Circadian Rhythms and Sleep
1/71
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
72 Terms
Endogenous, Exogenous changes
Endogenous biological clocks (i.e., that are internal to the individual) influence biological rhythms.
last about a day, sleepier at night and more alert in the day even without sleep.Higer cortisol in the day, higher melatonin at night, higher body temp during day.
Exogenous: Changes in the environment, external to an individual influencing biological rhythms.
Endogenous circannual vs circadian rhythms
Endogenous biological clocks (i.e., that are internal to the individual) influence biological rhythms
Circannual: Year-long (migration, internal, self-regulated rhythm)
Circadian: 24-hour rhythms → Sleepier at night and more alert in the day, even without sleep.Higher cortisol in the day, higher melatonin at night, higher body temp during the day.
Exogenous rhythm
Changes in the environment (i.e., those that are external to the individual) influence biological rhythms.
Light–dark cycle (most important)
Temperature
Internal changes occurring in the circadian cycle
Cortisol (stress hormone) circadian response: Peaks right what you wake up and diminishes through the day and drops and replenishes in sleep
Melatonin circadian response: released by the pineal gland - builds though the day, fluctuates high in sleep, drops right before you wake up
Body temp: Drops at high and rises through the day → rising body temp tells you to wake up
Chronotypes
There are individual differences in this called chronotypes → morning person vs night
Early chronotypes: Wake up energized and get tired as the day goes on
Late chronotypes: Wake up tired and get more energy as the day goes on
This often changes with age: as a kid you are an early chronotype and then you become late and then go back towards early
Should we push school hours to better align with adolesent sleep patterns? - reduces absense (13-16) and better school performance (14-16)
Free running rhythms
Shift in sleep time without external cues - sun coming up is not resetting clock
So when you don’t have external signals, you would see sleep time would start to shift later and later → too much light would = the opposite
(when we don’t have the circadian cues, our internal clock isn’t actually 24 hours, its longer)

Blindness and circadian rhythm
Unexposed to the sun → insomnia and daytime sleepiness
Your clock isn’t resetting (typically more significant in people who are completely blind (destroyed optic tract or retina)
Can experience a free-running tract
Zeitgebers
Anything in the environment that helps reset the clock and circadian rhythem - Most powerful one is light (resetting SCN)
Others:
Melatonin: sleep onset
Exercise: high intensity in evening can delay next days cercadian cycle
External temp, exercise
Mealtime routines
Social influence
Jet lag
Disruption of circadian rhythms due to time zone changes.
Stress elevates cortisol, which damages the hippocampus; adjusting to circadian rhythms damages hippocampus.
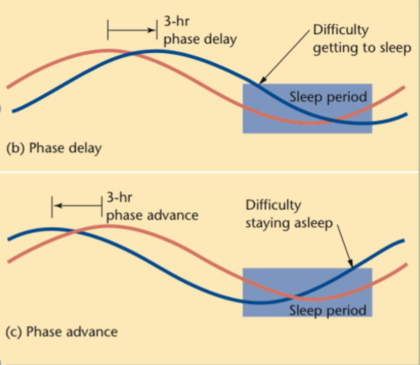
Canadian example - phase delay and phase advance
Toronto → Vancouver (west): you lanmd 10pm but 7am vancouver time = phase delay (stay up later) - easier to do
Vancouver → Toronto (east): you land 7pm but 10pm toronto time = phase advance moving the clock forward (harder to do so you stay up late and wake up toronto time tired)
If your going for a short period of time you should try and stay on the time your coming from → better than taking meletonin
Suprachiasmatic Nucleus location, what does it do
DOESNT RELY ON ANYTHING ELSE
located in the hypothalamus above the optic chiasm
Main driver of sleep and body temp rhythms
Generates circadian rhythms automatically, even if in cell culture isolated from the rest of the body.
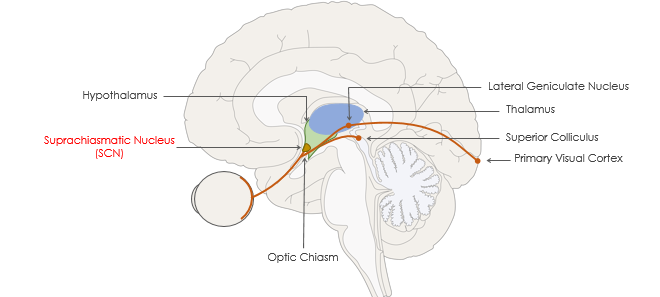
Three major visual pathways (RGR)
There are three different pathways collecting info from the retina
Retinal-collicular pathway: retina to the superior colliculus - primary visual cortex (NON-IMAGE FORMING)
Geniculostriate pathway: lateral geniculate nucleus, not going to the primary visual cortex; synapse with different cells around it (IMAGE FORMING)
Retinohypothalamic Tract: some axons coming from ganglion cells in the retina go off early just above the optic chiasm and activate in SCN involved in regulating circadian rhythms allowing it to act as a zeitgeber
Located near nose and see towards the periphery, respond to the overall amount of light.
Respond mostly to short wavelength or blue light.
ipRGCs
Intrinsically Photosensitive Retinal Ganglion Cells (ipRGCs)
How the Retinohypothalamic Tract Gets Information
Ganglion cells that have opsins able to transduce light energy into ion formation
Contain the pigment melanopsin and respond directly to light. Light resets the SCN via these ganglion cells
Circadian rhythm genes
Two key circadian clock genes that produce PER and TIM proteins.
Proteins rise and fall over 24 hours, helping regulate the body’s sleep–wake cycle.
High PER/TIM levels promote sleepiness, and their daily oscillation keeps the internal clock running.
PER = period → affects the length of the daily cycle.
TIM = timeless → without it, the body has no timekeeping signal.
PER and TIM feedback loop
Cells functioning as an internal clock:
Genes are transcribed into proteins inside the SCN (from per & tim mRNA to per and tim proteins - slow at first) - DNA → MRNA → Proteins
When PER and TIM proteins accumulate (after a lag) they inhibit the transcription of per and tim genes that create the mRNA molecules.
Fewer proteins are produced = less inhibition on the genes which makes them start to produce more (mRNA has declined leading to PER and TIM protein levels decline again.)
During the day, PER and TIM mRNA increase concentration which delays the increase PER and TIM protein concentrations.
During the night PER and TIM protein concentrations remain high to promote sleep and by the next morning, mRNA has declined leading to PER and TIM protein levels decline again.
How does light effect TIM protein
Light helps facilitate breaking down the tim protein to speed up this reset process (starting to produce the MRNA again faster)
Different types of Intrinsically Photosensitive Retinal Ganglion Cells (ipRGCs)
M1: Non-image-forming → axons done help us make an image they send axons to SCN and convey how much light is coming in (not ab shapes or objects) → THIS IS WHAT RESETS THE SCN
M3: Not sure what they do
M2, M3, M4: Image forming: gives info about light contrasts → some going to the superior colliculus
What would happen to SCN if it was taken out of the brain
They would still be able to keep time
Process of melatonin entering the blood stream
Starting at the Suprachiasmatic Nucleus → sends axons to the paraventricular nucleus both in the hypothalamus
Axons move from para down to the intermediolateral nucleus of the spinal cord
Connects to superior cervical ganglion
This triggers the SCN, which activates the pineal gland, secreting melatonin (hormone) 2-3 hours before sleep
Feedback effect on the SCN through MT1 and MT2 receptors
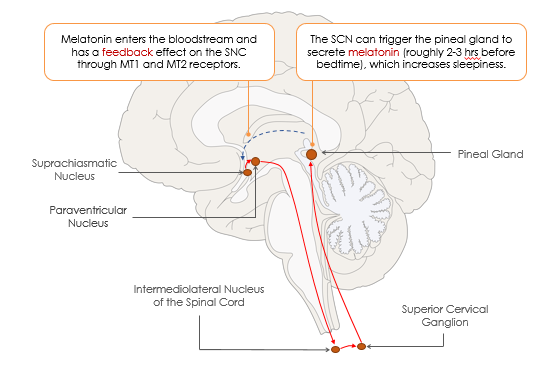
How do melatonin supplements work
They trick the system into thinking the pineal gland has been activated secreting melatonin
What kind of gland is the pineal gland
Endocrine gland releasing melatonin
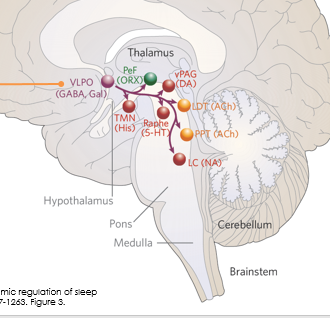
Pedunculopontine nuclei & Laterodorsal tegmental nuclei
2 nuclei responsible for regulation of arousal
Secreting Acetylcholine
Locus Coeruleus
In the basal forebrain
Secretes adrenaline (norepinephrine)
Dorsal and medial raphe nuclei
Secretes serotonin (5HT)
Tuberomammillary nucleus of hypothalamus
Secretes histamines in the hypothalamus → if you have allergy symptoms, you have a lot of histamine activation
Antihistamines = make you drowsy because it stops the excretion of histamine which is excitatory
Lateral Hypothalamus
Releases orexin - alerts the system to keep the other areas active (excitatory) → lack or orexin = narcolepsy
Releases melanin-concentrating hormone more active during sleep (can be inhibatory more in REM)
Ventral Periaqueductal Grey
Releases dopamine (excitatory)
Basal Forebrain
Releases Acetylcholine (excitatory) and GABA (can have inhibitory effects in REM)
Ventrolateral preoptic nucleus
Primarily active during sleep
Contains inhibitory neurotransmitters galanin and GABA
It is connected to and inhibits all the excitatory neurons
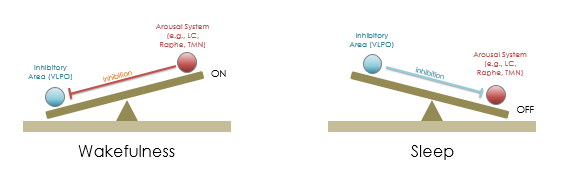
Flip-fop switch
When the arousal system is active → it inhibits the VLPO → you stay awake.
When the VLPO is active → it inhibits the arousal system → you fall asleep.
Inhibitory area (VLPO) shuts off when the arousal system is activated on when the arousal system is inactive
Changes your state in a rapid period of time (unconscious to conscious)
One is inhibited and one isn’t
Sleep pressure
Buildup of adenosine, which is inhibitory
Ultimately, there is enough; it inhibits the excitatory area, meaning it cant inhibit LPVO
If you inhibit the excitatory area, it can’t inhibit the VLPO
What makes the flip switch
In the daytime, the suprachiasmatic nucleus inhibits the VLPO and excites the excitatory areas
At night, it stops sending excitatory and inhibitory signals, allowing inhibitory signals to take over, and because excitatory isnt getting a boost from the SCN it’s inhibited
Another elements driving flip if the switch – adenosine build up
SCN is no longer tipping the scales towards excitatory area and sleep pressure had built up inhibiting sleep
Alpha waves
relaxation
Coma
Extended unconsciousness with low brain activity
Polysomnography
How do we record sleep stages - a combo of EEG and eye-movement records
Stage 1 of sleep
Stage 1: sleep has just begun showing low-voltage, irregular, lagged alpha waves (brain activity is beginning to decline) - eyes are generally stable
K-complex
Sharp wave inhibiting neuronal firing temporarily
Stage 2 of sleep
Two EEG patterns emerge
Sleep steadiness: Sleep spindles 12- to 14-Hz waves showing a burst that lasts at least half a second
K-complex: a sharp, LARGE-amplitude negative wave followed by a smaller, slower positive wave → might be related to external stimuli (noises)
Related to the consolidation of memory
Sleep spindle
Burst of 12-14 Hz waves, improves memory.
Result from oscillating interactions between cells in the thalamus and cortex, increase after new learning and improve memory.
Paradoxical sleep
REM sleep
Called paradoxical sleep bc even through brain activity looks like its more active, your postural muscles are completely inhibited - brain more active
The cornea creates a bulge that makes an indentation on the eyelids
Light sleep
Electrooculogram
Tracks the movement of eyes in REM sleep Measures the electrical activity of the eye muscles
EEG shows irregular voltage signals, indicating neural activity has increased relative to stage 4
Stage 3-4 of sleep
Slow-wave sleep (deepest sleep):
EEG recording of slow, large amplitude waves
Slowing of HR, breathing rate, & brain activity
Highly synchronized neuronal activity
• Periods of rapid eye movement sleep (REM); aka paradoxical sleep
EEG waves are irregular, low-voltage & fast indicating ↑ neuronal activity (light sleep)
Postural muscles of the body are more relaxed than other stages (deep sleep)
Eyes move back and forth
Why do the waves become larger amplitude in stage 3 & 4
neural activity is synchronizing
What would an average sleep cycle look like
Repeating every 90 mins
Typically goes through stages 1,2,3,4
Going up to REM and going back down to deep sleep over and over
With some random wake up periods
Low wave is earlier in the night → stages aren’t equally distributed (if you woke up at hour 4 you would miss out on a lot of REM sleep but have a lot of slow wave sleep)
PGO wakes
High-amplitude electrical potentials in pons, lateral geniculate, occipital cortex.
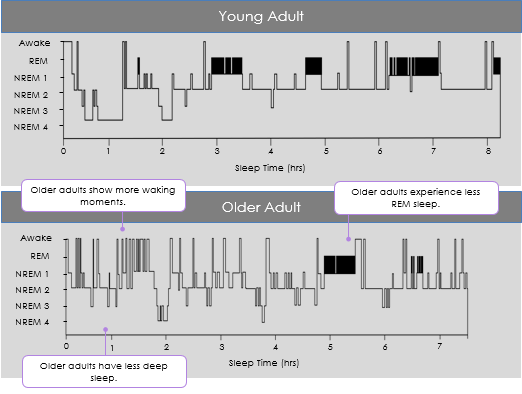
Hypnogram - what are common things to see
Measures the time spent in various stages of sleep during a single night
Slow sleep waves = earlier in sleep period
Cycles repeat roughly every 90 mins
REM increases later in the sleep period
Sleep differences among the lifespan
You sleep mostly as a baby, mostly in REM (16 hours)
Old: More waking moments, less deep sleep, less REM sleep (overall worse)
You sleep less over time and less REM sleep - there are always individual differences
adenosine cannot be cleared, and your adenosine load increases
What happens if you don’t get enough sleep
adenosine cannot be cleared, and your adenosine load increases
What are the main functions of sleep
Upregulation of growth hormones, especially in children
Cell restoration and replication go up - won’t be as efficient in cell rep without it
Clearance of byproducts built up from the day
How do biproducts clear (study on rat)
During the day, the beta-amyloid builds up and needs to be removed (very little movement in the day)
Space between the cells is bigger in sleep, allowing for more movement of the fluid between the cells
Movement of substances through the interstitial space (space between cells in the brain) was more efficient while the rat was asleep than when it was awake (tracked by a tracer) - adenosine is also moved out
Beta Amyloid build up can cause alzhimers’s
Memory consolidation and sleep
If given a task, you can become faster and make fewer errors after sleep
While you're asleep your brain is consolidating the learning and benefiting first thing in the morning – training gets better with time – leads to durable learning (consolidation stays)
If you engage in some learning before bed and then sleep, you will do better
Longer stage 2 non-REM sleep, more benefit obtained
Just before you go to sleep, go over notes, key: RETREVAL things are easier to remember
How does dreaming work - activation synthesis model
Mess of emotions, memories, etc, with no filter - won’t even realize it’s weird until after
Deactivated:
When you're asleep, the prefrontal cortex is deactivated, reducing insight, reasoning, and volition (typically suppresses things)
Processing of incoming stimulation is reduced
Motor system is deactivated (so you don’t act on what is happening in the dream)
Activated:
Amygdala and hippocampus are activated, triggering emotions and memories
Visual association areas are activated, leading to visual imagery
Brainstem arousal neurons activate various areas in the brain
EMG vs EOG
EMG = Electromyogram → tracks muscle tension/tone
EOG = Electrooculogram → tracks eye movements
Lucid Dreaming
Sharing characteristics of wakefulness and dreaming (its not either, it’s a hybrid) - your aware that your dreaming
How can people become better lucid dreamers
Sleep studies done using EEG, EOG, EMG
Awake with eyes closed → practice specific eye movement pattern tracked by EOG (lots of activity seen in the prefrontal cortex
Then when they are sleeping there are irregular eye movements (lower prefrontal cortex activity)
But when you tell them before sleep “when you notice something strange in you sleep notice it but stay asleep” signal to us that your in this state by moving your eyes in the original pattern they trigger a level of awareness and do the pattern (muscle activity is still inhibited, prefrontal is in hybrid state not as active as awake not as inactive as normal sleep)
What is narcolepsy
Sleep disorder with a dysregulation of sleep and normal waking times - Loss of orexin-producing neurons in the lateral hypothalamus, which normally activate other areas promoting wakefulness.
Sleep attacks → unexpected moments of sleepiness during normal waking hours
Cataplexy → Unexpected moments of muscle weakness
Sleep Paralysis → Inability to move during transitions between waking and sleep (conscious but can’t move)
Hallucinations → might occur with paralysis
Might not have all
Cause of narcolepsy
Caused by a loss of hypothalamic cells that release orexin (for staying awake), often caused by an autoimmune reaction where the immune system attacked those cells
Low orexin levels can diagnose.
Flip-flop switch not controlled.
Treating with stimulant drugs that enhance dopamine and norepinephrine activity
Orexin itself cannot cross the blood-brain barrier.
Hypnagogic vs Hypnopompic
Hypnagogic (while falling asleep)
Hypnopompic (while waking up)
Physiology of cataplexy
orexin loss - associated with strong positive emotions
Activate amygdala and arousal areas (hypothalamus) releasing orexin
But with orexin loss that part doesnt get activated - the amygdala activation reduces activity in brain regions that inhibit REM sleep and therefore REM sleep is premoted (in the brainstem/nuclei)
This inhibits muscle movement like would happen in REM = weakness in muscles
OSAS
Obstructive Sleep Apnea Syndrome
Airway in your neck and back of mouth collapses, restricting air flow → all of a sudden stop breathing, triggering gasping for air - back to bed, gasp back again
They don’t realize it, don’t feel rested
Treated with a Continuous Positive Airway Pressure Machine → forces air down the airway
What are risk factors for sleep apnoea
Older age
Male sex
Obesity (especially upper-body obesity)
Upper airway narrowing from craniofacial or soft-tissue abnormalities
Genetic predisposition (family history)
Smoking
Nasal congestion
Genetically smaller airways
Menopause or post-menopause
Medical conditions: hypertension, diabetes, Marfan syndrome, acromegaly, hypothyroidism, end-stage renal disease, congestive heart failure, COPD, neurological disorders, pregnancy
Medications/substances: alcohol, benzodiazepines, narcotics
NREM Insomnias
Unusual behavioral experiences during sleep
Confusion Arousal: Aroused momentarily during sleep (gets confused and disoriented and then goes back to sleep - not fully awake)
Sleep Terrors: Sudden arousal state, waking up terrified maybe run around, screaming, etc - almost impossible to consol, when episode has ended they will go back to sleep and not remember in the morning
Somnambulism - asleep but engaging in some movement
Different kinds of somnambulism
Sometimes purposful
Sleep walking
Sexsomnia
Sleep-related eating disorder
Sleep texting
REM Parasomnias
REM Behavior Disorder
Dream-enactment behavior can occur when muscles become disinhibited during REM sleep.
Can involve movements of limbs and even getting out of bed
Mucles inhibition isn’t strong enough
Onset vs Maintenance Insomnia
More common than parasomnias
Onset: difficulty getting asleep - Phase delay (body temp had trouble going down)
Maintence: staying asleep - phase advance (body temp says its time to wake up)
Can be caised my a cercadian shift (phase delay or phase advance
Triggers of insomnia
Stress
Too much light at bedtime (serving as zygabers)
High temperatures at bedtime (serving as zygabers)
Late night exercise
Late night eating
Drugs (caffeine & alcohol)
Irregular bedtimes: -you need a stable circadian rhythm - theres an aspect of sleep that’s contextually learned (routines signal to you that you need to start lowering body temp, etc) aka you can classically condition yourself
Late night media use: Studying on the bed is bad because your signaling your body to sleep (being in bed when your not sleeping will make it harder to sleep later)
Why does alcohol make it hard to sleep
To some extent it does help because it’s a neural inhibitor
but then it is seen as the body and a toxin, and it will raise the body temperature and you will get waken up later because the body is hot
Unresponsive wakefulness syndrome
Higher than coma, alternates between sleep and arousal
Minimally concious state
Higher than UWS, brief purposeful actions, limited speech comprehension.
Brain Death
No brain activity ot response to stimuli
Polysomnograoh
Records EEG and eye movements to measure sleep stages.
Thalamic neuron hyperpolarization
Reduces response to stimuli during sleep, neurons firing less than usual rate is caused by inhibition to keep us asleep (GABA release from pons and medulla).