Principles of Antimicrobial Therapy
1/19
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
20 Terms
Why are heavy metals antimicrobial?
mercury binds to (and damages) many proteins non-specifically (both ours and microbial ones)
so antimicrobial (yay!) but also toxic (noooo!)
What is the principle one which every antimicrobial works?
to be more toxic to the microbe than to us :)
what different types of treatments require antimicrobials?
bacterial (antibiotics)
fungal
viral
and helminth/protozoan
*different types of microbials are required for each
therapeutic dose
amount of medication required to produce the desired effect in treating the disease
toxic dose
specific quantity of a substance that can cause harmful effects to the host
therapeutic index
calculated from the ratio of the toxic dose to the therapeutic dose
higher therapeutic index = safer drug
what is the easiest way to make a highly effective and safe drug?
to target cell processes that humans do have
ex: many antimicrobials target the cell wall (create pores for lysis) because human cells do not have cell walls
Penicillin
first antibiotic that is selectively toxic for bacteria
targets crosslinking of cell wall on bacteria
weakened cell wall → lysising
modification to penicillin helps target other bacteria and change how we can administer it
Bacteriostatic
keep bacteria from growing (when drug is gone bacteria will resume growth)
bacericidal
kill bacteria
ex: penicillin
60:40 rule
cure is 60% immune system and 40% antibiotic
fully functioning immune system will provide optimal outcome for antimicrobial therapy
pharmacokinetics (PK)
what the body does to the drug
Pharmacodynamics (PD)
what the drug does to the pathogen
Questions to ask to figure out what drug to use:
What do we know about the bacteria?
what is this bacteria and what antibiotics is it susceptible to?
PD understanding
culture and antibiotic sensitivity data
if there is not antibiotic sensitivity data, choose drug that would typically kill the organism
What do we know about the host?
PK understanding
how sick are they?
immunosuppressed?
are there host factors that might alter pharmacokinetics?
obesity, renal or hepatic impairment
What kind of infection is it? Where does the drug need to go?
ex: meningitis needs to get all the way to the central nervous system but for intestinal infections, absorption may not be required and for intracellular pathogens antibiotic must get inside mammalian cells
What do we know about how the drug behaves?
a. route of administration needed
b. distribution (circulatory system, diffusion into tissues)
c. removal (metabolism or excretion)
d. next dose?
Should antimicrobials be used in combination?
yes if:
we don’t know whats causing the infection but know we need to kill it
more than one kind of microbe is causing the infection (polymicrobial)
prevents emergence of resistance through mutation
synergy (two antibiotics will work better when combined)
combining will allow reduction of dose of a toxic antimicrobial
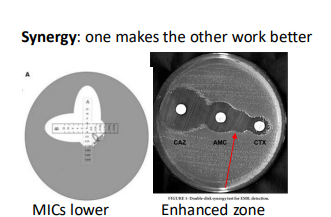
antibiotic synergy
one makes the other work better
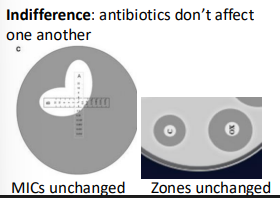
antibiotic indifference
antibiotics don’t affect one another
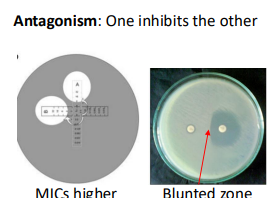
Antibiotic antagonism
one inhibits the other
Benefits of Antibiotics
shorter, less severe infections
cure infections
prevent infections (prophylactic)
reduced morbidity and mortality
Drawbacks of Antibiotics
side effects
allergies
emergence of resistance
secondary infections