Enteral/Parenteral Nutrition in Foals and Adult Horses VCNA
1/43
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
44 Terms
How long can a healthy, adult horse tolerate food deprivation (protein/calorie malnutrition [PCM] or simple starvation) for with few systemic effects?
72 hours
Glucose Sources During Starvation
During the first hours to days of starvation, glycogen stores are used from various tissues (liver, kidney, muscle) for glucose production
As glucose becomes limited, many body tissues begin to rely on fatty acid oxidation and the production of ketone bodies as energy sources
Glycerol produced from lipid degradation, lactate from the Krebs cycle, and amino acids provided from muscle tissue breakdown continue to be used for gluconeogenesis to provide energy to glucose-dependent tissues (CNS and RBCs)
This response to starvation correlates with an increase in circulating levels of growth hormone, glucagon, epinephrine, leptin, and cortisol and a decrease in insulin and thyroid hormones
Hunger Drive and Metabolism in Protein/Calorie Malnutrition
There is an increased drive to eat and a decrease in energy expenditure
Metabolism slows in an effort to conserve body fuels, and the body survives primarily on fat stores, sparing lean tissue until such a time as refeeding occurs
Response to Protein/Calorie Malnutrition in the Neonate
The healthy newborn foal should have neough liver glycogen to support energy needs for several hours of life
Glycogen stores at birth can vary significantly with illness or prematurity
Lack of nutritional reserves can result in hypoglycemia and hypothermia and quickly affect the ability to maintain normal function and behavior
Metabolic Response to Injury in the Horse
The metabolic response to injury is characterized by an increased metabolism and the onset of a catabolic process leading to excessive breakdown of tissue proteins, which are used as metabolic fuel
Insulin resistance develops and hyperglycemia may occur despite the absence of food intake
Designed to provide endogenous substrates for gluconeogenesis, wound healing, immune cell replication, and synthesis of acute phase
Long-term muscle breakdown results in loss of muscle strength, visceral orang dysfunction secondary to loss of structural and enzymatic proteins, impaired wound healing, immunosuppression, and compromise to overall health
Effects of Nutritional Response to Catabolic State
Nutritional supplementation will reverse the catabolic processes occurring during simple starvation, but will not completely reverse those occurring during metabolic stress because as long as tissue injury persists, catabolic processes are maintained
Goals of Nutritional Support in Critical Illness
Save life
Maintain muscle mass
Preserve and improve cellular and tissue function
Speed recovery
Indications for Nutritional Support
Patients with an increased metabolic rate (young growing animals), a history of malnutrition or hypophagia, underlying metabolic abnormalities that could worsen with food deprivation (equine metabolic syndrome, hyperlipidemia), and disorders such as severe trauma, sepsis, burns, or strangulating bowel obstruction that result in an increased energy demand
Underweight horses require nutritional support earlier
Obese or overconditions individuals, particularly pony breeds, miniature horses, and donkeys, individuals with Cushings or EMS, and pregnant or lactating mares are at risk for hyperlipidemia and should receivenutritional support to try to prevent or minimize hyperlipidemia
Benefits of Enteral Feeding
Provides most of the nutrition to the gut
Has been shown to improve gut barrier integrity, gut mass, protein content, gut motility, and function
Metabolic Needs of Sick Patients
May fall more closely within the range of the resting to maintenance energy requirements or normal healthy individuals
Exceptions are individuals with extreme trauma, burns or severe sepsis, surgical conditions that require intestinal resection, and large areas of devitalized tissue (eg clostridial myositis patients that undergo multiple fasciotomy procedures)
Resting Energy Requirements
The amount of energy needed to maintain an individual (no weight gain or loss) in a thermoneutral environment without the metabolic demands of digestion
Maintenance Energy Requirements
The amount of energy needed to maintain an individual (no weight gain or loss) in a thermoneutral environment with the metabolic demands of digestion
What % higher than resting energy requirements are maintenance energy requirements?
About 30%
Estimate for Resting Energy Requirement
22-23 kcal/kg/day for the average full sized horse
Estimate for Maintenance Energy Requirement
30-35 kcal/kg/day
Protein Requirement of the Healthy Adult Horse
0.5-1.5 g/kg/day
Protein Requirement for the Growing Foal
7 g/kg/day
Lysine requirements of growing horses are higher than for mature horses
Protein Considerations in Critically Ill Horses
During critical illness or severe injury, protein catabolism and utilization of amino acids as a source of fuel continue despite the presence of energy stores so recommended to provide the higher end of the estimated need
Supplementation of nonessential amino acids that may improve the outcome in illness
Glutamine supplementation has been shown to improve clinical outcome
Used as a fuel for enterocytes and other rapidly dividing cells
Branched chain amino acids and arginine supplementation
Arginine is a precursor to nitric oxide, is an important vasodilating agent, upregulates immune function and secretion of several hormones, and may reduce ischemia-reperfusion injury
Advantages of Complete Pelleted Feeds
Relatively inexpensive and well balanced for the maintenance requirements of an adult horse
Contain fiber, which is beneficial for intestinal motility, increasing colonic blood flow, enzymatic activity, and colonic mucosal cell growth and absorption
Disadvantages of Complete Pelleted Feeds
Difficulty involved in giving them via NG intubation
Disadvantages of Powdered Commercial Diets
Cost over complete pelleted diets
Associations with Liquid Diets in Horses
Studies in healthy horses have found that the feeding of liquid diets is associated with decreased intestinal transit time and decreased prececal starch and fat digestion
Avoid high starch (>25% DE) and high fat (>6% DE) diets
Use highly digestible carbohydrate sources (processed corn starch
Similarities between Mare’s and Goat’s Milk
The major whey protein in both goat’s and mare’s milk is B-lactoglobulin
The major whey protein in cow’s milk is a-lactoglobulin
Recommendations for Milk Replacer for Foals
Choose a replacer that is developed for foals rather than all-species
Use replacers that contain whey protein rather than other protein sources because of digestibility concerns
Provide a source of fresh water as they are much higher in salt than natural mare’s milk and hypernatremia can develop if a water source is not provided
Metabolic Demands of a Sick Neonates
5-10% of its bodyweight (500-100 kcal/kg/d)
Advantages of Parenteral Nutrition
Ability to supply nutrition when the enteral route is unavailable
Ability to tailor the types of nutrition provided for each individual animal
Decreases weight loss, particularly lean body mass, and improves wound healing, immune function, and outcome in human and animal studies when the enteral route cannot be used
Candidates for Parenteral Nutrition
In the adult horse, to supply partial nutrition when oral intake is insufficient or the oral route cannot be used
Individuals that are recumbent or dysphagic, have GI disease, or have pre-existing protein/calorie malnutrition
Disadvantages of Parenteral Nutrition
Expense
Loss of the beneficial effect of enteral nutrition on maintaining the gut function and mass
What are carbohydrates and lipids used for in parenteral nutrition?
To meet the horse’s energy needs
What are amino acids used for in parenteral nutrition?
Wound healing, immune function, and muscle maintenance
What are lipids for parenteral nutrition composed of?
Come in 10%, 20%, and 30% emulsion
Composed primarily of soybean oil (or safflower), egg yolk phospholipids, and glycerin
When should lipids be added to the parenteral nutrition solution?
Last, to avoid destabilization of the emulsion because of an acidic environment
What % of nonprotein calories can lipids provide in parenteral nutrition?
Up to 30-60% of the nonprotein calories
When is adding lipids to parenteral nutrition beneficial?
In patients with persistent hyperglycemia or hypercapnia, reducing dependency on glucose as the principal energy source
When should lipids be avoided in parenteral nutrition?
In horses with known hyperlipidemia or in horses suspected of being lipid intolerant
Lipid intolerance can be seen in patients with systemic inflammation, sepsis, or underlying metabolic derangements
What should the ratio of nonprotein calories (NPC) to nitrogen be in the final solution?
At least 100:1 to limit the use of protein as an energy source
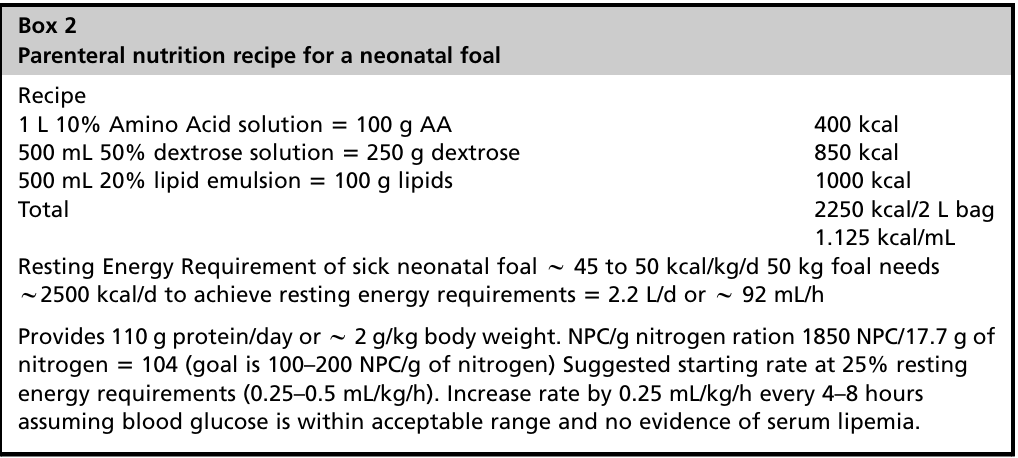
Parenteral Nutrition Recipe for a Neonatal Foal
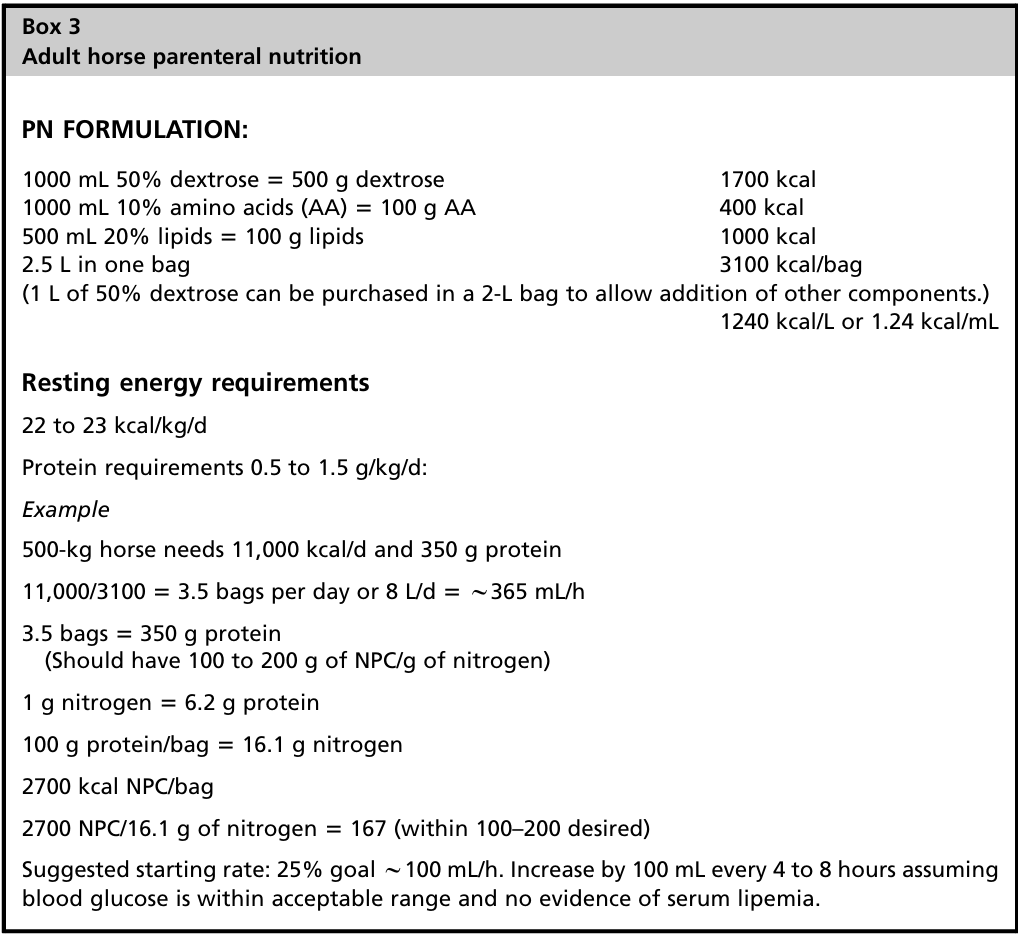
Adult Horse Parenteral Nutrition Recipe
What are additional components that can be added to parenteral nutrition or given separately to supplement?
Electrolyte solutions and vitamin and mineral supplements
Recommended to supplement water-soluble B vitamins daily as deficiencies can exacerbate problems associated with refeeding
Some vitamins are best given orally (vitamins C and E) or added to separate crystalloid solutions (B vitamins)
Fat-soluble vitamins suchs ad E, D, and A are stored in body tissue so they are generally not supplemented unless an individual is off feed for a prolonged period or has an illness that may result in greater use or need
Antioxidant benefits of vitamin E may make it worth providing oral supplementation in early illness
Minerals, if required, are best supplemented in separate crystalloid solutions, as divalent cations may destabilize lipid emulsions
Infusion Rate for Parenteral Nutrition
Generally start with an infusion rate targeting approximately 25% of the calculated goal
If blood glucose concentrations are within reference ranges, then the rate can be increased by an additional 25% every 4-8 hours
Complications Associated with Hyperglycemia
Hyperglycemia both at admission and during hospitalization has been associated with an increased risk of complications including infections and renal failure, longer hospital stays, and reduced survival in humans and horses with critical illness or injury
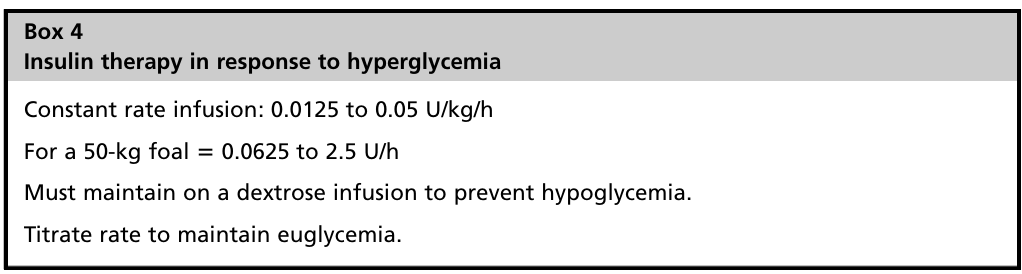
Insulin Therapy in Response to Hyperglycemia
Complications Associated with Lipid Infusions
Lipid infusions have been associated with allergic reactions, hyperlipidemia, alterations in liver function, and fat embolism
The risk of fat embolism is higher in larger droplet emulsions or in emulsions that have been stored too long and have begun to destabilize
Thrombocytopenia, coagulopathy, fat embolization ,thrombocytopenia, and alterations in cellular immunity are reported with lipid infusions
Triglyceride levels and platelet counts should be monitored regularly when lipids are added to parenteral nutrition solutions
Complications Associated with Parenteral Nutrition
Hyperammonemia and elevations in serum urea nitrogen level from excess protein catabolism, hypercapnia caused by excess carbohydrate metabolism, thrombophlebitis caused by hypertonicity and pulmonary embolism (thought to be caused by destabilized lipid emulsions), and sepsis