Pathoma Chapters 1-3
1/156
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
157 Terms
Hypertrophy vs Hyperplasia:
These processes happen in response to an increased or decreased stress/stimulus?
Increased
Hypertrophy vs Hyperplasia:
Which involves protein synthesis and production of organelles?
Hypertrophy
Hypertrophy vs Hyperplasia:
Which involves activation of Stem Cells?
Hyperplasia
Hypertrophy vs Hyperplasia:
What are the 3 permanent tissues?
1. CNS
2. Cardiac Muscle
3. Skeletal Muscle
Hypertrophy vs Hyperplasia:
What defines a Permanent tissue?
No Stem Cells
Hypertrophy vs Hyperplasia:
What is the only Hyperplasia that doesn't have an increased risk for cancer?
BPH
Benign Prostatic Hyperplasia
Hypertrophy vs Hyperplasia:
Which can progress to dysplasia?
Hyperplasia
Atrophy:
This response happens due to an increase or decrease in stimulus/stress?
Decrease
Atrophy:
Is a decrease in cell size, number or both?
Both
Decrease in Size and Number
Atrophy:
Decrease in cell number occurs via apoptosis or necrosis?
Apoptosis
Atrophy:
Decrease in cell size occurs via which pathway?
Ubiquitinization
Metaplasia:
What are the 3 kinds of Epithelium?
1. Squamous
2. Transitional
3. Columnar
Metaplasia:
What disease is a classic example of this process?
Barret's Esophagus
Metaplasia:
Barret's Esophagus is a change of epithelium from what type to what type?
Squamous to Columnar
Metaplasia:
Occurs via reprogramming of what cells?
Stem Cells
Metaplasia:
Does this process increase risk of CA?
Yes
Metaplasia:
What is the only metaplasia that does not increase risk of CA?
Apocrine Metaplasia of Breast
i.e. Fibrocystic Changes
What is the difference between Aplasia and Hypoplasia?
Aplasia = Failure of Cell production during embryogenesis
Hypoplasia = Decreased Cell production during embryogenesis
Oxygen Delivery:
Hypoxia is an inability to get Oxygen to what?
Tissue
Oxygen Delivery:
Hypoxemia is an inability to get Oxygen to what?
Blood
Oxygen Delivery:
What is FiO2?
Percent of O2 in Air we breath
Oxygen Delivery:
What are the 3 Important components of FiO2?
1. Oxygen
2. CO2
3. Nitrogen
Oxygen Delivery:
What is PAO2?
Percent of O2 in Alveolus
Oxygen Delivery:
What are the 2 important components of PAO2?
1. Oxygen
2. CO2
Oxygen Delivery:
What is the relationship between Oxygen and CO2 in Alveolus?
Oxygen = 1/CO2
Oxygen Delivery:
What is the relationship between CO2 and Ventilation in Alveolus?
Ventilation = 1/CO2
Oxygen Delivery:
What is PaO2?
Oxygen dissolved in blood
Oxygen Delivery:
FiO2 → PAO2 → PaO2 → SaO2;
What do the 3 arrows represent?
1st Arrow = Airway
2nd Arrow = O2 transfer from Lung to Blood i.e. Diffusion
3rd Arrow = O2 transfer from Blood to Hb
Oxygen Delivery:
FiO2 → PAO2 → PaO2 → SaO2;
What parts above represent Hypoxemia?
FiO2 → PAO2 →
Oxygen Delivery:
FiO2 → PAO2 → PaO2 → SaO2;
What parts above represent Hypoxia?
PaO2 → SaO2
Oxygen Delivery:
What is a classic description in Methemoglobinemia?
Chocolate-Colored Blood
Ischemia can be caused by a decrease of what 2 things?
1. Arterial Perfusion
2. Venous Drainage
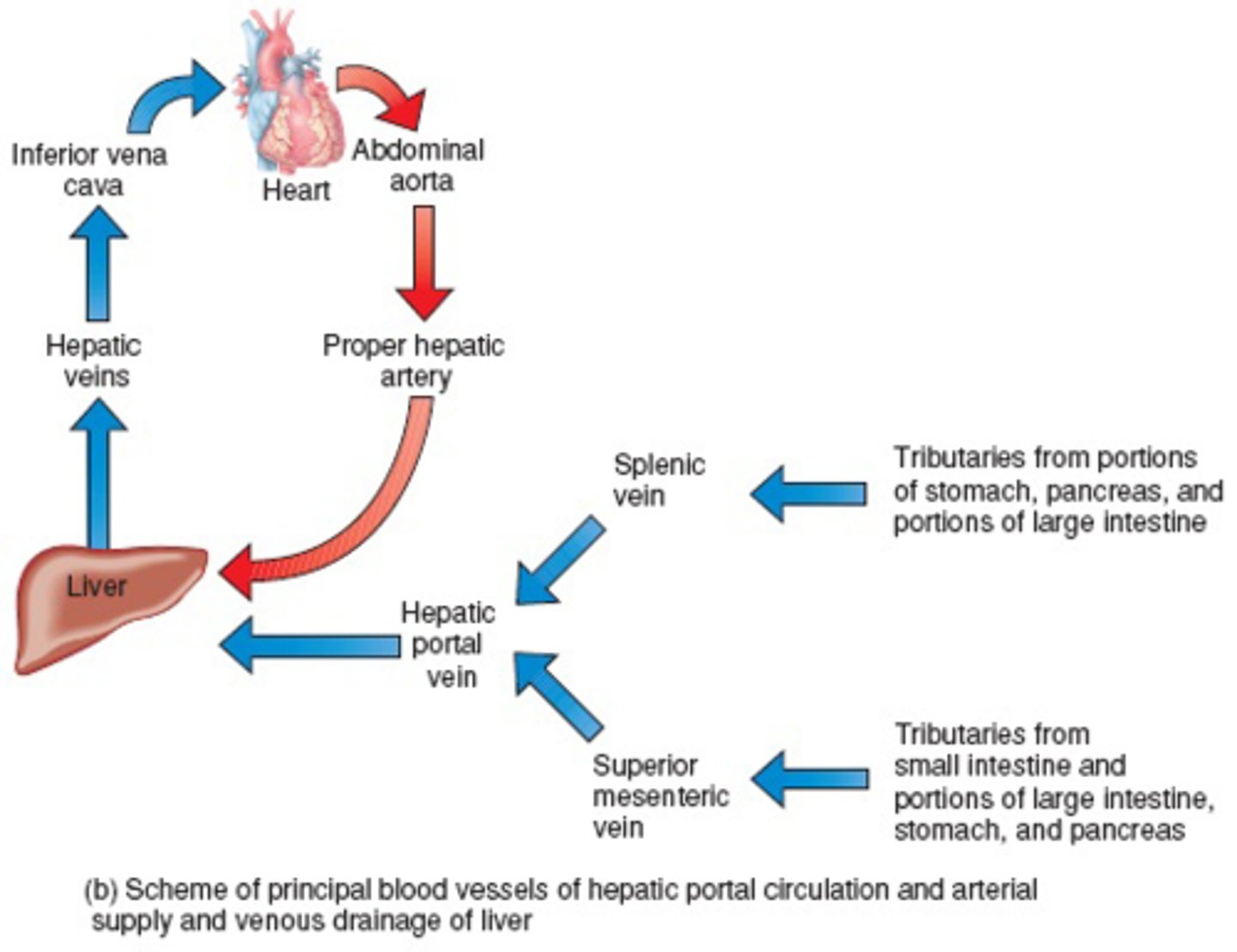
What is a classic example of Ischemia via venous drainage?
Budd-Chiari (Thrombus of Hepatic vein)
Necrosis:
What is the only necrosis that becomes liquefied?
Liquefactive
Necrosis:
Ischemia leads to what kind of necrosis?
Coagulative
Necrosis:
What is the only tissue that becomes Liquefactive with ischemia?
Brain Tissue
Necrosis:
What is the classic macroscopic shape of Coagulative necrosis?
Wedge Shaped
Necrosis:
What kind of necrosis happens in Red Infarction?
Coagulative
Blood RE-ENTERS through tissue
Necrosis:
What are 2 areas that suffer Red Infaction?
1. Testes
2. Lungs
Necrosis:
What are 3 examples of Liquefactive necrosis?
1. Brain Infarct
2. Abcess
3. Pancreatitis
Necrosis:
What are the 2 types of Gangrenous Necrosis?
1. Dry
2. Wet
Necrosis:
Gangrenous Necrosis is a type of Coagulative necrosis that happens in what 2 areas?
1. Lower Limb
2. GI
Necrosis:
Wet Gangrenous necrosis is a mix of what 2 kinds of necrosis?
Coagulative and Liquefactive
Necrosis:
What causes Wet Gangrenous Necrosis?
Infection of Gangrenous Tissue
Necrosis:
What is the classic macro description of Fat Necrosis?
Chalky-White
Necrosis:
What causes Fat necrosis to look Chalky-White?
Calcium Deposition
Necrosis:
What are 2 kinds of Calcium deposition?
1. Dystrophic Calcification
2. Metastatic Calcification
Necrosis:
Ca++ deposits in _____1___ tissue and has ______1_____ serum Ca++ in ______1______ Calcification.
Ca++ deposits in necrotic tissue and has normal serum Ca++ in Dystrophic Calcification
Necrosis:
Ca++ deposits in ___2_____ tissue and has ______2_____ serum Ca++ in ______2______ Calcification.
Ca++ deposits in normal tissue and has high serum Ca++ in Metastatic Calcification
"Ca++ is high so it spreads"
Necrosis:
Fibrinoid necrosis is found where?
Blood Vessel Wall
Necrosis:
What are 2 causes of Fibrinoid Necrosis?
1. Vasculitis
2. HTN
Necrosis:
Preeclampsia causes what kind of necrosis in placenta?
Fibrinoid
Due to HTN
Apoptosis:
What are the 3 pathways for apoptosis?
1. Intrinsic Mitochondrial
2. Extrinsic Receptor Ligand
3. CD8+
Apoptosis:
All apoptosis pathways are dependent on what enzyme type?
Caspases
Apoptosis:
What is the function of BCL2?
Maintains Cytochrome C in Mitochondria
Apoptosis:
What does Cytochrome C do in Cytoplasm?
Activates Caspases
Apoptosis:
Damage→↓BCL2→↑Cytoplasmic Cytochrome C→↑Caspase
What apoptotic pathway is this?
Intrinsic Mitochondrial
Apoptosis:
What are the 2 triggers for Extrinsic Receptor Pathway?
1. FAS Ligand → FAS Receptor aka CD 95
2. TNF → TNF Receptor
Apoptosis:
What do CD8+ cells secrete to activate caspases?
Granzyme
Apoptosis:
How does granzyme, secreted by CD8+, get into the other cells cytoplasm?
Perforins
Free Radicals:
What is the most damaging free radical?
Hydroxyl Free Radical
Free Radicals:
What are 2 MCC of Hydroxyl Free Radicals?
1. Ionizing Radiation
2. Metals
Free Radicals:
How does your body remove Hydroxyl Free Radicals?
Glutathione Peroxidase
Amyloidosis:
What are 2 characteristics shared by amyloid?
1. Beta Pleated Sheet Configuration
2. Congo Red or Apple Green Birefringence
Amyloidosis:
Gene for Beta Amyloid is found on what chromosome?
21
Amyloidosis:
B2-Microglobulin Amyloidosis is specific to what kind of patient?
Dialysis
Amyloidosis:
Calcitonin Amylodosis happens in what CA?
Medullary Thyroid
Inflammation:
Allows what 3 things into Interstitial Space?
1. Inflammatory Cells
2. Plasma Protein (Complement)
3. Fluid
Inflammation:
Vasoconstriction usually refers to what kind of vessel?
Arteriole
Inflammation:
Vasodilation usually refers to what kind of vessel?
Post-Capillary Venule
Inflammation:
Increased Vascular Permeability usually refers to what kind of vessel?
Post-Capillary Venule
Inflammation:
What is the function of TLR (Toll Like Receptor) in inflamation?
Increases NF-KB
Inflammation:
What is a classic TLR?
CD 14 on Macrophage recognizes LPS
Inflammation:
What is NF-KB?
Transcription Factor
Inflammation:
What arachadonic acid derivative activates Neutrophils?
LTB4
Inflammation:
What are the 4 neutrophil chemotactic substances?
1. Bacterial Products
2. IL 8
3. C5a
4. LTB4
Inflammation:
What are the 3 ways to activate a MAST Cell?
1. Tissue Trauma
2. C3a or C5a
3. Crosslinking of Cell Surface IgE by Antigen
Inflammation:
What coagulation factor activates Inflamation?
Factor XII aka Hageman Factor
Inflammation:
Hageman Factor activates what 3 systems?
1. Kinin i.e. Inflammation
2. Complement
3. Coagulation and Fibinolysis
Inflammation:
What state Classically activates Hageman Factor?
Gram - Sepsis + DIC
Inflammation:
What are the 2 substances that mediate pain?
1. Bradykinin
2. PGE2
Inflammation:
IL1 and TNF-a act on what cells in the hypothalamus in order to cause fever?
Perivascular Cells
Inflammation:
What enzyme is activated in Perivascular Cells of the Hypothalamus in the presence of IL1 and TNF-a?
COX
Inflammation:
What is the product of COX when activated by IL1 and TNF-a in the Perivascular Cells of the Hypothalamus?
PGE2
Inflammation:
What is the function of PGE2 in the Perivascular Cells of the Hypothalamus?
Raise the Temperature set point (cause fever)
Inflammation:
What are the 4 steps taken for a Neutrophil to arrive where needed?
1. Margination
2. Rolling
3. Adhesion
4. Transmigration
Inflammation:
Margination occurs in what part of the blood vessely?
Post-Capillary Venule
Inflammation:
What substance is expressed by endothelial cells in Rolling?
Selectin
Inflammation:
What 2 selectins are expressed by endothelial cells in Rolling?
1. P Selectin
2. E Selectin
Inflammation:
Where are P selectins Stored?
Weible-Palade Bodies
Inflammation:
Which selectin is mediated via histamine?
P Selectin
Inflammation:
Which selectin is mediated via TNF and IL1?
E Selectin
Inflammation:
What substance is expressed by leukocytes in rolling?
Sialy Lewis X
Inflammation:
What 2 molecules are expressed by the endothelium in adhesion?
1. ICAM
2. VCAM
Inflammation:
What molecule is expressed by the leukocyte in adhesion?
Integrin
Inflammation:
What disease has a deficiency of Integrins or CD 18?
Leukocyte adhesion deficiency
Inflammation:
Chediak-Higashi is an autosomal recessive deficiency that causes what?
Microtubule Dysfunction
Inflammation:
O2 is converted into Radical O2 via what enzyme?
NADPH Oxidase
Inflammation:
Radical O2 is converted into H2O2 via what enzyme?
Superoxide Dismutase
Inflammation:
H2O2 is converted to bleach (HOCl) via what enzyme?
Myeloperoxidase