CH. 5 - Documentation
1/93
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
94 Terms
_____________ is a method of charting that addresses the patients problems and what is done to solve them, It is seen most often in nurses notes
PIE Charting
The type of charting in which no set formula is followed rather, the HCP writes a detailed account of the care that the patient receives and the events that occur in chronological order. this is the most thorough but the most time consuming method and is known as
narrative charting
the method of charting that can be used with both source-oriented and problem-oriented records is called
soapier charting
a charting format in which notes are written by the HCP that focus only on abnormal findings and where normal finding are not charted, but rather checklists are use for routine care is known as ___________ this method works best with EHR.
charting by exception
___________ is a style of charting that is focused on the patient and less structured than PIE. Commonly, it follows the format of data, action and response.
Focus Charting
A slightly more formal term that refers to the recording of data in a patient chart and is synonymous with charting is
documentation
a type of flip chart with a page for each resident that contains a summary of care required by the resident is an
kardex
which of the following is (are) a purpose of documentation
a. to provide a record for administration to prove that the nurses have earned their pay
b. to provide a permanent record of medical diagnoses, nursing diagnoses, plan of care, care provided, and the patient response to that care.
c. to serve as a punitive measure for nurses who will not do all the intervention
d. to serve as a record of accountability for quality assurance, accreditation, and reimbursement purposes
b. to provide a permanent record of medical diagnoses, nursing diagnoses, plan of care, care provided, and the patient response to that care.
d. to serve as a record of accountability for quality assurance, accreditation, and reimbursement purposes
The process of providing effective patient care that is delivered and evaluated continuously, systematically and smoothly from one hour to the next, including through the staffing changes between shifts, is known as what?
a. internal assessment
b. accreditation
c. quality assurance
d. continuity of care
d. continuity of care
Which of the following statements is(are) true in reference to the joint commission?
a. the joint commission audits medical records to verify facility compliance in meeting established health care standards
b. the joint commission sets the standards by which the quality of health care is measured nationally and internationally.
c. the joint commission seeks to improve safety and quality of care that health care organization provide to the public.
d. the joint commission is a group of commissioned individuals who collectively represent all the medical insurance companies who set the standards for medical care reimbursement.
a. the joint commission audits medical records to verify facility compliance in meeting established health care standards
b. the joint commission sets the standards by which the quality of health care is measured nationally and internationally.
c. the joint commission seeks to improve safety and quality of care that health care organization provide to the public.
Why do insurance companies review medical records?
a. reimbursement is dependent on documentation of specific data in the medical record.
b. insurance reimbursement depends on the specific consents that the patient or family member have signed
c. records help insurance companies to detect problems, less than desirable outcomes, or area of weakness the delivery systems so that improvement can be made.
d. because the medical record is the property of the patient insurance company.
a. reimbursement is dependent on documentation of specific data in the medical record
which of the following statement regarding a patient hospital medical record is accurate?
a. all the information within the chart belongs to the patient
b. access to a patient medical record is restricted to the physician the nurse and the patient.
c. HIPAA guarantees the patient the right to view his or her own medical record.
d. the patient may not take the original medical record because it is the property of the hospital
e. the medical record belongs to admitting physician.
f. the hospital must provide the patient with a written explanation of how the patients health information will be used
g. the patient has the right to a copy of any or all of his or her own medical records.
a. all the information within the chart belongs to the patient
c. HIPAA guarantees the patient the right to view his or her own medical record.
d. the patient may not take the original medical record because it is the property of the hospital
f. the hospital must provide the patient with a written explanation of how the patients health information will be used
g. the patient has the right to a copy of any or all of his or her own medical records.
what is the military time for 1:15 am?
a. 0115
b. 1315
c. 1115
d. 1150
a. 0115
what time would the military time 2210 be?
a. 1022 am
b. 1022 pm
c. 221 am
d. 1010 pm
d. 1010 pm
which of the following would be subjective data?
a. pain
b. itching
c. grimacing
d. flushing
e. 124/74
f. WBC-13,200
g. sleeping
h. snoring
a. pain
b. itching
g. sleeping
Which of the following are sections of a source oriented chart?
a. database
b. graphic sheet
c. laboratory
d. medication administration record
e. nurses notes
f. physician progress notes
b. graphic sheet
c. laboratory
d. medication administration record
e. nurses notes
f. physician progress notes
which of the following types of data should be included in weekly summaries in a long-term care facility?
a. use of prosthesis
b. activity level
c. length of time the resident has been at the facility
d. whether continent or incontinent of bowel and bladder
e. whether the resident can speak
f. whether the resident routinely has relatives and visitors
g. social activities in which the resident participates
h. staff members with whom the resident does not get along
i. ability to bathe and feed self, including type of bath
j. type of diet, percentage generally consumed
k. whether the resident is self pay or third party reimbursement
a. use of prosthesis
b. activity level
d. whether continent or incontinent of bowel and bladder
e. whether the resident can speak
f. whether the resident routinely has relatives and visitors
g. social activities in which the resident participates
i. ability to bathe and feed self, including type of bath
j. type of diet, percentage generally consumed
which of the following charting "omission" (meaning they were not charted) would carry potential legal risk just by the nature of the omission?
a. the time a patient consumed his or her evening meal
b. a rash and swelling noted during assessment
c. the fact that the patient has a history of hemophilia
d. a physicians order for a medication
e. the nurse instructed the patient that he needs to increase oral intake
f. noting of a physicians order to make a patient NPO
b. a rash and swelling noted during assessment
c. the fact that the patient has a history of hemophilia
d. a physicians order for a medication
f. noting of a physicians order to make a patient NPO
you can safely delegate documentation of certain data to an unlicensed staff member. which of the following data cannot be delegated?
a. administration of medication
b. documenting vital signs
c. items on a patient care flow sheet, such as type of bath, ambulation, or percentage of diet consumed
d. items on a patient care flow sheet, such as prn use of oxygen, that heart sounds are distinct, or presence of edema.
a. administration of medication
d. items on a patient care flow sheet, such as prn use of oxygen, that heart sounds are distinct, or presence of edema.
T or F
statistics such as rates of hospital-acquired infections, mortality rates, success rates of specific procedures, and number of incidents and accidents serve as factors of a medical facility reputation.
True
T or F
Failure to document administration of medication does not carry a potential legal risk?
False
T or F
A federal law known as OBRA mandates that an extensive assessment form called the MDS must be completed on every patient admitted to the hospital
True
T or F
the omission of a patient latex allergy in his medical history carries a potential legs risk
True
T or F
An advantage of computerized documentation is that it is easy to read.
True
T or F
In charting by exception, normal findings are charted and checklists are used for routine care
True
T or F
When documenting patient teaching, the only thing that must be included is the subject that was taught and the methods used to teach the subject
False
T or F
If your cursive writing is not legible, you must print your documentation on a paper chart
True
T or F
The only time that it is okay to share your computer password with another student or coworker is if he or she is going to document vital signs for you
False
What can you do to help ensure the intended recipient is the only one who receives a faxed medical record you send?
Telephone the intended recipient to let him or her know
that the document's arrival is imminent.
When documenting with focus charting, which acronym is generally used?
a. soap
b. soapier
c. pie
d. DAR
c. pie
when using electronic (or computerized) documentation which process should the nurse use to ensure that no one alters the information the nurse has entered?
a. charting in code
b. logging off
c. charting in privacy
d. signing on with a password
b. logging off
Which are accurate statement about EHR?
a. it is a record of the patient interaction with the primary care doctor, but not with specialist
b. it is a record of an individuals lifetime health information easily updated and transferable
c. it has built-in security and confidentiality, so nurses do not have to take any additional precautions
d. the nurse is only supposed to access the record of the patient that he or she cares for, not every patient on the nursing unit
e. it is only available on hand held computers.
b. it is a record of an individuals lifetime health information easily updated and transferable
d. the nurse is only supposed to access the record of the patient that he or she cares for, not every patient on the nursing unit
in which facilities might EHR be used?
a. hospital
b. clinics and HCP offices
c. laboratories
d. pharmacies
e. home health
a. hospital
b. clinics and HCP offices
c. laboratories
d. pharmacies
e. home health
List at least 9 to 10 categories of specific data that should be documented for every patient.
physical assessment findings; nutrition; hygiene
provided; activity level; physician visits; elimination,
both bowel and bladder; nursing care provided; patient's
responses to nursing care; safety issues; laboratory,
x-ray, and other diagnostic tests that were prepped
and done; all patient complaints.
Which of the following rule(s) do(es) not apply to paper documentation?
a. avoid leaving blank lines
b. write in complete sentences using correct grammar
c. capitalize the first letter of the first word of each phrase.
d. the only subjective data that you should document are that which the patient or patients family members may tell you verbally
e. use only approved abbreviations
f. attempt to accurately label the patients behaviors with terms that are descriptive
g. end each phrase or sentence with a period.
b. write in complete sentences using correct grammar
f. attempt to accurately label the patients behaviors with terms that are descriptive
Guidelines for paper documentation include which of the following?
a. all documentation for your shift must be signed after you have charted your last entry for the shift
b. all documentation must be done in cursive writing
c. charting should be done in blocks of time to reduce the number of unnecessary entries
d. the date and time should be included with each entry.
d. the date and time should be included with each entry.
The correct signature for documentation includes which of the following?
a. first and last names
b. first name, last initial and credentials
c. first initial, middle initial, last initial and credentials
d. first name, middle name, and last name
e. first initial, last name, and credentials
e. first initial, last name, and credentials
some of the following documentation phrases include subjective terminology that needs to be changed to objective terminology. select the phrases with subjective terms and underline the subjective word(s) that need(s) to be changed to objective.
a. snored loudly most of night between 0030 and 0530
b. green purulent drainage increased from yesterday ABD pad has 6" circle of drainage.
c. procedure tolerated well
d. ADA diet-ate 75% tolerated poorly
e. bouncing foot almost continually. rubbing hands and flicking finger with thumb at intervals. verbally denies feeling nervous or anxious
f. got mad while ambulating in the hall
g. has a bad attitude.
c. procedure tolerated well
d. ADA diet-ate 75% tolerated poorly
e. bouncing foot almost continually. rubbing hands and flicking finger with thumb at intervals. verbally denies feeling nervous or anxious
f. got mad while ambulating in the hall
g. has a bad attitude.
Occurrences that should be documented on an incident report from include some of the following. which ones are included?
a. a patient fall
b. a medication error
c. a 1/4 inch scrape on a visitors leg from brushing the leg against the edge of the wheelchair
d. a lack of supplies needed to perform a procedure
e. a nursing assistant bumped her head on the television mounted on the wall
f. an unsafe staffing situation for the number and type of patients on the unit
a. a patient fall
b. a medication error
c. a 1/4 inch scrape on a visitors leg from brushing the leg against the edge of the wheelchair
d. a lack of supplies needed to perform a procedure
e. a nursing assistant bumped her head on the television mounted on the wall
f. an unsafe staffing situation for the number and type of patients on the unit
which of the following entries are succinct?
a. I took her temp and it was up to 104.2 degrees Fahrenheit
b. after giving a complete bed bath, oral care was performed with toothpaste, toothbrush, and mouthwash. lotion was applied liberally over arms, back, legs, feet and hands. Her feet and back were massaged for quite a while.
c. 18 Fr. Foley cath inserted without difficulty and hung to gravity drainage. returned 275 ml clear pale yellow urine.
d. the patient said she is really nauseated badly but that she hasnt vomited yet. she asked for her nausea medication that comes in an injection.
e. C/O constant sharp, stabbing pain in Rt, great toe, began 1 hr afo, now a 7 on 0-10 scale.
c. 18 Fr. Foley cath inserted without difficulty and hung to gravity drainage. returned 275 ml clear pale yellow urine.
e. C/O constant sharp, stabbing pain in Rt, great toe, began 1 hr afo, now a 7 on 0-10 scale.
Which of the following phrases are written objectively?
a. ate 45% full liquid diet. did not act very hungry and acted like sh should not have drunk all that she did
b. complaining of really severe pain and wants some thing for it
c. ambulated unassisted the length of hallway without complaints of fatigue or shortness of breath
d. does not feel good today. angry and depressed
c. makes good eye contact, smiling. states feels much better today than yesterday
c. ambulated unassisted the length of hallway without complaints of fatigue or shortness of breath
c. makes good eye contact, smiling. states feels much better today than yesterday
when you use an EHR, you may enter information in which of the following ways?
1. hand held computer
2. computer at a computer station in the hallway
3. computer at the nurses station
4. bedside terminal in the patient room
5. your personal laptop wherever it is convenient
1. hand held computer
2. computer at a computer station in the hallway
3. computer at the nurses station
4. bedside terminal in the patient room
Which of the following times during a 7 am to 7 pm shift would be appropriate to document on a patient chart?
a. as soon as possible after an occurrence or event
b. once at the begining of the shift, again about midway through the shift, and the last time at the end of the shift
c. before the physician makes morning rounds at 1015 am
d. following the performance of physical assessments
e. not until all your patient care has been completed for the shift
f. at least every 2 hrs
a. as soon as possible after an occurrence or event
c. before the physician makes morning rounds at 1015 am
d. following the performance of physical assessments
e. not until all your patient care has been completed for the shift
which of the following entries are good examples of succinct charting?
1. bed bath was given and teeth brushed. hair was shampooed and tangles combed out. soaked fingernails in warm soapy water for 20 min. then filed them and cleaned them using an orange stick. legs were shaved and lotion applied to all pressure points and area of dry skin. gave her a back rub.
2. sacral wound measures 2by4 cm with 1cm depths, circumferences by 0.5 cm dark erythema. no granulation noted. moderate amount foul smelling green purulent drainage.
3. patient is having moderate amount of cramping in her abdomen. it seems to be from her uterus. when I inquired, the patient said it is time for her to start her menses. The patient also said she usually does not experience premenstrual cramping.
4. BP 124/72, T 98.8 orally, P 64 strong and reg. r 17 reg and even
2. sacral wound measures 2by4 cm with 1cm depths, circumferences by 0.5 cm dark erythema. no granulation noted. moderate amount foul smelling green purulent drainage.
4. BP 124/72, T 98.8 orally, P 64 strong and reg. r 17 reg and even
What type of documentation would you, as a nurse, be responsible for performing in the section marked physician orders?
1. the patient plan of care to be followed
2. the vital signs taken during your shift along with the I&O total
3. Transcription date, time, and your initials
4. when you noted the orders
5. verbal order given to you by the physician
6. nursing orders
3. Transcription date, time, and your initials
4. when you noted the orders
5. verbal order given to you by the physician
In a source oriented medical record, which of these would be found in the nurse notes section?
1. nurse assessment data
2. HCP assessment data
3. patient response to initiation of IV therapy
4. patient living will
5. report of chest x ray result
6. patient complains of incision pain
1. nurse assessment data
3. patient response to initiation of IV therapy
6. patient complains of incision pain
Which document would be found in the advanced directive section of sources oriented medical record?
1. signed surgical consent
2. living will
3. discharge plans
4. treatment plan for the diagnosis
2. living will
which setting may use kardexes and paper charts?
1. inpatient hospitals
2. outpatient surgery center
3. home health care
4. long term care
4. long term care
when working in long-term care, the nurse is required to document assessment data on a resident how often?
1. every 2 hrs
2. every 24 hrs
3. every week
4. every month
3. every week
CBE (charting by exception)
A type of charting in which only variances from "normal" in all activities of daily living, vital signs, and assessment findings are charted as entries. This method of charting is designed to drastically reduce time spent completing paperwork; however, opinions vary about its efficacy and safety
Documentation
The act of charting or making a written notation of all the things that are pertinent to each patient for whom a nurse provides care
EHR (electronic health record)
A computerized database that typically includes present and past medical and surgical information, laboratory, radiographic and drug information about a patient; most also contain billing and insurance information as well.
Focus Charting
A type of charting that is focused on the patient and patient concerns, problems, and strengths. Unlike PIE charting, there is not a constructed list of specific problems. It includes data, action, and response
Kardex
A type of flip chart with a page for each patient on a unit or floor that contains a summary of care required by the patient; it requires continual updating and maintenance by nursing staff
Pie Charting
A type of charting styles that is shorter and documents fewer data than the SOAPIER charting style. It only addresses the patient's problems; therefore, the concept of treating the patient holistically is lost. It stands for problem, interventions, and evaluation.
Patients chart
A combination of several different written forms making up a record of the visit
SOAPIER charting
One of the lengthier documentation formats that typically is used in progress notes and the nurse's notes. It includes subjective data, objective data, assessment data, a plan, an intervention, an evaluation, and, as needed, a revision.
medical record
A collection of data recorded when a patient seeks medical treatment.
Written Documentation
Serves at least 4 purposes:
1. To communicate pertinent data that all health-care team members need in order to provide continuity of care.
2. To provide a permanent record of medical diagnoses nursing diagnosis, the plan care, the care provided, the patient's response to that care
3. To serve as a record of accountability for quality assurance accreditation, and reimbursement purposes
4. To serve as a legal record for both the patient and the health-care provider
Diagnostic
Determines the cause of a particular health problem
HITECH
Health Information Technology for Economic and Clinical Health Act
MARS (Medication Administration Record)
The electronic Medication Administration Record (MAR or eMAR) is used to electronically track and record administration of most medications at UHN. The MAR serves as a legal document for UHN's drug administration, with the exception of out-of-scope drugs that are currently still being documented on paper.
Incident report
A report documenting an incident and the response to the incident; also known as an occurrence report or event report.
Which of the following phrases are written objectively?
1. "Ate 45% full-liquid diet. Did not act very hungry and acted like she should not have drunk all that she did."
2. "Complaining of really severe pain and wants something for it."
3. "Ambulated unassisted the length of hallway without complaints of fatigue or shortness of breath."
4. "Does not feel good today. Angry and depressed."
5. "Makes good eye contact, smiling. States feels 'much better today than yesterday.'"
3 ("Ambulated unassisted the length of hallway without complaints of fatigue or shortness of breath.")
5 ("Makes good eye contact, smiling. States feels 'much better today than yesterday.'")
When you use an EHR, you may enter information in which of the following ways?
1. Hand-held computer
2. Computer at a computer station in the hallway
3. Computer at the nurses' station
4. Bedside terminal in the patient's room
5. Your personal laptop wherever it is convenient
1. Hand-held computer
2. Computer at a computer station in the hallway
3. Computer at the nurses' station
4. Bedside terminal in the patient's room
Which of the following times during a 7 a.m. to 7 p.m. shift would be appropriate to document on a patient's chart?
1. As soon as possible after an occurrence or event
2. Once at the beginning of the shift, again about midway through the shift, and the last time at the end of the shift
3. Before the physician makes morning rounds at 10:15 a.m.
4. Following the performance of physical assessments
5. Not until all your patient care has been completed for the shift
6. At least every 2 hours
1. As soon as possible after an occurrence or event
3. Before the physician makes morning rounds at 10:15 a.m.
4. Following the performance of physical assessments
5. Not until all your patient care has been completed for the shift
Which of the following entries are good examples of succinct charting?
1. "Bed bath was given and teeth brushed. Hair was shampooed and tangles combed out. Soaked fingernails in warm soapy water for 20 minutes, then filed them and cleaned them using an orange stick. Legs were shaved and lotion applied to all pressure points and areas of dry skin. Gave her a back rub."
2. "Sacral wound measures 2 × 4 cm with 1-cm depth. Wound bed pale and dry, with 1-cm black eschar center circumferenced by 0.5-cm dark erythema. No granulation noted. Moderate amount foul-smelling green purulent drainage."
3. "Patient is having moderate amount of cramping in her abdomen. It seems to be from her uterus. When I inquired, the patient said it is time for her to start her menses. The patient also said she usually does not experience premenstrual cramping."
4. "BP - 124/72, T - 98.8°F orally, P - 64 strong & reg, R - 17 reg & even."
2. "Sacral wound measures 2 × 4 cm with 1-cm depth. Wound bed pale and dry, with 1-cm black eschar center circumferenced by 0.5-cm dark erythema. No granulation noted. Moderate amount foul-smelling green purulent drainage."
4. "BP - 124/72, T - 98.8°F orally, P - 64 strong & reg, R - 17 reg & even."
What type of documentation would you, as a nurse, be responsible for performing in the section marked Physician’s Orders?
1. The patient’s plan of care to be followed
2. The vital signs taken during your shift along with the I&O totals
3. Transcription date, time, and your initials
4. When you noted the orders
5. Verbal order given to you by the physician
6. Nursing orders
3. Transcription date, time, and your initials
4. When you noted the orders
5. Verbal order given to you by the physician
In a source-oriented medical record, which of these would be found in the Nurse’s Notes section?
1. Nurse’s assessment data
2. HCP’s assessment data
3. Patient’s response to initiation of IV therapy
4. Patient’s living will
5. Report of chest x-ray results
6. Patient’s complains of incisional pain
1. Nurse's assessment data
3. Patient's response to initiation of IV therapy
6. Patient's complains of incisional pain
Which document would be found in the Advanced Directive section of a source-oriented medical record?
1. Signed surgical consent
2. Living will
3. Discharge plans
4. Treatment plan for the diagnosis
2. Living will
Which setting(s) may use Kardexes and paper charts?
1. Inpatient hospitals
2. Outpatient surgery centers
3. Home health care
4. Long-term care
4. Long-term care
When working in long-term care, the nurse is required to document assessment data on a resident how often?
1. Every 2 hours
2. Every 24 hours
3. Every week
4. Every month
3. Every week
The nurse is caring for a resident in a long-term care facility. Which action should the nurse take when charting care about this resident?
1. Sign just the last entry on the page.
2. Use a specific time for each entry.
3. Write illegibly with a black pen.
4. Chart the procedure before it is done.
2. Use a specific time for each entry.
The nurse writes the following in a patient’s chart: Heart tones strong. However, the nurse meant to write weak rather than strong. What should the nurse do?
1. Scratch out strong and add weak.
2. Place correction fluid over strong and then write weak.
3. Write weak over the word strong.
4. Make a single horizontal line through strong and initial it.
4. Make a single horizontal line through strong and initial it.
Which is an appropriate action for the nurse to take when computer charting?
1. Review patient chart that was transferred to another floor for care
2. Allow another nurse to use the password to chart a late entry
3. Log off immediately after charting patient information
4. Copy and paste notes because there has been no change in status
3. Log off immediately after charting patient information
Which action by the LPN/LVN indicates a correct understanding of the LPN’s/LVN’s role in the nursing process?
1. Formulates a nursing diagnosis
2. Develops expected outcomes
3. Performs an admission assessment
4. Carries out interventions
4. Carries out interventions
Place the steps of the nursing process in order.
1. Evaluation
2. Assessment
3. Diagnosis
4. Implementation
5. Planning
2,3,5,4,1
Assessment
Diagnosis
Planning
Implementation
Evaluation
subjective data
things a person tells you about that you cannot observe through your senses; symptoms
objective data
information that is seen, heard, felt, or smelled by an observer; signs
Which patient finding would the nurse report as subjective data?
1. Patient vomited green fluid.
2.Patient has stomach cramps.
3. Patient is rubbing abdomen.
4. Patient moans occasionally.
2.Patient has stomach cramps.
A patient has a fever. Which independent intervention can the nurse implement?
1. Administer acetaminophen every 4 hours.
2. Place a cool washcloth on the patient’s forehead.
3. Start intravenous (IV) fluids for hydration.
4. Obtain blood cultures to determine the cause of fever.
2. Place a cool washcloth on the patient’s forehead.
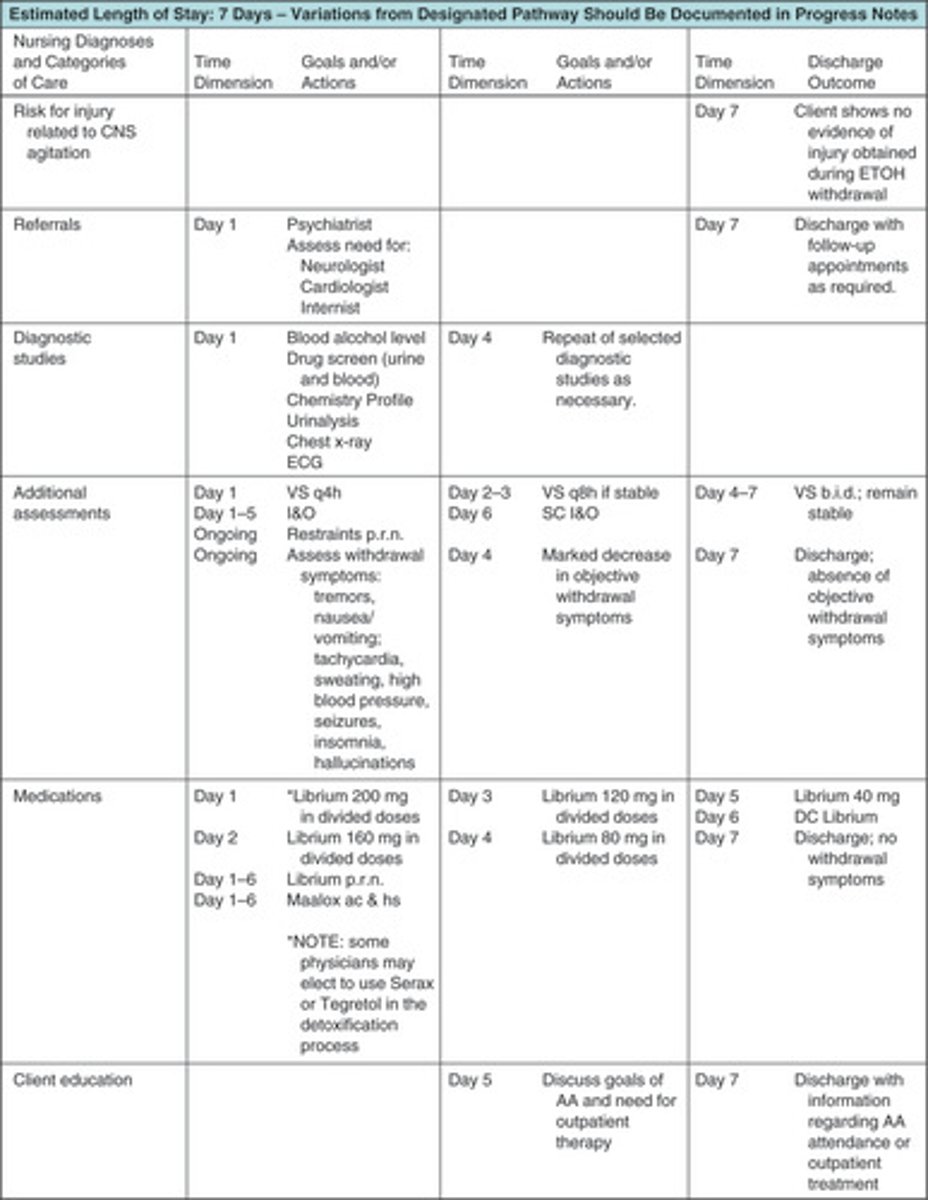
Which type of nursing care plan (see image) is the nurse using?
1. Concept map
2. Critical pathway
3. Computerized care plan
4. Multidisciplinary care plan
2. Critical pathway
Which phrase should the nurse use to describe the nursing process?
1. Written plan of care
2. Decision-making framework
3. Another word for critical thinking
4. Validation of information
2. Decision-making framework
Which charting entry best reflects the nurse’s evaluation of patient learning for constipation?
1. States that was glad to learn about constipation
2. Nodded head in agreement to increase fluids
3. States, “I will eat more high-fiber foods”
4. Seemed to understand instructions
3. States, “I will eat more high-fiber foods”
The nurse changes a dressing and observes a patient’s wound has decreased in size. Where in a problem-oriented medical record would the nurse chart this information?
1. Database
2. Problem list
3. Plan of care
4. Progress notes
4. Progress notes
The nurse spills coffee on a patient’s chart while charting. Which action should the nurse take?
1. Write (continued) at the bottom of the damaged nurse’s notes followed with signature.
2. Throw the damaged page away and start over.
3. Note on the damaged page that the information will be rewritten.
4. Shred the damaged page after notes are recopied word for word.
3. Note on the damaged page that the information will be rewritten.
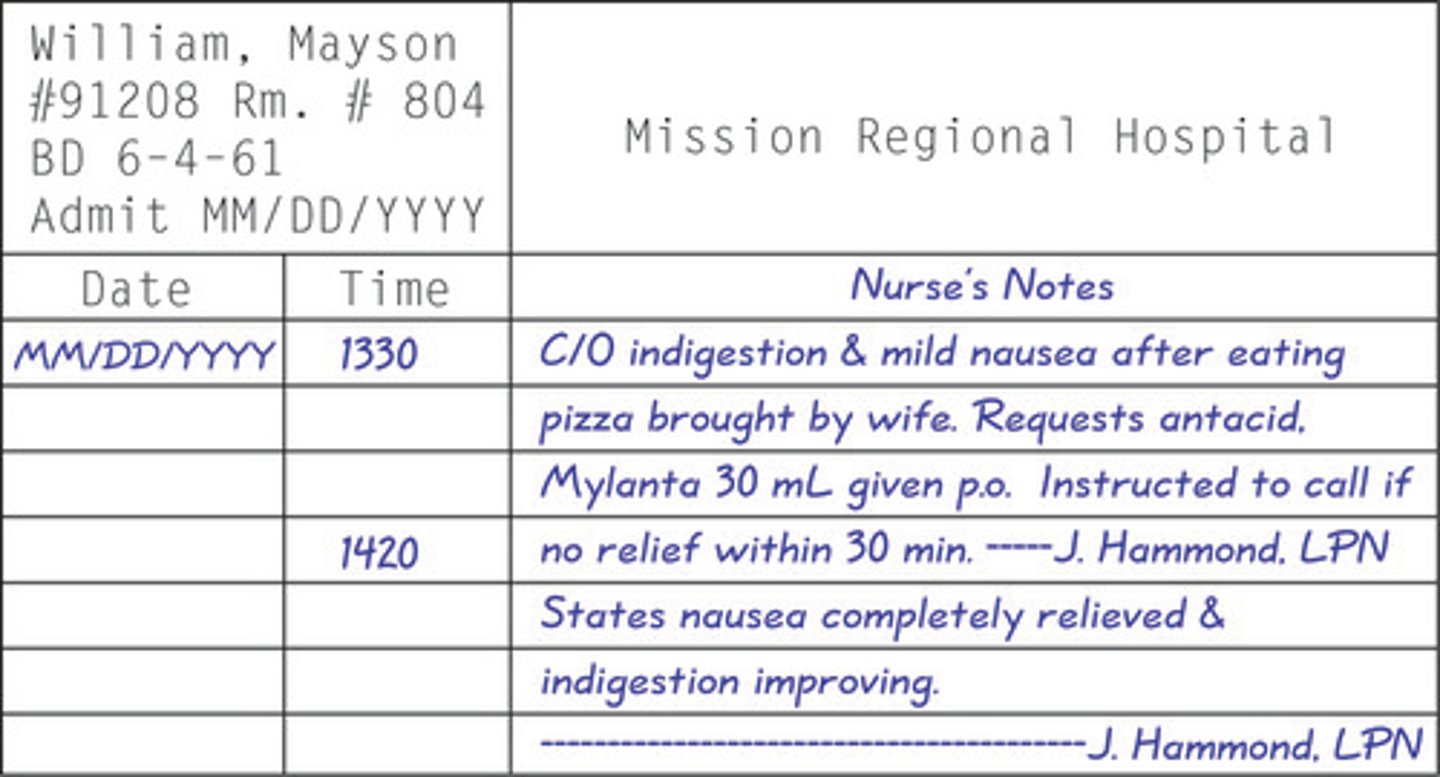
Evaluate the nurses notes below (see image). Which finding could cause the nurse legal issues?
1. Wrote illegibly
2. Used the wrong format for signature
3. Left a blank space in the nurse’s notes
4. Charted with the wrong color of ink
3. Left a blank space in the nurse’s notes
The nurse observes a patient pacing and believes the patient is anxious. Which initial action should the nurse take?
1. Inform the registered nurse.
2. Validate findings with the patient.
3. Notify the primary health-care provider.
4. Document the findings in the patient’s chart.
2. Validate findings with the patient.
The nurse is interviewing a patient about nausea. The patient constantly talks about the possible causes of the nausea. Which response should the nurse make?
1. Nod head and continue to listen
2. Ask, “What have you tried to relieve the nausea?”
3. Say, “I just need the most important facts.”
4. Reply, “Thank you for your time.”
2. Ask, “What have you tried to relieve the nausea?”
Which actions should the nurse take before suctioning a patient who is having problems swallowing? Select all that apply.
1. Gather supplies for the procedure.
2. Identify patient using one method of identification.
3. Explain the procedure to the patient.
4. Lower the bed to its lowest height to reduce falls.
5. Research the procedure on the Internet before performing it for the first time on a patient.
1. Gather supplies for the procedure.
3. Explain the procedure to the patient.
Which information that the nurse gives in report is objective?
1. Patient has severe stomachache.
2. Patient’s blood pressure is 120/70.
3. Patient is apprehensive about surgery.
4. Patient likes grapefruit juice.
2. Patient’s blood pressure is 120/70.
Which expected outcome would the nurse most likely observe written in a patient’s care plan?
1. Patient’s vital signs will be taken every 4 hours until discharge.
2. Patient will rate pain level at a 2 or below by discharge.
3. Patient will have a good understanding of diagnosis by discharge.
4. Patient will lose weight by discharge.
2. Patient will rate pain level at a 2 or below by discharge.
The nurse is using SOAP to chart patient care. Which information would the nurse place after the S?
1. Experiencing impaired gas exchange.
2. Nailbeds bluish, sitting on edge of bed.
3. Notify health-care provider for oxygen.
4. Reports, “Hard to catch breath when I take a deep breath.”
4. Reports, “Hard to catch breath when I take a deep breath.”
The nurse is preparing to reinforce teaching with a patient about medications. Which finding would cause the nurse to proceed with the teaching session?
1. Patient states, “My heart is racing.”
2. Patient feels feverish and is chilled.
3. Patient just received news of cancer diagnosis.
4. Patient has just finished going to the bathroom.
4. Patient has just finished going to the bathroom.