PDA III - Exam 2: Anticonvulsants and Circuits RW
1/126
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
127 Terms
What is epilepsy defined as?
CNS disease characterized by recurrent seizures
Chronic, periodic, and unpredictable seizure conditions
May or may not involve convulsions
What are seizures?
Abnormal (excessive) neuronal activity
Either due to excessive excitation or deficient inhibition
Usually self-limiting (run out of energy)
What are the 3 main descriptors of seizure activity?
Disordered
Synchronous
Rhytmic
What are the two main classifications of seizures?
Generalized
Focal
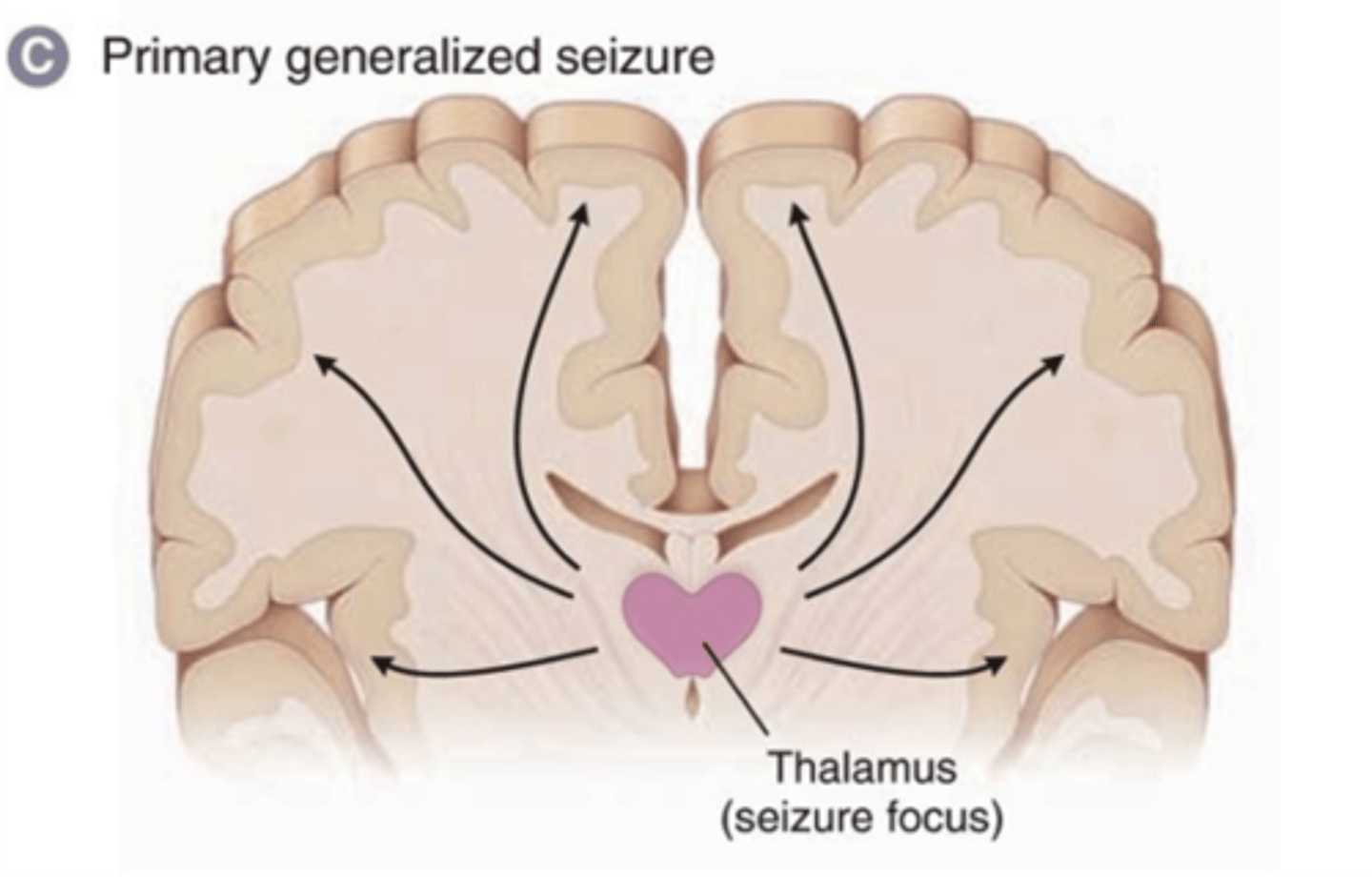
What are generalized seizures?
Affect both hemispheres
Cause loss of consciousness
How do generalized seizures affect both hemispheres?
Seizure focus (start) is in the thalamus
Thalamus connects the two hemispheres
Spreads to both sides
What are the types of generalized seizures?
Tonic-clonic (Grand Mal)
Absence (Petit Mal)
Myoclonic
Atonic
What are characteristics of Tonic-clonic (Grand Mal) seizures?
Generalized seizure
Max involvement of both hemispheres
Starts with rigid phase (tonic)
Followed by jerking of limbs (clonic)
Each phase lasting <1min
Ends with post-ictal state
What is described by the "post-ictal state" of Tonic-clonic (Grand Mal) seizures?
Last phase of seizure
Lasts 15-30 mins
Pt. is either asleep or confused/disoriented
Pt. has no recollection of seizure
What are characteristics of Absence (Petit Mal) seizures?
Generalized seizure
Mainly occurs in childhood
(dx. often missed, assume child is distracted)
Abrupt interruption in consciousness
Pt. has blank stare straight ahead
Sometimes may see lip smacking or rapid blinking
Lasts 15-20 seconds
Can happen >100x/day
What are characteristics of Myoclonic seizures?
Generalized seizure
Brief (about 1 second)
Occurs very quickly
Rapid jerking of the arms
Often mistaken for nervousness/clumsiness
What are characteristics of Atonic seizures?
Generalized seizure
Sudden loss of muscle tone
Pt. appears to pass out
May require pt. to wear a helmet (due to fall risk)
What are focal (partial) seizures?
Only involve 1 hemisphere
Seizure focus is only 1 area of the brain
Spread limited to the hemisphere it started in
(can progress to generalized)
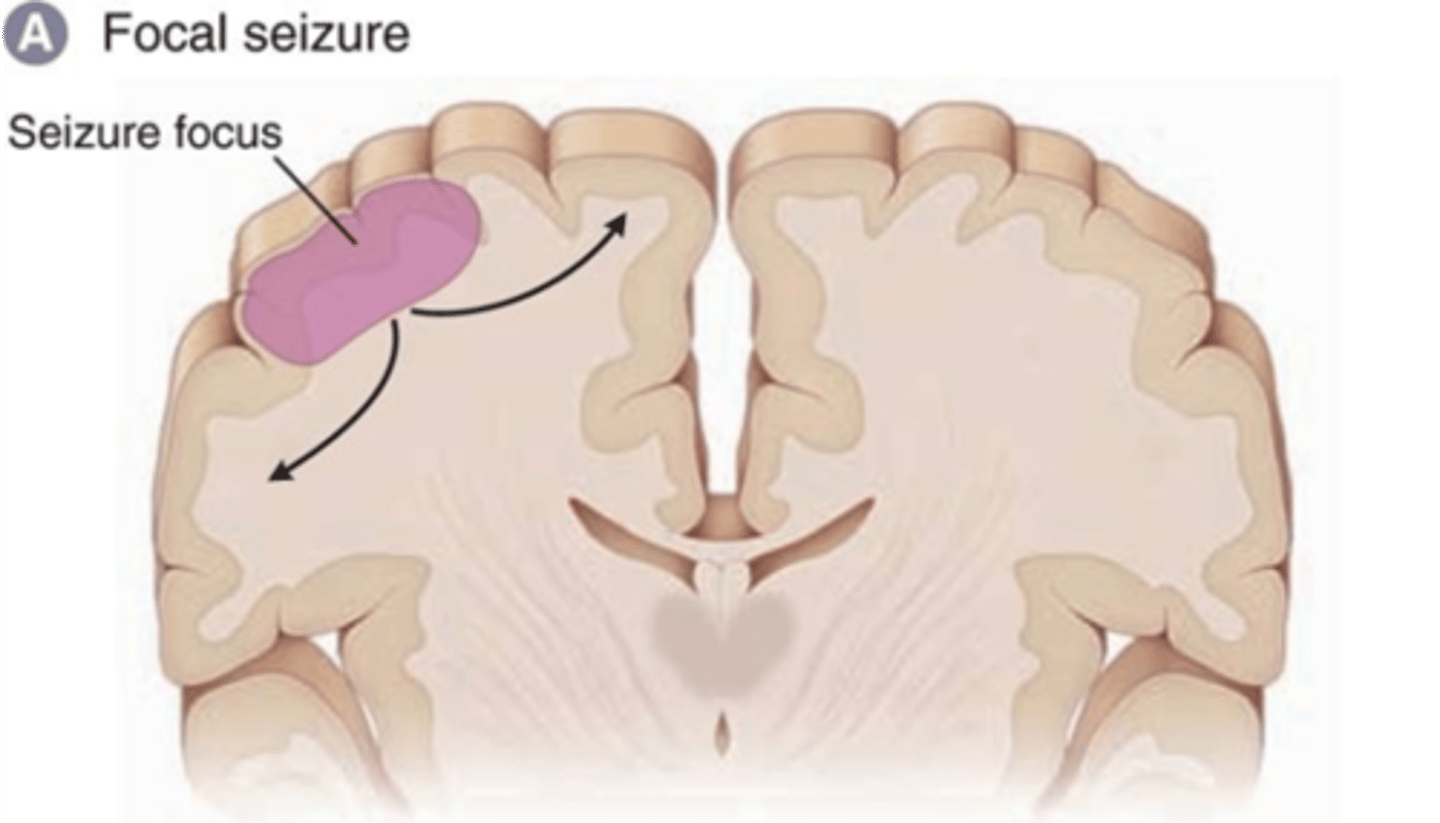
What do focal (partial) seizures normally indicate?
Often due to presence of a brain lesion
Lesion due to injury, stroke, tumor, etc.
What are types of focal (partial) seizures?
w/o altered mental awareness
w/ altered mental awareness
w/ secondary generalization
What are characteristics of focal seizures without altered mental awareness?
Confined to area of brain that serves basic function
(ex. motor or sensation)
No loss of consciousness (preserved)
Symptoms depend on location
Can spread ipsilaterally (on same side)
What symptoms would be present if a focal seizures without altered mental awareness affected an area serving motor control?
Motor involvement usually confined to clonic (jerking)
Of one arm or leg
What symptoms would be present if a focal seizures without altered mental awareness affected an area serving sensation?
Sensory involvement includes:
Smelling/tasting something foul
Visual disturbances
Numbness in arm or leg
What are characteristics of focal seizures with altered mental awareness?
Seizure involves brain region that serves a complex fxn
(hippocampus, frontal lobe)
Consciousness is impaired
Usually preceded by an aura
What symptoms are seen during focal seizures with altered mental awareness, due to impaired consciousness?
Pt. has coordinated, involuntary movements
But, is unable to communicate or understand
What is the main difference between focal seizures w/ or w/o altered mental awareness?
W/ altered mental awareness causes loss of consciousness,
W/O does not
What complex functions can be affected by focal seizures with altered mental awareness?
Language, memory, and emotions
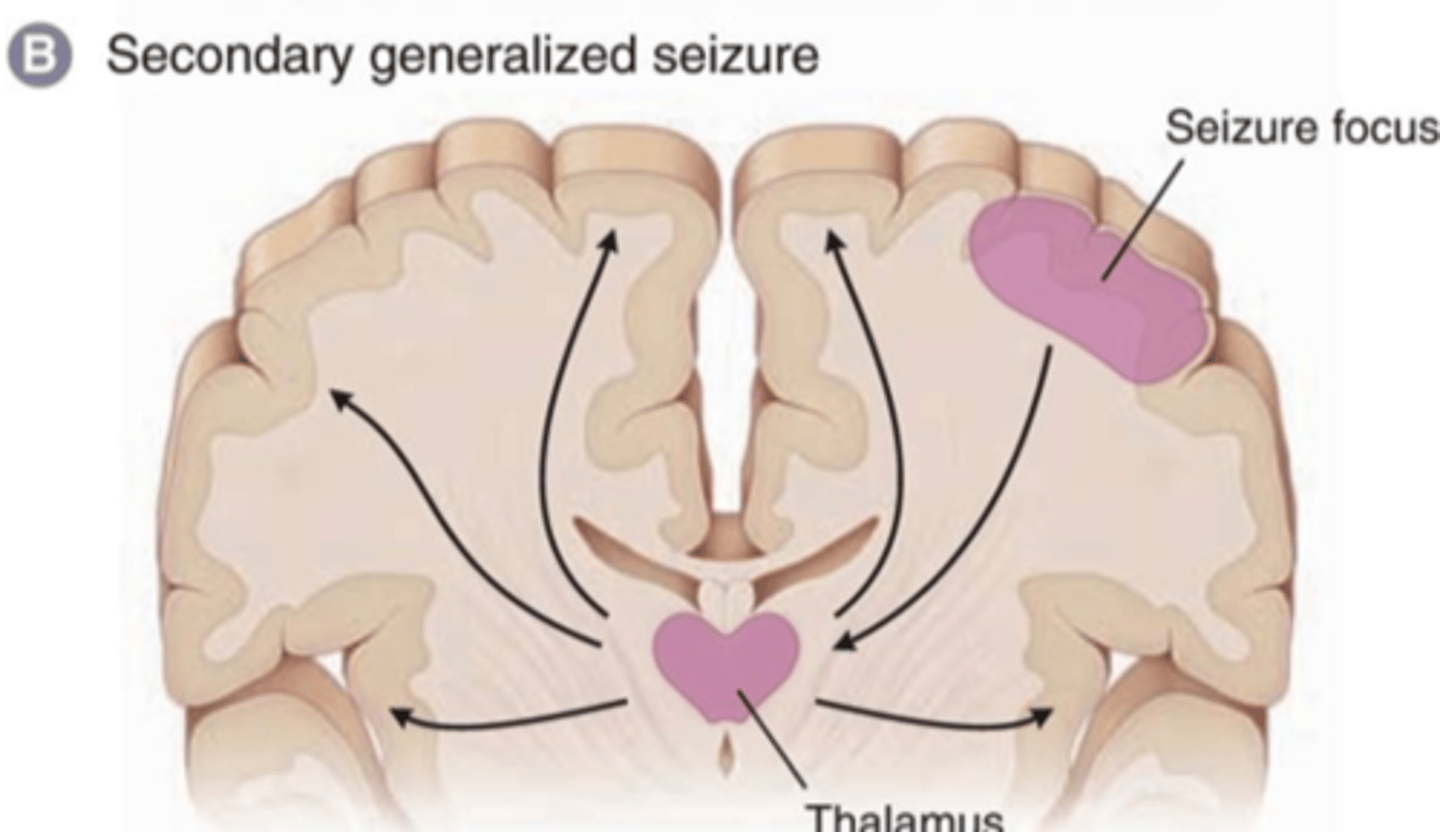
What are characteristics of focal seizures with secondary generalization?
Seizure starts of as focal
Evolves into a tonic-clonic (Grand Mal) seizure
How do focal seizures with secondary generalization spread into the 2nd hemisphere?
Start in only 1 hemisphere
Seizure activity reaches the Thalamus
Thalamus connects the hemispheres
Seizure spreads to the second hemisphere
What are the 3 steps of focal seizures?
Initiation
Synchronization
Spread
What is described by the initiation step of focal seizures?
Initiation of inc. electrical activity at the cellular level
What is described by the synchronization step of focal seizures?
Synchronization of electrical activity of surrounding neurons
What is described by the spread step of focal seizures?
Spread of electrical activity to adjacent regions
If spreads to the second hemisphere it becomes generalized
What is the theory of why focal seizure develop?
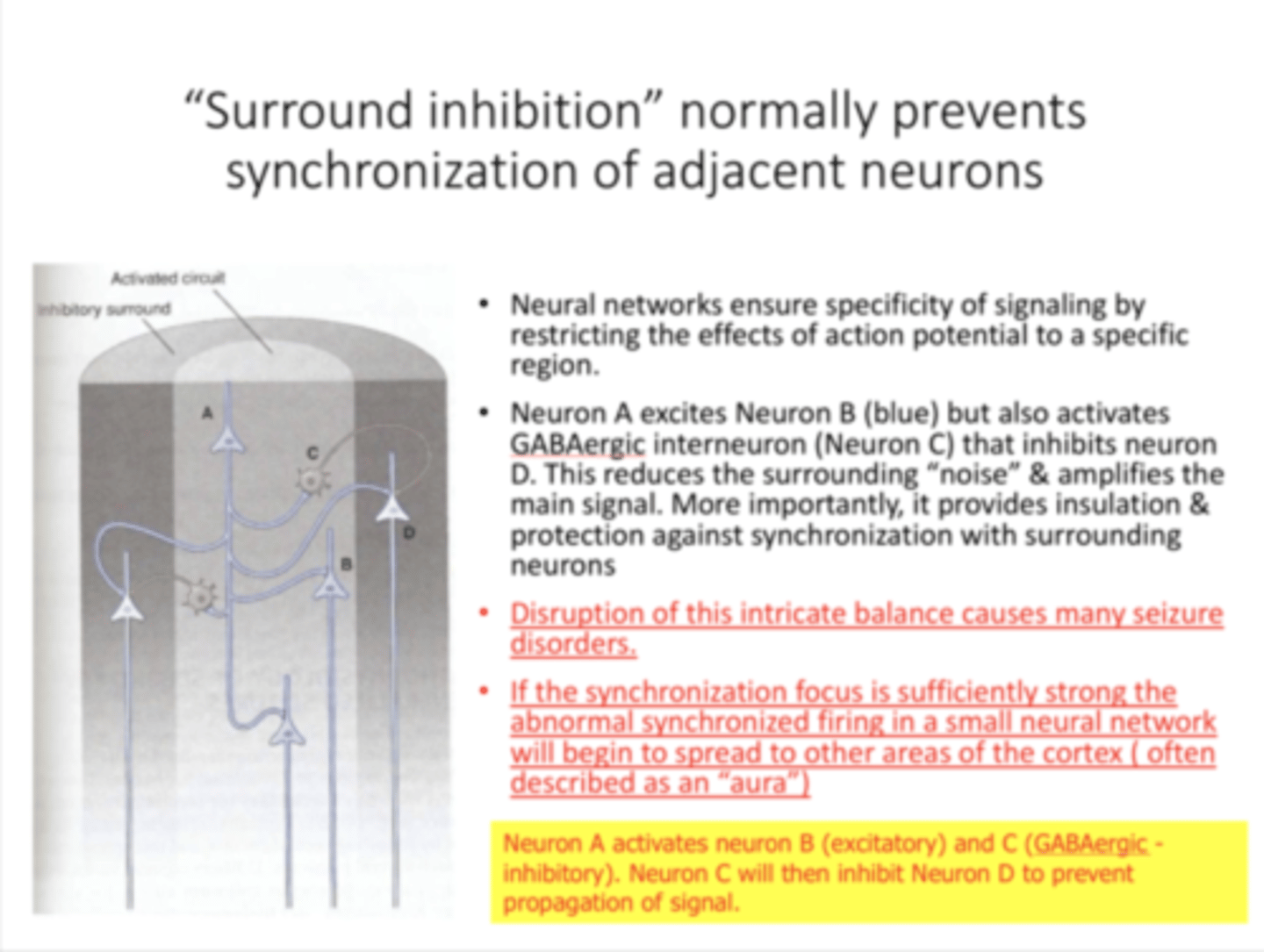
Many focal seizure most likely result from a failure of surround inhibition
What are possible causes of failure of sorround inhibition?
Infections, tumors, genetic variation
What is sorround inhibition?
Mech. in the brain to prevent synchronicity in surrounding areas
Preventing over-excitation, and therefore preventing seizures
Where is surround inhibition occuring?
Cerebral cortex
What is described by the inhibitory surround?
Area that is inhibited when cortical pyramidal neurons are activated
Inhibition prevents spread of over-excitation
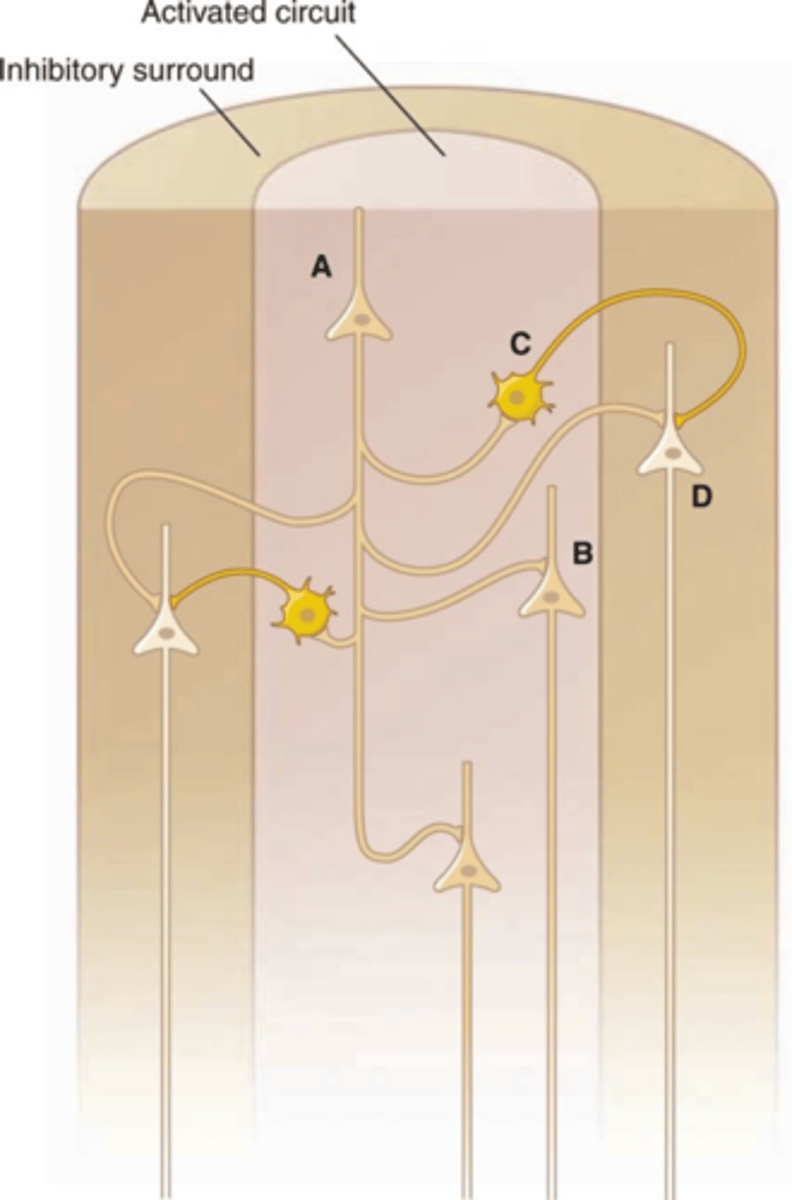
What are cortical pyramidal neurons, as part of surround inhibition?
Glutamatergic neurons
Excitatory function
Located in the cerebral cortex
Part of surround inhibition circuit
Neurons A, B and D on the diagram
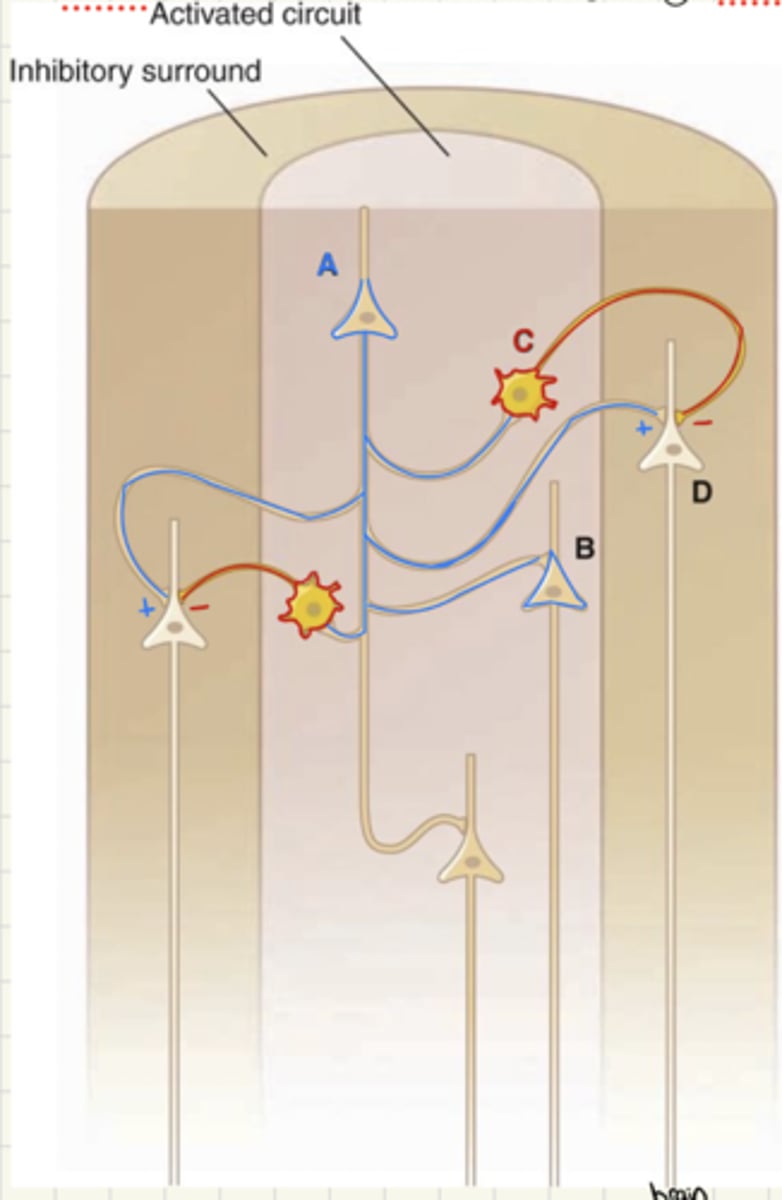
What are interneurons, as part of surround inhibition?
Mainly GABAergic
Inhibitory function
Located in the cerebral cortex
Part of surround inhibition circuit
Neurons C on the diagram
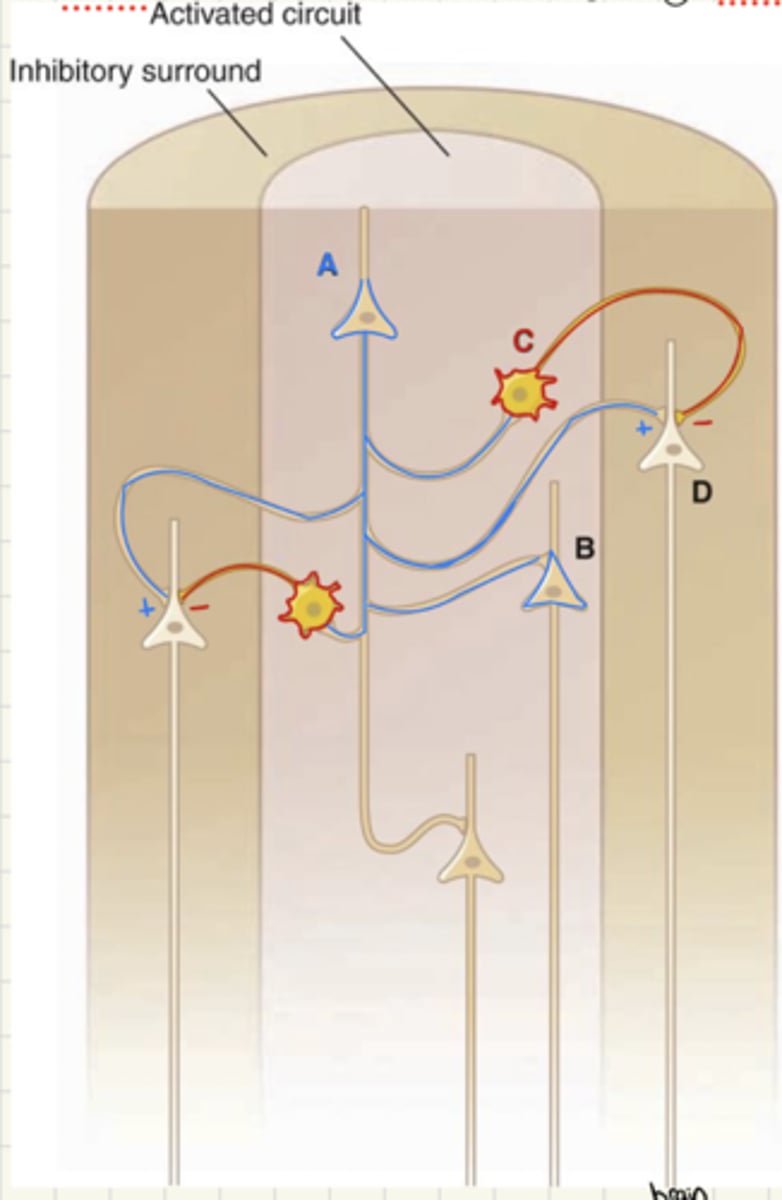
What is the first step in surround inhibition?
Some brain function excites cortical pyramidal neuron A
Once the cortical pyramidal neuron A is excited, what is the next step in surround inhibition?
Excited neuron A fires and AP
AP cause release of Glu
Glu causes excitation of connected neurons
What neurons are excited by the cortical pyramidal neuron A during surround inhibition?
A excites B and C
B is a cortical pyramidal neuron (excitatory)
C is a GABAergic interneuron (inhibitory)
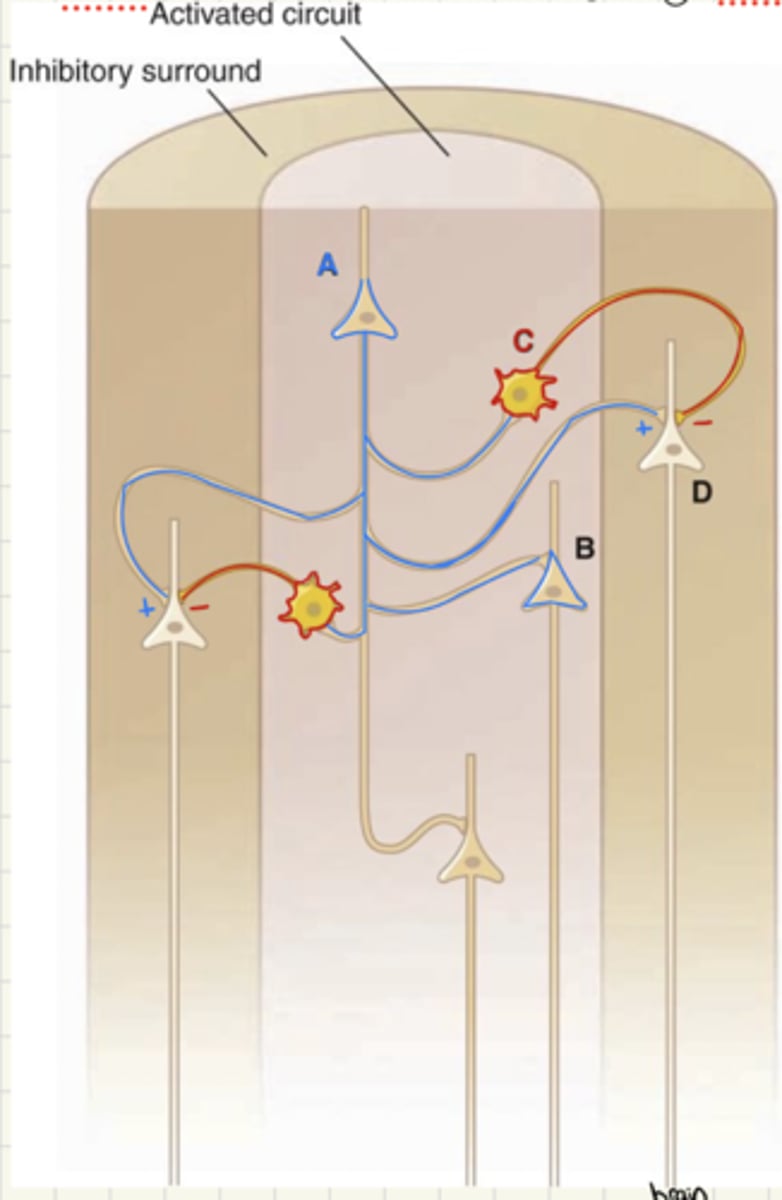
When the GABAergic interneuron, C, is excited by the cortical pyramidal neuron, A, what is the resulting effect?
Prevents neurons connected to C from becoming excited
Stopping "synchronization" with connected neurons
D is not excited despite being connected to A, because it is also connected to C
("excitation leading to inhibition")
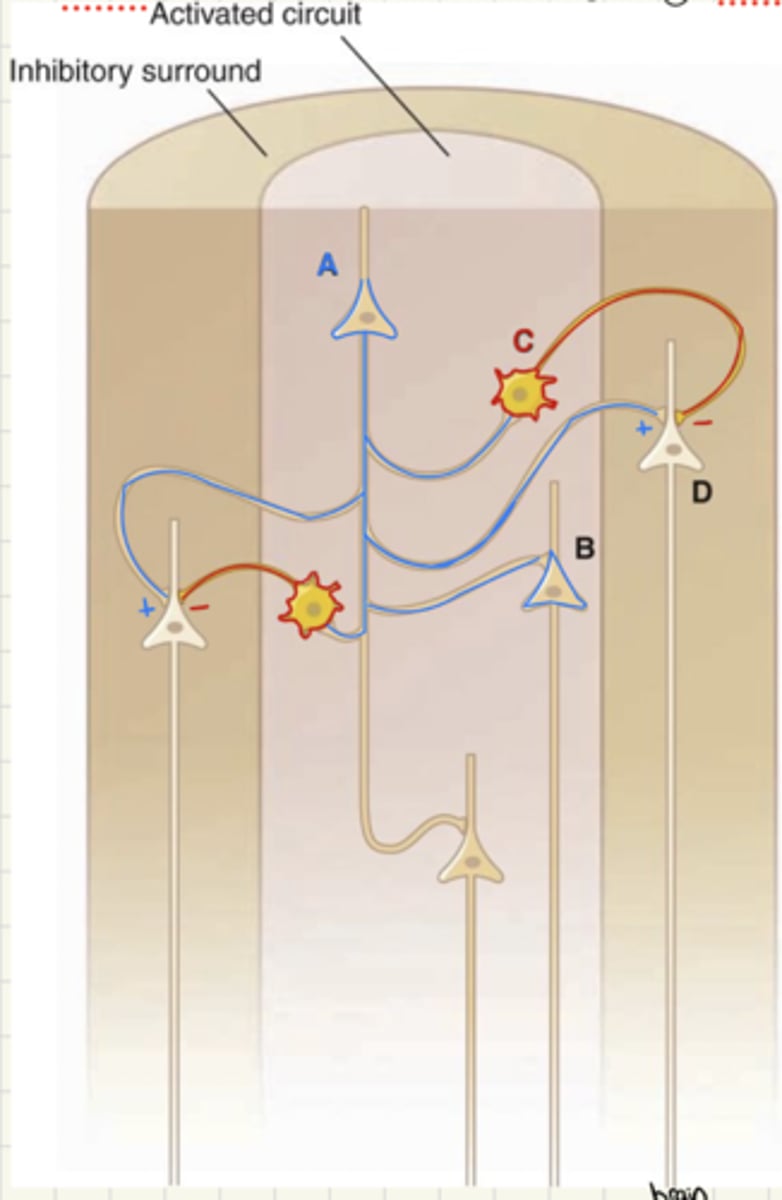
Summary of surround inhibition for reference:
How is signal transmission characterized while awake?
During awake phase neuron is in transmission mode
Signals transmitted as single spikes
Small, desynchronized, low voltage waves
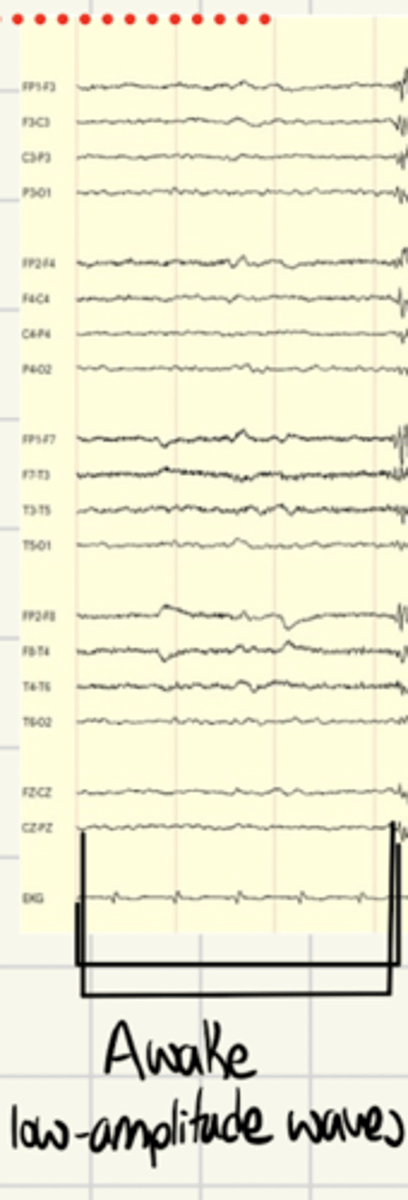
How is signal transmission characterized while in slow wave sleep?
During slow wave sleep there is a burst mode
Large waves in a rhythm
Results in oscillations that cancel out stimuli
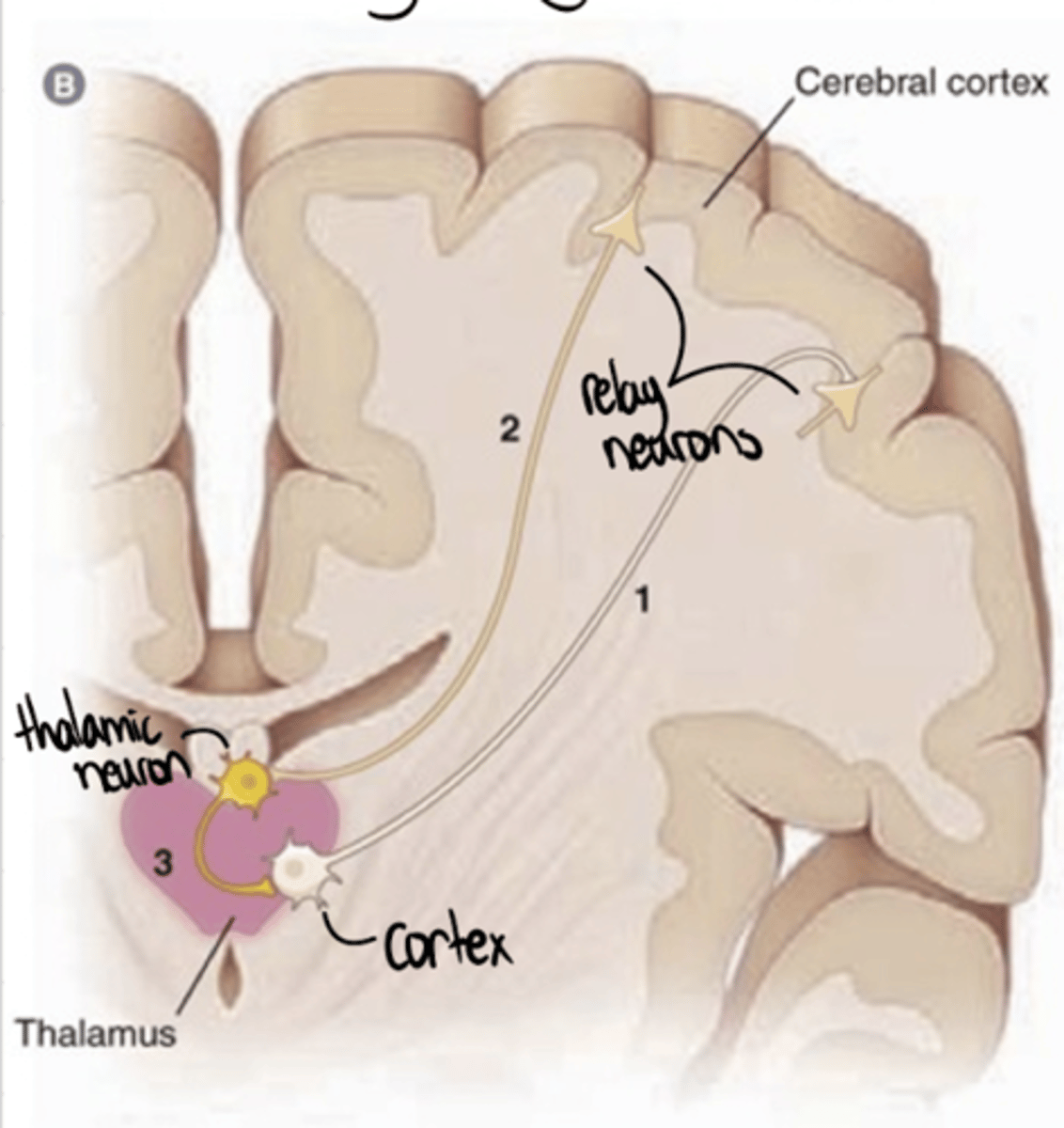
What do absence seizure EEG readings mimic?
Absence seizures produce "sleep like" waves
Large waves of electrical activity for 15-20 secs
Preventing stimuli from having an effect
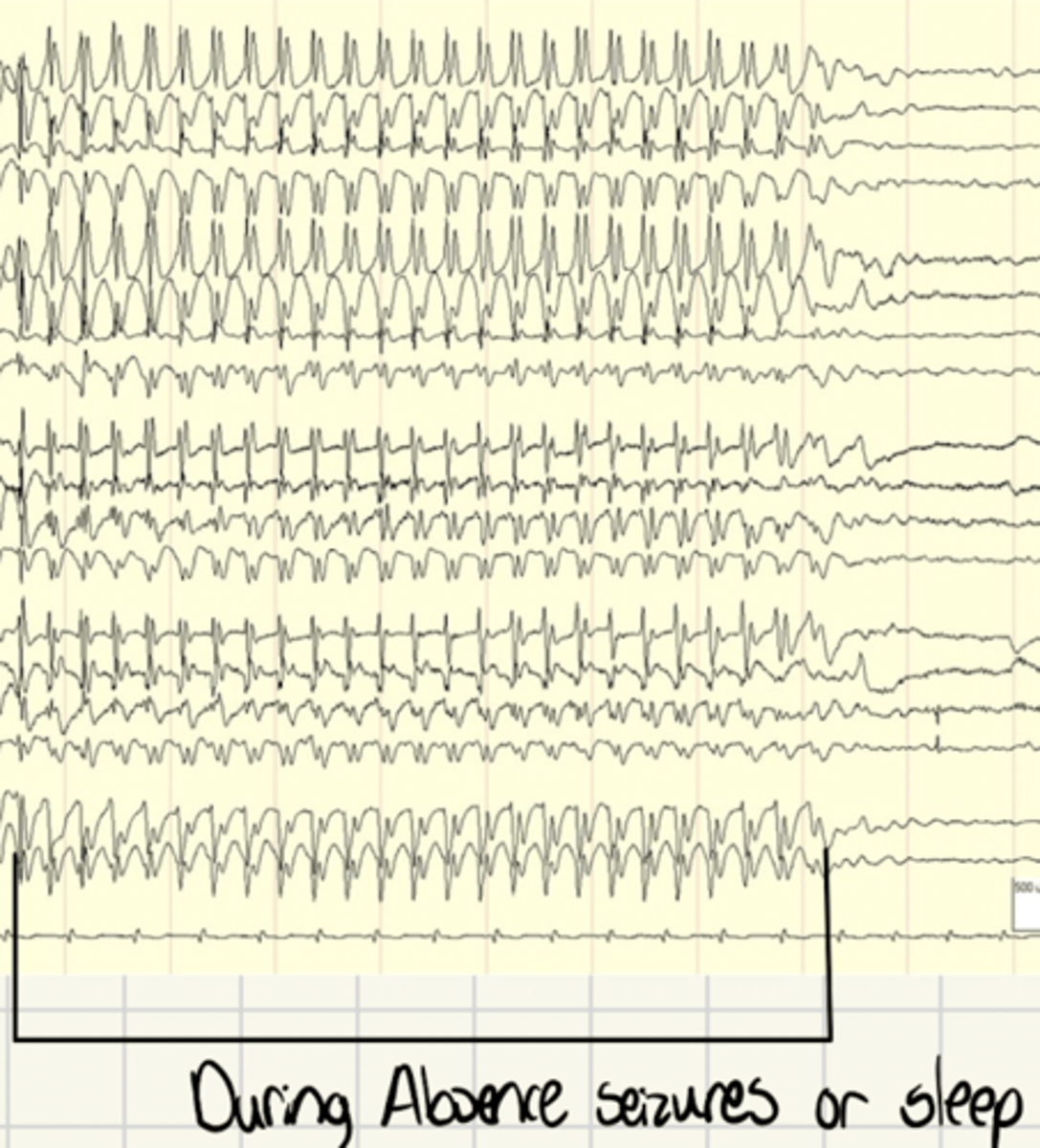
What is the mechanism of Absence seizures?
Thalamocortical-Cortical symphony
Leading to oscillatory, synchronized, pattern of excitation
What is the Thalamocortical-Cortical symphony?
Oscillations of activity between the thalamus and cortex
What is the first step in the Thalamocortical-Cortical symphony?
Hyperpolarization of relay neurons
What are the thalamocortical-cortical relay neurons?
Glutamatergic (excitatory) neurons
Cell body in thalamus
Axon in cortexv
Once relay neurons are hyperpolarized, what is the next step in the Thalamocortical-Cortical symphony?
Hyperpolarization opens T-type Ca channels
Causing burst of activity of T-type Ca channels
(Ca influx)
What are T-type Ca channels?
Voltage-gated Ca channels
Opened by hyperpolarization
What occurs as a result of T-type channel activity, in the Thalamocortical-Cortical symphony?
Ca influx causes depolarization, leading to an AP
Results in synchronous depolarization in the cortex
(seen as spike and wave pattern on ECG)
What occurs as a result of synchronous depolarization in the cortex, in the Thalamocortical-Cortical symphony?
Excitatory input from the cortex
(Glu neurons located in the cortex)
Activates thalamic neurons
What are thalamic neurons?
GABAergic (inhibitory) neurons
Located in thalamus
Release GABA back to the cortex onto relay (thalamocortical) neurons
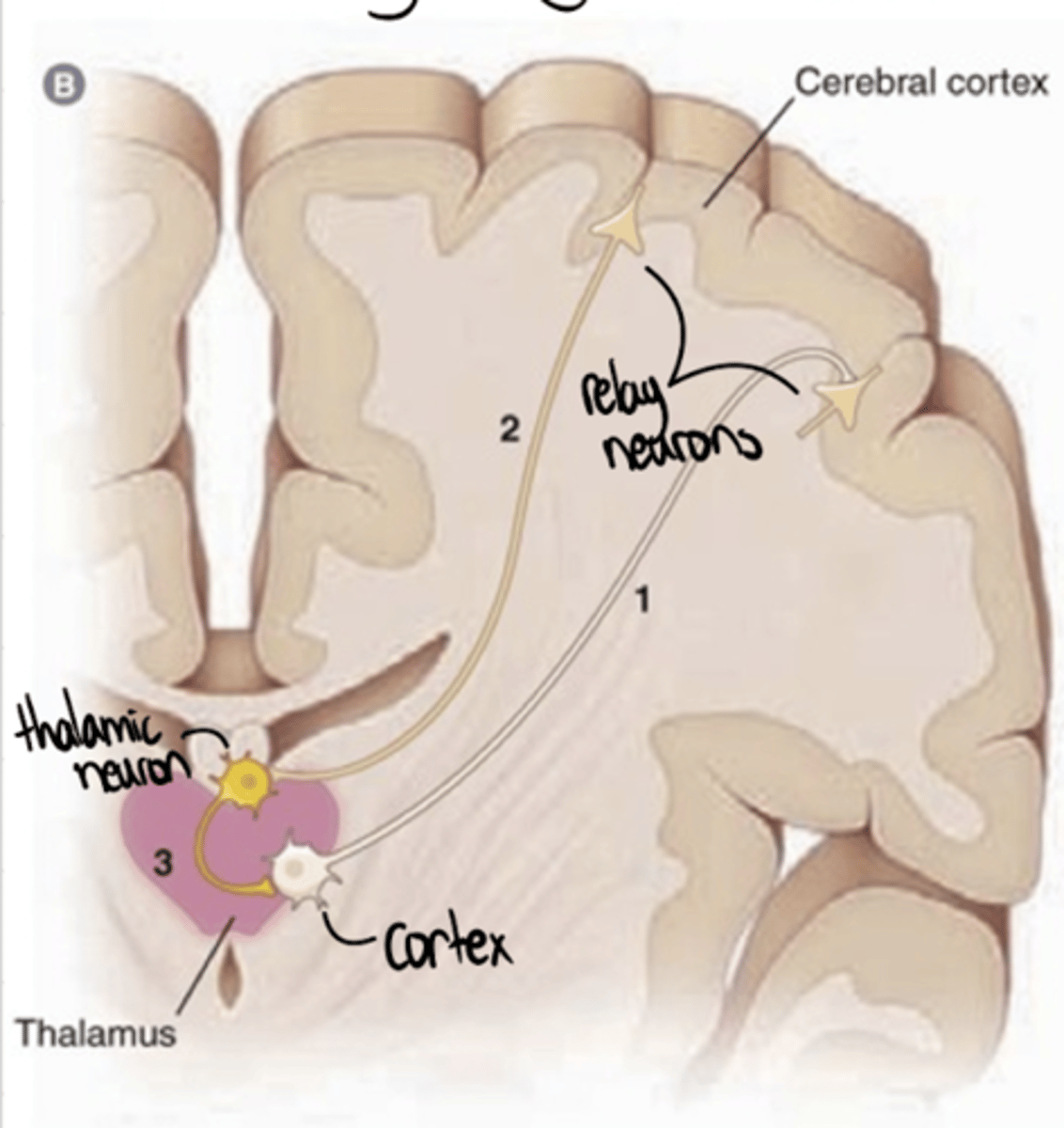
After thalamic (GABA) neurons are activated, what is the next step in the Thalamocortical-Cortical symphony?
GABAergic thalamic neurons release GABA onto relay (thalamocortical neurons)
Cause hyperpolarization of relay neurons
After relay (thalamocortical) neurons are hyperpolarized, what happens in the Thalamocortical-Cortical symphony?
Cycle is reinitiated
T-type Ca channels on thalamocortical neurons are excited by hyperpolarization
Hyperpolarization of T-type Ca channels causes another depolarization, leading to continuation of the cycle
Why is GABA, the major inhibitory NT, able to cause excitation in the Thalamocortical-Cortical symphony?
Causes hyperpolarization of T-type Ca channels
But, T-type Ca channels are excited by this hyperpolarization
Leading to further excitation downstream
What is the major therapeutic target for Absence seizures?
T-type Ca channels
Why is blocking T-type Ca channels helpful in absence seizures?
Blocking ability to be hyperpolarized (activated)
Therefore, won't depolarize and stimulate cortical neurons
"Breaking" the cycle
What drugs are used for absence seizures?
Ethosuximide (only used in absence seizures)
Valproic acid (Valproate)
Lamotrigine
Clonazepam
What drug is 1st line for absence seizures?
Ethosuximide
Only used in absence seizures
What drug is 2nd line for absence seizures?
Valproic acid (valproate)
What drug is 3rd line for absence seizures?
Lamotrigine
What drug is 4th line for absence seizures?
Clonazepam
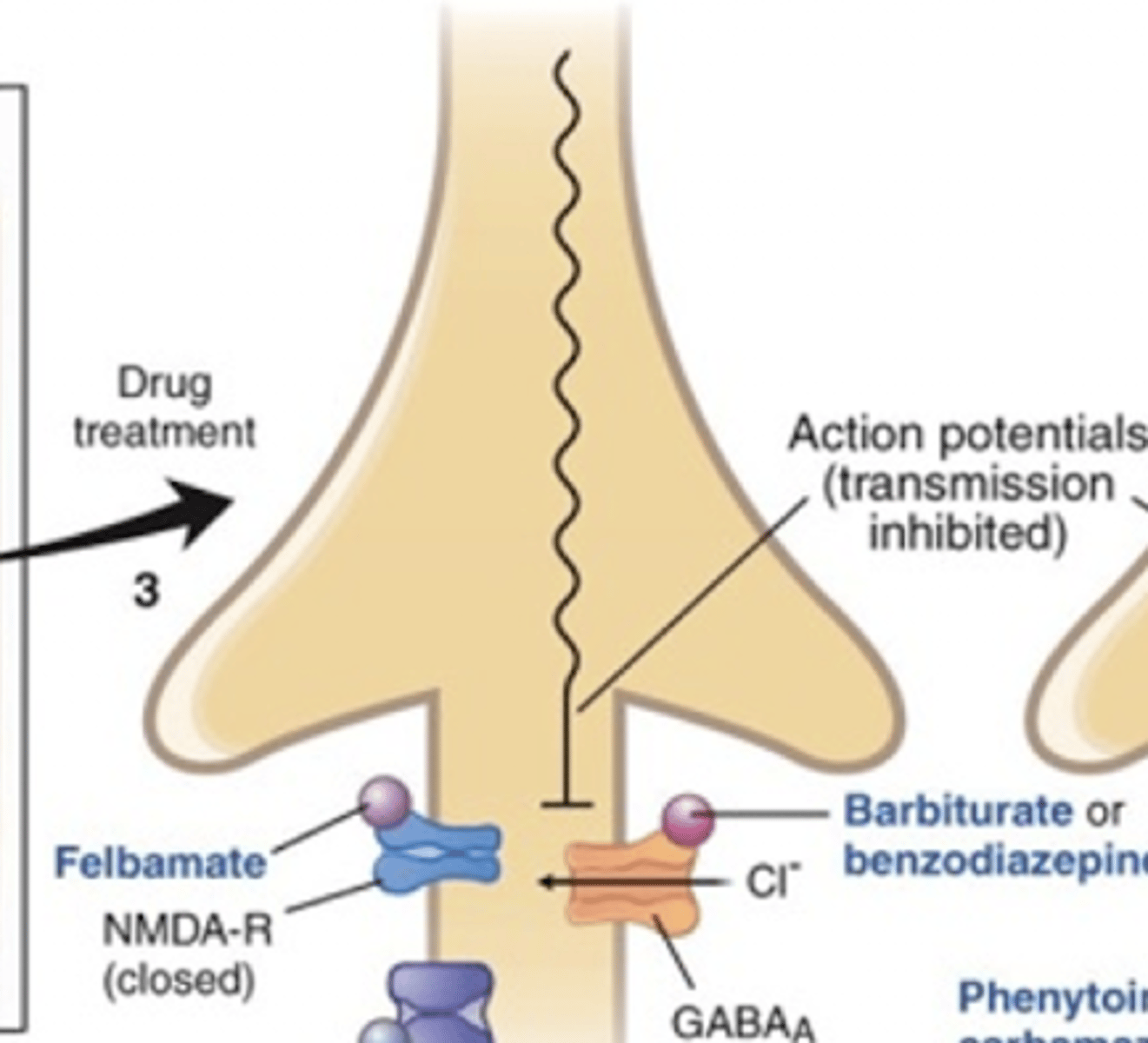
What is the therapeutic problem in seizures drugs try to adress?
Excessive neuronal activity
Either due to too much excitation or too little inhibition
What are the proposed solutions to the excess neuronal activity therapeutic problem in seizures?
Dec. excitatory transmission in the brain
OR
Inc. inhibitory transmission in the brain
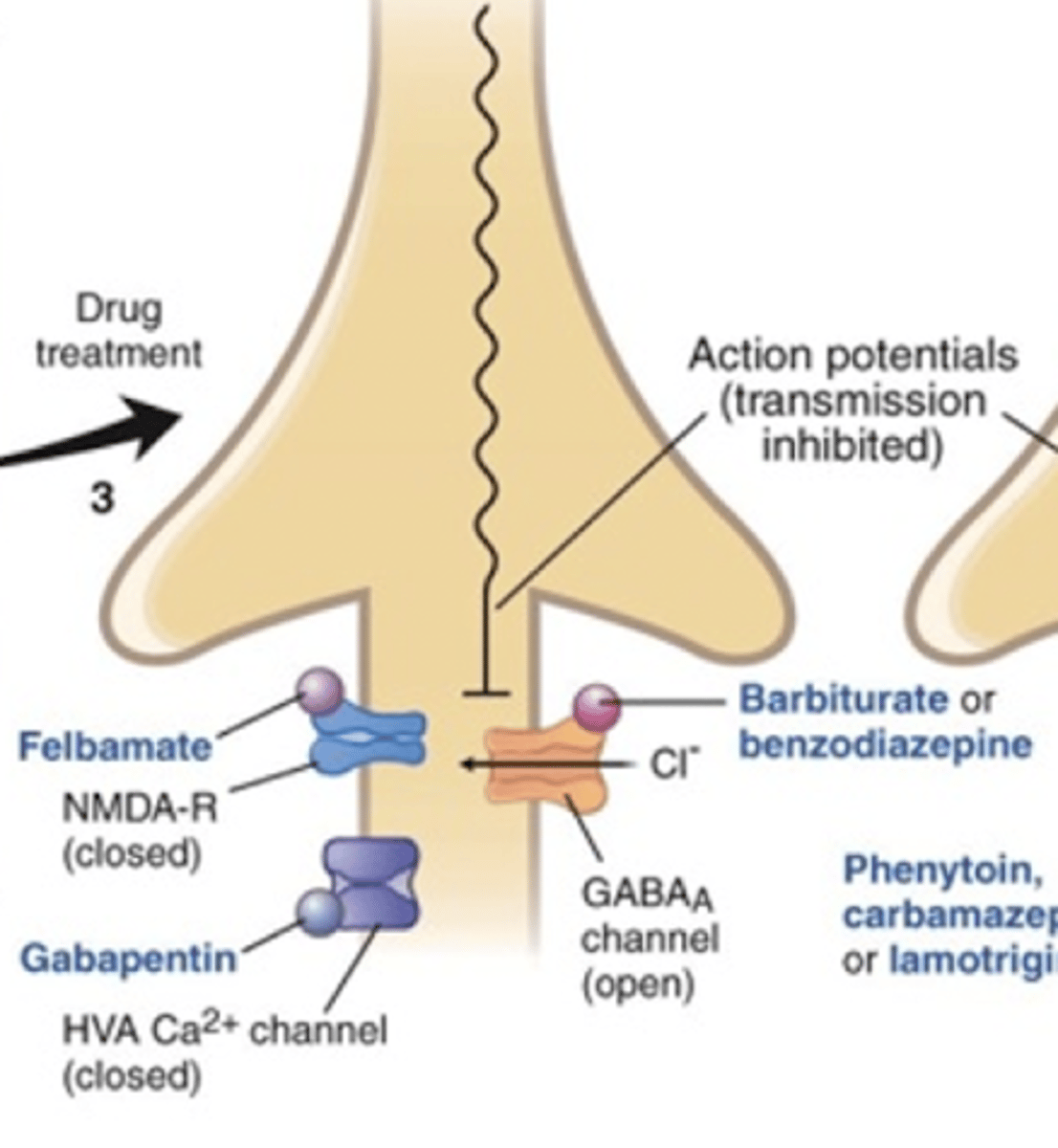
What are the 5 MOA's of anticonvulsants?
Prolong inactive conformation of voltage-gated Na channels
Inc. GABA activity
Block T-type Ca channels (only for absence)
Enhance K channels, inc. inhibition
(no drug examples)
Inhibit Glu activity
How does prolonging the inactive conformation of voltage-gated Na channels treat seizures?
Limits repetitive firing of neurons
Decreasing excitatory transmission
(inhibition of AP propagation)
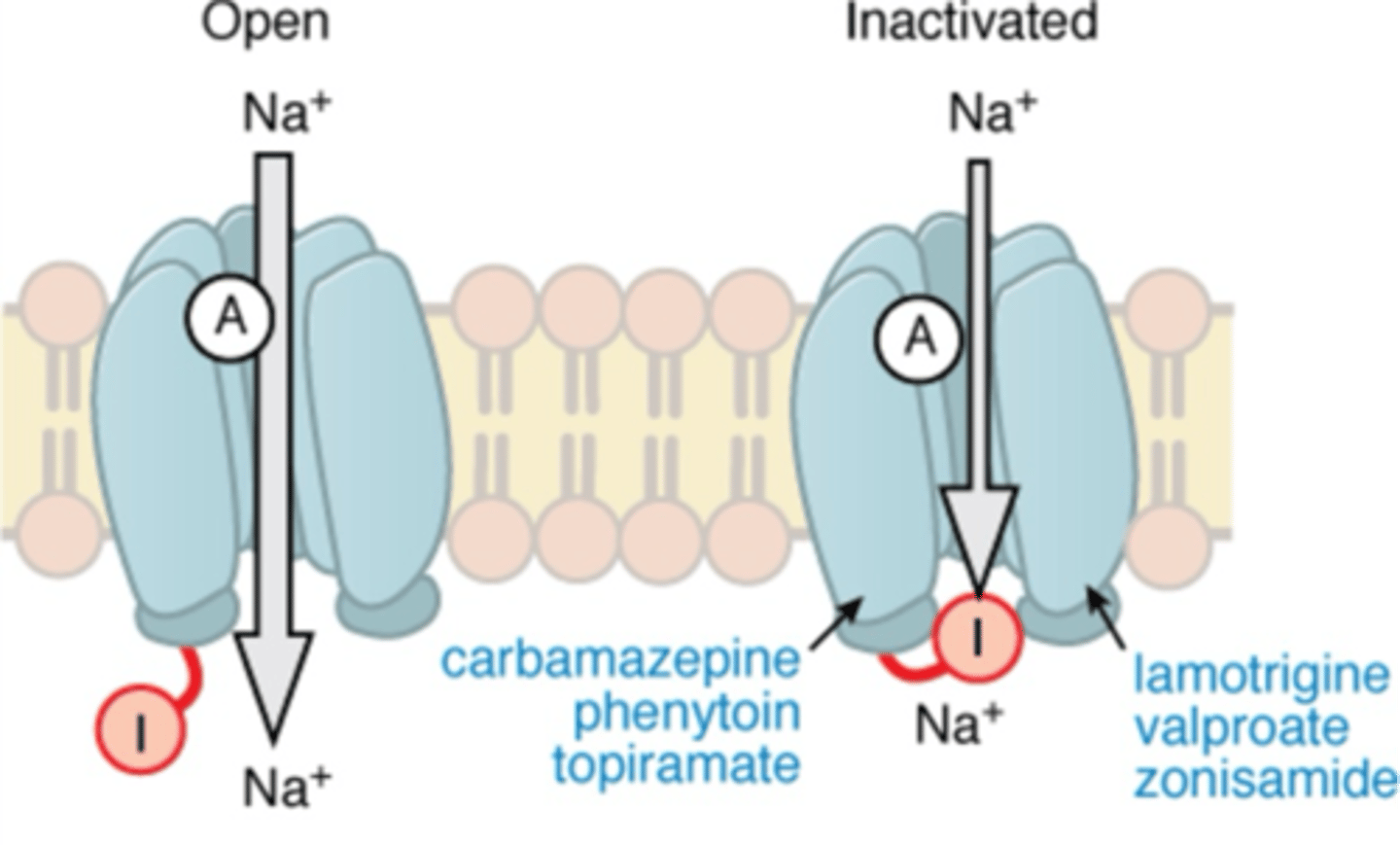
What anticonvulsants work by prolonging the inactive conformation of voltage-gated Na channels?
Carbamazepine
Phenytoin
Topiramate
Lamotrigine
Valproic acid (Valproate)
Zonisamide
What is the MOA of Carbamazepine?
Na channel blocker
Binds and stabilizes fast voltage-gated Na channels
High affinity for refractory (inactive) conformation
Prolongs inactive conformation
Inhibiting propagation of APs
Leading to dec. AP freq.
What is the MOA of Phenytoin?
Na channel blocker
Binds and stabilizes fast voltage-gated Na channels
High affinity for refractory (inactive) conformation
Prolongs inactive conformation
Inhibiting propagation of APs
Leading to dec. AP freq.
What is the MOA of Topiramate?
Na channel blocker
Binds and stabilizes fast voltage-gated Na channels
High affinity for refractory (inactive) conformation
Prolongs inactive conformation
Inhibiting propagation of APs
Leading to dec. AP freq.
What is the MOA of Lamotrigine?
Na channel blocker
Binds and stabilizes fast voltage-gated Na channels
High affinity for refractory (inactive) conformation
Prolongs inactive conformation
Inhibiting propagation of APs
Leading to dec. AP freq.
What is the MOA of Zonisamide?
Na channel blocker
Binds and stabilizes fast voltage-gated Na channels
High affinity for refractory (inactive) conformation
Prolongs inactive conformation
Inhibiting propagation of APs
Leading to dec. AP freq.
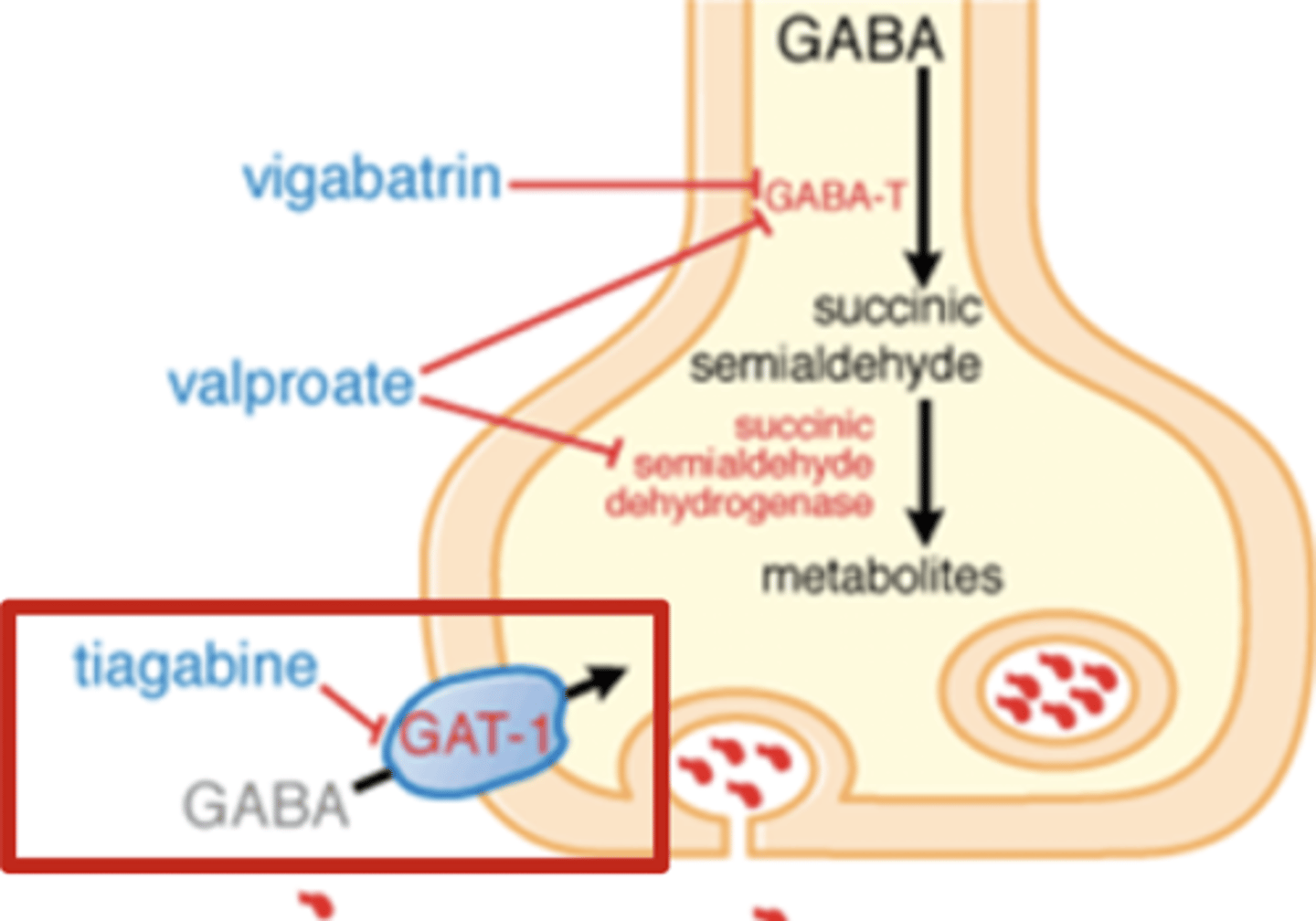
How does increasing GABA activity treat seizures?
Inc. inhibitory tone
Prevents excessive excitation
A cause of excessive neuronal activity (seizures)
What anticonvulsants work by increasing GABA activity?
Barbiturates
Benzodiazepines
Vigabatrin
Valproic acid (valproate)
Tigabine
What is the MOA of Vigabatrin?
Inhibits GABA-T
Dec. GABA metabolism
Inc. GABA conc.
Inc. inhibitory tone
(GABA-T = GABA transferase)
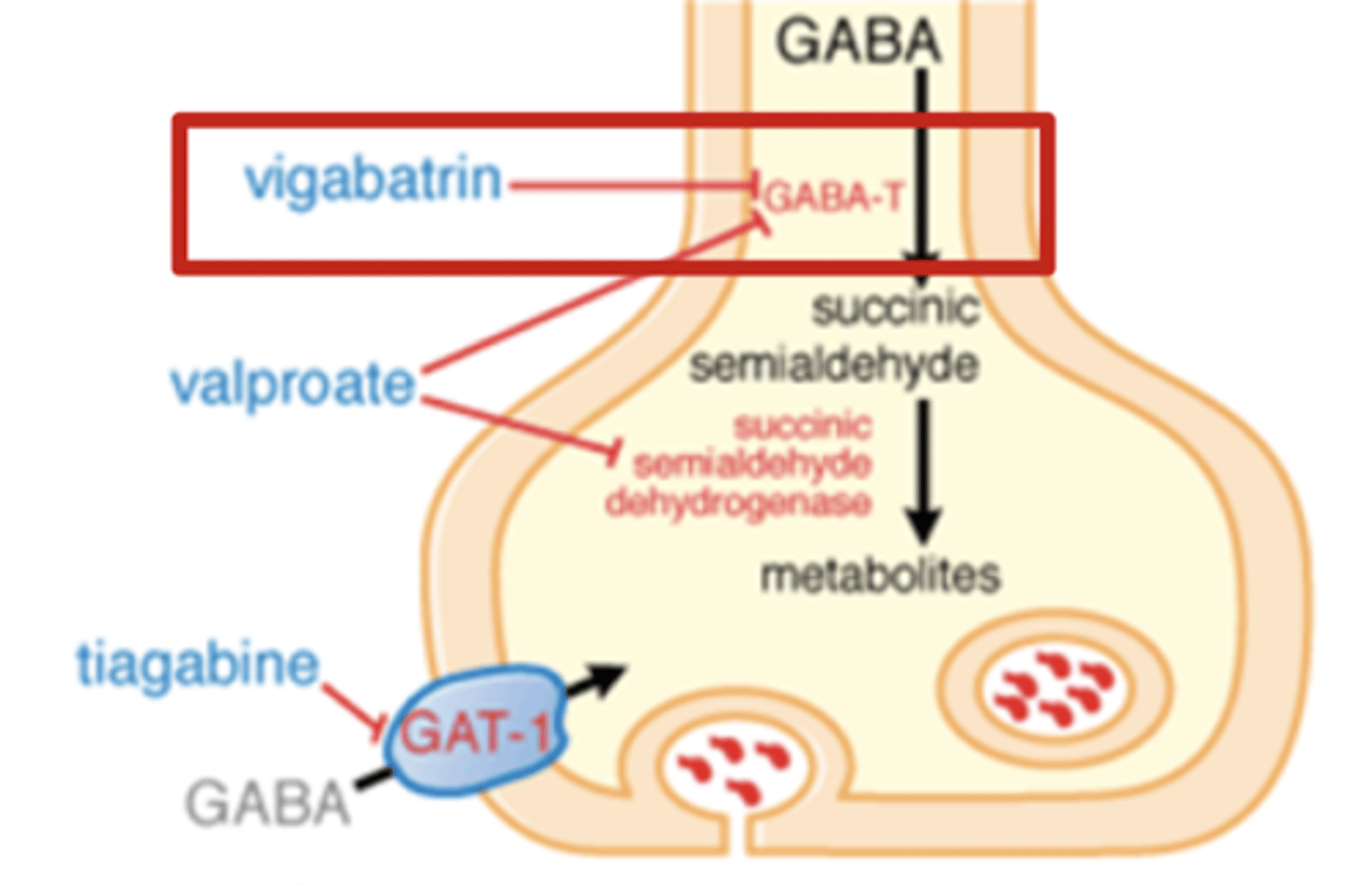
What is the MOA of Tigabine?
Blocks GAT-1
Inhibits GABA reuptake
Inc. GABA conc.
Inc. inhibitory tone
(GAT-1 = GABA transporter, neg. regulator of GABA - performs reuptake)
What is the MOA of Benzodiazepines and Barbiturates?
Potentiate effects of GABA at GABA-A
Inc. effect of GABA
Inc. inhibitory tone

How does blocking T-type Ca channels treat seizures?
Only for absence seizures
T-type Ca channels present in the thalamocortical network
Prevents reinitiation of oscillation cycle
What anticonvulsants work by blocking T-type Ca channels?
Valproic acid (Valproate)
Ethosuximide
What is the MOA of Ethosuximide?
Blocks T-type Ca channels
Prevents from being opened by hyperpolarization, and causing subsequent depolarization
Used for absence seizures
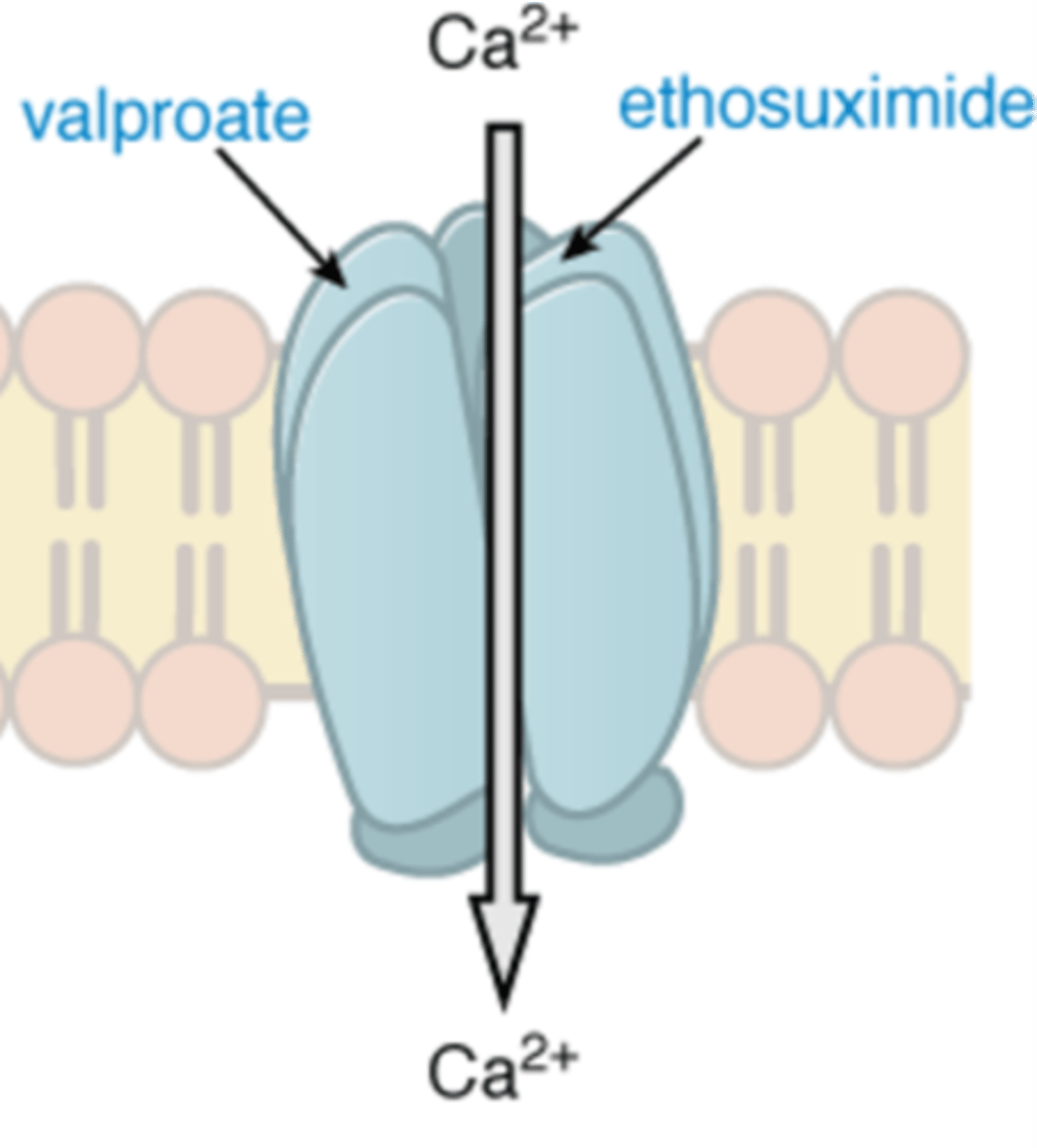
What is the MOA of Valproic acid (Valproate)?
Prolongs inactive conformation of voltage-gated Na channels
Inhibits GABA-T and SSADH --> dec. metabolism of GABA)
(inc. GABA activity)
Blocks T-type Ca channels
Why can Clonazepam, a benzo, be used in Absence seizures?
GABA neurons express their own GABA-A
GABA-A can be inhibited by Benzo's
Clonazepam is selective for GABA-A present on GABAergic interneurons
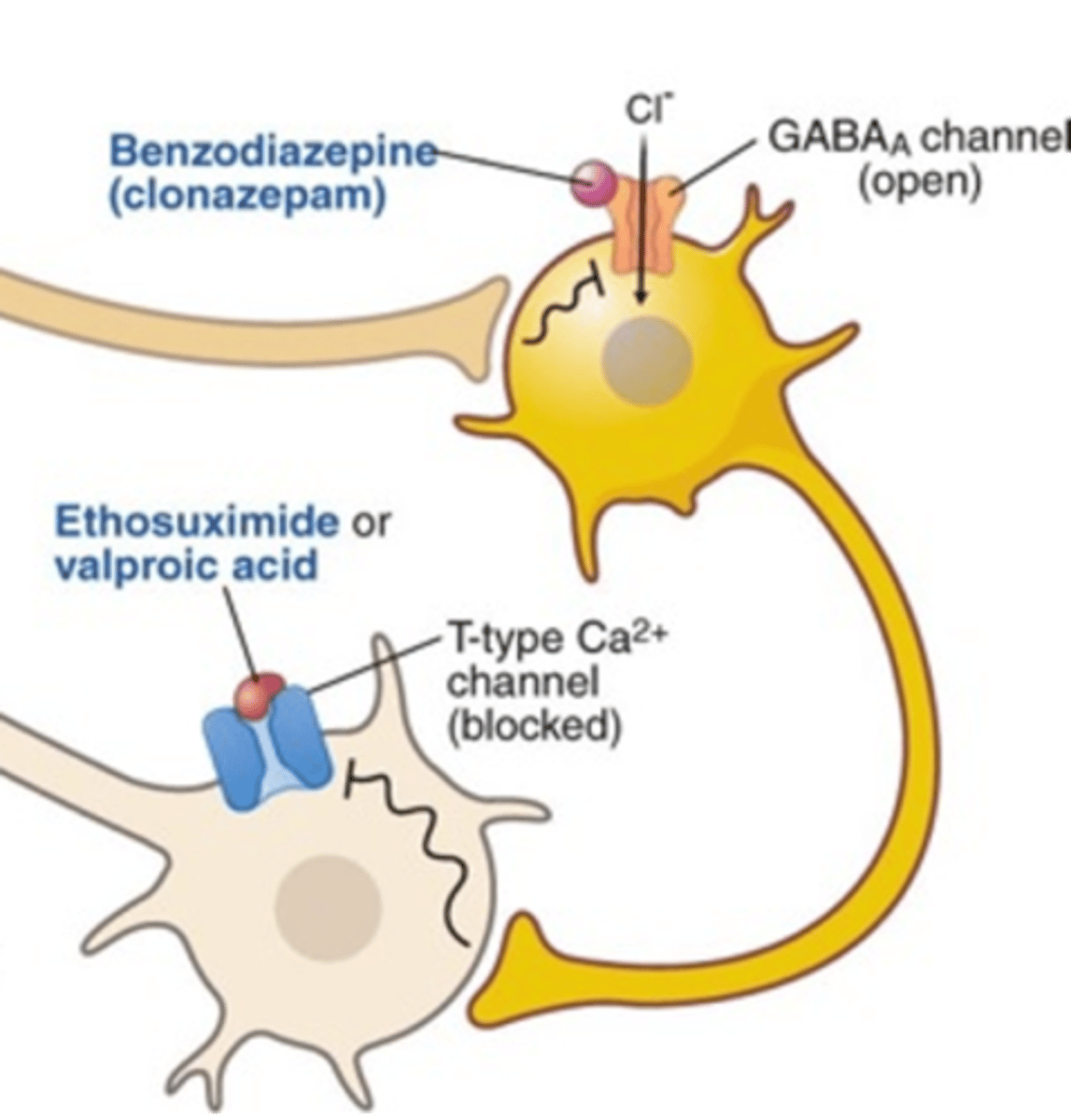
What type of GABA-A is Clonazepam selective for?
Selective for GABA-A present on GABAergic interneurons
(ones involved in absence seizures)
What is the effect of Clonazepam in Absence seizures?
Acts at GABAergic interneuron
Potentiates effects of GABA at GABA-A
Leading to inc. inhibition
Causes interruption of hyperpolarization cycle that is present in Absence seizures
How does inhibiting Glu activity treat seizures?
Block Glu activity to reduce excitatory transmission
Prevents excessive excitation
What anticonvulsants work by blocking Glu activity?
Felbamate
Gabapentin
What is the MOA of Felbamate?
NMDA receptor antagonist
Inhibits Glu excitation by antagonizing it's receptor
Prevents AP transmission
What is the MOA of Gabapentin?
Inhibits voltage-gated Ca channels
Prevents Ca entry, which prevents NT release
Prevents excitation and spreading cause by NT
What is status epilepticus (SE) defined as?
1 continuous, unremitting seizure lasting >30 mins
OR
Recurrent seizures, w/o regaining consciousness between, lasting >30 mins
(brain in persistent seizure state; life threatening medical emergency
What is the treatment for status epilepticus (SE)?
IV diazepam or lorazepam
Why are IV Diazepam/Lorazepam used for status epilepticus (SE)?
Penetrate BBB quickly
Effective at stopping SE
What is the downside of using IV Diazepam/Lorazepam for status epilepticus (SE)?
Have short DOA when given by IV
(due to redistribution)
Seizures may recur
How is seizure recurrence prevented in status epilepticus (SE) treatment?
Give loading dose of a longer acting drug
SUch as phenytoin, phenobarbital, or carbamazepine
How are anticonvulsants metabolized?
Most are CYP450 substrates
Some may also inhibit or induce CYP enzymes
(D/I concerns)
How does enzyme induction occur?
Drug induces gene expression
Inc. gene expression eventually inc. conc. of enzyme
(takes time to accum. enzyme)
Inc. enzyme conc. leads to inc. metabolism of it's substrates
When do effects enzyme induction manifest?
Inc. enzyme activity 2-4 weeks after continuous dosing
Doesn't follow drugs kinetics
Need to wait to adjust dose
Can an inducer be spaced out from it's interacting drug to negate the interaction?
No, the issue is the enzyme has accum.
Enzyme accum. will still be present even if inducing drug isn't
When do effects enzyme induction disappear?
Inx. activity continues after drug discontinuation
(≥2-4 weeks)
Need time for accum. enzyme to be cleared
Doesn't follow drugs kinetics
How does enzyme inhibition occur?
Drug binds to and inhibits the metabolizing enzyme
When do effects enzyme inhibition manifest?
Dec. enzyme activity whenever the drug is present
Follows the drugs kinetics