L13 & 14 small animal ectoparasites
1/50
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
51 Terms
Fleas Introduction/Importance
Spread all over the world
The most important ecto-parasites of dogs and cats;
Intermediate host for Dipylidium caninum, Acanthocheilonema reconditum;
Can transmit bacteria
Ctenocephalides felis

Fleas Significance for humans
Ctenocephalides spp. can bite humans, especially when:
• Pets are temporarily removed;
• Flea populations are large.

Ctenocephalides spp.
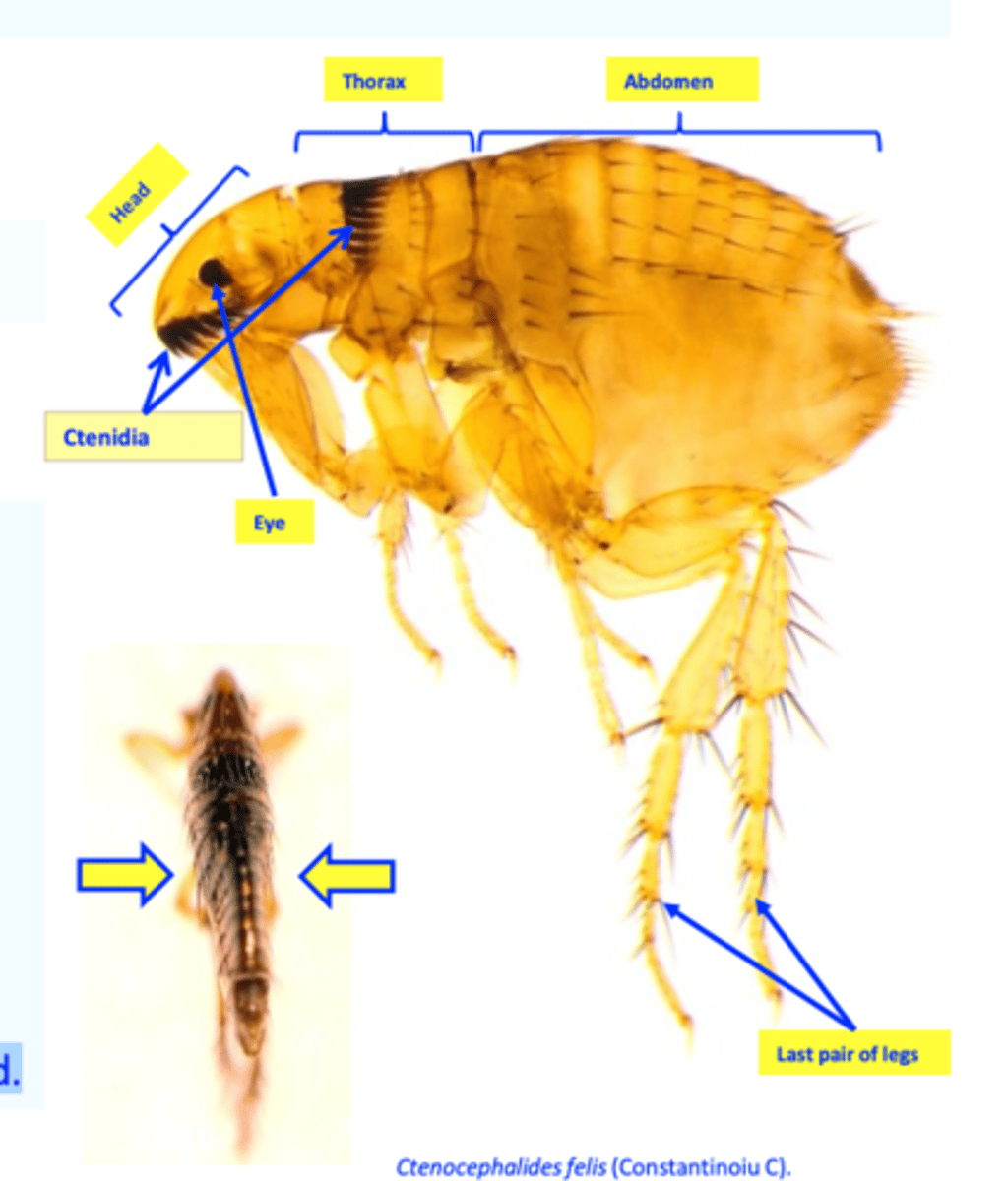
Morphology
Ctenidia
Up to 2.5 mm long, brown/black, flattened laterally;
Body made up of head, thorax and abdomen;
Genal (7-8 spines) and pronotal (16 spines) ctenidia (combs)
Eyes present;
Legs: developed, 3rd pair most developed.
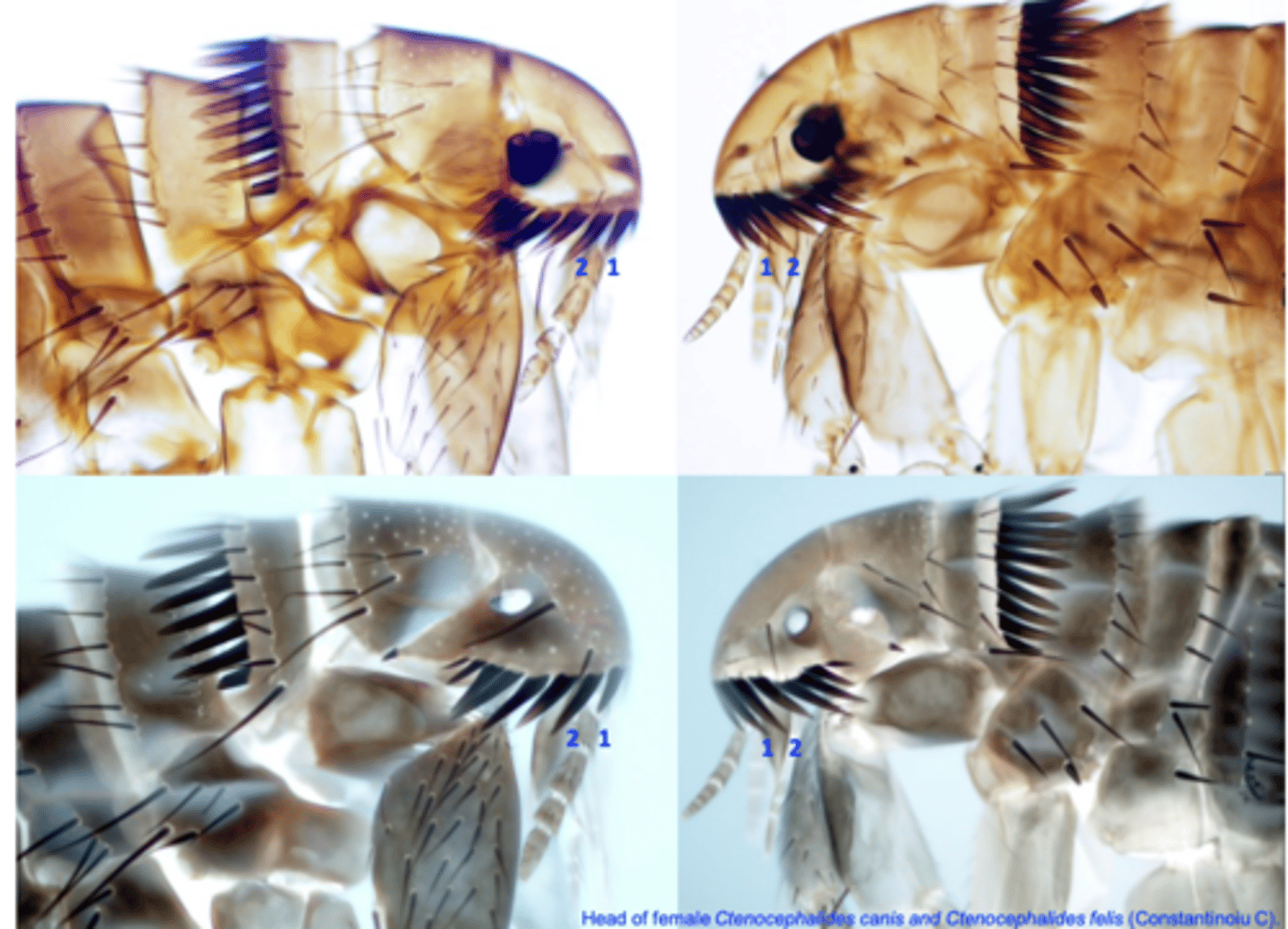
Morphology: Ctenocephalides felis vs C. canis
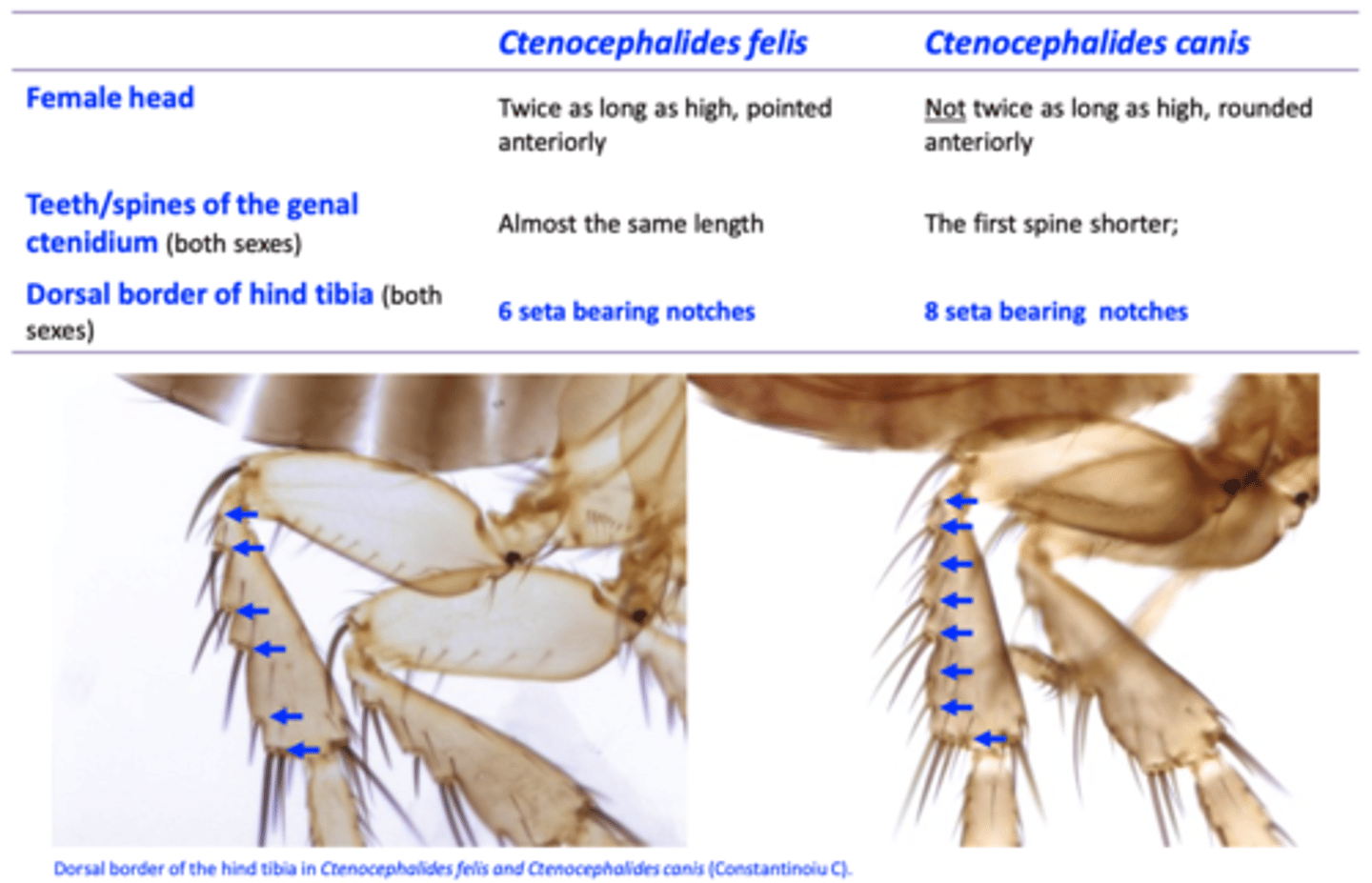
Head of female Ctenocephalides canis and Ctenocephalides felis
Ctenocephalides spp. Feeding
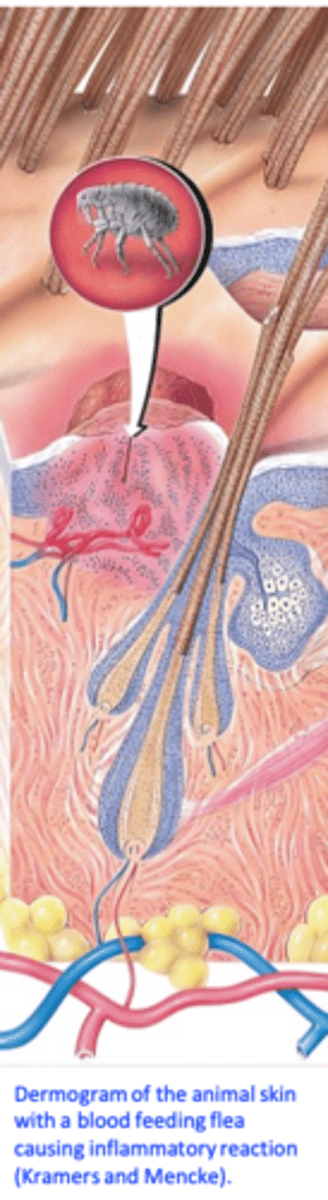
• The adult fleas feed on blood (piercing-sucking mouth parts);
Once on a host fleas start feeding within minutes
Fleas ingest more blood than they need => nutrition for larvae
• 220 females might consume 10% of an 0.45 kg kitten’s blood/day => anemia;
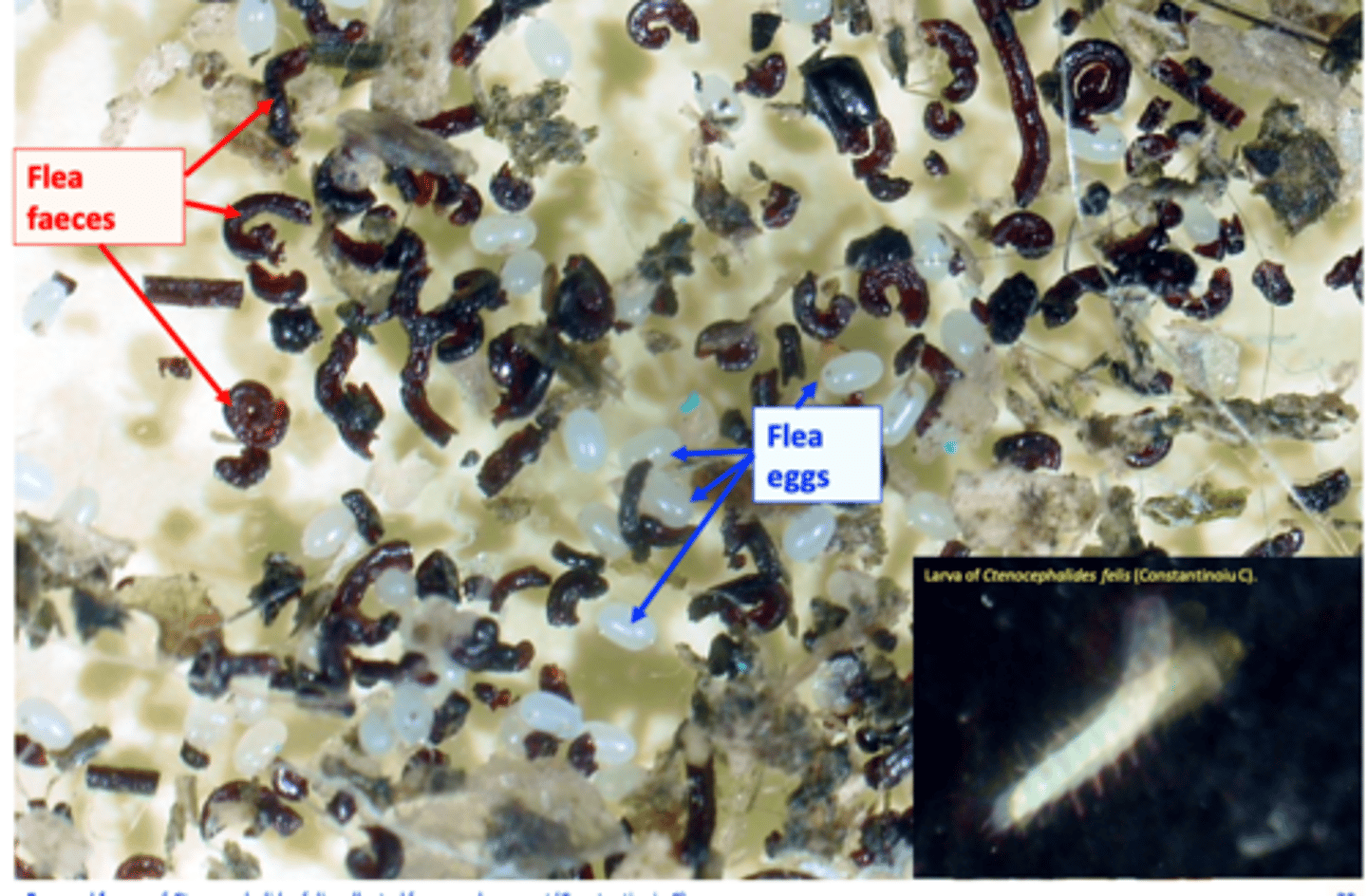
Larvae feed on adult fleas faeces, each other (cannibalism) and egg shells (chewing mouthparts).
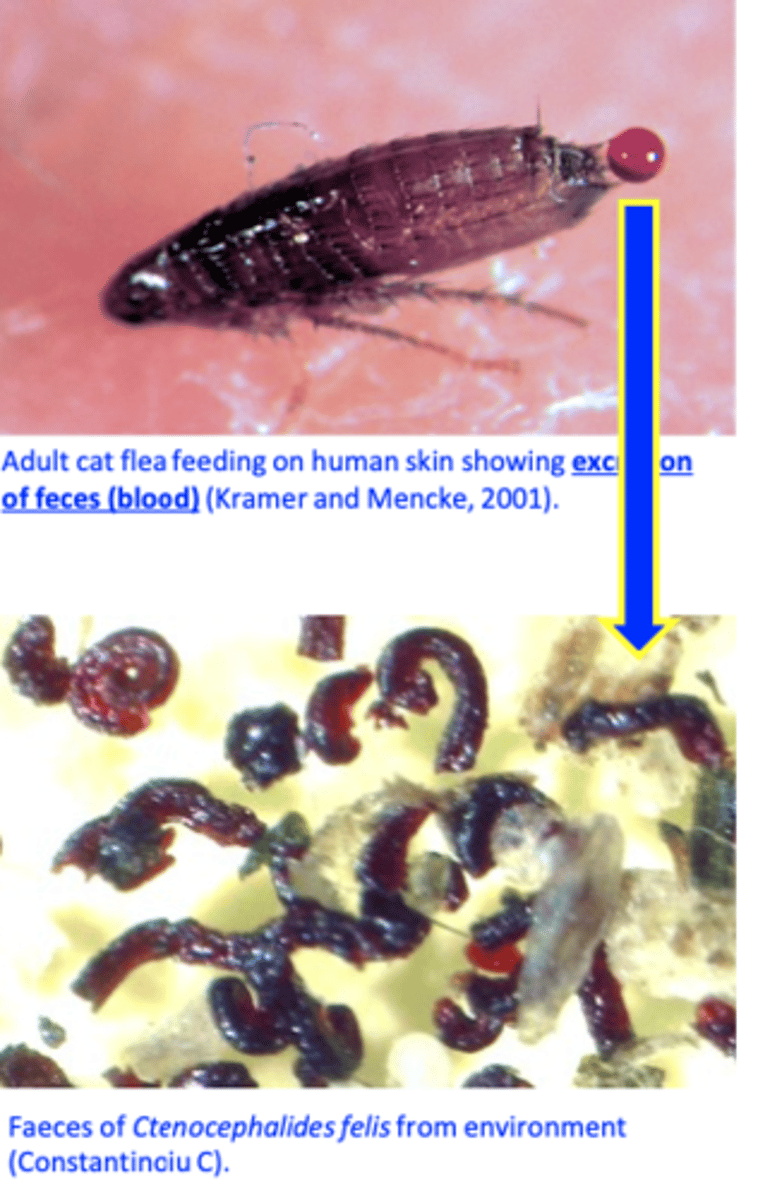
Ctenocephalides spp.: Feeding image
Ctenocephalides spp. Life cycle
Adults: permanent ectoparasites;
Eggs: laid on the host but fall in the
environment;
Larvae: develop in the environment;
Pupae: develop in the environment;
Pre-emerged adults: environment
Host environment
• Bedding and carpeting
• Backyard
• Garage, porch, under the house
• Parks
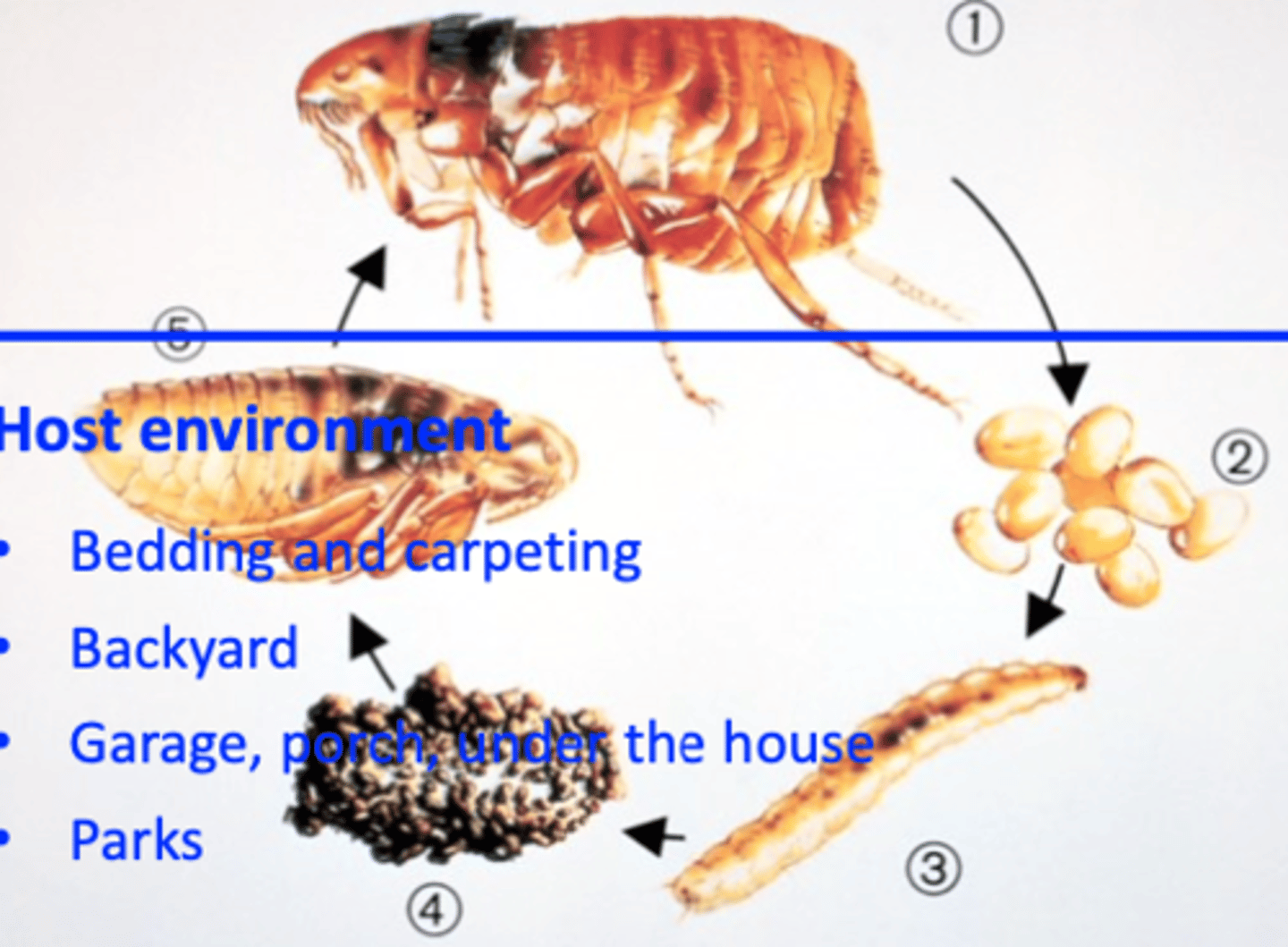
Ctenocephalides spp.: Adult stage
• Permanent parasites, less than 15 % would leave the host => the usual way of acquiring fleas: from the environment
• Grooming is very important in parasite-host relationship

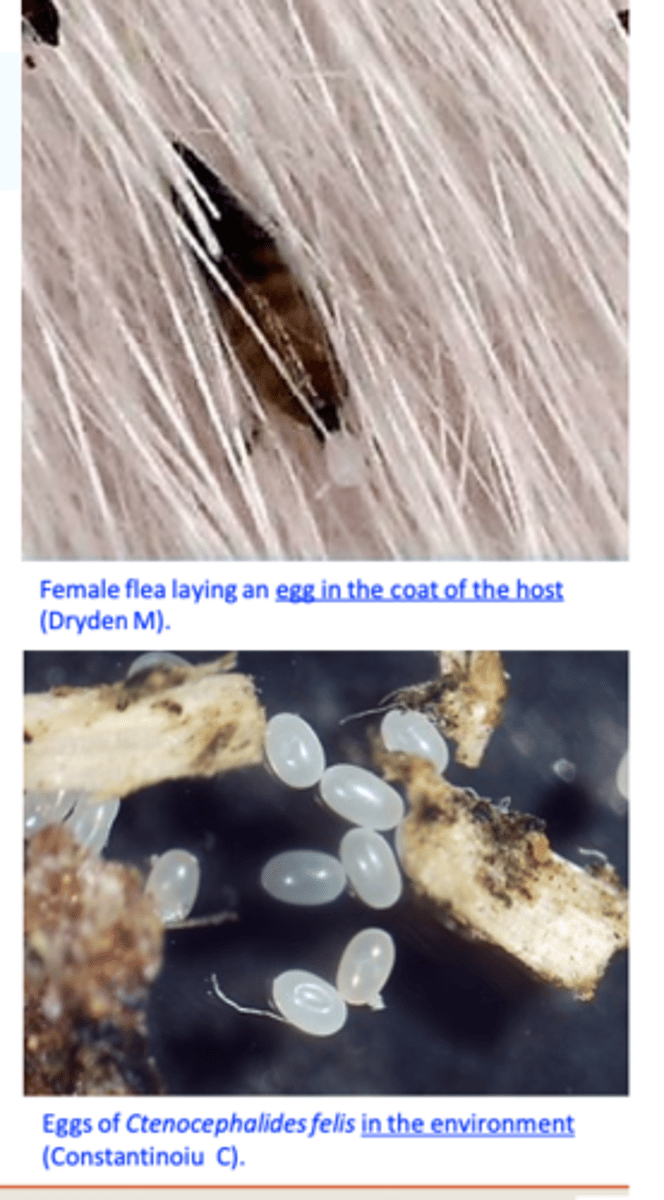
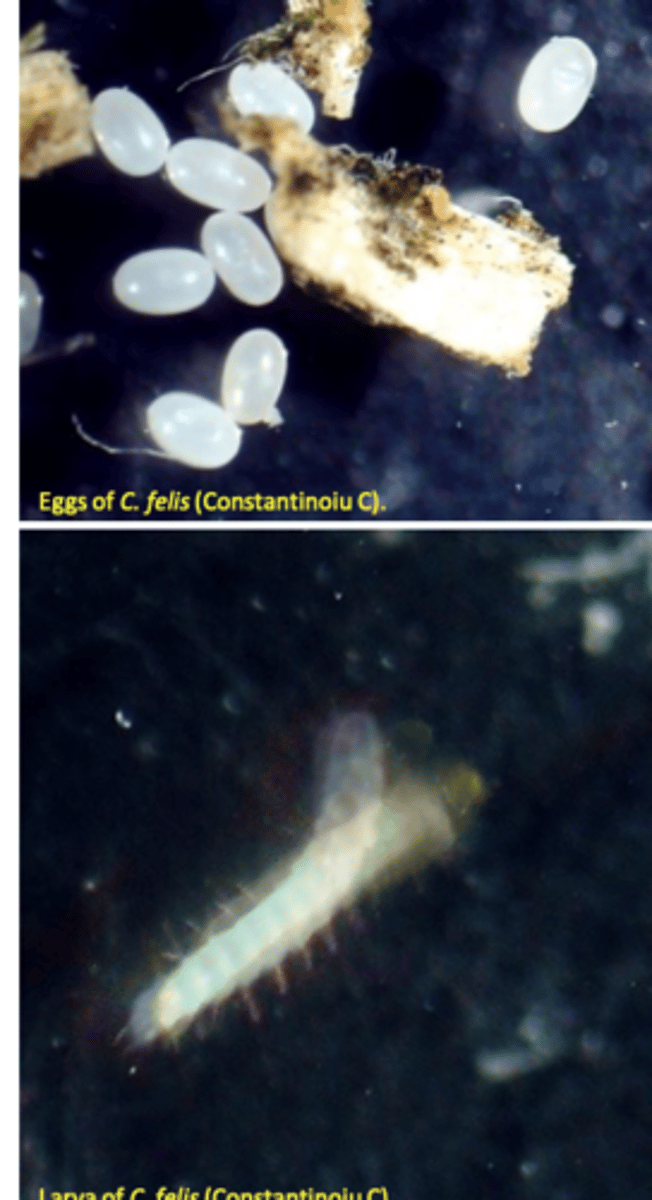
Ctenocephalides spp.: Eggs
Females begin laying eggs 24 to 36 hours after first blood meal
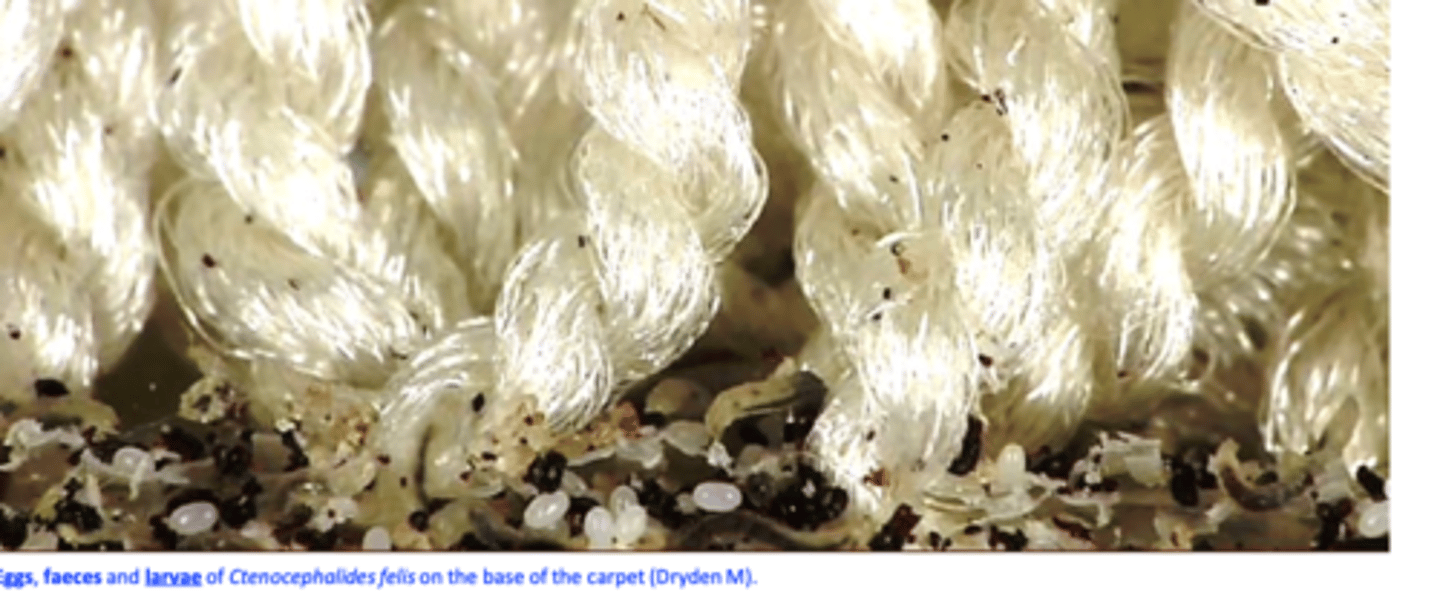
Most eggs fall off the host within 8 h they accumulate where pets sleep and rest;
• Favourable conditions for development: relative humidity >50%, temperature around 25° C;
Ctenocephalides spp: Larvae
• Most larvae develop at the base of carpet: inaccessible to many insecticides;
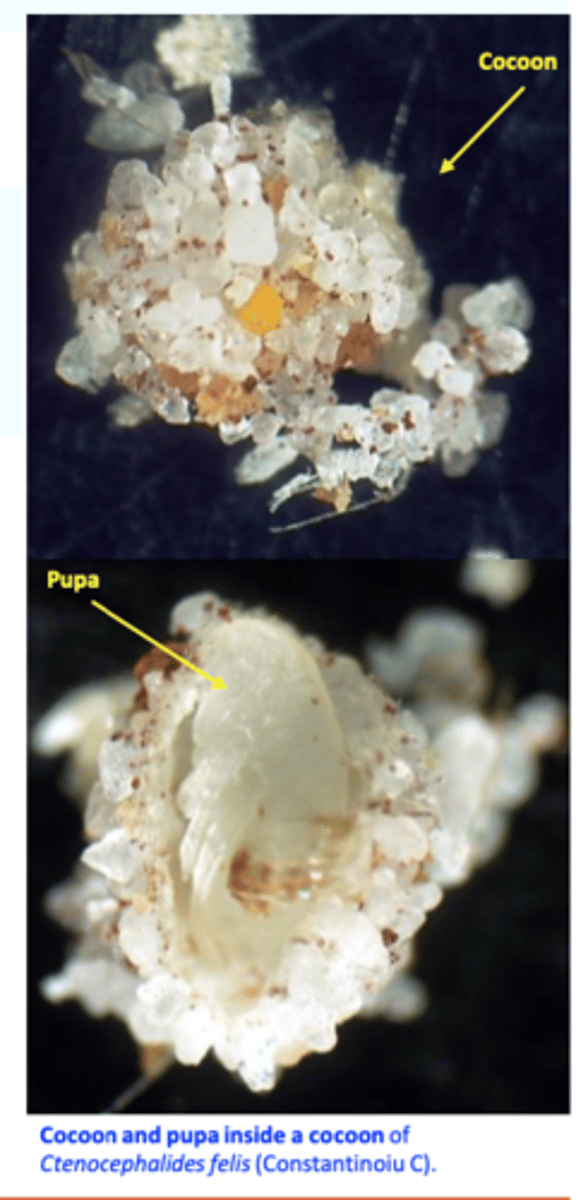
Ctenocephalides spp: Pupae
• L3 spins a silk like cocoon in which it turns into a pupa (time to build 5 - 14 days);
• Best protected and resistant life stage;
Ctenocephalides spp.: Pre-emerged adults
• The “waiting stage”, ideal for survival during the absence of hosts;
• Emergence after 10 days or 6 months (known as “the pupal window”) problems in control;
• Factors responsible for adult emergence: host stimuli:
- pressure, heat, light, air currents
Ctenocephalides spp. Epidemiology
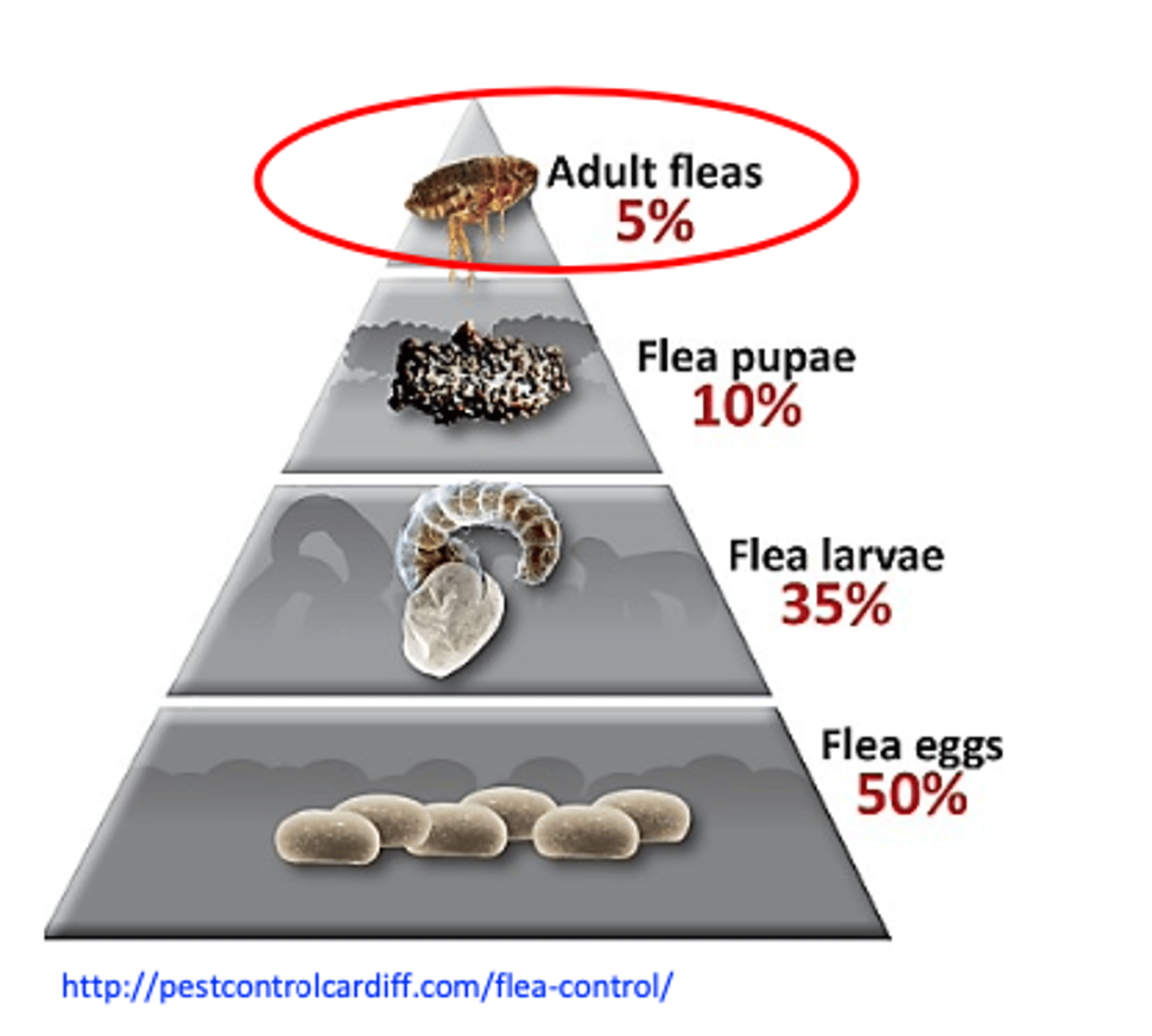
About 5% of the flea population live and feed on the animals, the rest (eggs, larvae & pupae) is in the environment;
Ctenocephalides spp. can feed on many host species
• The houses offer conditions for the life cycle to be completed all year around;
Pre-emerged adults can survive long time within the cocoon (up to 6 months): ‘pupal window’;
• Infestation usually is carried out with fleas from the environment
• Sites of infestation: home, garage, yard, under house, parks etc;
The flea populations and the prevalence of infestations with fleas depend on the season => higher prevalence during the spring and summer;
Ctenocephalides spp. Effect on the host 1
1) Irritation• Physical presence of the fleas and their movement;
• Action of sucking blood (the flea bite is seen as a red spot with a halo varying in width and elevation).
• Injection of saliva
Ctenocephalides spp. Effect on the host 2
2) Anemia from blood loss
In non-allergic dogs clinical signs and skin lesions are minimal
- Pruritus, scratching, alopecia, chewing, have tapeworms etc
Ctenocephalides spp. Effect on the host 3
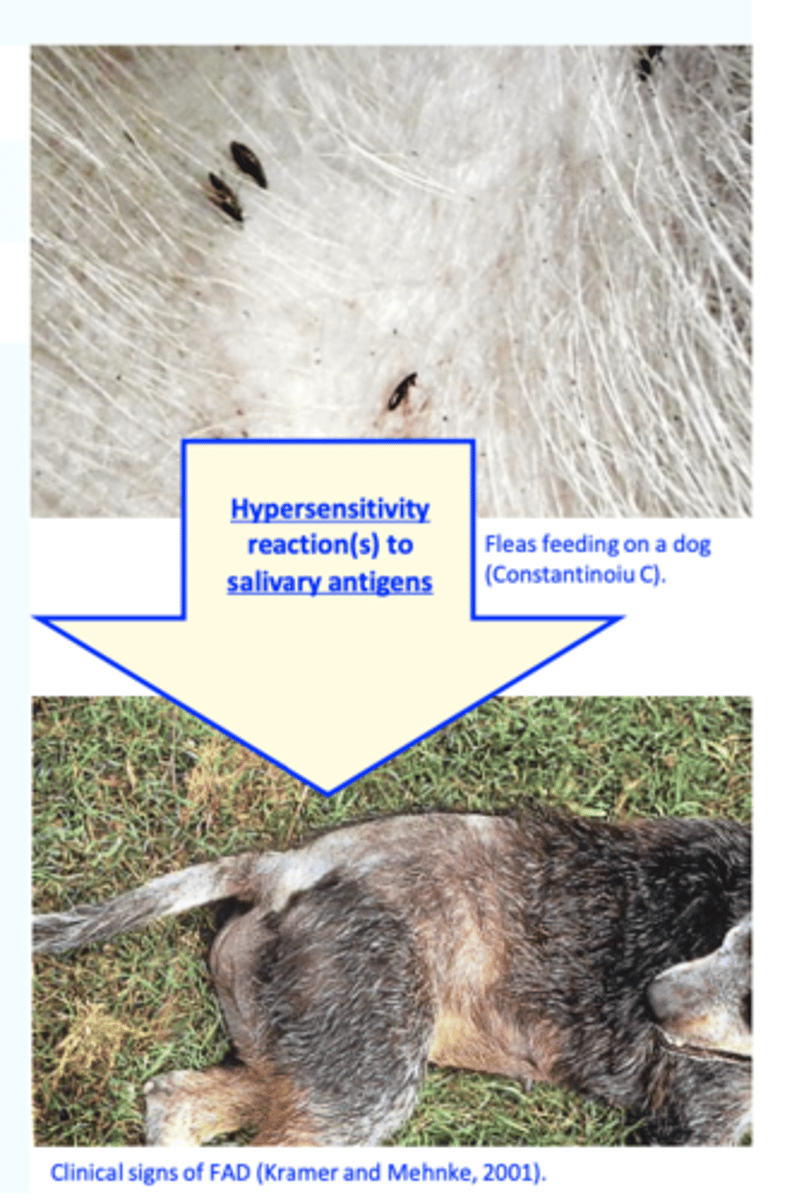
3) Flea allergy dermatitis (FAD)
• Most, if not all dogs, become allergic to salivary antigens of fleas;
Type I (immediate, IgE mediated => mast cell degranulation);
Type IV (delayed, cell mediated – T-DTH)
Cutaneous basophil hypersensitivity
Ctenocephalides spp pathogenesis depends on
• Genetic predisposition to develop allergic diseases (dogs with other allergic diseases are at high risk);
• The numbers of fleas feeding and amount of antigen injected (one flea enough?);
• Frequency of flea exposure – intermittent exposure favours the development of the FAD while continuous exposure favours immune tolerance;
• The age at which first exposure occurs - early exposure probably protects against the development of FAD;
• Presence of secondary or other concurrent skin disease;
• Effects of previous or current treatments;

Ctenocephalides spp. Clinical signs of FAD 1
FAD can occur in dogs of any age but the most common age of onset is 2 to 5 years (occasionally it may
be seen in very old dogs and cats or those as young as 6 months);
No sex or breed predisposition;
In temperate climates FAD is typically worse in
the summer and fall (in warm climates the problem may be non- seasonal);
• The dermatitis is typically confined to the dorsal lumbosacral area, forming a typical triangular shape;
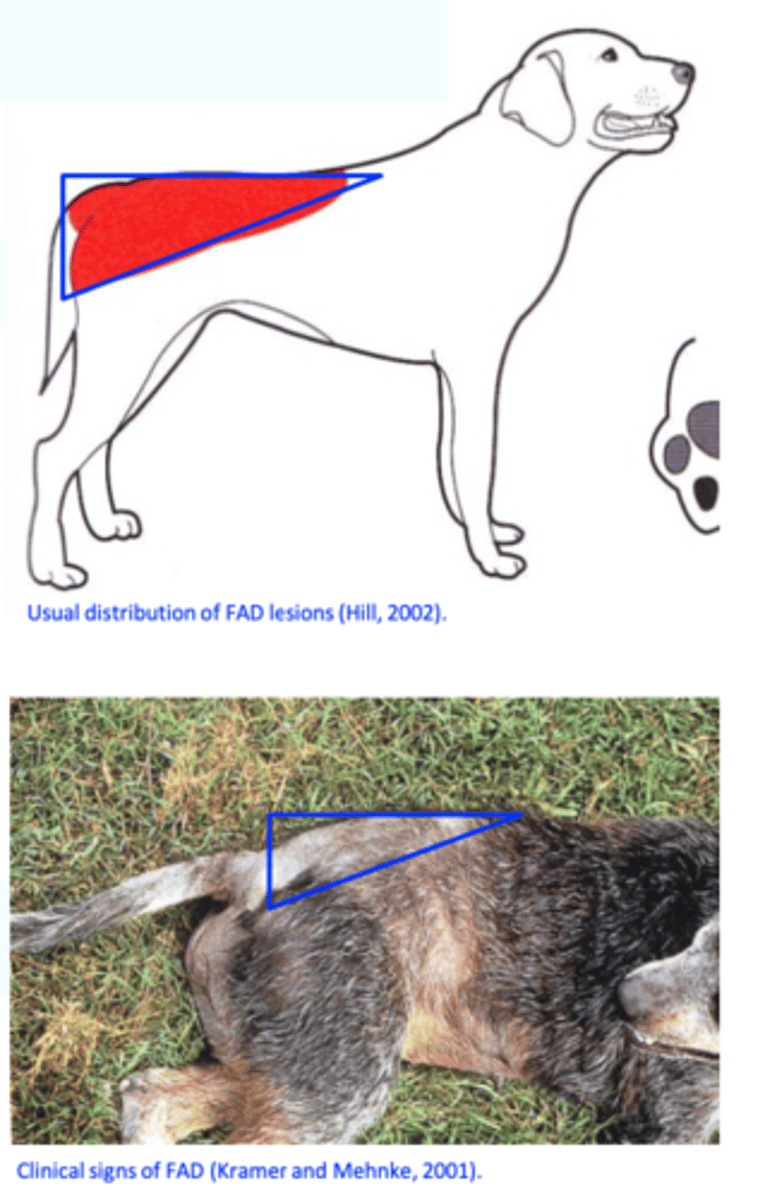
Ctenocephalides spp. Clinical signs of FAD 2
Small pruritic, erythematous wheal can be seen at the flea bite site;
Develops into a pruritic papule that might be short lived being
disturbed by self-trauma;
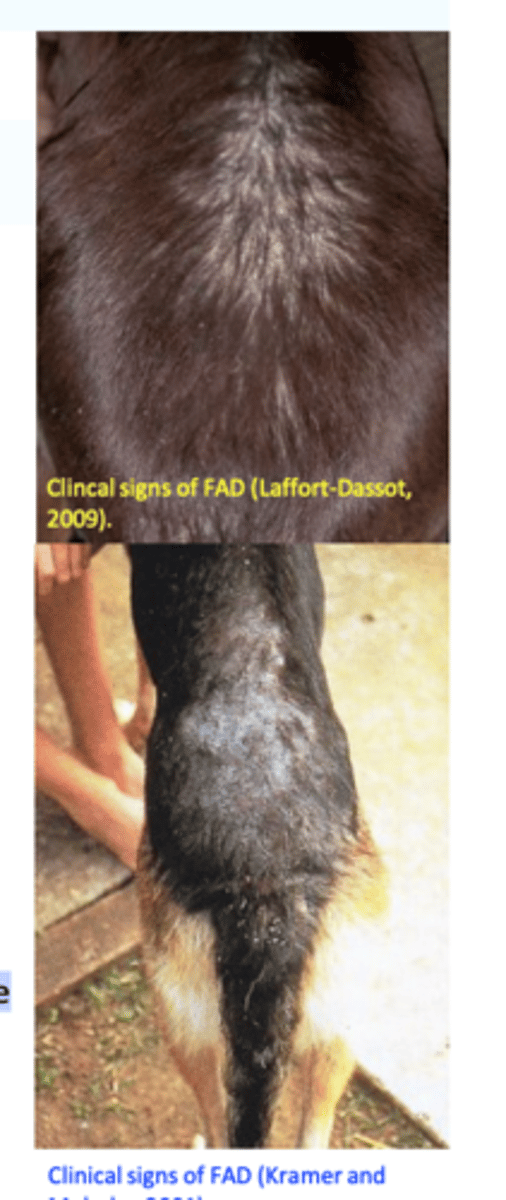
Pruritus and repeated self trauma, chewing, licking => diffuse erythema, excoriations, alopecia, stubbed or broken hairs, crusts etc;
The dogs try to bite or chew at the areas where fleas are/bite seem to hunt the fleas down in their hair coat (nibbling/corncob biting);
Ctenocephalides spp.
Clinical signs of FAD in dogs
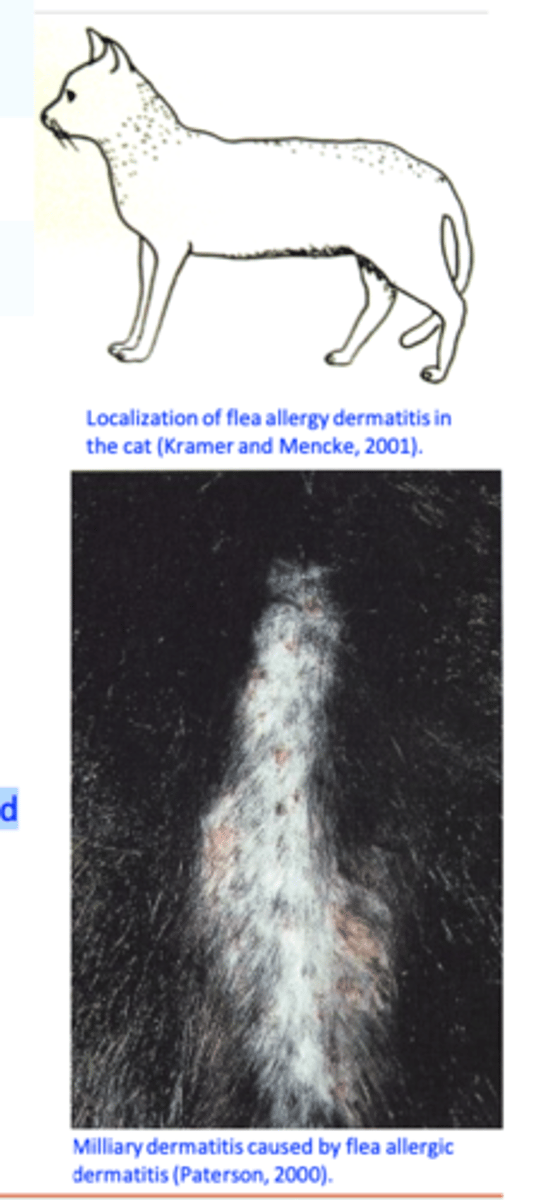
• Pyotraumatic dermatitis
Ctenocephalides spp.
Clinical signs of FAD in dogs
In time, lichenification and hyperpigmentation, crusts and scales develop;

Ctenocephalides spp.
Clinical signs of FAD in dogs
• Fibropruritic nodules
• Secondary infections;

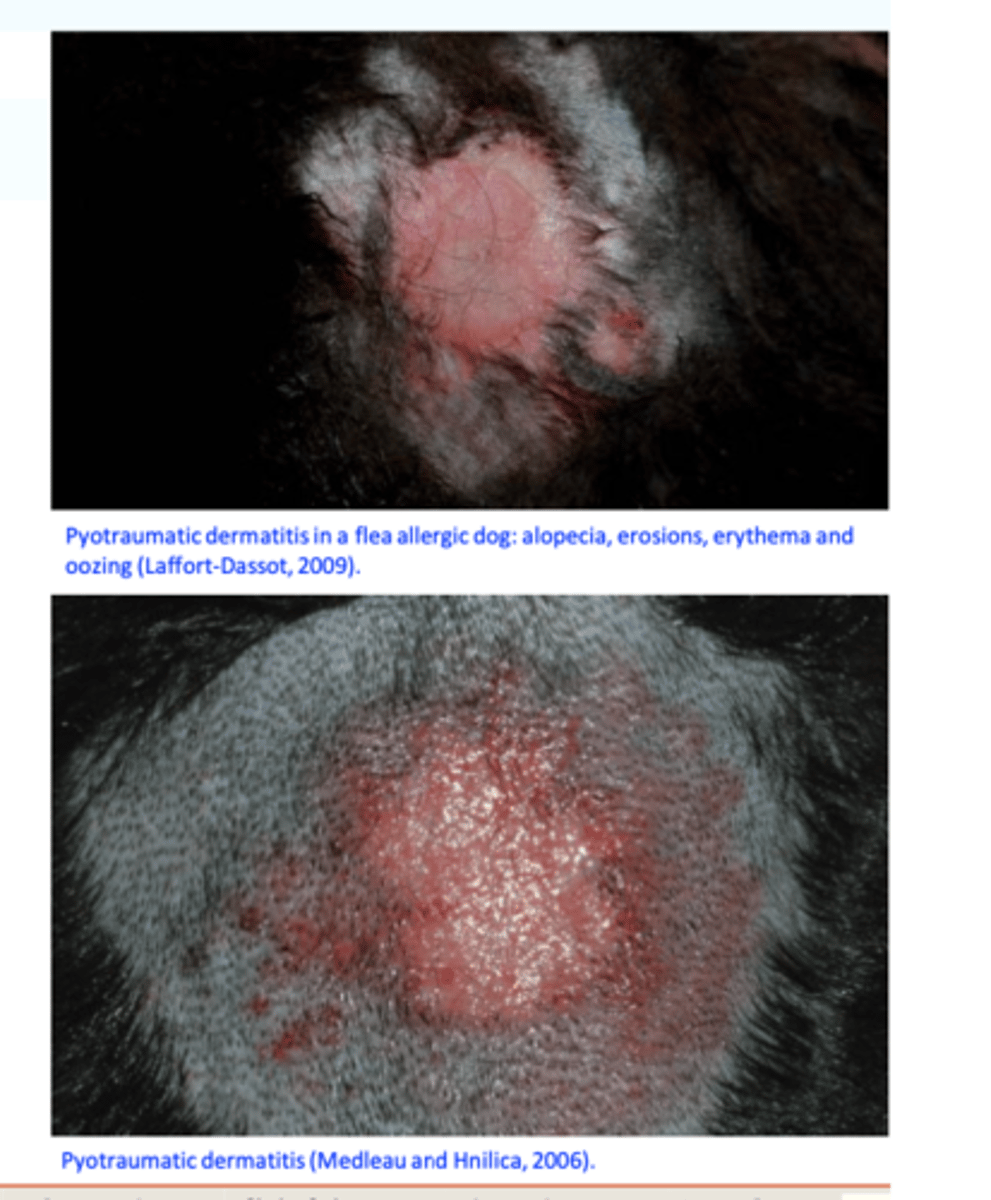
Ctenocephalides spp. Clinical signs of FAD in cats
FAD is seen in cats of any age, sex and breed;
The most common cause of ‘feline miliary dermatitis’;
The primary clinical lesion seen in the cat is an erythematous papule covered by a small reddish-brown crust (miliary dermatitis type lesion);
• These pruritic lesions are usually most severe on the head, neck, and dorsal lumbosacral regions but have a tendency to generalize;
Ctenocephalides spp.
Clinical signs of FAD in cats
PRUITUS
moderate to severe pruritus => licking, scratching, chewing, and violently attacking areas of the skin without visible provocation;
Scaling, broken hairs, restlessness, weight loss etc;
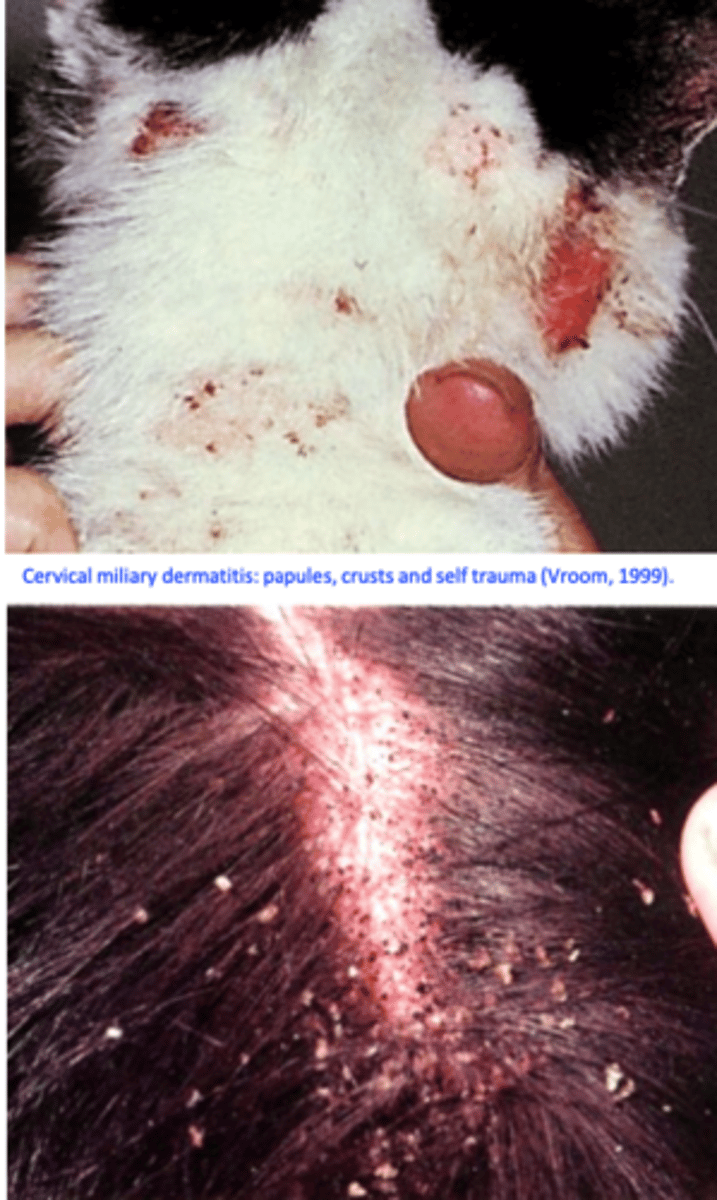
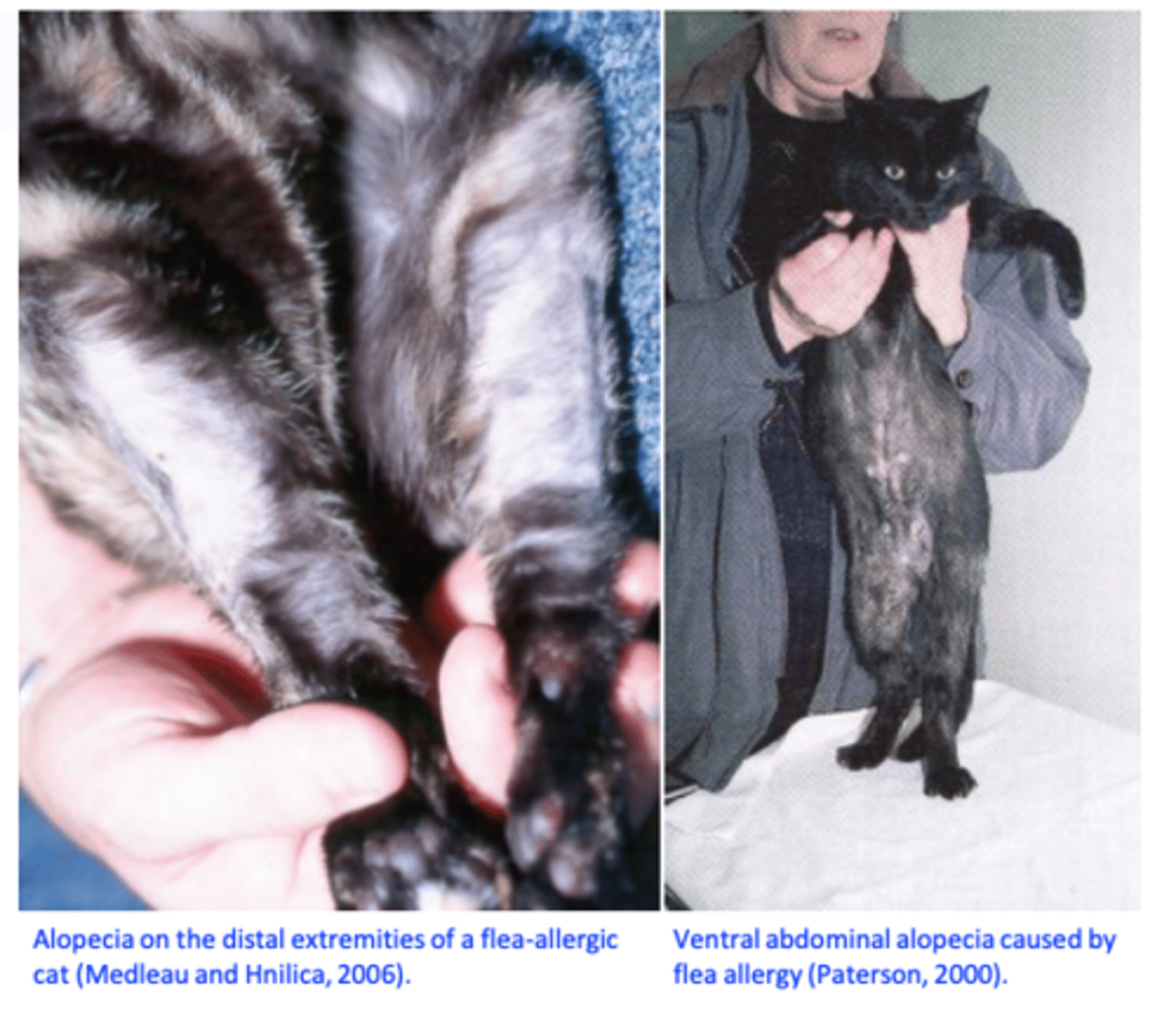
Ctenocephalides spp.
Clinical signs of FAD in cats
• Alopecia
highly variable
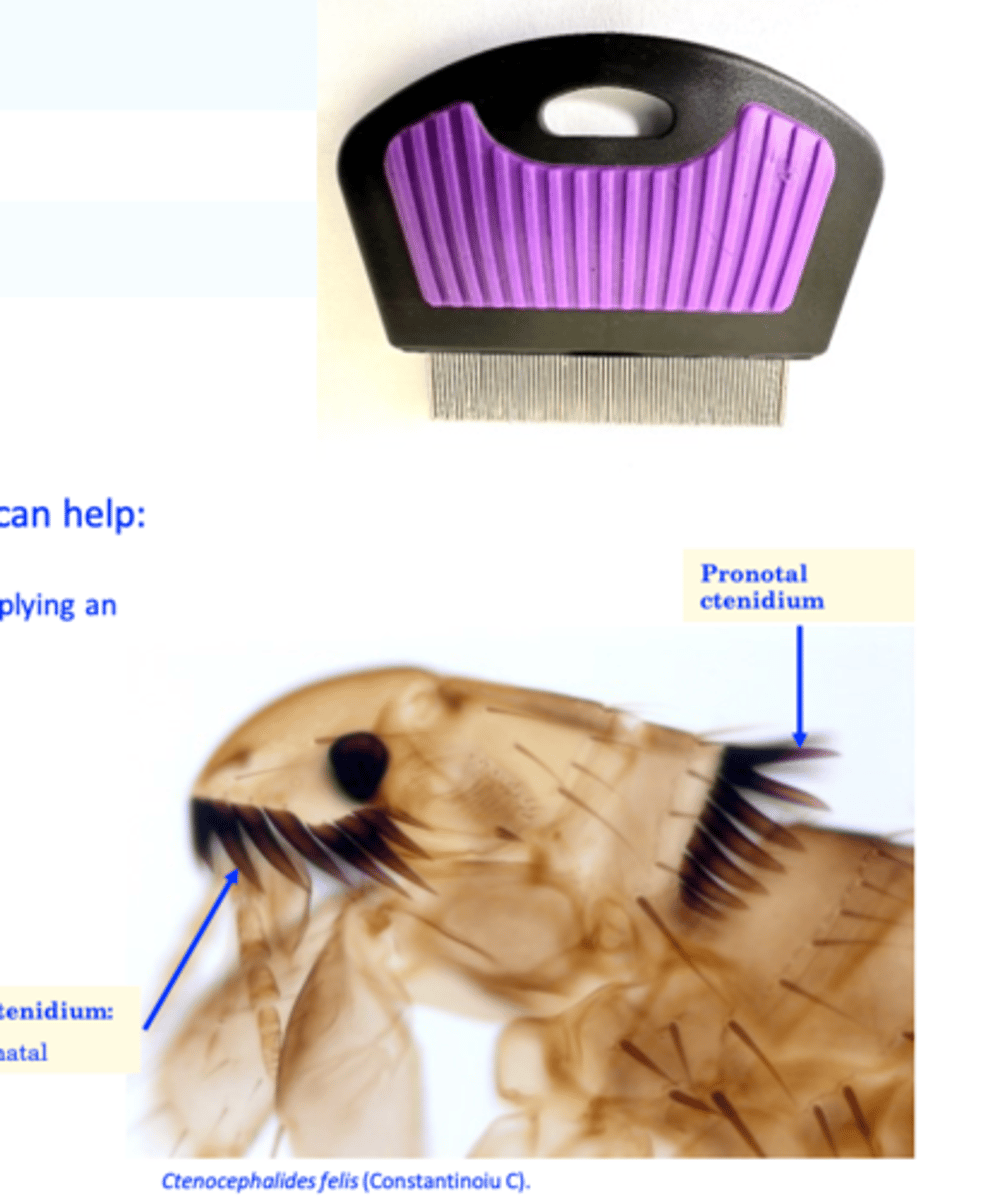
Ctenocephalides spp. Diagnosis
1. Clinical signs and history (timing, presence of in-contact animals, lack of preventive treatments, owners bitten by fleas etc);
2. Response to insecticidal (corticosteroids?) treatment;3. Visualization of fleas or flea faeces on the body of the host;
The use of a fine-toothed metal comb can help:
• Pick fleas out of the coat (combing after applying an insecticide);
• Flea faeces: reddish-brown particles that will dissolve in water or alcohol to form reddish stains;
Visualization of Dipylidium caninum proglottids
(faeces, bedding, body of the host)
Physical examination
Dogs: examine the dorsal lumbar area for papules, which are the primary lesions seen in canine FAD;
Cats:carefullypalpatetheskinincats(thesmall,crusted papules (miliary crusts/dermatitis) often are more easily felt than seen;
7. Allergy testing
Intradermal testing•
In vivo test used to demonstrate immediate (20 min) and delayed (48
hrs) hypersensitivity reactions;
ELISA: • Detect specific IgE
Ctenocephalides spp.: DD
sarcoptic mange
Sarcoptic mange
History (exposure to infested dogs – boarding kennels, grooming facilities, played with other dogs etc);
Highly contagious;
Lesions usually starts on the head/ears;
Intense pruritus;
Deep skin scrapings (ear margins) needed to visualize the mites;
Humans (owners): might be affected intense itching;
Response to treatment
Results of serological tests (ELISA) and pinnal-pedal reflex;

Ctenocephalides spp.: DD
demodicosis
History (mother & siblings suffered from demodicosis);
Not contagious and humans not affected;
Not very itchy before bacterial complications occur;
Distribution of the lesions (commonly head affected initially), features of the lesions (well defined in localized demodicosis);
• Positive skin scrapings;

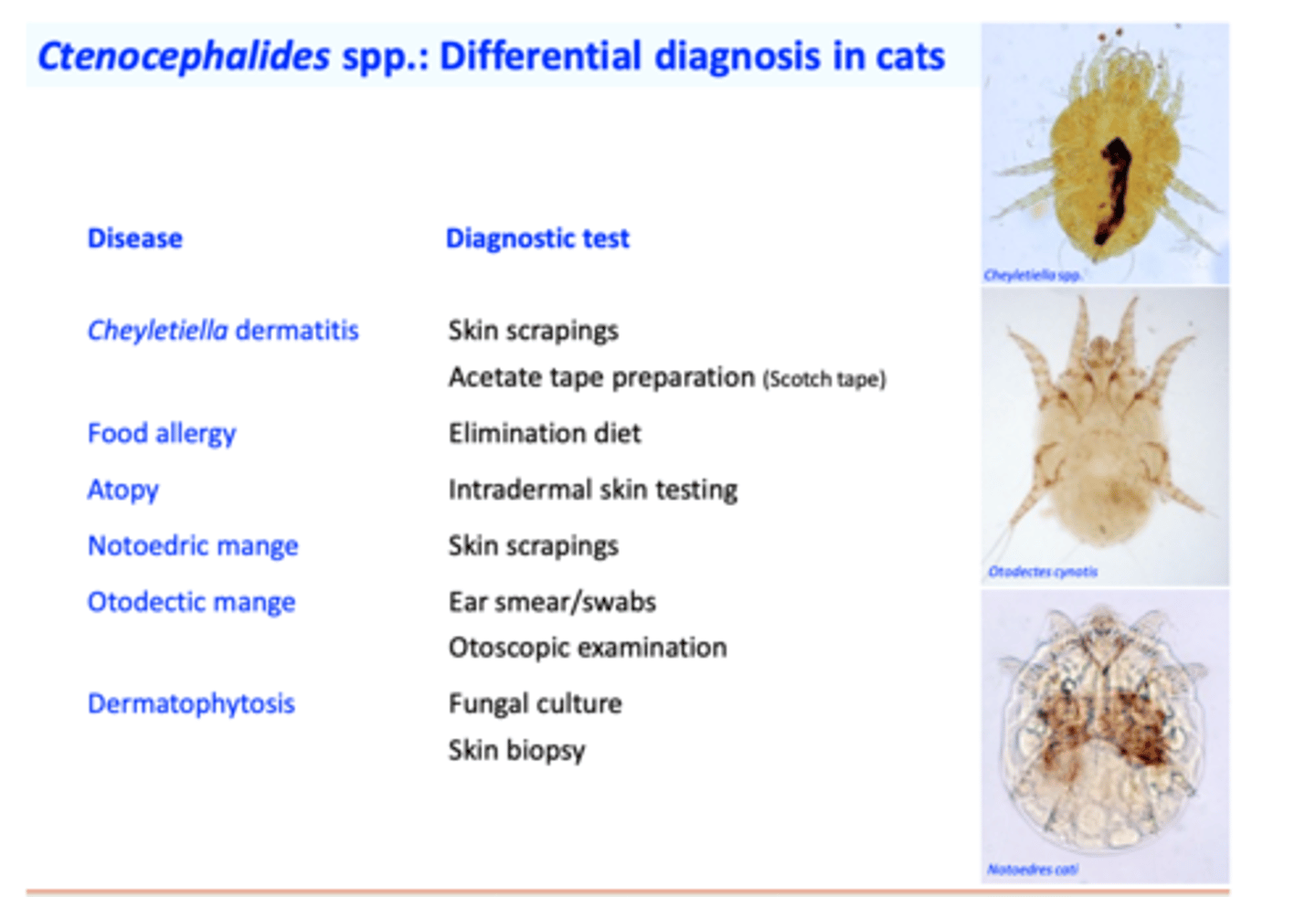
Ctenocephalides spp.: Differential diagnosis in cats
1) Integrated Flea Control
• Kill the (adult) fleas on the dog/cat
- High initial speed of kill of the product => quick relieve of the pet discomfort;
- High residual speed of kill of the product => resolve FAD and control the flea infestations
• Eliminate the immature stages from environment
• Insect growth regulators (IGRs) => break the life cycle;
• Treat the indoor/outdoor environment;
Education of the pet owner.
Mechanical control measures;
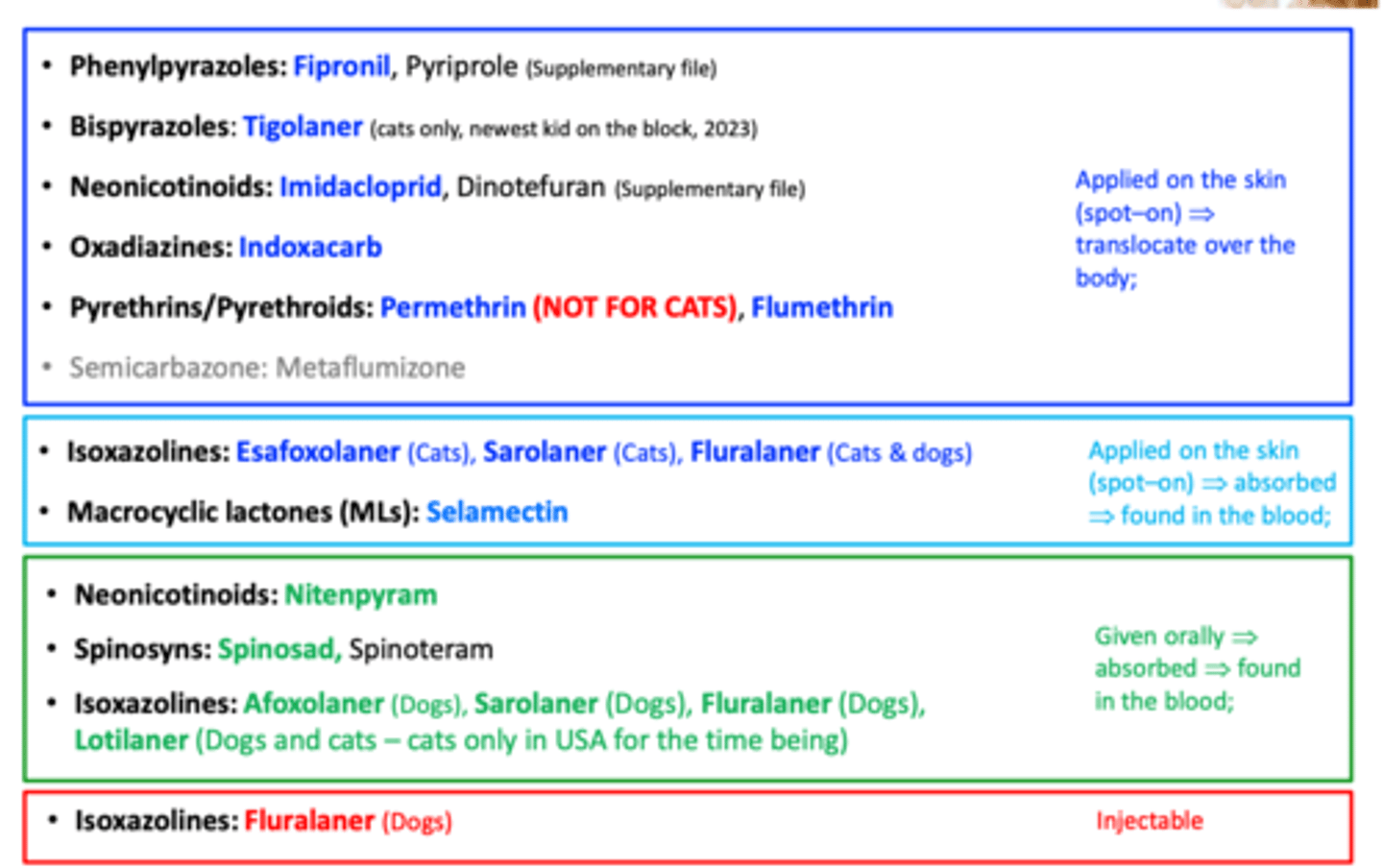
a) Commonly used adulticides
Phenylpyrazoles: Fipronil
Bispyrazoles: Tigolaner
Neonicotinoids: Imidacloprid
Oxadiazines: Indoxacarb
Pyrethrins/Pyrethroids: Permethrin (NOT FOR CATS), Flumethrin
Isoxazolines: Esafoxolaner (Cats), Sarolaner (Cats), Fluralaner
Macrocyclic lactones (MLs): Selamectin
Neonicotinoids: Nitenpyram
Spinosyns: Spinosad
Isoxazolines: Afoxolaner (Dogs), Sarolaner (Dogs), Fluralaner (Dogs), Lotilaner
Isoxazolines: Fluralaner
b) Insect Growth Disruptors/Regulators (IGDs/IGRs)
Interfere with growth and development of immature stages of the insects;
Eliminate the environmental stages => prevent re- infestations;
Generally they have no effect on adults => lag between the initiation of treatments and reduction in the number of adult fleas on the host;
Commonly combined with adulticides;
Juvenile hormone analogues (JHAs):• Methoprene (spot-on), pyriproxyfen
Insect development inhibitors (Chitin synthesisinhibitors (CSIs): Pupa
Cocoon
• Lufenuron
c) Mechanical means of environmental control
• Vacuum of carpets, rugs will remove many of the eggs (59%), faeces and larvae (up to 27%);
• Wash the pet bedding or bed cloths with boiled water;
• Treat the indoor and outdoor environment with
insecticides
Failure of control measures
Chemoresistance?
Proven to carbamates, organophosphates and pyrethroids;
Fipronil?
Ask the owner if the products were applied correctly (on the skin and not on the haircoat for the topical drugs), observing the timing etc;
Ask the owner if she/he treated all the pets in the household;
Is the pet's environment shared with wildlife or unknown animals?
2) Provide the animals with relief from pruritus/allergic reactions
3) Treat any secondary infections

Pediculosis
Infestation with lice in small animals
• Trichodectes canis
• Heterodoxus spiniger
• Linognathus setosus
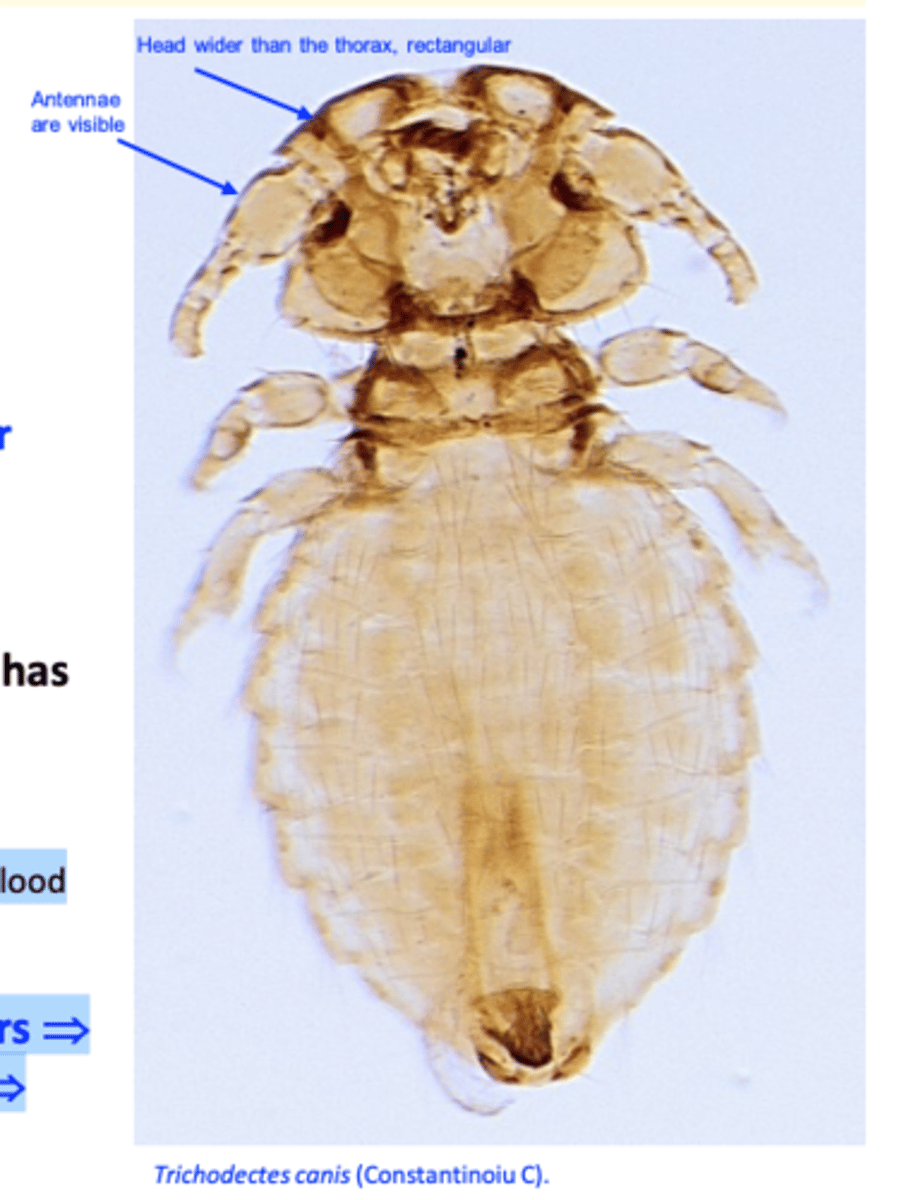
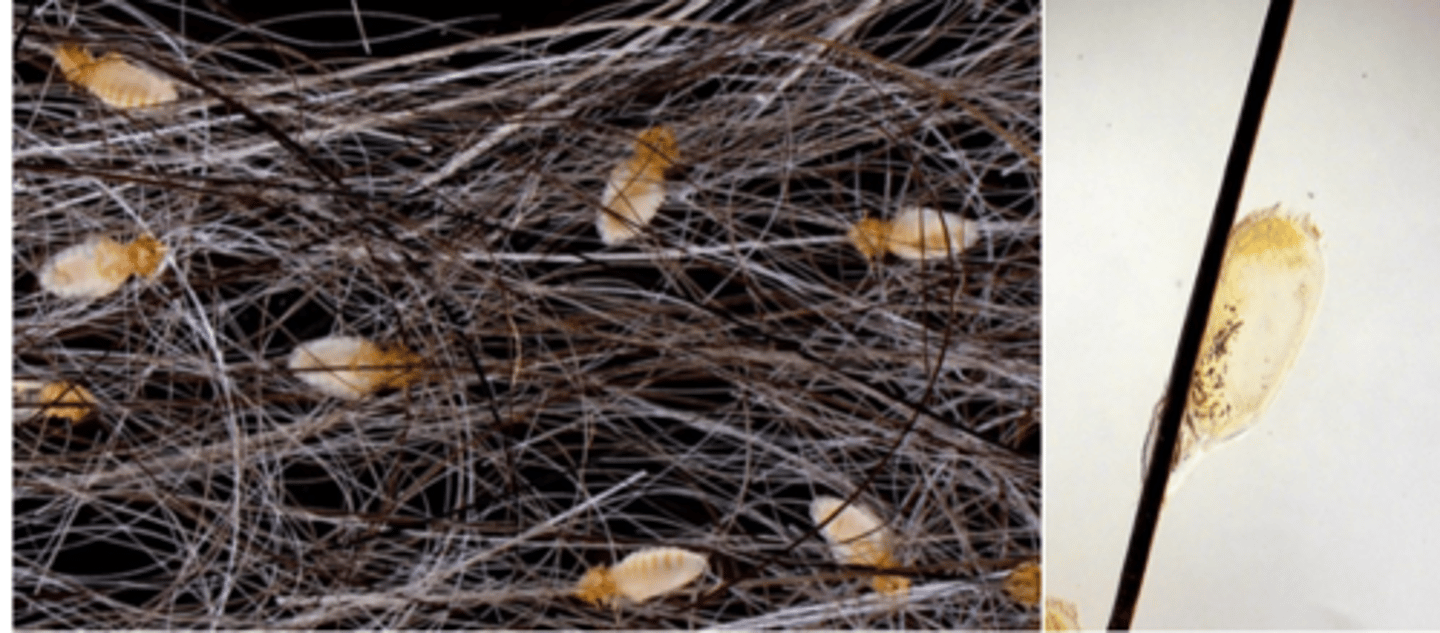
Lice in dogs: Trichodectes canis
Head, wider than the thorax and of rectangular shape (broader than long); antennae are visible;
Legs (3 pairs) are stout, end in single claws;
The abdomen is wide (almost circular in female) and has many rows of large, thick setae; Feed on epidermal debris and blood
Life cycle: eggs are glued at the base of the hairs => nymphs hatch in 1-2 weeks => moult 3 times => adults (30 days);
Lice in dogs: Heterodoxus spiniger
Morphology
Yellowish, about 3 mm long;
Head:
Triangular, rounded forehead;
Provided with is a pair of strong, ventral, spine-like
processes;
Antennae not visible;
Legs: provided with 2 claws;
Feeding: seems to prefer blood.

Heterodoxus spiniger (Kangaroo louse)

Lice in dogs: Linognathus setosus
Head
Narrower than the thorax;
Legs: first pair smaller than the 2nd and 3rd pairs,
Feeding: blood;
Lice in dogs
Epidemiology
Host specific;
All developmental stages are present on the host (unlike fleas and ticks);
Less common than in the past
More common during the cold season
Common in young animals and immunosuppressed or neglected /debilitated animals =>massive populations can develop rapidly in these animals
Transmitted mainly by direct contact => infestations are common where animals are housed together;
Lice in dogs
Pathogenesis
Pathogenesis
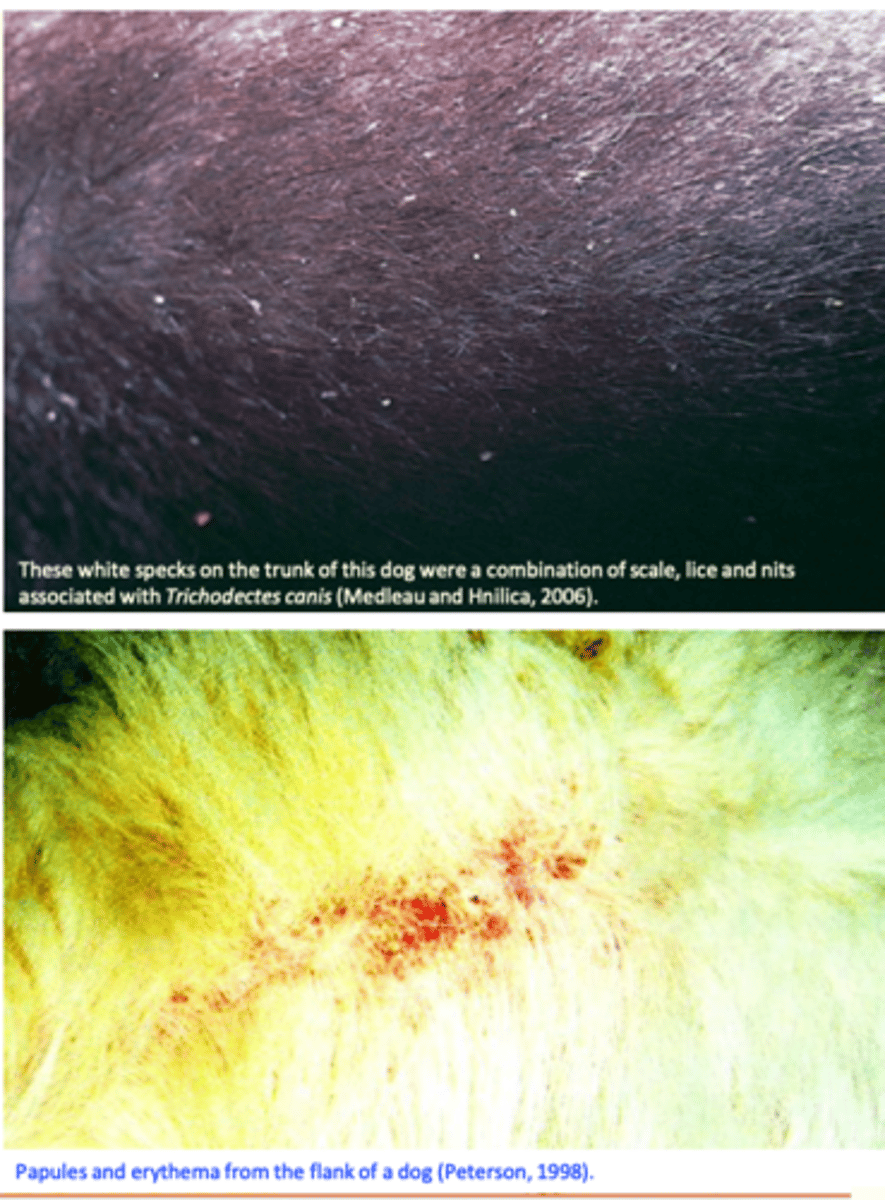
Location: generally on the head, neck, ears, back and trunk;
Some individuals may suffer less and others may suffer from severe dermatitis
Huge populations may develop rapidly on neglected, poorly nourished, newborn puppies;
Chewing lice are more active and tend to be more irritant than sucking lice => itching => scratching => alopecia, excoriations, scaling, bacterial complications etc;
Sucking lice cause anemia and debilitation;
Lice in dogs
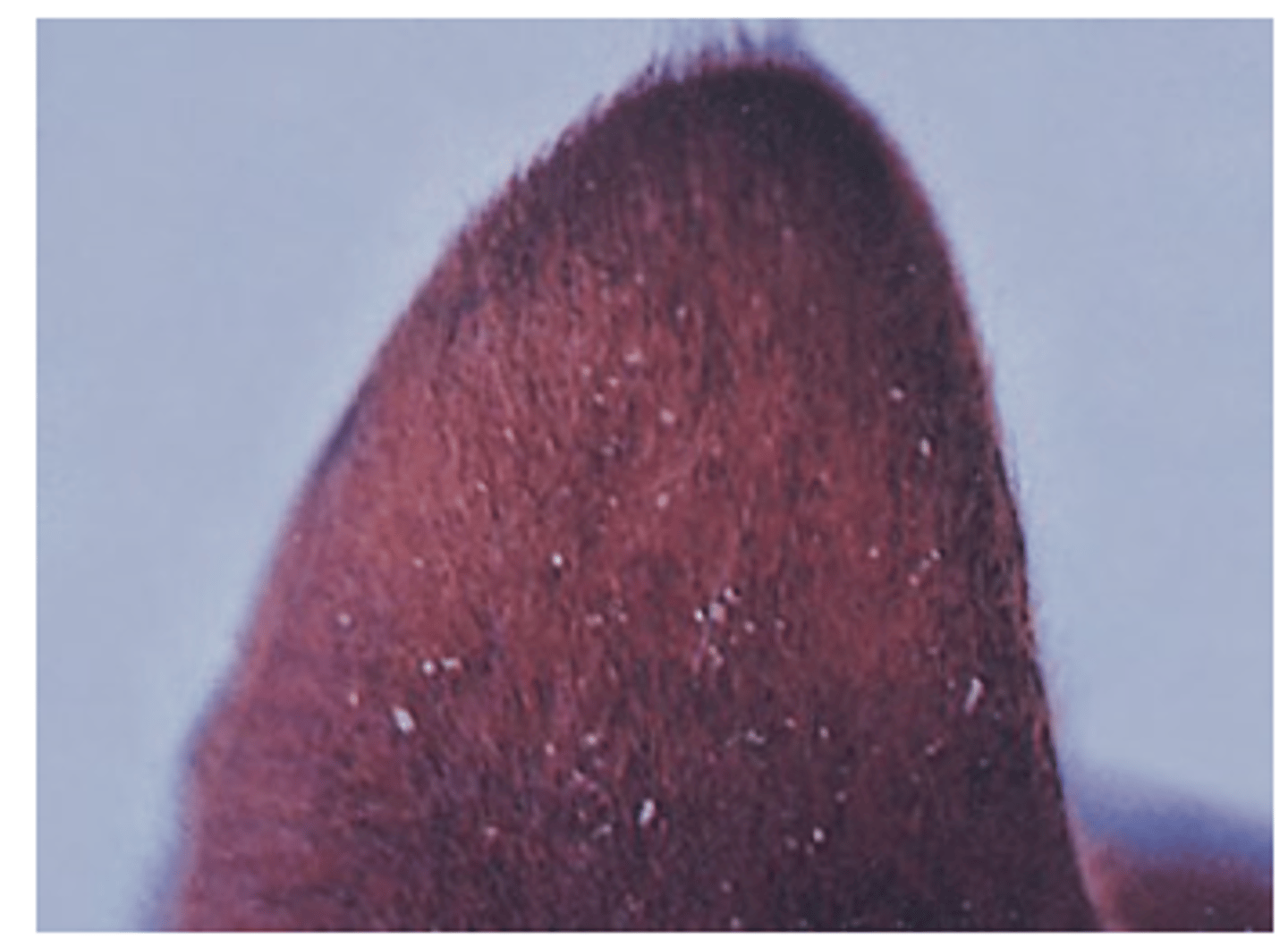
Clinical signs
Pruritus => alopecia => restlessness;
Thickly matted hairs;
Small papules and crusts;
In severe infestations: anemia, weakness, debilitation;
Lice in dogs
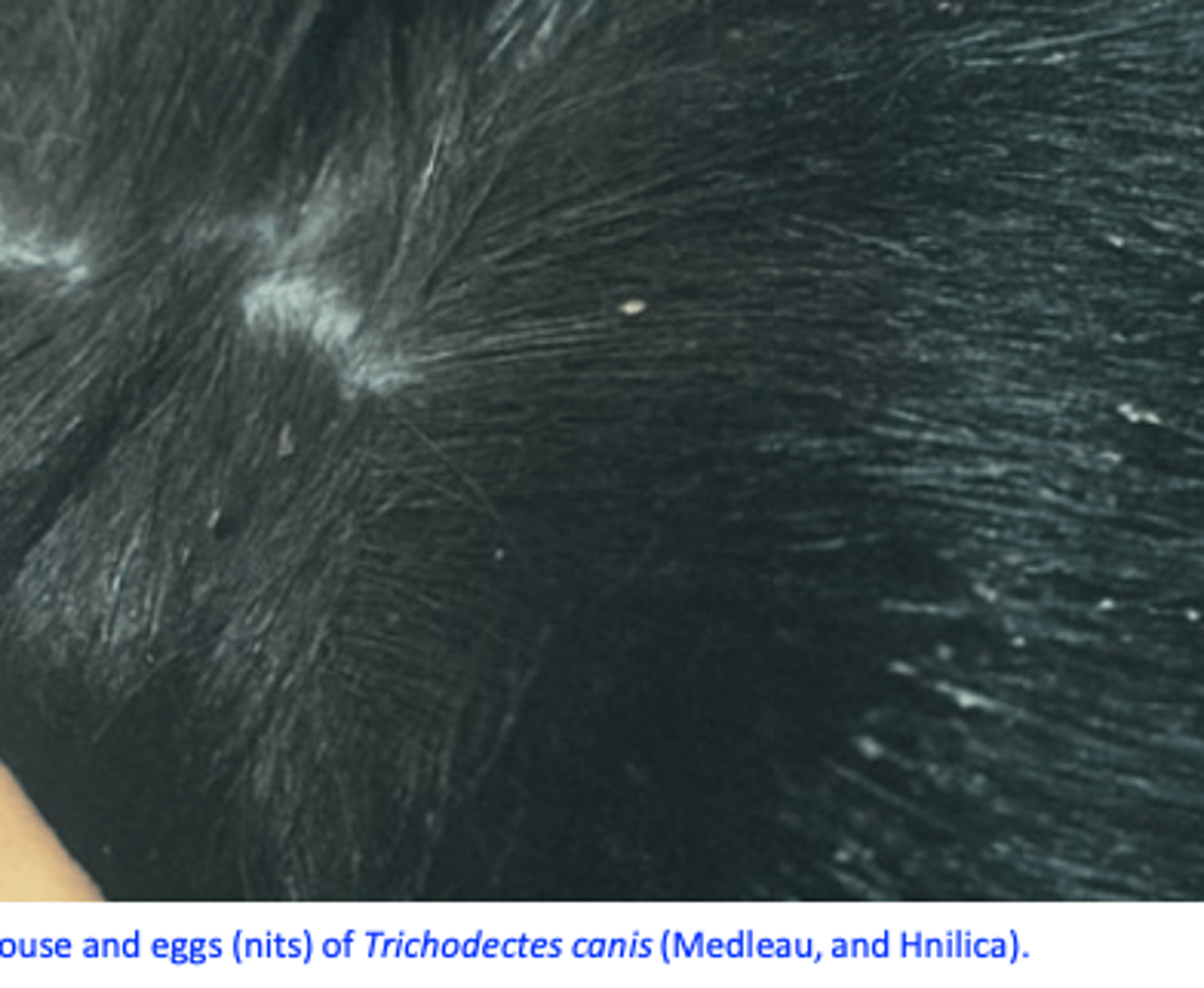
Diagnosis
History
Clinical signs (pruritus, scratching, alopecia etc);
Visualisation/identification of the lice or eggs
Adhesive tape
Differential diagnosis
Lice in dogs
Treatment
Generally, drugs used for the treatment of flea infestations work well against lice;
Treat all in contact animals;
Clean and treat the bedding, grooming supplies etc.
- Pyrethrin, pyrethroids
- Fipronil
- Imidacloprid
- Selamectin
- Isoxazolines: seem to be highly effective

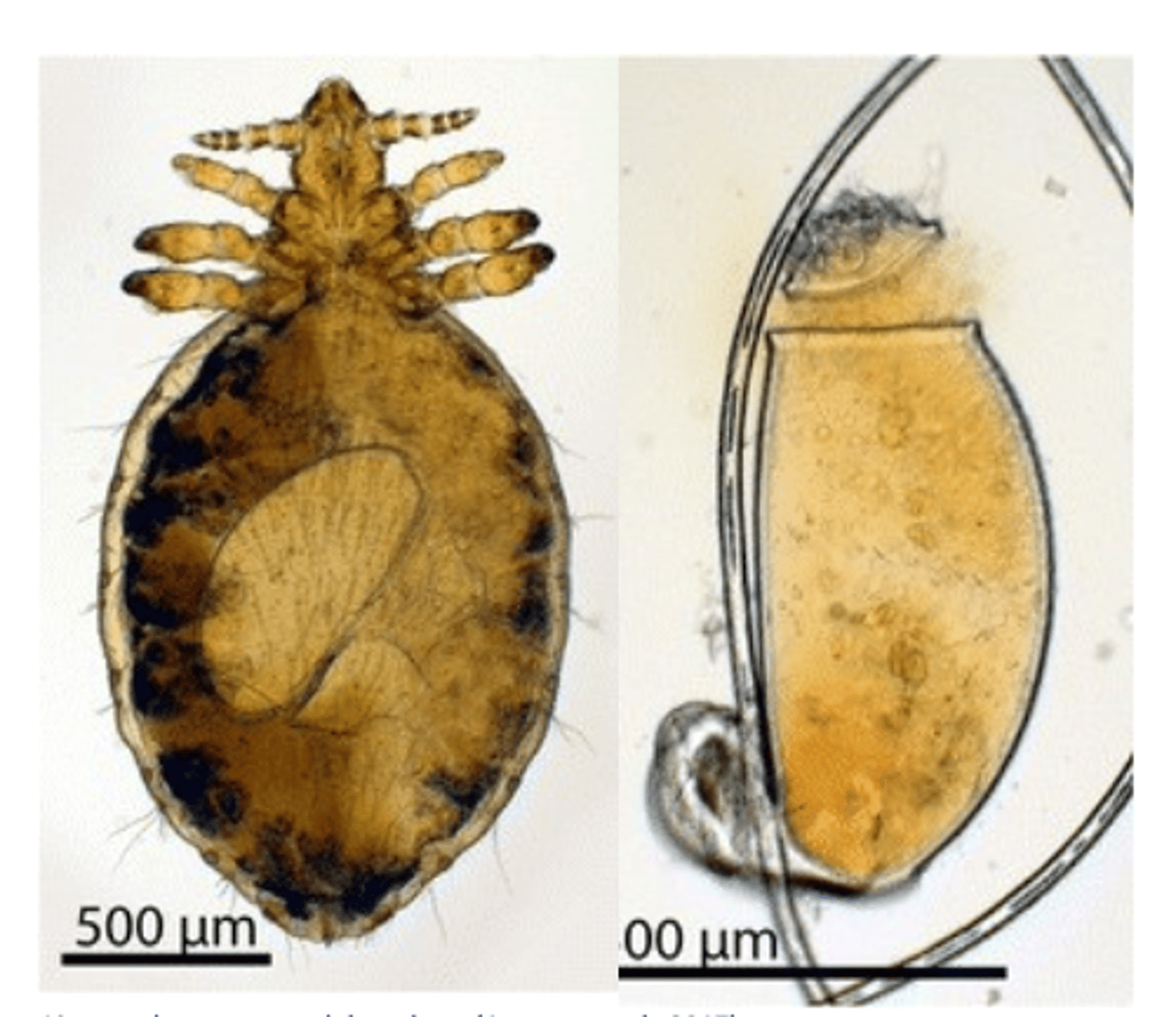
Lice in Cats: Felicola subrostrata(us)

Felicola subrostrata(us)
Shape of the head is triangular, pointed anteriourly;
Median longitudinal groove on the head;
Life cycle
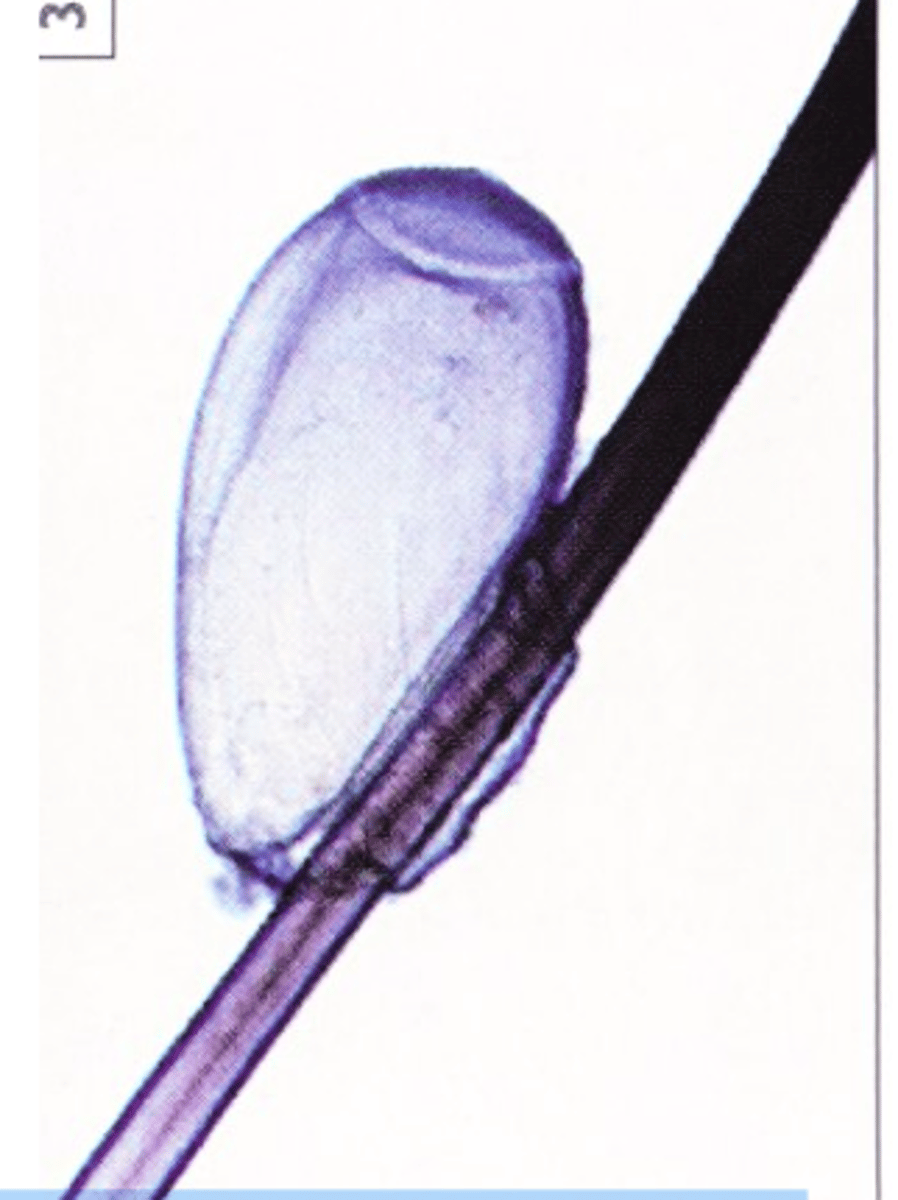
Eggs are glued by the female lice to the hair shafts =>3
nymphal stages => adults;
Life cycle can be completed in 30-40 days;
Feed on skin debris and probably skin exudates.

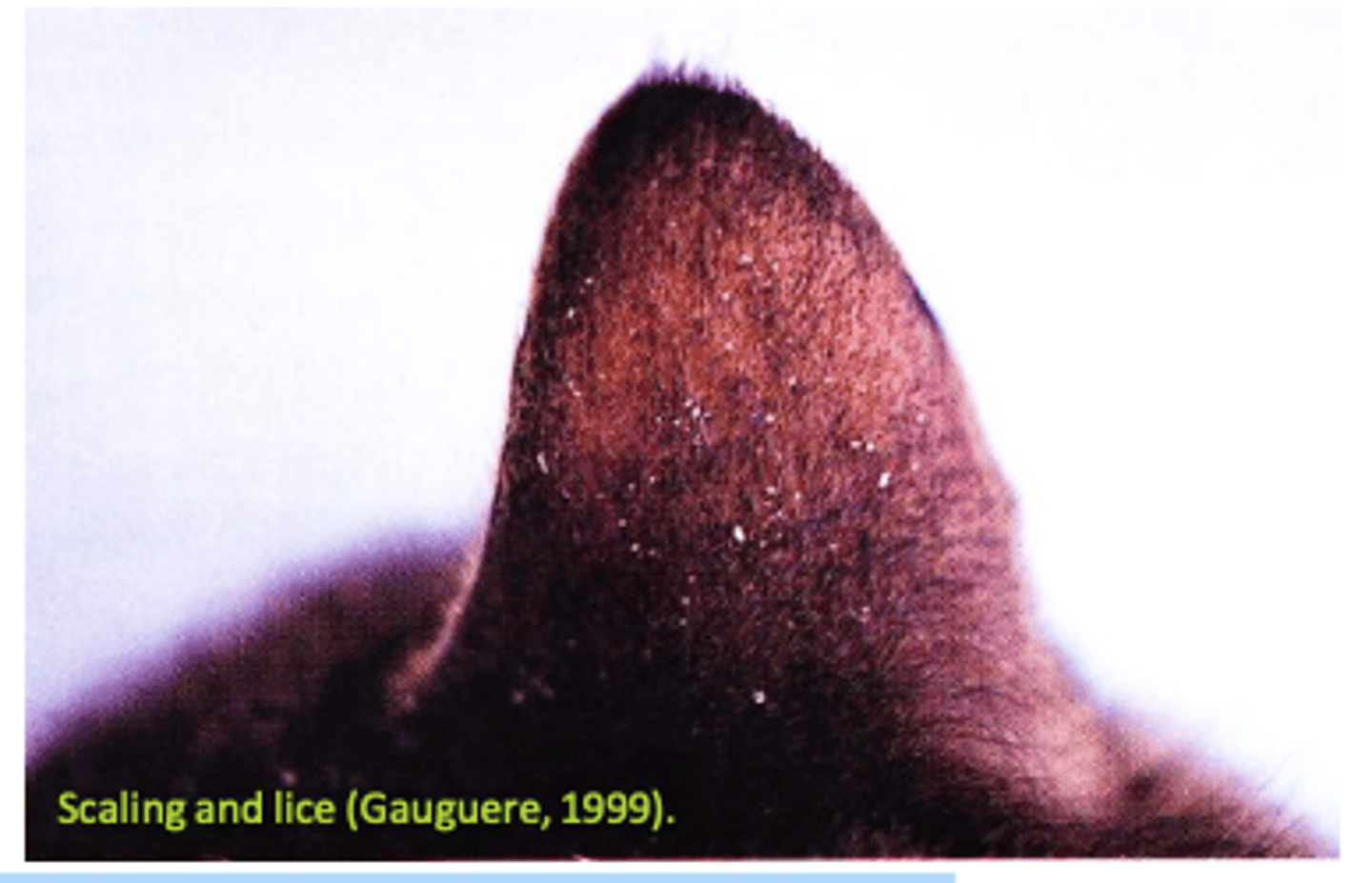
Felicola subrostrata: Epidemiology and Clinical signs
Transmitted mainly by direct contact (grooming supplies);
Common in animals kept in poor conditions, older, long-haired cats that are unable to clean themselves;
Areas most commonly affected: head, face, pinnae, neck, back, tail;
Scaling and lice (Gauguere, 1999).
Irritate the host => pruritus & restlessness => scratching => alopecia, skin lesions;
Scaling, dull coat, papule, crusts;
The hair coat may be matted and have a ruffled appearance, due in part to the accumulation of skin exudates in the hair;
Anorexia, debilitation;
Felicola subrostrata: Diagnosis
Clinical signs;
Finding lice and/or eggs on the body of the cats
Felicola subrostrata: Treatment
Fipronil
Imidacloprid
Selamectin
Treat all cats in the household;
Clean and treat the bedding and the grooming supplies.
