2. Pain Management: Local Anaesthetics
1/21
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
22 Terms
What are local anaesthetics and their use?
Local anaesthetics cause a loss of sensation to pain in a specific area without affecting consciousness.
They are used for minor surgical procedures.
Cocaine was the first local anaesthetic.
All local anaesthetics are ____ bases.
All local anaesthetics are weak bases.
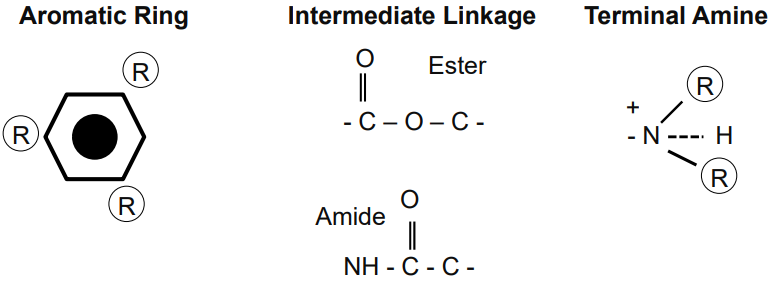
What is the structure of local anaesthetics & what are the 2 classes?
Local anaesthetics have a general structure with:
Aromatic ring (lipophilic)
Intermediate linkage (either ester or amide)
Terminal amine (hydrophilic)
They are all weak bases.
Amino esters and amino amides are the two classes of local anaesthetics.
How can you identify if a medicine is a local anaesthetic?
Most local anaesthetics end with -caine (e.g., lidocaine, bupivacaine, procaine).
What are the characteristics of amino esters as local anaesthetics?
Unstable in solution and fast-acting
Rapidly metabolised in plasma by pseudocholinesterases
Excreted in urine
Metabolic product PABA (para-aminobenzoic acid) causes allergic reactions
Examples:
Cocaine
Procaine
Benzocaine
Tetracaine (used in venous cannulation)
Chloroprocaine (used in spinal anaesthesia)
What are amino amides and how do they differ from amino esters?
Amino amides are heat stable, have a long shelf life, and are less likely to cause allergies.
They are metabolised in the liver and have a slower onset and longer half-life than amino esters.
Examples with uses:
Lidocaine (dentistry)
Bupivacaine (epidural block)
Levobupivacaine (acute post-operative pain)
Mepivacaine (nerve block anaesthesia)
Prilocaine (minor skin procedures)
Ropivacaine (peripheral nerve block)
Articaine (dentistry)
how is local anaesthetic injected.
near a nerve, but not directly in the blood.
How do local anaesthetics work?
Local anaesthetics are weak bases, injected as salts (ionised form).
They shift to the non-ionised form, allowing them to pass through the neuronal membrane.
Inside the cell, they return to the ionised form, blocking voltage-gated sodium channels.
This prevents depolarisation, stopping action potential and pain transmission.
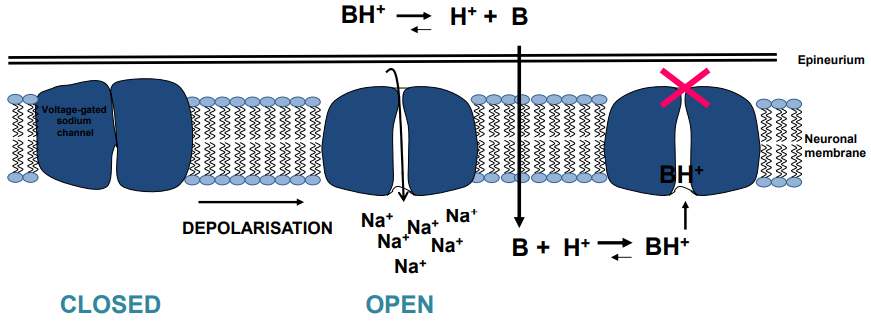
What are the states of voltage-gated sodium channels, and how do they relate to local anaesthetics?
Three states:
Deactivated (closed): At resting membrane potential.
Activated (open): At threshold (~-55mV), leading to depolarisation.
Inactivated (closed): After depolarisation, leading to the falling phase.
Local anaesthetics bind to sodium channels, blocking them in the inactivated state, preventing action potentials and pain transmission.
They are applied near nerves to prevent pain for as long as needed.
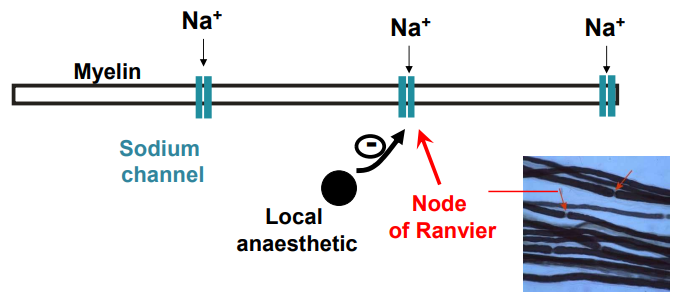
How do local anaesthetics affect different nerve fibres and what is their order of sensitivity?
Local anaesthetics block nerve fibres in the order of their diameter:
Aδ (1–5 μm): Sharp pain (myelinated)
Type C (0.2–1.5 μm): Dull pain & autonomic postganglionic (unmyelinated)
Aβ (5 μm): Sensory (myelinated)
Aα (12 μm): Motor (myelinated)
In myelinated fibres, local anaesthetics act at the Nodes of Ranvier.
The order of nerve sensitivity is:
Autonomic > Pain > Temperature > Touch > Pressure (Proprioception) > Skeletal Muscle Tone.
What factors influence the activity of local anaesthetics?
Lipid solubility = higher lipid solubility = higher potency
Volume of agent
Sites of injection
pKa value = lower pKa = lower degree of ionisation = better cell penetration = faster onset rate = longer duration of action
How does pH influence anaesthetic activity?
Most local anaesthetics have a pKa of ~7.6 – 8.9
At pH 7.4, the ionised cationic form predominates
At alkaline pH = low proportion of ionised molecules = increased onset of action & effect duration
In inflamed tissues (acidic pH) = decreased onset & effect duration
How do vasoconstrictors affect local anaesthetics?
Most local anaesthetics cause vasodilation (except cocaine)
Adding vasoconstrictors prolongs local effects
Not suitable for patients with severe hypertension or unstable cardiac rhythm
Example: Lidocaine + Adrenaline
What are the symptoms of local anaesthetic toxicity?
Central Effects:
CNS irritability → Seizures
Tinnitus, lightheadedness, metallic taste in mouth
Nausea, slurred speech, drowsiness
CNS depression
Agitation, confusion, dizziness, blurred vision
Muscle twitching, tremor
Cardiovascular Effects:
Depression of cardiac conduction and excitability → Slowing/blocking of heart's electrical signals.
Atrio-ventricular block
Cardiovascular collapse
Cocaine → Enhances sympathetic activity, leading to tachycardia, increased cardiac output, vasoconstriction, and increased arterial pressure.
What is the treatment for local anaesthetic toxicity?
Stop injection
Seizure treatment with benzodiazepines
Cardiovascular support: adrenaline, vasopressors, cardioversion
Lipid emulsion therapy
What is lipid rescue & how is it used in local anaesthetic toxicity?
20% lipid emulsion (Intralipid) used to scavenge uncharged local anaesthetic molecules
Aqueous IV infusion of fine lipid droplets
Used in severe toxicity
NICE guideline:
1.5 mL/kg over 1 min
Followed by 15 mL/kg/hour
Can be repeated twice during cardiac arrest
What are the clinical applications of topical & regional nerve block anaesthesia?
Topical anaesthesia:
Applied to mucous membranes (nose, mouth, trachea, genitourinary tract), cornea, or skin
E.g. lidocaine, tetracaine, benzocaine (not used in ophthalmology/ for eye)
Regional nerve block:
Injected near a peripheral nerve trunk or plexus (e.g. dental nerves)
Used for regional anaesthesia in dentistry/surgery
May include vasoconstrictor
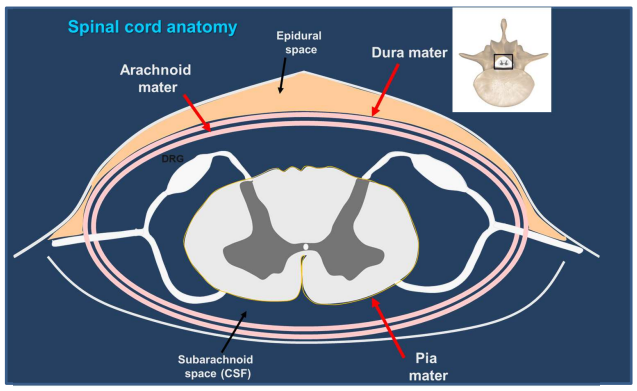
What are the clinical applications of infiltration & spinal anaesthesia?
Infiltration anaesthesia:
Direct injection near nerve branches & terminals
Used for minor surgery
Adrenaline often added for vasoconstriction
Spinal anaesthesia:
Injected into lumbar subarachnoid space (below L2) into CSF
Blocks spinal roots or cord
Used in abdominal & lower body surgery
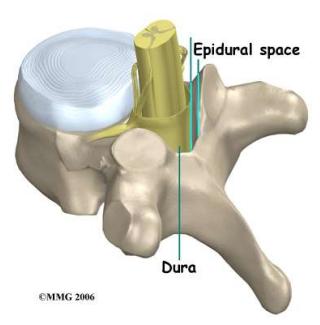
What is epidural anaesthesia used for & how is it administered?
Drug injected into the epidural space at any spinal level
Blocks spinal roots
Produces anaesthesia of the thorax, abdomen & lower limbs
What are some properties & side effects of the cocaine (e.g. cocaine, procaine, benzocaine)?
Cocaine:
First local anaesthetic
Effective surface anaesthetic
Used in otolaryngology (e.g. nasal spray – low dose)
Side effects:
Euphoria
↑ Sympathetic activity = tachycardia, ↑ cardiac output & arterial pressure, vasoconstriction
Addictive – never given by injection
Procaine (Novocaine®): first cocaine derivative
Benzocaine: low potency & toxicity, used topically (e.g. throat lozenges)
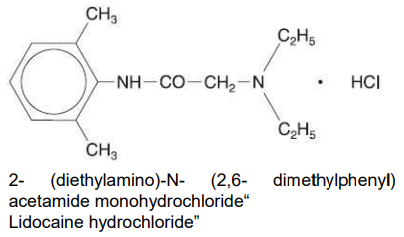
What are the properties, uses & side effects of lidocaine?
Properties:
Hypoallergenic (less likely to cause allergic reactions)
Rapid onset
Effective for several hours
Administration methods:
Injections (e.g. dental cartridges)
Surface anaesthesia: gel, ointment, solution, cream (EMLA®), jet spray
Topical solution for ear, nose, oropharynx (with phenylephrine)
Side effects:
Confusion
Respiratory depression
Convulsions
Hypotension
Bradycardia
What are the properties, uses & side effects of bupivacaine?
Properties:
Longer duration of action than other local anaesthetics
Slow onset (~30 min)
Uses:
Principal drug for spinal anaesthesia
Suitable for continuous epidural analgesia in labour
Side effects:
Similar to lidocaine (e.g. confusion, respiratory depression, convulsions, hypotension, bradycardia)