Digestive Tumors
1/87
Earn XP
Description and Tags
Principles of Oncology Exam 3
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
88 Terms
What cancer is Skip Mets associated with?
Esophageal Cancer
What are skip mets?
cancerous lymph node groups at distant sites from primary tumor
longitudinal lymph fluid along esophagus
make lymph spread unpredictable
What are the 4 regions of the esophagus?
Cervical
Upper thoracic
Middle thoracic
Lower thoracic
At what levels is the cervical portion of the esophagus?
Cricorid cartilage (C6) to SSN (T2-3)
At what levels is the upper thoracic portion of the esophagus?
SSN (T2-3) to Carina (T4-5)
At what levels is the middle thoracic portion of the esophagus?
Carina (T4-5) to EG junction
At what levels is the lower thoracic portion of the esophagus?
EG junction to T10-T11
What is the etiology/risk factors of esophageal cancer?
Excessive smoking and alcohol (most common)
Barrett’s syndrome
Achalasia
What is Barrett’s syndrome?
Mucosal changes (stratified squamous to columnar) in distal esophagus due to long-term GERD
What is Achalasia?
Esophagus loses the ability to contract and relax
Have an increased risk of dysphagia and regurgitation
Clinical presentations of Esophageal cancer?
weight loss
dysphagia
What detections are used for esophageal cancers?
Barium swallow test/ GI upper series
What is the purpose of Barium swallow test/ GI upper series?
Allows the clinical staff to visualize the tumor
What is the most common site of occurrence for esophageal cancers?
the lower 1/3 of esophagus (lower thoracic)
What is the pathology for the Upper 2/3rds of the esophagus?
Squamous Cell Carcinoma
What is the most common pathology for esophageal cancers and where does it occur?
Adenocarcinoma
occurs in distal 1/3 (lower thoracic)
associated with barrett’s syndrome
What are the most common mets for esophageal cancers?
liver
lung
What are the primary goals of treatment for esophageal cancers?
provide relief for dysphagia
a chance for a cure
What is the most common treatment method for esophageal cancers?
Chemo + radiation = chemoradiation
What are the radiation techniques for esophageal cancers?
AP/PA with off-cord boost at 45 GY
VMAT
What are the organs at risk for esophageal cancers?
heart
lungs
esophagus
spinal cord
liver
kidneys
What is the TD 5/5 for the heart?
40 Gy (4000 cGy)
What is the TD 5/5 for the lungs?
17.5 Gy (1750 cGy)
What is the TD 5/5 for the esophagus?
55 Gy (5500 cGy)
What is the TD 5/5 for the spinal cord?
47 Gy (4700 cGy)
What is the TD 5/5 for the liver?
30 Gy (3000 cGy)
What is the TD 5/5 for the kidney?
23 Gy (2300 cGy)
Surgery is the option for which esophageal cancers?
middle and lower thoracic tumors
If entire esophagus is removed, stomach/ left colon is placed in thoracic cavity
Acute side effects of esophageal cancers
Esophagitis (most common)
decreased blood count
Nausea and vomiting (chemo)
What does esophagitis result in for esophageal cancers?
dysphagia (eat small food/many small meals, frequent weight checks)
odynophagia (liquid analgesics before food, TB)
Chronic side effects associated with esophageal cancers
pneumonitis
pericarditis
fistula
stenosis and stricture
What is the etiology/risk of stomach cancer?
Diet:
salted/pickled food
high nitrites
low fruit and veggies
What is the pathology for stomach cancer?
Adenocarcinoma (most common)
What chemotherapy drug is used for stomach cancer?
5-FU (fluorouracil)
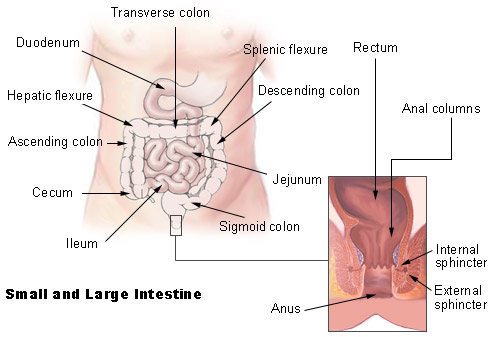
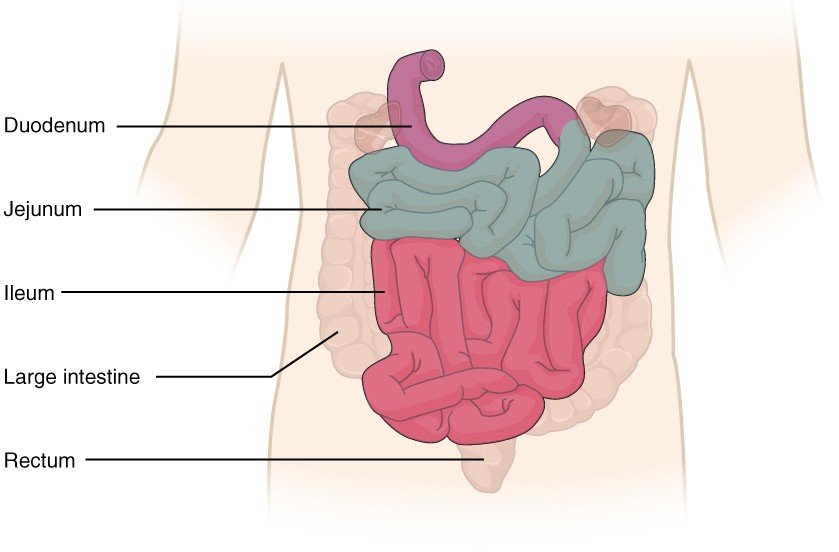
What are the parts of the small intestine?
duodenum (upper)
jejunum (middle)
ileum (lower)
What is the most common histology/pathology of small intestine cancer
Adenocarcinoma
What is the main treatment for small intestine cancers?
Surgery
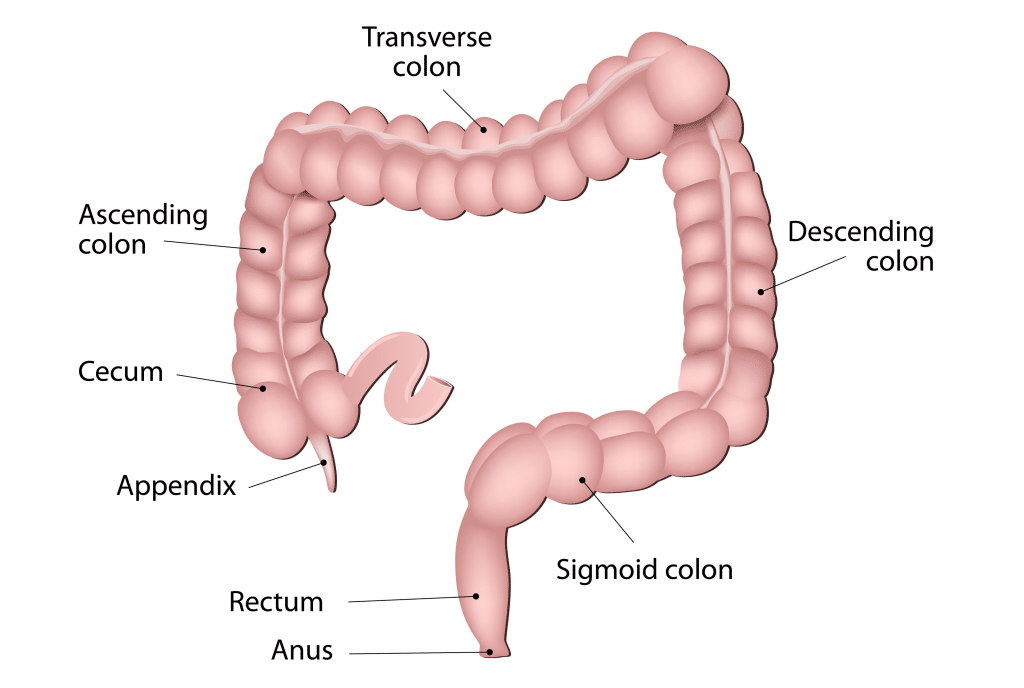
What anatomical structures are involved in colorectal cancers
colon
rectum
anus
What does it mean when we say organs are located intraperitoneally?
anterior
organs are completely covered by visceral peritoneum
organs are freely mobile
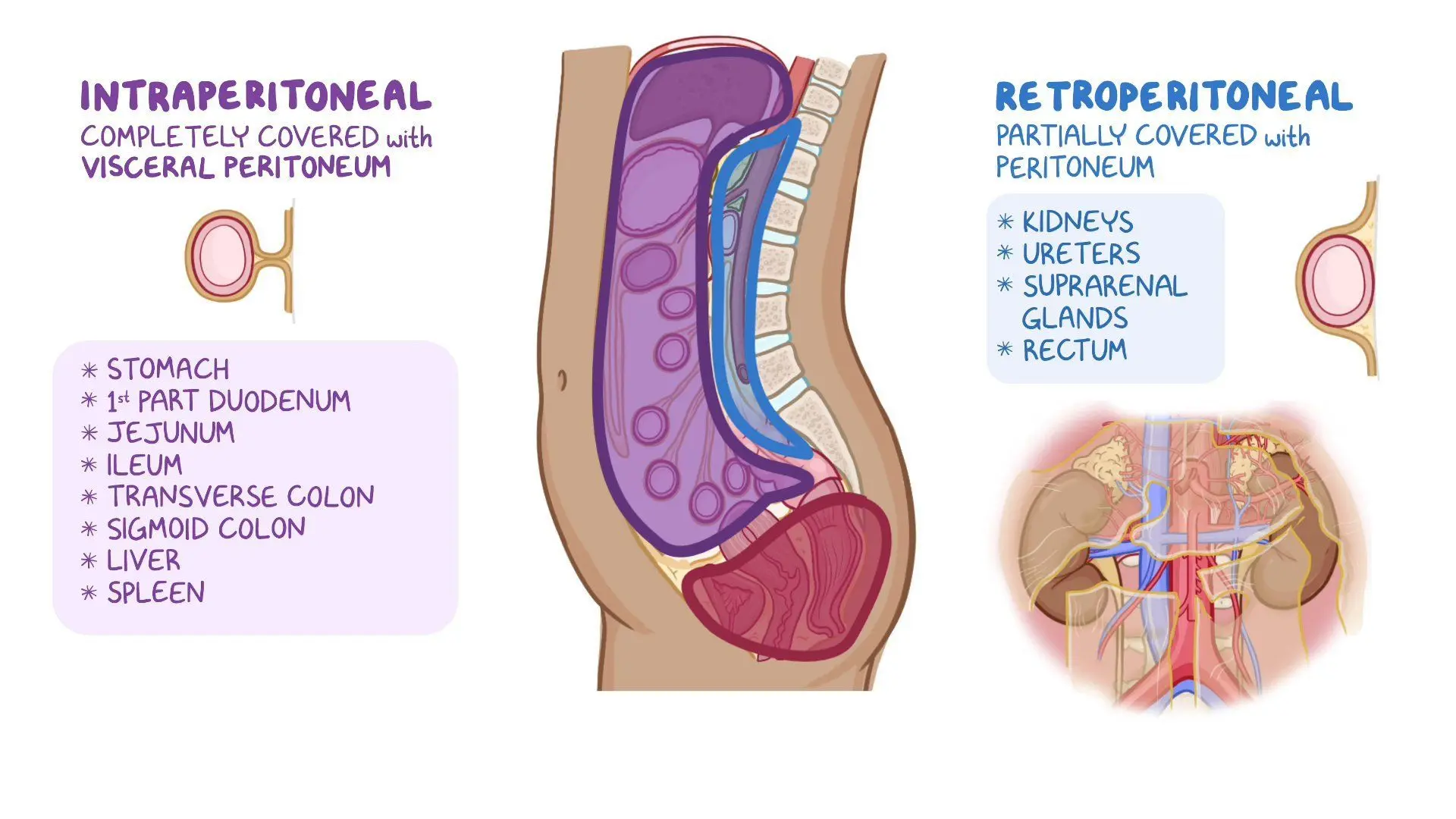
Examples of intraperitoneal organs
transverse colon
sigmoïd colon
stomach
liver
spleen
cecum
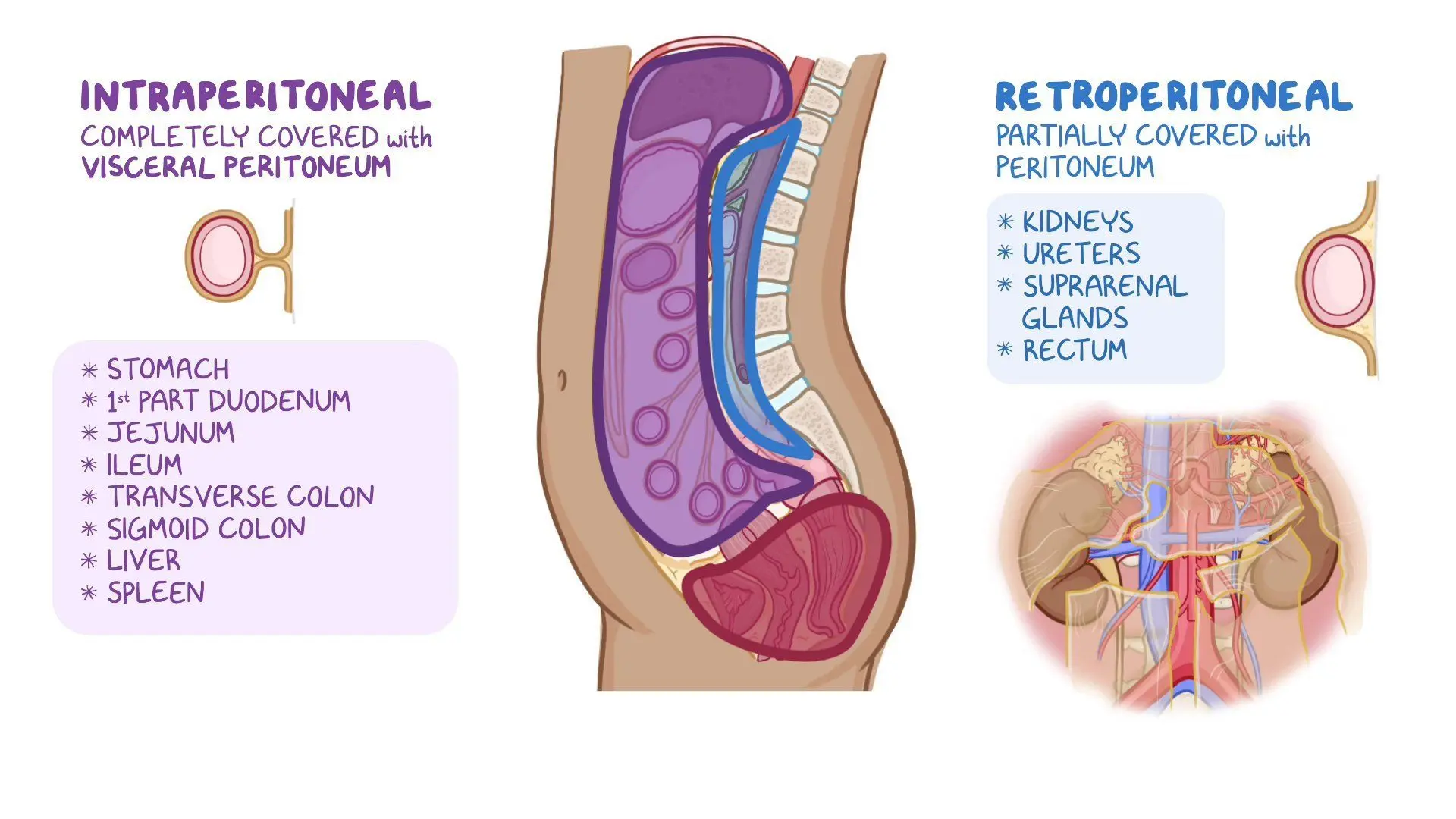
What does it mean when we say organs are located retroperitoneally?
located behind the peritoneum
only covered anteriorly by parietal peritoneum; posterial and lateral lack covering (easier spread)
organs are fixed
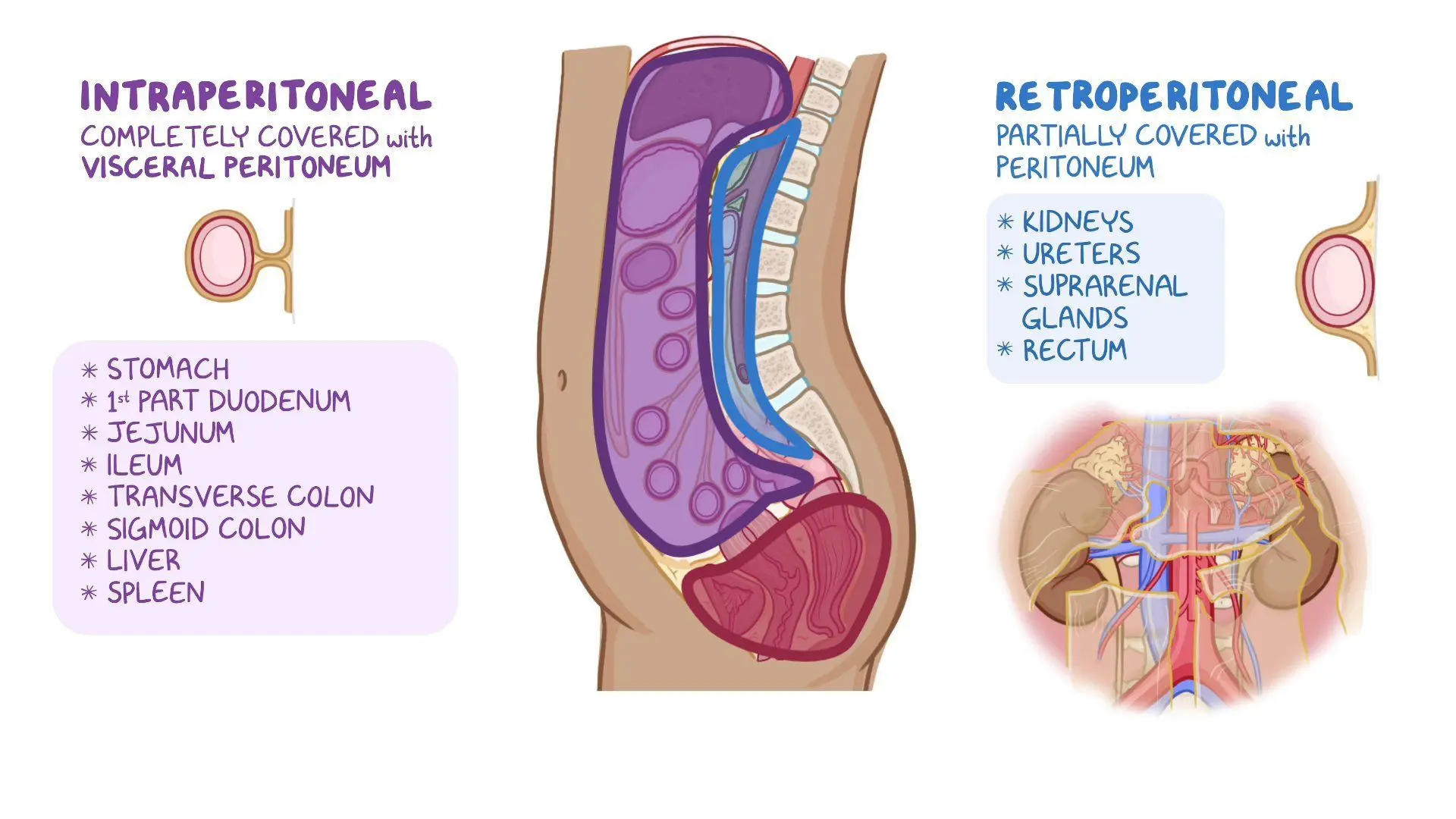
Examples of retroperitoneal organs
ascending/descending colon
hepatic/splenic fixtures
lower half of rectum
What are the 4 layers of the bowel?
Innermost to outermost layer:
Mucosa (innermost)
submucosa
muscularis
serosa (outermost)
What structures are located in the submucosa layer?
It’s a layer of lymphatic and hematologic spread
blood vessels
lymphatics
What is the most common GI malignancy?
Colorectal cancer (best prognosis)
What is the etiology/risk factors of colorectal cancer?
diet high in animal fat (processed/red meat) and low fiber
Hereditary: Family adenomatous polyposis (FAP)
Chronic ulcerative colitis
What are the clinical presentations for colorectal cancer?
hematochezia (rectal bleeding)—1st sign
tenesmus (spasm with desire to empty bowel)
obstructive symptoms
What are the ACS screening recommendations for colorectal cancer?
fecal occult blood test annually
fecal DNA test every 3 years
flex sigmoidoscopy, barium enema, CT colonography-5 years
colonoscopy- 10 years
ACS age recommendation for colorectal cancer
45 years
What is the carcinoembryonic antigen (CEA) tumor marker?
lab studies—the higher the number of CEA proteins present in blood, the more the disease is present
What is the most common pathology/histology for colorectal cancer?
Adenocarcinoma
TNM staging system (previously Duke’s)
What are the routes of spread for colorectal cancers?
rectal-perirectal
colorectal- peritoneal seeding
What is peritoneal seeding?
tumor grows through walls of the bowel onto peritoneal surface of the colon.
Tumor cells shed into abdominal cavity
find their way to other organ surfaces and grow
What are the mets for colorectal cancer?
liver (most common)
lung
Treatment techniques for colorectal cancer
surgery (treatment of choice)- first
Radiation (Pre and Post OP)
What surgeries are done for colorectal cancer?
colon-hemicolectomy
rectal:
Low Anterior Resection (LAR)
Abdominoperineal Resection (APR)
What is a hemicolectomy procedure of the colon?
segment of colon + nodes/blood vessels removed
What is the Low Anterior Resection (LAR) procedure for rectal?
removal of tumor/margin and nodes (upper rectum)
bowel is reanastomosed; no colostomy
What is the Abdominoperineal Resection (APR) procedure for rectal?
lower 1/3rd of rectum and anus removed
colostomy needed
Why is radiation done preoperatively (neoadjuvant) for colorectal cancer?
The goal is to shrink the tumor so that LAR can be done to spare the patient from APR (colostomy)
Why is radiation done postoperatively for colorectal cancer?
Gets rid of microscopic disease and prevents chance of reoccurrence
includes chemo (5-FU continuous infusion—fanny pack)
What are the organs at risk for colorectal cancer?
small bowel
liver
kidney
femoral heads
colon
TD 5/5 for small bowel
40 Gy (4000 cGy)
TD 5/5 for Colon
45 Gy (4500 cGy)
TD 5/5 for femoral heads
52 Gy (5200 cGy)
What is intraoperative radiation therapy (IORT)?
A concentrated dose of radiation is delivered directly to a tumor bed or area at high risk for recurrence during surgery, immediately after the tumor is removed.
a boost/supplement to external beam radiation therapy
Acute side effects of colorectal cancer
enterits (small bowel inflammation)
diarrhea
abd cramps
bloating
proctitis (rectal inflammation)
bloody/mucosal discharge
dysuria (painful urination)
decreased blood count
most desquamation in perineum
chronic side effects of colorectal cancer
bladder atrophy
fistula
persistent diarrhea
chronic enteritis
obstruction of small bowel
Management of side effects of colorectal cancer
sitz baths (inflammation relief for skin irritation)
Domeboro soak (inflammation relief for skin irritation)
Low-residue diet
Anti-diarrheal meds (Imodium, Lomotil)
Lymph nolvement for anal cancer
inguinal
Etiology for anal cancer
Human papillomavirus (HPV)-16
genital warts
Clinical presentation for anal cancer
bright red rectal bleeding
Most common pathology for anal cancer
squamous cell carcinoma
Organs at risk for anal cancer
small bowel
femoral heads
bladder
TD 5/5 for bladder
65 Gy (6500 cGy)
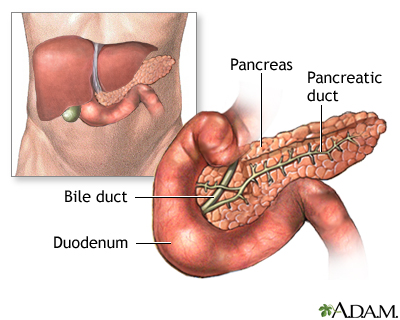
What is the anatomy of the pancreas?
head (in duodenum)
body
tail
What is one of the deadliest malignancies?
Pancreatic cancers, have high mortality rate
found in advanced stages—poor prognosis
Clinical presentations of pancreatic cancers?
abdominal pain
anorexia
weight loss
jaundice
Most common pathology for pancreatic cancers?
Adenocarcinoma
Is surgical removal an option for pancreatic cancers?
No, due to the location of the ,pancreas near critical structures
What surgical procedure can be done for pancreatic cancers?
Whipple procedure = pancreaticoduodenectomy
What structures are removed during a Whipple procedure?
head of pancreas
entire duodenum
distal stomach
gallbladder
common bile duct
What is the most common chemotherapy agent used for pancreatic cancers?
Gemcitabine
Acute side effects of pancreatic cancer
nausea and vomiting
decreases blood count, diarrhea
What is the common chemo agent for digestive cacners
5- FU
TD 5/5 for rectum
60 Gy (6000 cGy)
What helps to displace small bowel out treatment field for the pelvic irradiation?
having a full bladder
belly board
What does the ileum of the small intestine connect to?
cecum of the colon (ileocecal junction)