Chapter 28: Head & Spine Injuries
1/116
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
117 Terms
Spinal Cord
Relays messages to brain
Nerve fibers connecting the brain to the body
Spinal Injury Severity
Higher up on the cord the worse the injury is
Spinal Injuries MOI
Compression
Excessive flexion, extension, rotation
Lateral bleeding
Spinal Injury Classifications
Sprains
Strains
Fractures
Dislocations
Sacral fractures
Coccygeal fractures
Cord injuries
Immobilize Patients with...
Suspected spinal trauma
Signs and symptoms of SCI
Assume Spinal Injury if...
Significant trauma and use of intoxicating substances
Seizure activity
Pain/paresthesia in neck/arms
Neck tenderness
Unconsciousness because of head injury
Significant injury above clavicle
Fall more than three times patient's height
Fall and fracture of both heels
Injury from car crash at high speed
Damage Further Complicated by...
Age
Preexisting bone disease
Congenital spinal cord anomalies
When do Primary Injuries Happen?
Occur at time of impact
When do Secondary Injuries Happen and why?
Later due to swelling, ischemia, movement of bony fragments
Cord Injuries
Concussed
Contused
Compressed
Lacerated
Severity of Injuries Depend on...
Amount and type of force
Duration of injury
Cord Lesions Classified by...
Complete
Incomplete
Complete Cord Lesions
Usually spinal fracture/dislocation
Absence of pain, pressure, and joint sensation
Complete motor paralysis below injury
Automatic dysfunction
Signs of Autonomic Dysfunction
Bradycardia
Hypotension
Priapism
Loss of sweating/shivering
Loss of bowel/bladder control
Incomplete Lesions
Central Cord Syndrome
Central Cord Syndrome
Seen with hyperextension or flexion cervical injuries
Greater motor impairment of upper than lower extremities
Signs and Symptoms of Central Cord Syndrome
Paralysis of arms
Decreased sensation of pain and temperature below lesion
Intact light touch and position sensation
Quadriplegia
Inability to move all four limbs or entire body below the neck
Injury at cervical level
Loss of function below injury site
Paraplegia
Total inability to move both legs and usually the lower part of the trunk
Result of disease/injury of spine
Thoracic/lumbar level injury
Loss of lower trunk function
Hemiplegia
Total or partial inability to move experienced on one side of the body, caused by brain disease or injury
Reflex Resposnses
Some indicate autonomic injury
Babinski's sign
Babinski's Sign
Plantal reflex
Dorsiflexion of great toe with or without fanning of toes
Absence of Neurological Deficits...
Does not rule out spinal injury
Ability to walk...
Should not be a factor in determining need for spinal precautions
MOI
Decreased LOC in trauma patient
Pain in spine or paraspinal area
Pain in back of head, shoulders, legs, arms
Absent, altered sensation (numbness, paresthesias, loss of temperature, position, touch sense)
Absent, altered motor functions
Management
ABC with C-spine
Ensure adequate oxygenation, ventilation
Keep entire spine immobilized
Repeatedly assess, document neurologic status
Repeatedly monitor respirations and blood pressure
Neurologic Status
Position sense
Pain
Motion
Treating Spinal Injuries
Instruct the patient not to move
Stablize cervical spine and ABC
Evaluate MOI
Evaluate neurological system
Assess pulse, movement, sensation in extremities
Assess neck and spine
Administer oxygen
Apply properly sized cervical spine immobilization device
Apply and secure patient to appropriate immobilization device
Significant Head Injury =
Neck injury until proven otherwise
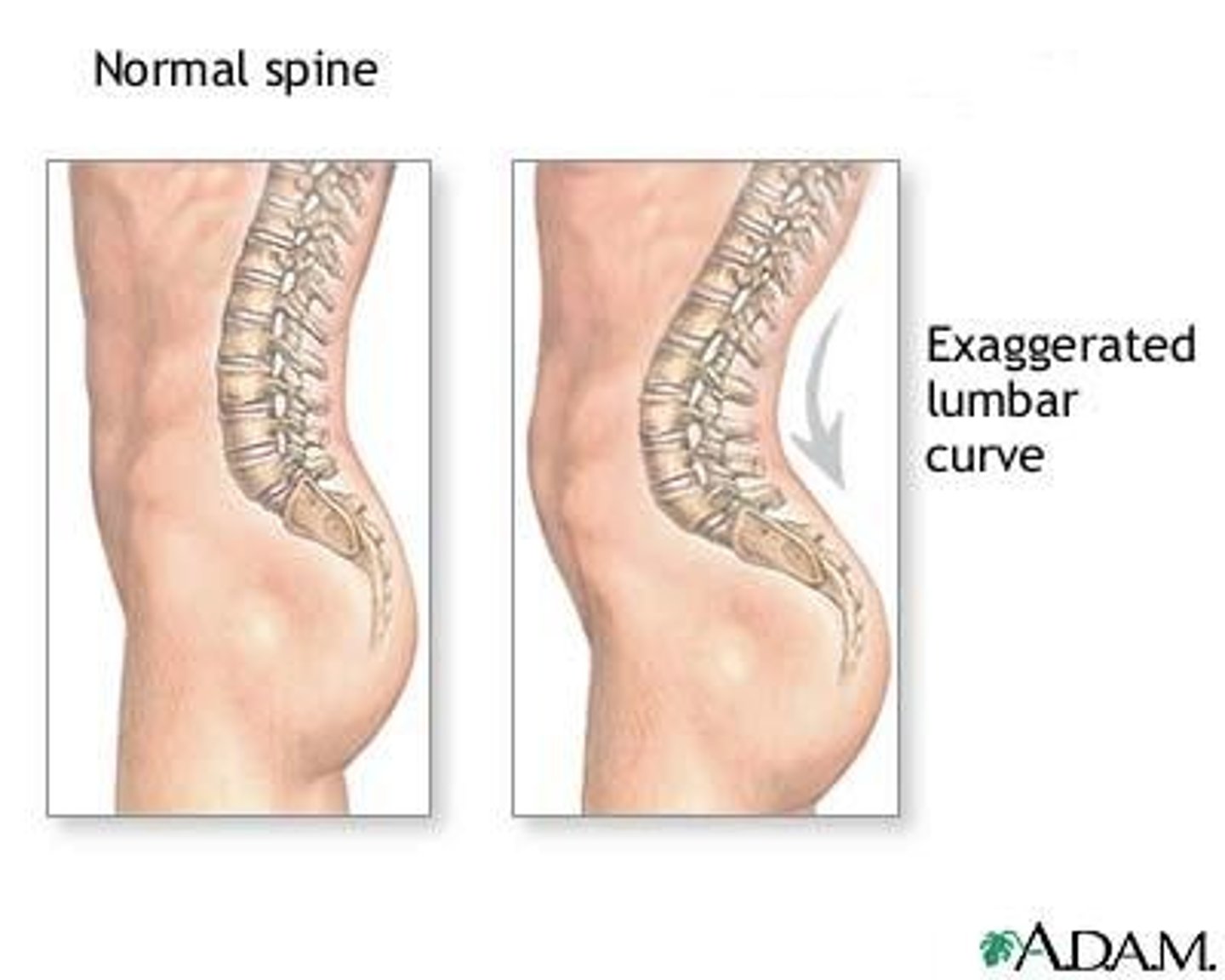
Lordosis
Swayback
Spine of person curves significantly inward at the lower back
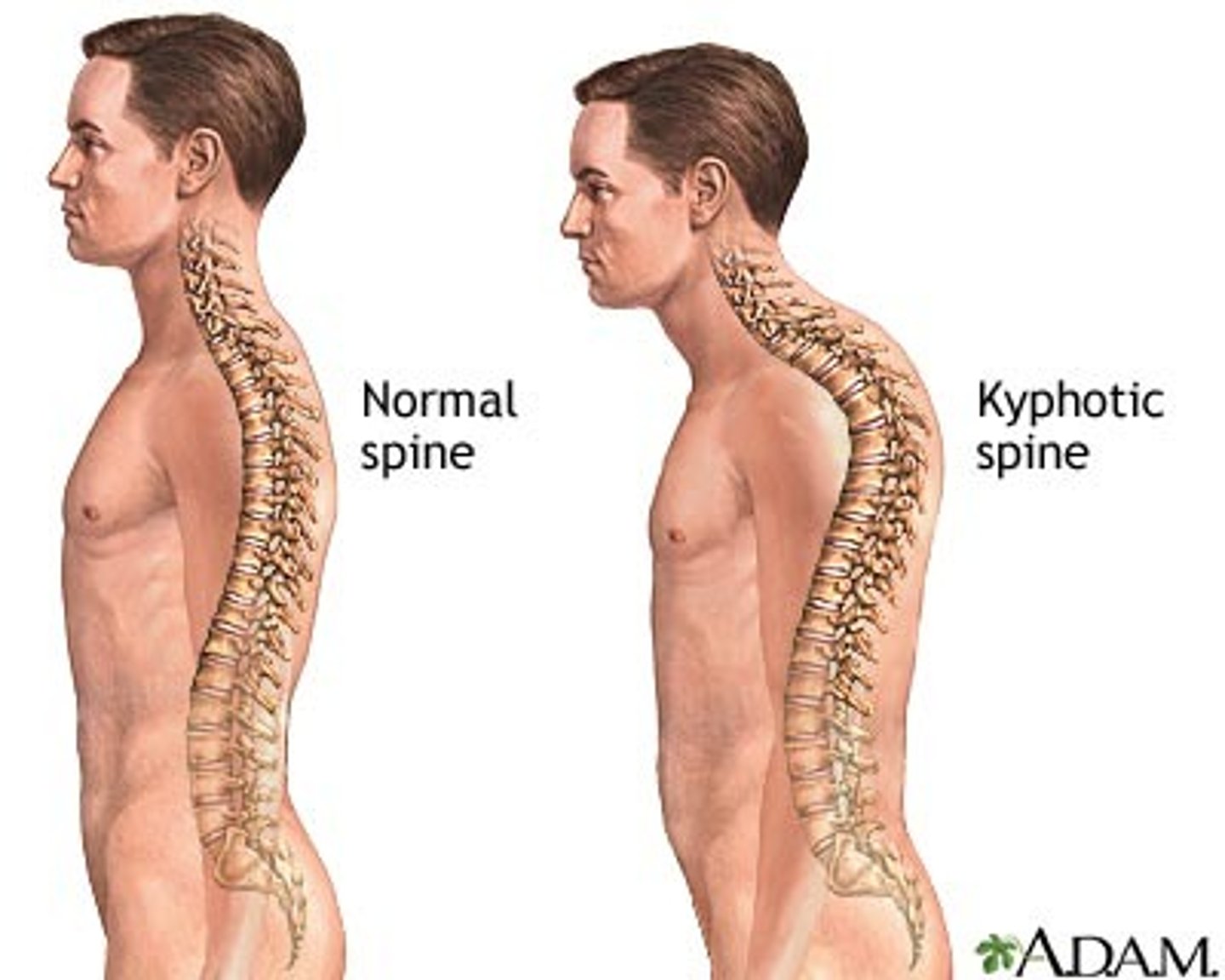
Kyphosis
Abnormally rounded upper back
More than 50 degrees of curvature
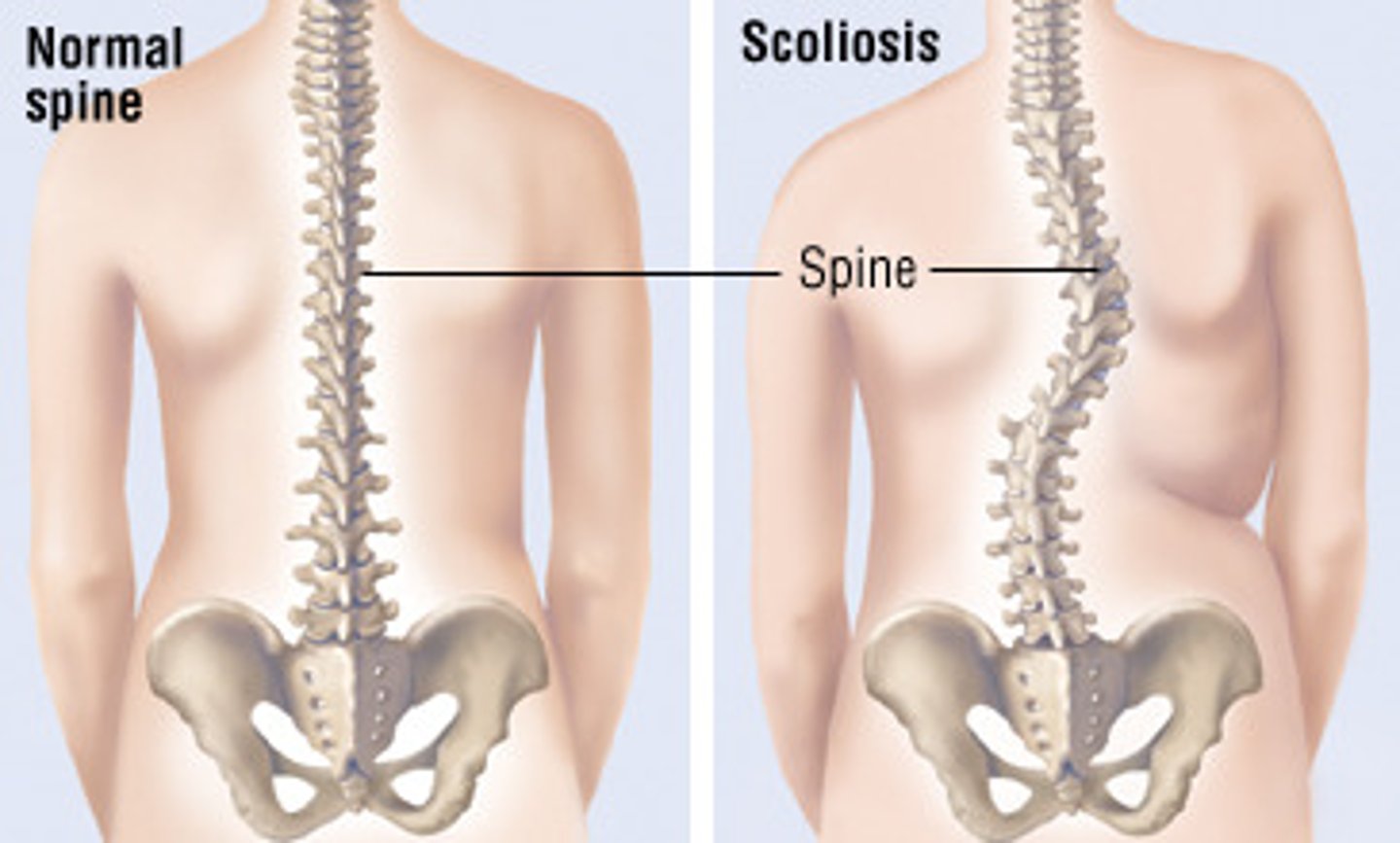
Scoliosis
Sideways curve of spine
S/C shaped
Non-Trauma Transportation
Transport in position of comfort
Trauma Transportation
Move to backboard maintain C spine stabilization
Pad under patient's head if needed
Skull
Divided into 2 major areas
Bones used as locations when describing area involved in injury
2 Areas of Skull
Cranium and face
Lobes of the Brain
frontal, parietal, occipital, temporal

Cerebrum
Most anterior portion of the brain
Largest and most developed portion of the brain
75% of total brain volume
Responsible for movement, sensory processing, olfaction, language and communication, learning and memory
Cerebellum
Controls emotion
Motor control
Coordinates body movement
Language and attention
Brain Stem
Posterior part of the brain
Cranial nerves 2-12 emerge from brain stem
Essential controls of the body such as respiratory, circulatory, pain, consciousness
Common Cause of Brain Disorder
Stroke
Seizures
Altered mental status
Cerebrovascular Accident
CVA
Interruption of blood flow to the brain that results in the loss of brain function
Stroke
Loss of brain function that results from CVA
Maxillofacial Injury Causes
Crashes
Home accidents
Athletic injuries
Animal bites
Intentional violent acts
Industrial injuries
Maxillofacial Trauma Classifications
Soft tissue injuries
Facial fractures
Soft Tissue Injuries
Facial soft injuries often appear serious
Usually not life threatening, except when compromised airway, potential for significant bleeding
History of Patient
MOI
Events leading up to injury
Time of injury
Associated medical problems
Allergies
Medications
Last oral intake
Management of Head/Facial Trauma
Spinal precautions
Assess for airway obstructions
Secure/Maintain airway
Ensure ventilation and oxygenation
Control bleeding
Facial Fractures
Common after blunt trauma
Fractures of the mandible
Dislocations of the mandible
Fractures of Zygoma
Articulates with frontal, maxillary, and temporal lobes
Associated with orbital fractures with similar clinical signs
Zygoma
Cheekbone
Fractures of the Orbit
Blowout fractures to orbit
Suspect injury to orbital contents with any facial fracture
Fracture of Nose
Most often fractured
Displace to one side or epistaxis and swelling without skeletal deformity
Epistaxis
Nosebleed
Apply external pressure to anterior nares
Conscious patient- Seat upright/leaning forward with EMT compress nares
Unconscious patient- Positioned on side and treat for shock if bleeding is severe
Management of Facial Fractures
Assume spine is injured and use spinal precautions
Assess airway for obstruction
Ensure adequate ventilation and oxygenation
Control bleeding through direct pressure and bandages
Control epistaxis by external direct pressure
Nasal and Ear Foreign Bodies
Foreign bodies in nose or ear common in children
Remove foreign body in ear if easy
Do not remove nasal foreign body unless airway is compromised or it can be removed without equipment
Ear Trauma
Lacerations and contusions
Usually blunt trauma
Treated with direct pressure to reduce bleeding and ice/cold compress to reduce swelling
Never use pressure to stop bleeding out of the ear canal
Retrieve avulsed tissue if possible wrap in moist gauze, seal in plastic, place on ice, transport for surgical repair
Thermal
Chemical
Traumatic perforations
Eye Trauma Causes
Crashes
Sports activities
Violence
Chemical exposure
Foreign bodies
Animal bites/scratches
Eye Trauma Evaluation
History (mode of injury and use of corrective glasses/contact lenses)
Visual activity (test injured eye and compare to uninjured)
Pupillary reaction
Eye movement
Specific Eye Injuries
Ocular trauma should be evaluated by physician
Foreign bodies
Corneal abrasion
Blunt trauma
Penetrating injury
Protruding intraocular foreign bodies
Chemical injuries to the eye
Contact Lenses
Hard lenses
Soft Hydrophilic lenses
Rigid gas-permeable lenses
Do not remove contact lenses
Plastic lenses can mix with chemical and fuse to cornea
Dental Trauma
32 teeth in adult
Crown and root
Hard and soft tissue of tooth
Tooth Fracture
Tooth Avulsion
Anterior Neck Trauma
Blunt and penetrating trauma
Can damage... skeletal structures, vascular structures, nerves, muscles, and glands of neck
Common MOI of Anterior Neck Trauma
Crashes
Sports activities
Industrial accidents
Violence
Hangings
Evaluation of the neck: Zones
Zone I
Zone II
Zone III
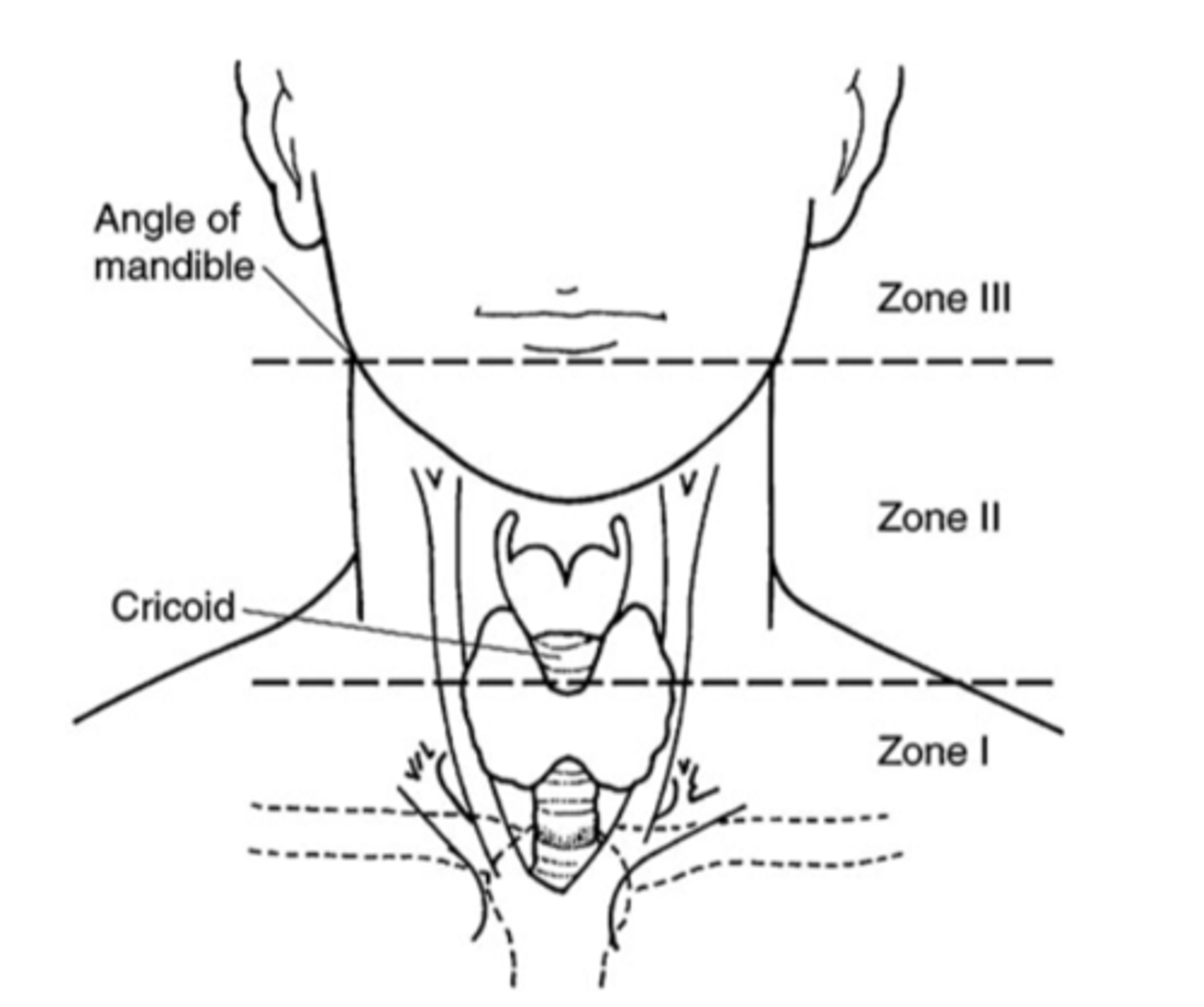
Zone I
Injuries carry highest mortality rate
Zone II
Most common injuries
Lower mortality rate than zone I
Zone III
Greatest risk of injury to distal carotid artery, salivary glands, and pharynx
Asphyxiation
Suffocation
Edema
Swelling
Edema of pharynx, larynx, trachea, epiglottis, and vocal cords may obstruct airways
Measures to Treat Edematous Airways
Cool, humidified oxygen
Slight elevation of patient's head
Lacerations and Puncture Wounds
Superficial Injuries
Deep Penetrating Wounds
Superficial Injury Management
Cover the wound
Deep Penetrating Wound Management
Aggressive airway therapy
Ventilatory support
Suction
Hemorrhage control (direct pressure)
Signs and Symptoms of Significant Penetrating Neck Trauma
Shock
Active bleeding
Tenderness on palpation
Mobility
Crepitus
Large or expanding hematoma
Pulse deficit
Neurological deficit
Dyspnea
Hoarseness
Stridor
Subcutaneous emphysema
Hemoptysis
Dysphagia
Hematemesis
Vascular Injury Management
Secure airway with spinal precautions
Adequate ventilatory support
Control hemorrhage by direct pressure
Fluid replacement for hypovolemia guided by medical direction
Esophageal Injury Suspect in Patients with...
Trauma to chest or neck
Tracheal fractures
Penetrating trauma from stab or gunshot wounds
Ingestion of caustic substances
Esophageal Injury Signs/Symptoms
Subcutaneous emphysema
Neck hematoma
Oropharyngeal/nasogastric blood
Subcutaneous Emphysema
Air under the skin
Esophageal Varices
Thinking of esophageal lining
Head Trauma: Scalp
Subcutaneous Tissue (major scalp veins bleed profusely)
Muscle (Attached above eyebrows at base of occiput)
Galea (Freely movable sheet of connective tissue and helps deflect blows)
Loose Connective Tissue (contains emissary veins that drain intracranially)
Soft Tissue Injuries to the Scalp
Irregular linear laceration
May lead to profuse bleeding and hypovolemia
Soft Tissue Injuries to the Scalp Management
Prevent contamination of open wounds
Direct pressure or pressure dressings to decrease blood loss
Consider potential for underlying skull fracture and brain and spinal trauma
Classification of Skull Fractures
Linear
Basilar
Depressed
Open Vault
Linear Fractures
80% of fractures to skull
Not usually depressed
May occur without an overlaying scalp laceration
Generally low complication rate
Basilar Fracture
Battle Signs
Raccoon Eyes
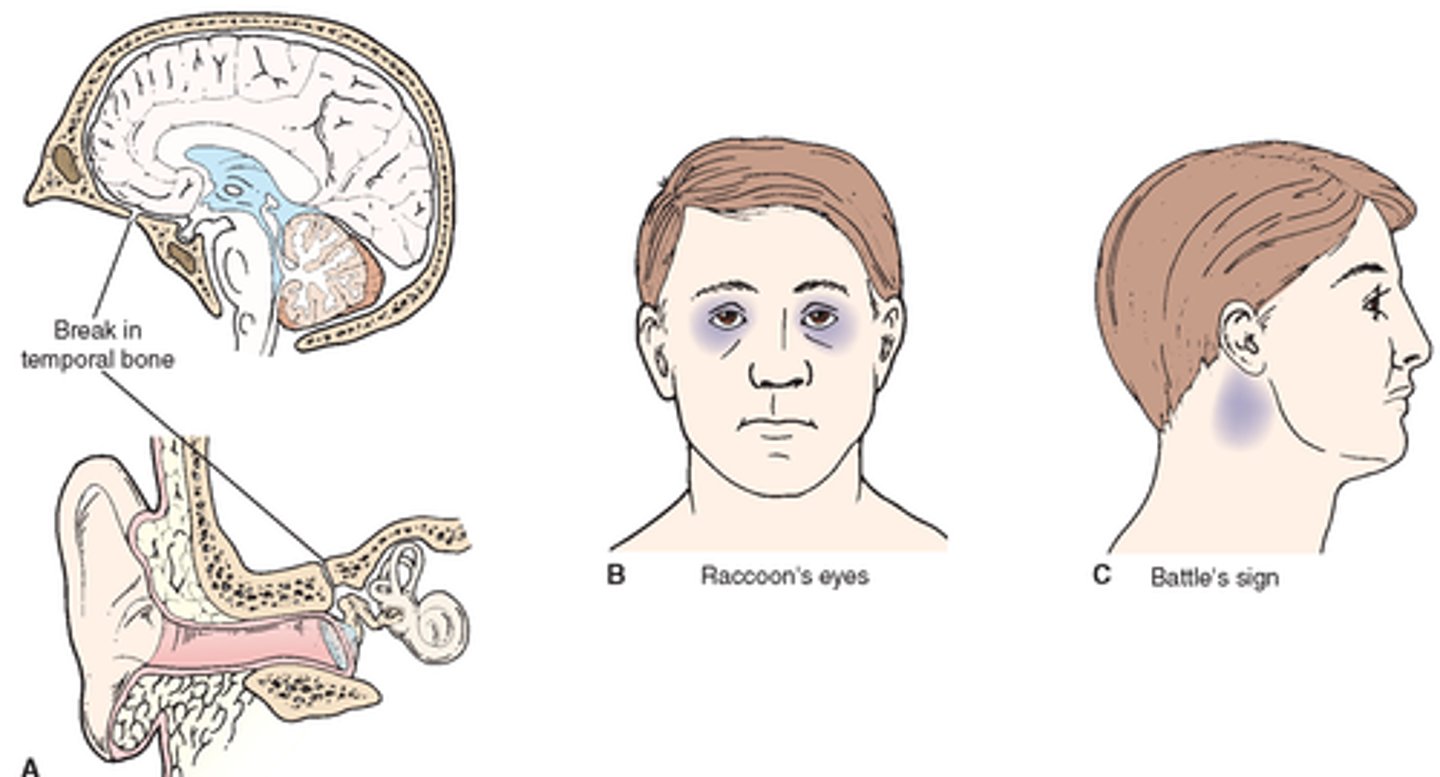
Battle Signs
Mastoid ecchymosis
Indication of fracture of base of the posterior portion of the skull
Raccoon Eyes
Purplish discoloration around the eyes following fracture of the frontal portion of the skull base
Depressed Fractures
Relatively small object strikes head at high speed
Often scalp lacerations
Frontal and parietal bones most often affected
Open Vault Fractures
Direct communication between scalp laceration and cerebral substance
Often occur with multi-system trauma
High mortality rate
May lead to infection (meningitis)
Types of Head Injuries
Open and Closed
Head Injury Symptoms
Nausea
Severe headache
Glossy eyes
Sudden sleepiness
Head Injury
May appear minor but can be life-threatening
Scalp lacerations may not have any brain involvement but can bleed severely leading to significant blood loss
Cerebral Spinal Fluid
CSF
Clear, watery fluid
Produced in the third ventricle, a chamber in the brain
Acts as a shock absorber to spinal cord and brain
Protects brain from being injured, if injured the fluid comes out ears to give room for brain to swell
Halo Test
Detects CSF
Brain Injury
Traumatic or Non-traumatic
Altered or decreased mental status
Irregular breathing patterns
MOI present with traumatic injury
Brain Injury Symptoms
Contusion
Laceration
Hematoma
Blood/fluid from ears/nose
Bruising around eyes and behind ears
Neurologic changes
Nausea/vomiting
Unequal pupil size
Decreased heart rate and increased blood pressure
Seizures
Assessment of Head Injury
Early detection of increased intracranial pressure is critical
If pressure inside skull exceeds average blood pressure, blood flow to brain stops
Increasing intracranial pressure can force brain down into spinal canal, crushing it
AVPU system
Glasgow scale
Vital signs
Vital Signs in Head Injury
Body responds to increasing intracranial pressure by raising blood pressure
Increased BP moves blood into brain against rising ICP
Heart rate falls in response to rising BP
Cushing's Triad
Increased blood pressure
Altered breathing
Slow pulse