PATHO – Dermatology Flashcards 🧬 – IRAT 6 (Part 1)
1/116
Earn XP
Description and Tags
part 2
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
117 Terms
Viral Infections:What are common viral infections affecting the skin?
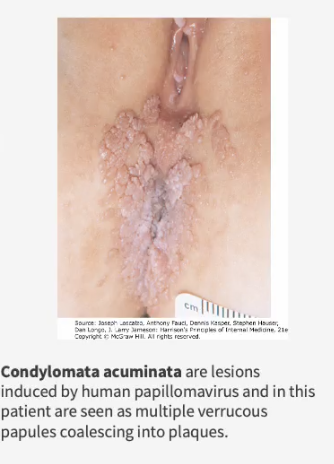
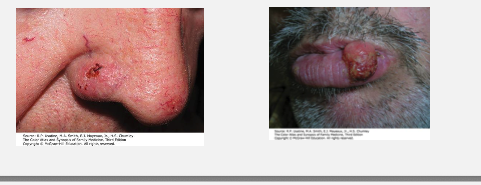
Condyloma Acuminatum- Describe this disease.
Herpes Simplex
Molluscum contagiosum
Varicella-zoster virus
Condyloma Acuminatum-— soft, skin-colored, fleshy lesions
What causes Condyloma Acuminatum?
Human papillomavirus (HPV) infection
Which HPV types cause most cases of Condyloma Acuminatum?
Types 6 & 11 — responsible for ~90% of cases (low-risk)
Which HPV types are associated with high-grade dysplasia and cancer risk?
Types 16, 18, 31, 33, 35 → linked to high-grade intraepithelial dysplasia (↑ cancer risk)
How is Condyloma Acuminatum transmitted?
Through unprotected sexual activity — highly contagious.
What are common risk factors for developing Condyloma Acuminatum? (*7)
Unprotected sex
Multiple sexual partners
Early sexual activity
History of other STIs
Immunosuppression (esp. HIV)
Cigarette smoking
Radiation therapy
Why is Condyloma Acuminatum linked to HIV?
Because both share sexual transmission routes and immunosuppression from HIV increases HPV persistence and severity
What is the pathophysiology of Condyloma Acuminatum?
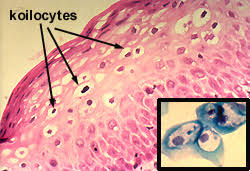
HPV exposure during sexual contact → microabrasions in skin/mucosa → HPV infects basal epithelial cells → viral replication in squamous epithelial cells → epithelial hyperplasia (thickened skin) + koilocytosis (vacuolated cells with perinuclear halos) → formation of soft, fleshy, skin-colored warts (condyloma acuminata)
What are common findings with Condyloma Acuminatum?
hyperkeratosis (Thickened stratum corneum (outer keratin layer) and acanthosis with thickened epidermis (increased squamous cell layers) & rounded epidermal ridges.

What are koilocytes and why are they significant in condyloma acuminatum?
Hint: “Koilocytes = HPV fingerprints under the microscope”
Koilocytes: Squamous epithelial cells with perinuclear halos and irregular, wrinkled nuclei
Represent HPV-infected cells
Found in the upper epithelial layers
Diagnostic hallmark of HPV infection
What are the key clinical features of Condyloma Acuminatum lesions? (*3)
Painless lesions
Warty appearance with multiple fingerlike projections
Large lesions have a cauliflower-like surface
Where do Condyloma Acuminatum lesions typically appear?
Anogenital skin: penis, scrotum, vulva, perianal area
Anogenital tract: vagina, cervix, rectum, urethra, anus
What is Verruca Vulgaris? What causes this? Which
note: vulgaris means common
common wart; caused by HPV
In which age group are verrucae most common?
Children and young adults.
What are the main types of verruca (warts)?
Verruca vulgaris – common wart (HPV 2, 4)
Verruca plantaris – plantar (foot) wart (HPV 1)
Verruca plana – flat wart (HPV 3, 10, 28)
Which HPV types are associated with each wart type?
Common warts (vulgaris): HPV 2, 4 (most common), 1, 3, 27, 29, 57
Plantar warts: HPV 1 (most common), 2, 3, 4, 27
Flat warts (plana): HPV 3, 10, 28
Hint: “Common = 2 & 4, Plantar = 1, Flat = 3 & 10.
What are the clinical features of verruca vulgaris and plantaris?
Vulgaris (hands): firm, hyperkeratotic papules (1–10 mm)
Plantar (soles):
Red-brown punctations (thrombosed vessels)
Tender to pressure
May form large mosaic warts when they coalesce
How do flat warts (Verruca Plana) appear clinically and where are they located?
Soft, flat, flesh-colored papules (1–5 mm)
Found on face, hands, shins; arranged in linear patterns
(Koebner phenomenon – appear along trauma lines) **koebnerization
Herpes Simplex:
What causes Herpes Simplex, and where does it remain latent?
Caused by HSV-1 or HSV-2.
Virus lies dormant in the dorsal root ganglion (DRG) after initial infection.
Reactivated by sun exposure, fever, or other viral infections.
Compare HSV-1 and HSV-2 in terms of spread and prevalence.
HSV-1
Infects >85% of U.S. population.
Acquired asymptomatically in childhood.
Spread by saliva or infected secretions.
HSV-2
Infects ~25% of U.S. population.
Acquired via sexual contact.
Spread primarily sexually.
What are the general clinical findings of HSV infection? (*4)
Burning and stinging pain, ± neuralgia.
Small, grouped vesicles on an erythematous base.
± Regional lymphadenopathy.
Lesions crust and heal within ~1 week.
What areas are commonly affected by HSV-1?
Mouth/oral cavity and face (cold sores, gingivostomatitis).
May involve genital area through oral-genital contact.
Whitlows (digital lesions) may occur on fingers of healthcare workers.
What areas are affected by HSV-2, and what are the key features?
Involves genital tract and external genitalia.
May occur in perianal region, buttocks, or upper thighs.
Often recurrent and may be asymptomatic between outbreaks.
Summarize the pathophysiology of an HSV infection.
Initial infection → virus enters sensory nerve endings → travels to dorsal root ganglion (DRG) → becomes latent → reactivated by stressors (sun, fever, illness) → vesicular outbreak on skin/mucosa → crust and heal
What causes Molluscum Contagiosum and how is it transmitted?
Caused by Molluscum contagiosum virus (poxvirus family)
What does self-limited mean?
“Self-limited” means your body can fight it off naturally
Is Molluscum contagiosum contagious? How does the treatment for this disorder vary with immunocompetent and immunocompromised people.
Highly contagious — spreads via:
Autoinoculation (self-spread by scratching)
Skin-to-skin contact
Sexual contact
Shared clothing or towels
Self-limited in immunocompetent patients
Difficult to treat in immunocompromised individuals
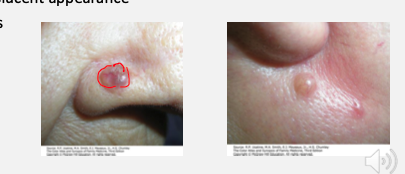
What are the key clinical features of Molluscum Contagiosum? Drescribe, name common sites and the duration of the disease.
Painless, umbilicated (central dimple) cutaneous papules.
Common sites: face, lower abdomen, genitals
Duration:
3–6 months= healthy individuals
Up to 12 months = immunocompromised patients
Name the disorder. Why?
Molluscum Contagiosum;
viral skin infection that causes raised, pearly lesions. It is often benign and self-limited in healthy individuals.

What are the two disease outcomes of Varicella-Zoster Virus infection?
1⃣ Varicella (chickenpox) – primary infection
2⃣ Herpes zoster (shingles) – reactivation of latent virus
What type of infection is caused by VZV?
A highly contagious exanthem (rash) with groups of pruritic vesicles on the skin and mucous membranes.
How is Varicella-Zoster Virus transmitted?
By inhalation of infective droplets or direct contact with skin lesions.
What immune response does exposure trigger?
Production of IgG, IgM, and IgA antibodies.
Where does the virus remain latent after infection?
In dorsal root ganglia (sensory nerves).
What causes herpes zoster (shingles) later in life?
Reactivation of the latent virus along a dermatomal nerve distribution.
Describe the appearance and progression of the Varicella rash.
Pruritic (itchy), papular rash that changes to vesicular → “dewdrops on a rose petal” 🌹
Lesions evolve into pustules, then crust over.

What are the clinical features of the Zoster rash?
Tingling and pain precede the rash.
Vesicular eruption in a dermatomal pattern (follows a single nerve root).
Lesions evolve to pustules, then crust over.
Hint: “Chickenpox spreads; shingles stays in a line.

⭐Keratotic Disorders:
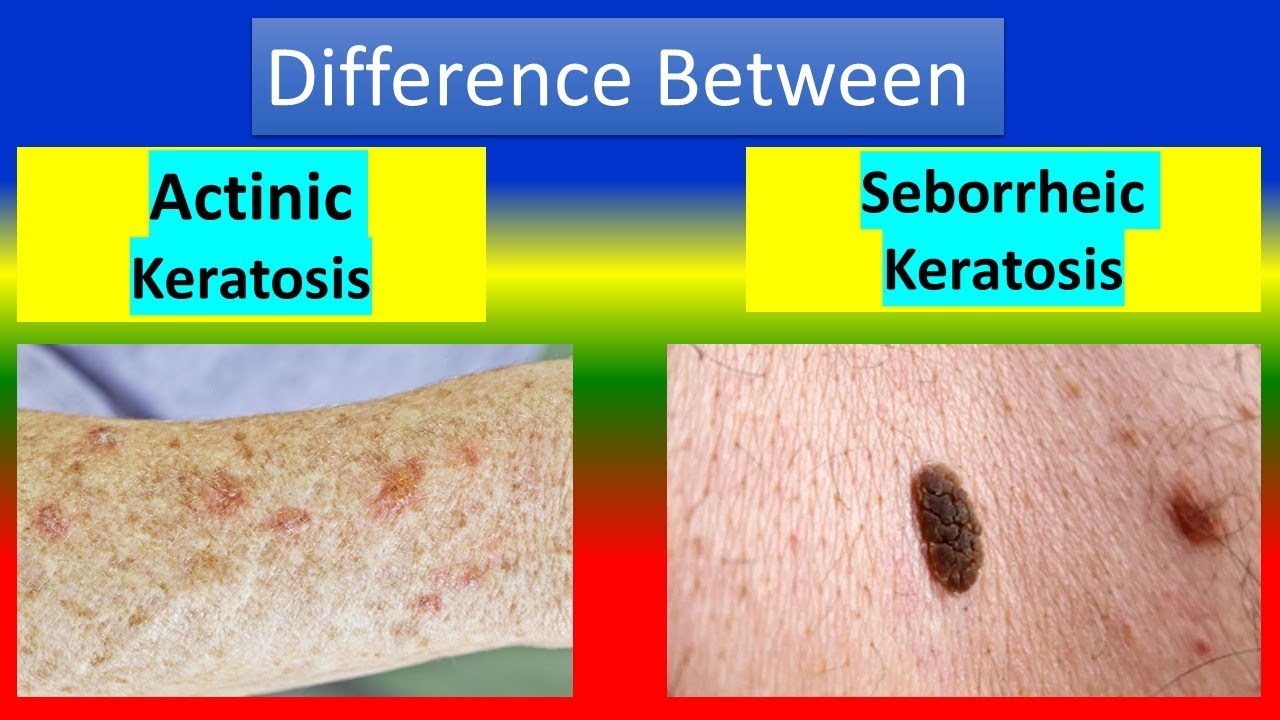
Actinic Keratosis- What is Actinic Keratosis (AK) and why is it clinically important?
Seborrheic Keratosis
Premalignant cutaneous lesion that can progress to squamous cell carcinoma (SCC).
Caused by chronic UV exposure → DNA damage → dysplastic keratinocytes.
Disrupts normal epidermal growth and differentiation pathways.
Hint: “AK → dysplasia → malignancy.”
What are key risk factors for Actinic Keratosis?
Increased age, male gender, fair skin
Chronic sun exposure or geographic UV exposure
Immunosuppression
Hint: Think “older, outdoor, and fair-skinned.”
How does Actinic Keratosis present clinically?
Flesh-colored, pink, or slightly hyperpigmented papules or plaques
Feels like sandpaper – rough, scaly, and tender to touch
Common on sun-exposed areas (face, ears, scalp, arms)
Sometimes has a horn-like projection (cutaneous horn)
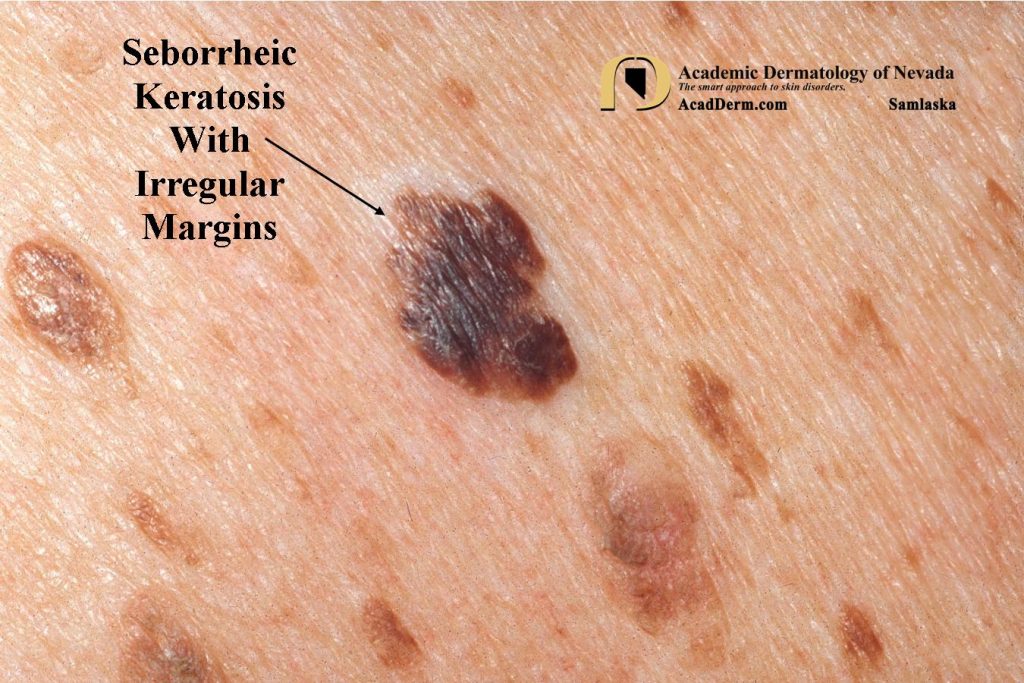
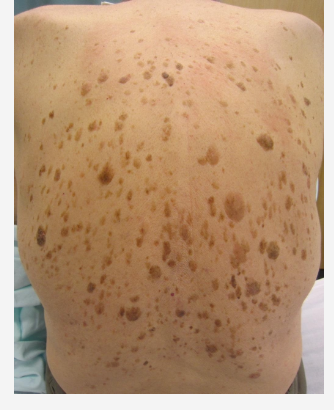
What is Seborrheic Keratosis and how does it form?
Benign, hyperpigmented lesion caused by clonal expansion of epidermal keratinocytes.
Extremely common in older adults and fair-skinned individuals.
May mimic melanoma, but is noncancerous.
What are the classic clinical features of Seborrheic Keratosis? (*5)
Asymptomatic:
Color:
Size:
Texture:
Appearance:
Asymptomatic: lesions
Color: beige, brown, or black
Size: 0.3–2 cm
Texture: velvety, greasy, or warty surface
Appearance: “Stuck-on” or pasted look on the skin
Hx of very acute SKs= Leser-Trélat sign—> can be a sign of GI cancer.
Neoplasms:
Basal Cell Carcinoma- What is Basal Cell Carcinoma (BCC)? **Most common form of skin cancer in the U.S.
Origin:
Cause:
Common sites:
Growth:
Squamous Cell Carcinoma
Malignant Melanoma
Origin: Basal cell layer of the epidermis
Cause: Usually due to chronic UV exposure
Common sites: Sun-exposed areas (face, ears, neck) also can be on the upper lip.
Growth: Slow, with low rate of metastasis
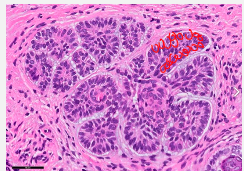
What is the hallmark histologic feature of Basal Cell Carcinoma?
Peripheral palisading of tumor cell nuclei — cells align in a fence-like arrangement around tumor nests.
What are the typical clinical features of Basal Cell Carcinoma?
Papule or nodule with raised/rolled borders and central erosion or ulceration
Waxy, pearly, or translucent surface appearance
Telangiectatic vessels (visible surface blood vessels)
What is Squamous Cell Carcinoma and what causes it?
Second most common skin cancer in the U.S.
Malignant proliferation of squamous cells.
Can arise from Actinic Keratosis.
What are the major risk factors and associations for Squamous Cell Carcinoma?
HPV infection
UVB (sun) exposure
Xeroderma pigmentosum- conjunctiva problems and can’t be in the sun.
Albinism- no protection against UV light due to no melanin
Chronic wounds
Immunosuppression
What is Squamous Cell Carcinoma called when it is confined to the epidermis?
Bowen disease (SCC in situ)
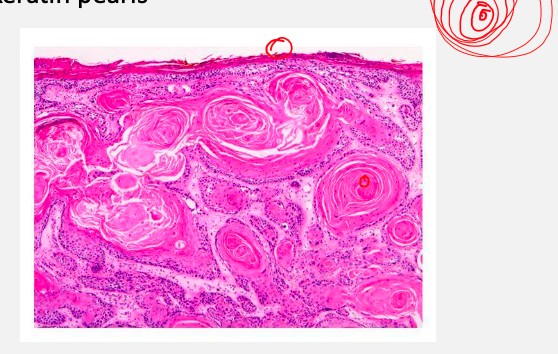
What is the key histologic feature of Squamous Cell Carcinoma?
Formation of keratin pearls (concentric layers of keratinized squamous cells) *note: no nucleus present (how we distinguish with basal cell carcinoma)
How does Squamous Cell Carcinoma present clinically?
Red, hard, hyperkeratotic papules, nodules, or plaques.
May ulcerate.
Commonly found on sun-exposed areas: ear, lip (lower lip), oral cavity, tongue, and genitalia.
What is malignant melanoma and where does it originate?
5th most common cancer in the U.S.
Leading cause of skin cancer death.
A tumor from malignant transformation of melanocytes.
What are the main subtypes of melanoma and how do they differ?
Subtype | Location / Population | Growth Pattern | Key Notes |
|---|---|---|---|
Superficial Spreading | Most common (≈70%); sun-exposed areas | Radial first | Flat or slightly raised, irregular borders |
Lentigo Maligna | Elderly, chronically sun-exposed skin | Slow radial | Begins as lentigo maligna; good prognosis |
Nodular | Any site, older adults | Early vertical | Fast-growing, poor prognosis |
Acral Lentiginous | Palms, soles, nail beds | Variable | Not UV-related, common in darker skin |
What are the two growth phases of melanoma?
Radial growth: spreads horizontally along the epidermis and superficial dermis (no metastasis).
Vertical growth: invades deep dermis (↑ risk of metastasis).
Hint: “Radial = wide; Vertical = deep and deadly.”
What is the most common subtype of melanoma?
Superficial spreading melanoma (≈70% of cases).
Found on intermittently sun-exposed skin; early radial growth.
What is lentigo maligna melanoma?
Occurs on chronically sun-exposed skin (elderly).
Has a slow radial growth phase.
Best prognosis if caught early.
What is nodular melanoma?
Aggressive; grows vertically early.
Common in older patients; poor prognosis.
What is acral lentiginous melanoma?
Appears on palms, soles, or nail beds.
Not related to UV exposure; more common in darker skin tones.
What does ABCDE stand for in melanoma evaluation?
A – Asymmetry: uneven shape
B – Border: irregular, notched
C – Color: multiple colors
D – Diameter: >6 mm
E – Evolution: change over time
What are other important melanoma warning signs?
Color variation (multiple pigments)
Elevation / nodularity
“Ugly duckling sign” – mole looks different from others
Rapid change in size, color, or shape
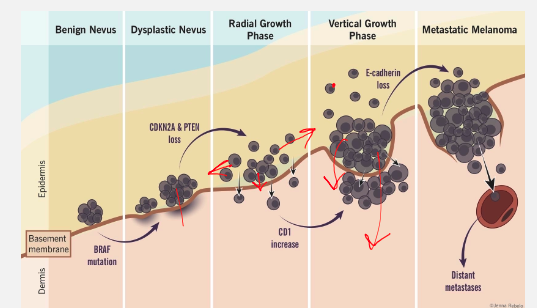
Benign Nevus:
What happens in a benign nevus?
Normal, noncancerous mole composed of melanocytes.
BRAF mutation may be present but cells remain contained above the basement membrane.
What characterizes a dysplastic nevus?
Shows atypical cells and irregular architecture.
Genetic changes include CDKN2A and PTEN loss, increasing malignancy risk.
What happens during the radial growth phase of melanoma?
Tumor spreads horizontally (laterally) along the epidermis and superficial dermis.
No metastatic potential yet.
CD1 expression increases → promotes immune evasion and cell migration.
What defines the vertical growth phase?
Tumor invades deeper dermis and connective tissue.
E-cadherin loss → cells detach and invade deeper layers.
Metastatic potential begins here.
What occurs in metastatic melanoma?
Melanoma cells penetrate blood or lymphatic vessels.
Distant metastases form (commonly to lungs, liver, brain).
Depth of invasion (Breslow depth) is the main prognostic factor.
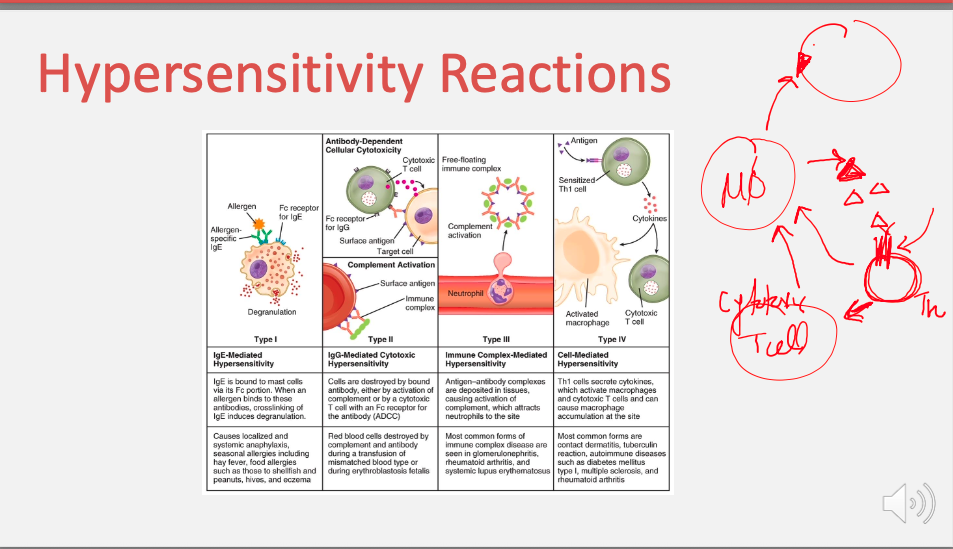
What is a Type I hypersensitivity reaction and how does it occur?
IgE-mediated (immediate) reaction.
Allergen binds to IgE on mast cells → degranulation → histamine release.
Causes anaphylaxis and allergic reactions (e.g., hay fever, food allergies, asthma, eczema).
What is a Type II hypersensitivity reaction?
IgG or IgM antibodies target antigens on cell surfaces → cell destruction.
Occurs via complement activation or antibody-dependent cytotoxicity (ADCC).
Examples: Hemolytic anemia, Goodpasture syndrome, blood transfusion reactions.
Antibody-mediated reaction targeting cell surfaces.
Involves IgG or IgM antibodies that lead to cell destruction through mechanisms such as complement activation or ADCC.
What is a Type III hypersensitivity reaction?
Immune complexes (antigen–antibody) deposit in tissues → inflammation and complement activation.
Attracts neutrophils, causing tissue damage.
Examples: Serum sickness, SLE, rheumatoid arthritis.
Hint: “Type III → Immune Complex → 3 words.”
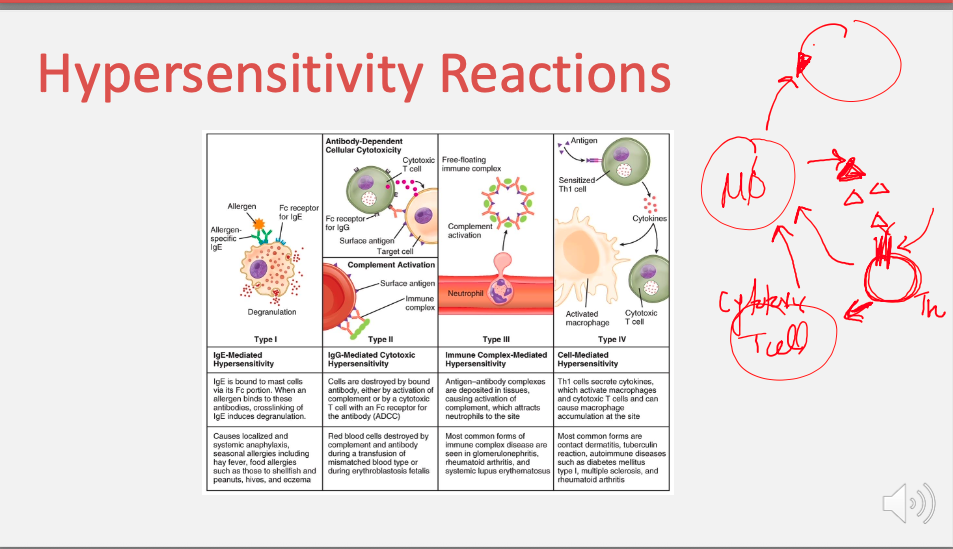
What is a Type IV hypersensitivity reaction?
T-cell mediated (delayed) response — no antibodies involved.
Cytotoxic T cells and Th1 cells release cytokines → macrophage activation → tissue injury.
Examples: Contact dermatitis, TB skin test, type 1 diabetes, multiple sclerosis.
Papulosquamous Disorders:
Contact Dermatitis- What is Contact Dermatitis and what causes it?
Eczema
Lichen Planus
Pityriasis rosea
Psoriasis
Acute or chronic skin inflammation caused by direct skin contact with irritants or allergens.
Irritants: soaps, detergents, solvents, prolonged exposure (urine/feces).
Allergens: poison ivy/oak, nickel, rubber, fragrances, topical antibiotics.
How does irritant contact dermatitis develop?
Chemical injury disrupts the skin barrier.
Keratinocytes release proinflammatory cytokines, causing inflammation.
Severity depends on concentration, duration, and frequency of exposure.
What are the two phases of allergic contact dermatitis?
Sensitization phase:
Allergen (hapten) binds to skin proteins → processed by APCs → activates CD4+ T cells.
Forms antigen-specific memory T cells.
Elicitation phase:
Reexposure → APCs present antigen again → memory T cells release cytokines → inflammation.
Hint: “1st exposure sensitizes, 2nd exposure reacts.”
How does Contact Dermatitis present clinically?
Acute: Erythematous papules or vesicles (linear/geometric), with ±itching, burning, stinging.
Chronic: Lichenification, fissures, and scaling from repeated exposure.
What causes eczema (atopic dermatitis)?
Chronic inflammatory skin disorder due to a defective skin barrier that allows drying and irritation.
Often associated with the atopic triad: atopic dermatitis, allergic rhinitis, and asthma.
What genetic mutation is linked to eczema and how does it affect the skin?
Filaggrin gene mutation → defective skin barrier (stratum corneum).
Leads to “leaky” skin, water loss, and dryness.
Allows antigens and microbes to penetrate → inflammation and infection risk.
What triggers eczema flare-ups?
Heat, perspiration, allergens, and contact irritants.
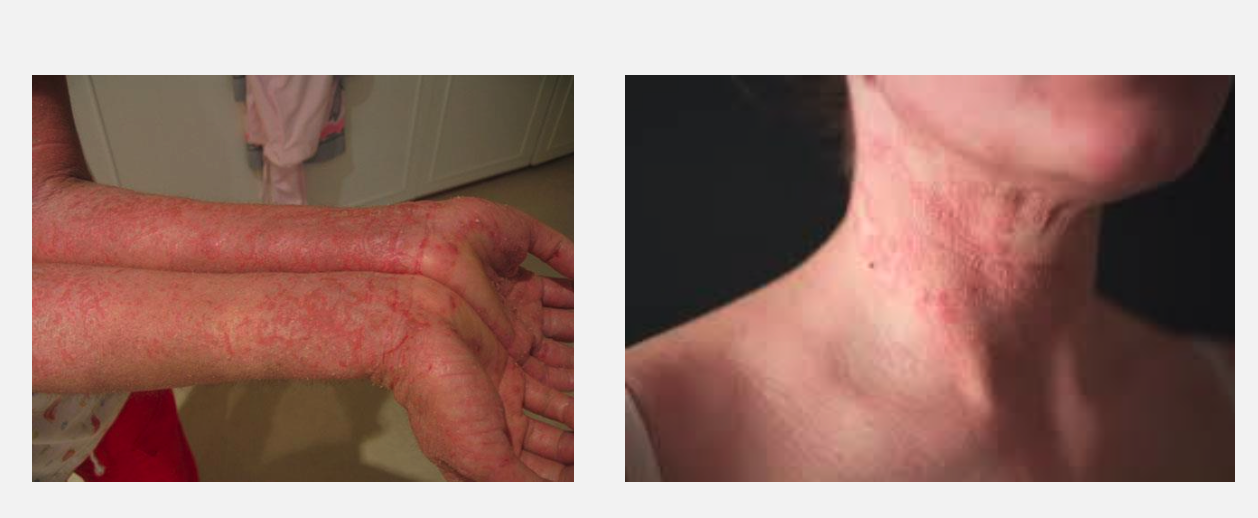
What are the key features of the eczema rash?
Pruritic, dry, erythematous papules or plaques.
Chronic cases may show lichenification (thickened skin from scratching).
Where does eczema typically occur in infants and adults?
Infants: Widely distributed—> Extensor surfaces (wrists, elbows, ankles, knees).
Adults: Flexural surfaces (antecubital and popliteal fossae).
What is Lichen Planus? Also, what is the cause?
Acute or chronic inflammatory disorder of the skin and mucous membranes.
Unknown cause, but involves inflammation at the dermal-epidermal junction → “saw-tooth” appearance on histology.
What conditions and medications are associated with Lichen Planus?
Hepatitis C infection
Drug-induced: thiazide diuretics, antimalarials, penicillamine, phenothiazines
Malignant lymphoma
What are the classic features of Lichen Planus?
**6 Ps
Pruritic (itchy)
Purple
Polygonal
Planar (flat-topped)
Papules / Plaques
What are other notable findings in Lichen Planus?
Koebner phenomenon: new lesions at trauma sites
Mucosal involvement: mouth, tongue, genitals (Wickham’s striae – fine white lines)
May cause alopecia and nail dystrophy

What is the characteristic histologic finding in Lichen Planus?
Inflammation at the dermal-epidermal junction → “saw-tooth” appearance.

What is Pityriasis Rosea and what causes it?
Acute, self-limiting papulosquamous disorder.
Exact cause unknown, but possibly linked to Human Herpesvirus 6 or 7 (HHV-6/7).
What is the “Herald patch” in Pityriasis Rosea?
First lesion: solitary salmon-colored, red or brown macule on trunk.
Size: 2–6 cm in diameter.
Appears before the main rash (precursor lesion).
How does the rash of Pityriasis Rosea progress?
1–2 weeks after Herald patch, multiple scaly oval plaques appear.
Typically follows a “Christmas-tree” pattern on the trunk (along skin tension lines).
What are the common symptoms and course of Pityriasis Rosea?
Pruritus (itching) is mild in most but severe in ~25% of patients.
Rash and Herald patch last 6–12 weeks.
Self-resolves without scarring.

What is psoriasis and what causes it?
Chronic inflammatory autoimmune skin disorder.
Multifactorial — genetic + environmental influences.
Strongly associated with HLA-C.
HLA-C = immune recognition gene
HLA-Cw6 variant = major genetic link to psoriasis.
What are key histologic features of psoriasis?
Hint: “Thick skin, thin granular layer, neutrophils up top.
Acanthosis: epidermal hyperplasia (thickened skin).
Parakeratosis: stratum corneum retains nuclei.
Stratum spinosum: thickened.
Stratum granulosum: thinned or absent.
Munro microabscesses: neutrophil clusters in stratum corneum.

What are the classic skin findings in psoriasis?
Well-circumscribed, salmon-colored plaques with silvery scale.
Common sites: elbows, knees, scalp, neck, gluteal cleft.

What are two hallmark clinical signs of psoriasis?
Auspitz sign: pinpoint bleeding when scale is removed.
Koebner phenomenon: new lesions at sites of trauma (also in eczema)
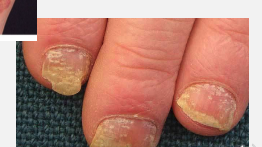
What nail changes are seen in psoriasis?
Pitting and yellow-brown discoloration.
Pigment Disorders:
Melasma- What is melasma and what causes it?
Vitiligo
Acquired hyperpigmentation on sun-exposed areas, especially the face.
Common in women with darker skin tones.
Triggered by UV light and increased estrogen (pregnancy, OCP use).
Leads to ↑ melanin synthesis in susceptible individuals.

How does melasma appear clinically?
Symmetrical, hypermelanotic macules (“mask-like” appearance).
Commonly affects cheeks, forehead, upper lip, and neck.
Worsens with sun exposure
What is vitiligo and what causes it?
Acquired depigmentation disorder due to autoimmune destruction of melanocytes.
May occur at sites of trauma (Koebner phenomenon).
Associated with other autoimmune diseases (e.g., thyroid disease, diabetes, alopecia areata).
What are the key clinical features of vitiligo?
Asymptomatic depigmented macules or patches.
No inflammation or scaling.
More visible in dark-skinned individuals.
Light-skinned individuals may have difficulty tanning in affected areas.
Vascular Abnormalities:
Cherry Hemangioma- What is a Cherry Hemangioma and who does it affect?
Telangiectasias
Benign capillary proliferation (noncancerous vascular lesion).
Most common vascular tumor in adults.
Occurs most often in middle-aged and elderly individuals and increases with age.
Caused by abnormal proliferation of mature capillaries in the dermal papillae.
Histology: Tortuous, dilated capillary loops separated by connective tissue.
Not associated with malignancy and does not regress (unlike infantile hemangiomas).
How does a Cherry Hemangioma present clinically?
Appears as small, bright red to purple papules (flat-topped or dome-shaped).
Typically 1–5 mm in diameter.
Blanch with pressure (blood temporarily displaced).
Commonly found on the trunk, arms, and shoulders.
May bleed easily following minor trauma.
Usually asymptomatic and discovered incidentally.
What would you see under the microscope in a Cherry Hemangioma?
Proliferation of capillary-sized blood vessels lined by flattened endothelial cells.
Located in the papillary dermis.
Lumen filled with red blood cells.
Surrounding tissue may show fibrosis with aging.
What are telangiectasias?
Permanent dilation of small blood vessels (capillaries, venules, or arterioles).
Appear as fine red lines or patterns on the skin and mucous membranes.
Can occur anywhere on the body but most visible on the face, chest, and legs.
Often secondary to other conditions (connective tissue disease, liver disease, etc.).
What conditions are telangiectasias associated with
Chronic sun exposure
Systemic sclerosis (scleroderma)
Rosacea
Chronic liver disease (spider angiomas)
Ataxia-telangiectasia (genetic disorder)
Prolonged corticosteroid use (skin thinning and vessel dilation)