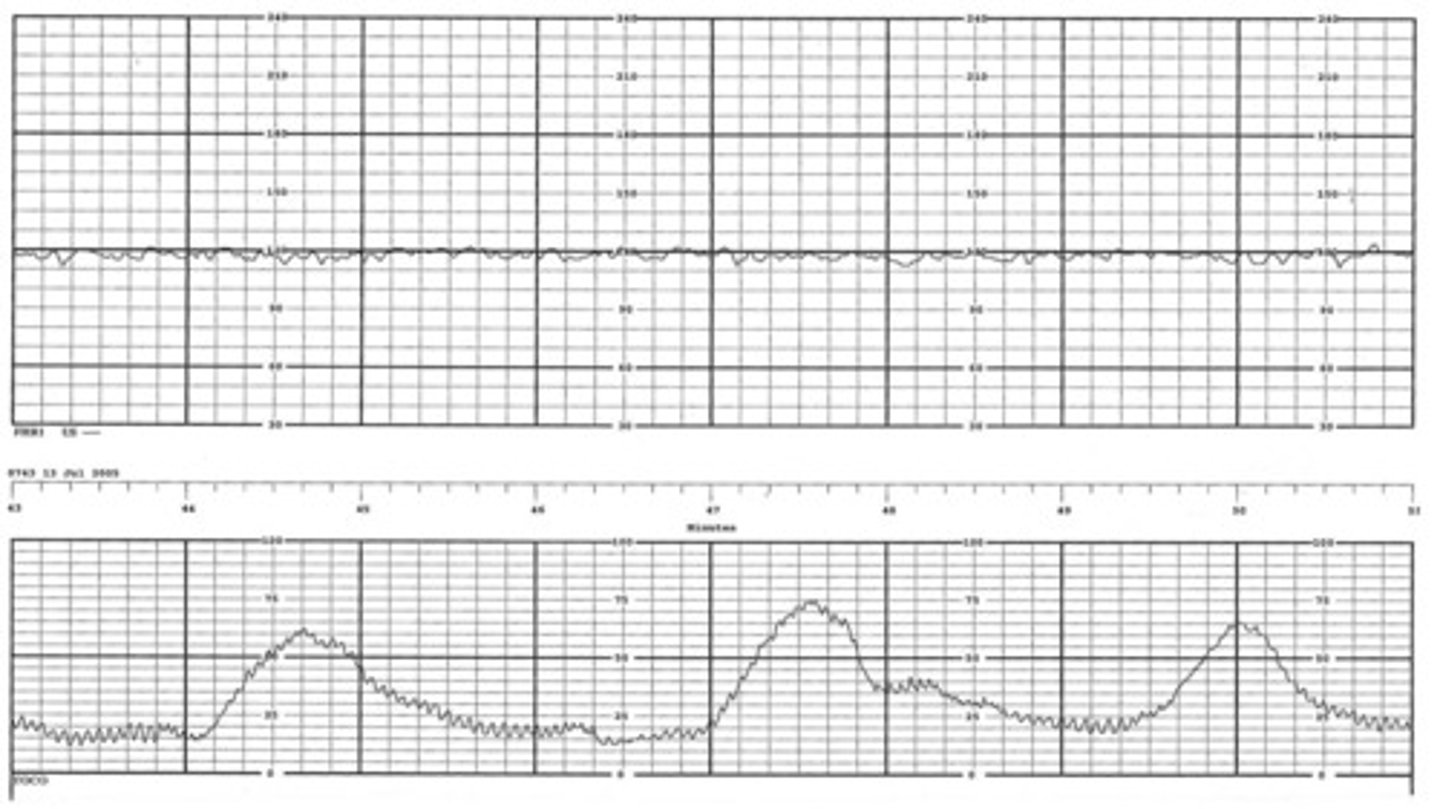
moderate FHR variability
-6-25 bpm
-normal (reassuring) and indicates that fetus is well oxygenated
marked FHR variability
Greater than 25 (bpm per minute)
accelerations
-indicator of fetal wellness and normal acid-base balance
-visible, abrupt increases of at least 15 bpm above the baseline FHR and lasts at least 15 seconds
"15 x 15"
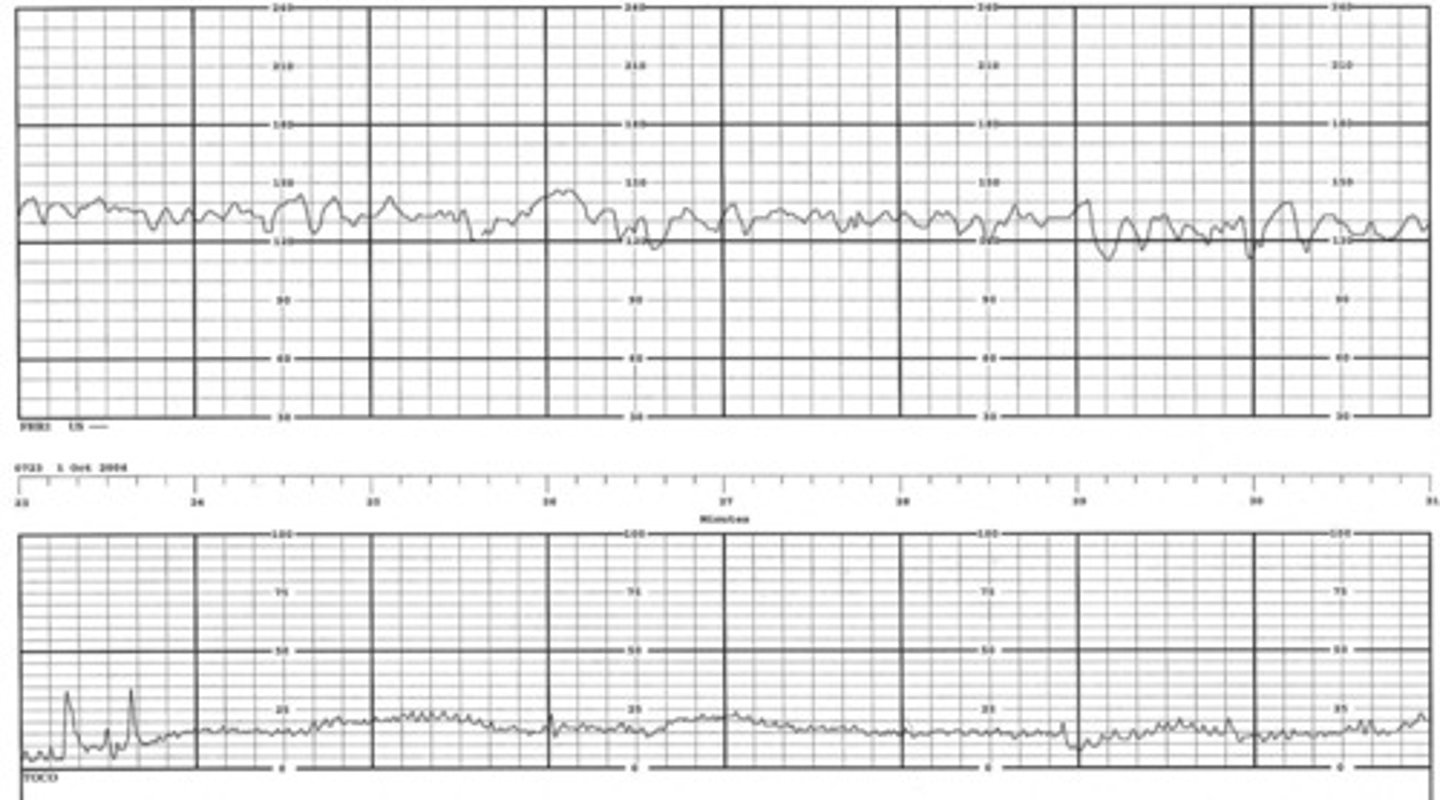
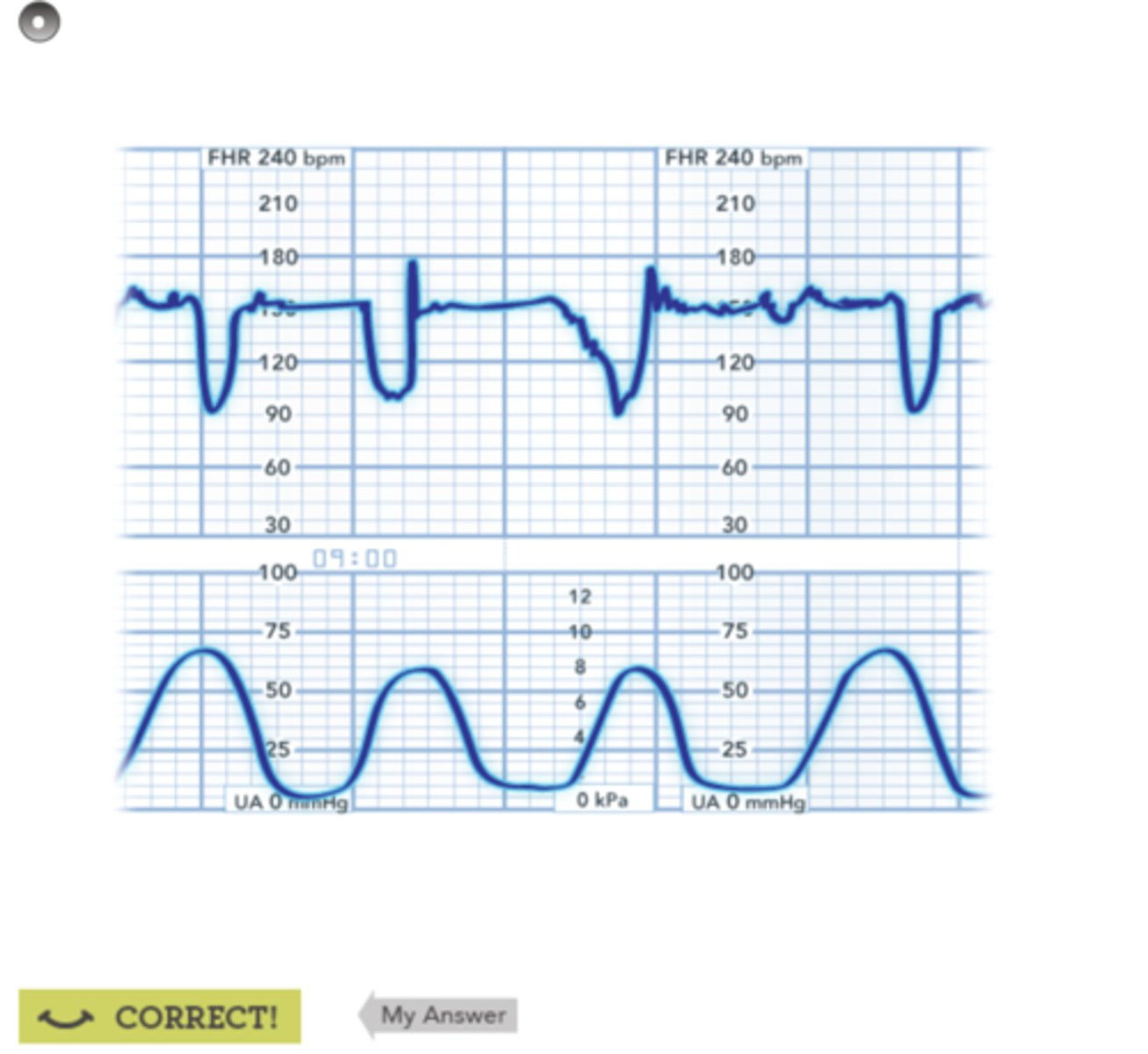
early decelerations
-The onset (point of lowest FHR) and recovery (return to baseline FHR) correspond to the beginning, peak, and end of contraction
-sometimes called a mirror image of a contraction
-safe!
-no lower than 30-40 bpm from baseline
-onset of nadir and return to baseline is at least 30 sec
head compression; fetal head is further pushed into the birth canal by contractions
What is the cause of early decelerations?
variable decelerations
-FHR "varies" in duration, intensity, and timing
-abrupt deceleration in HR, typically causing "U", "V" or "W" shape
entire variable occurs in 30 sec
umbilical cord compression
What's the cause of variable decelerations?
umbilical cord compression
-umbilical cord delivers oxygen and nutrients to fetus
-not dependent on contraction
-intervention: reposition
amnioinfusion
Infusion of a sterile isotonic solution into the uterine cavity during labor to reduce umbilical cord compression; may also be done to dilute meconium in amniotic fluid and reduce the risk that the infant will aspirate thick meconium at birth.
late decelerations
-slowing of the FHR after the contraction started has prolonged time before returning to baseline
-means infant switches to anaerobic metabolism, which leads to acidemia, which worsens cardiac function
uteroplacental insufficency
(decrease in uterine blood flow = decrease in fetal oxygenation)
What's a cause of late decelerations?
A. side-lying
B. Pitocin
C. IV fluid bolus
Interventions for Late Decelerations
1. Notify HCP.
2. Identify cause
Reposition Mother to (A) position, which releases aortocaval compression and increases fetal blood flow.
3. Stop (B) or oxytocin to reduce contractions.
4. Administer (C) to increase blood volumes.
5. Eight - ten L face mask of oxygen may be a short-term intervention to reduce anxiety.
If none of these interventions work, HCP may order emergent C-section.
V: variable deceleration
E: early deceleration
A: acceleration
L: late deceleration
coordinates respectively w/
C: cord compression
H: head compression
O: okay
P: placental insufficiency
Describe the mnemonic "Veal Chop."
congenital and acquired
What are two types of heart diseases present in children?
congenital heart diseases
-present from birth
-abnormal development of heart during pregnancy
acquired heart diseases
-develop later in life
-often caused by lifestyle choices
Kawasaki's disease
-acute, febrile, skin-erupting illness of children with a generalized vasculitis
-associated w/coronary artery aneurysms
-acute phase: implement IV fluids
Diagnosis of Kawasaki's disease
-fever of 5 days' duration
-bilateral nonpurulent conjunctivitis
-oral mucosal alterations (e.g., strawberry tongue; pharyngeal erythema; dry, fissured lips)
-Redness of the hands and feet followed by desquamation and rash on the trunk
-Cervical lymphadenopathy with large nodes
rheumatic fever
-diffuse inflammatory condition of the connective tissue that is most likely of autoimmune origin.
-primarily affects the heart, joints, subcutaneous tissues, brain, and blood vessels
-complication: rheumatic heart disease, which can result in permanent damage to the mitral and aortic valves.
-antibiotic prophylaxis
clinical manifestations of rheumatic fever
Arthritis
Carditis (inflammation of endocardium)
Chorea (involuntary, spastic movements of legs, arms, and face)
Erythema marginatum
Subcutaneous nodules
poor feeding, murmurs and/or unusual pulses, failure to thrive, tachycardia/tachypnea, frequent upper respiratory infections, sweating (SOB, and exercise intolerance)
What are six common signs/symptoms of congenital heart disease in children?
Eating and drinking takes a lot of energy
Why do children with congenital heart disease feed poorly?
Fluid stays stagnant in the respiratory system
Why do children with congenital heart disease experience frequent URIs?
radial, femoral, pedal
What are three locations to measure pulses on a kid?
brachial, femoral
What are two locations to measure pulses on an infant?
Assessing a Child w/Congenital Heart Disease
-obtain a history
-cardiac-focused exam
rapid, initial assessment and general survey
Respiratory
-color: cyanotic, pale, mottling
-work of breathing
-retractions
-late nasal flaring
Heart
-listen
-palpate for thrill
-palpate pulses
-capillary refill
-edema?
-urine output?
acyanotic defects
-No unoxygenated blood in the arterial circulation
-left to right shunt of blood
-oxygenated blood is flowing into de-oxygenated blood
-includes atrial septal defect, patent ductus arteriosus, and atrial septal defect
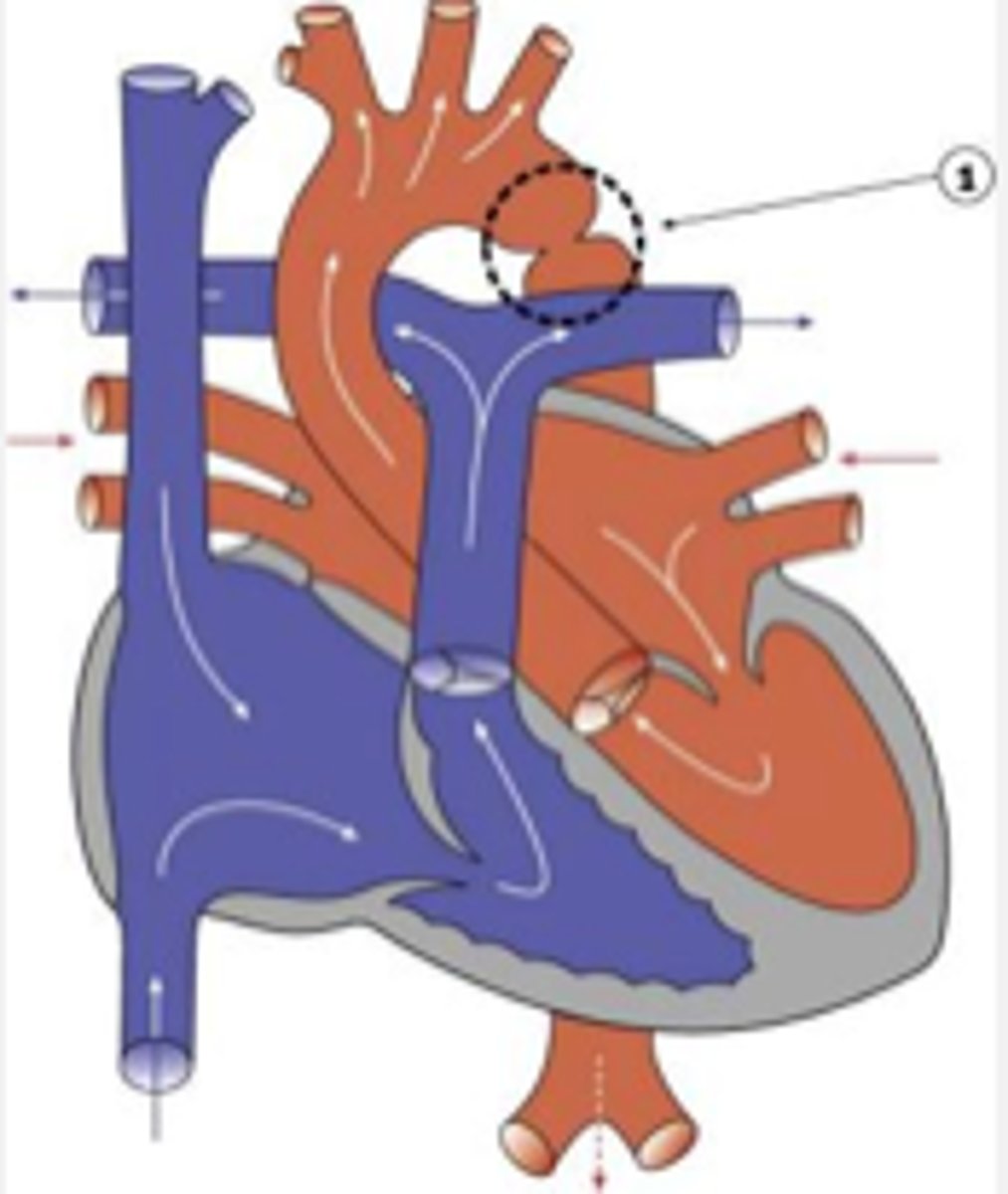
ductus arteriosus
-artery connecting aorta and pulmonary artery
-closes spontaneously around 2-3 weeks after birth
1. high pressure in the aorta
2. low pressure in the pulmonary artery
3. pulmonary blood flow
Patent Ductus Arteriosus (PDA)
Failure of the ductus arteriosus to close after birth, resulting in blood flowing from (1) to (2), which in turn results in a left-to-right shunting of blood and increases (3)
patent ductus arteriosus
-5-10% of all CHD defects
-allows for communication between aorta and pulmonary artery
prematurity, pulmonary HTN and CHD
What are three potential causes of PDA?
prostaglandin inhibitors
(i.e. ibuprofen; Prostaglandin may keep ducts open)
What are babies with PDA typically prescribed to close the ducts?
atrial septal defect
abnormal opening in the atrial septum, between the two upper chambers (right and left atria) of the heart
Normal: oxygenated blood flows from the left atrium into the left ventricle
ASD: oxygenated blood flows from the left atrium into the right atrium (left-to-right shunting)
1. left ventricle
2. right atrium
3. deoxygenated blood
4. lungs
Atrial Septal Defect
Normal: oxygenated blood flows from the left atrium into the (1)
ASD: oxygenated blood flows from the left atrium into the (2) (left-to-right shunting)
In the (2), the blood mixes with (3) and is pumped to the (4), increasing the total amount of blood that's pumped to the lungs, causing damage to pulmonary vessels.
potential problems of ASD
pulmonary HTN, increased risk of stroke, heart dysrhythmias, HF
prevalence of ASD
-approx. 3-10% of all CHD
-females > males, 2:1
ventricular septal defect
-more serious
-abnormal opening in ventricular septum, between right and left ventricles
1. right ventricle
2. deoxygenated blood
3. lungs
Ventricular Septal Defect
Normal: oxygenated blood flows from high pressure in the left ventricle to aorta
VSD: oxygenated blood flows from high pressure in the left ventricle to lower pressure in the (1) where there is (2), creating a left-to-right shunt and increasing blood flow to the (3)
prevalence of VSD
17-37%
obstructive (stenotic) CHD defects
-type of CHD that restrict or obstruct blood flow on the left or right side of the heart
-May all result in HF!
-If a cardiac problem is suspected, take BP in both extremities
pulmonary stenosis
a narrowing of the pulmonary valve or pulmonary artery that results in a back-up of fluid in the right ventricle
aortic stenosis
calcification of aortic valve cusps that restricts forward flow of blood during systole
coarctation of aorta
narrowing of the aorta, resulting in reduced blood flow from the ventricles
coarctation of aorta S/S
-higher pressure in upper extremities and head
headaches, nosebleeds, high BP in upper extremities --> stroke, bounding pulses
-low/weak femoral pulses, cool temperatures, low BPs in lower extremities
may see increased pulse pressures (BP differences bw upper and lower extremities)
cyanotic defects
-types of CHD defects that involve deoxygenated blood mixing w/oxygenated blood
-includes tetralogy of Fallot, transposition of the great arteries, truncus arteriosus, total anomalous pulmonary venous return, tricuspid valve anomalies, and hypoplastic left heart syndrome (HLHS)
pulmonary stenosis, hypertrophy of the right ventricle, ventricular septal defect, overriding aorta
What are the four anatomical malformations in tetralogy of fallot?
ASD, DiGeorge Syndrome (hypocalcemia), hypercyanotic spells
What are three other conditions associated w/tetralogy of fallot?
TET spells
-right ventricular outflow tract obsturction
-occur w/ToF
-w/exertion or agitation, baby turns blue (cyanotic) and hypoxic (O2 sat 65-85%)
-may develop clubbin adn polycythemia
1. Knees to chest
2. oxygen
3. morphine
Nursing Management of TET Spells
Acute
-(1), which increases oxygen and intrabdominal pressure
-give (2) and administer medications, i.e. (3)
-IV fluids
-document
Other
-calm infant
-small, frequent feedings
treatment of ToF
-surgical; primary repair requires bypass, between 3-12 months of age
-if not stable enough, palliative shunt (BT shunt), then complete repair
monitor for HF and serial ECHOs to evaluate residual defects, blood flow
Describe post-op nursing management of surgical treatment for ToF.
transposition of the great arteries
-Aorta arises from the right ventricle and the pulmonary artery arises from the left ventricle
-complete separate systemic and pulmonic circulations
-associated w/ASD, PDA, VSD
-incompatible w/life: cyanosis dependent lesion - depends on adequacy of left to right shunting
1. pulmonary artery
2. deoxygenated
3. pulmonary circulation
4. aorta
5. oxygenated
6. systemic circulation
Transposition of the Great Arteries
On the left side of the heart, blood is getting pumped from the left ventricle to the (1), when normally this would be the aorta. Blood is never getting (2), meaning there is hyper-oxemic (3)
On the right side of the heart, blood is getting pumped from the right ventricle to the (4), when normally this would be the pulmonary artery. Blood is never getting (5), meaning there is hypoxic (6).
cyanosis, tachycardia, tachypnea, poor feeding
What are four S/S of transposition of the great arteries?
Nursing Management of Transposition of the Great Arteries
-monitor vitals
-administer oxygen
-small, frequent meals
-give meds (prostaglandin e) to keep PDA open for PBF
surgical management of Transposition of the Great Arteries
-make ASD increase mixing
balloon atrial septostomy
-arterial switch operation (ASO)
Cardiac Cath: PreOp
-height and weight
-allergy history
-assess diaper area
-teaching parent and child as developmentally appropriate
-oxygen levels and peripheral pulses - bilaterally w/ documentation
Cardiac Cath: PostOp
-VS q15
-pulses/temperature of extremities
pulses will be weaker and colder on operated leg
-HR: one full minute
-dressing: hematoma/bleeding
-pressure dressing
-immobilize affected extremity; keep straight
4-6 hr; sedatives given
-pain control
-discharge instructions
-support respiratory function
-monitor fluid and electrolyte imbalance
-bathing limited to a brief shower
-assess for bleeding if child is tachycardic/hypotensive
Heart Failure
lesions causing volume or pressure overload
1. feeding
2. cardiomegaly
3. galloping
Manifestations of Pediatric Heart Failure
-(1), poor weight gain
-mild tachypnea, tachycardia
-(2), liver/spleen enlarged
-(3) rhythm
-poor perfusion, edema
-mottling, cyanosis, pallor
1. dehydration
2. BP; hyperkalemia
3. contractility
Medical Management for Pediatric HF
-diuretics, which help reduce preload
monitor for (1)
-ACE inhibitors, which help reduce afterload
monitor for (2) and (2)
-ionotropes to increase (3)
feeding the infant w/congestive heart failure
-feed in a relaxed environment
-small, frequent feedings
-hold infant in upright position
-monitor for feeding intolerance
-consult dietician and speech / OT
-support breast-feeding/breast milk
educating parents about HF
-S/S of HF
-increased cyanosis
-dehydration
-infection
-decreased nutritional intake
-activity levels
-medications
before
Parent/caregiver must be educated about digoxin and be monitored preparing/administering medication (1) leaving hospital.
digoxin toxicity
-Cholinergic—nausea, vomiting, diarrhea, blurry yellow vision (think van Gogh), arrhythmias, AV block.
-Can lead to hyperkalemia, which indicates poor prognosis.
1. 20-30 min
2. vomits
3. fevers, urine output
4. apical
Digoxin Administration
-Regular schedule: (1) before feeding
-don't mix with feeding
-don't repeat dose if infant (2)
-Report: (3), decreased (3), vomiting, green, yellow hazing in eyes
-Count (4) for one minute: if infant HR < 90 or child HR is < 70, HOLD DOSE!
Digoxin Administration
-requires 2nd nurse to check
-must monitor serum values of Digoxin