Pediatrics: Fever, Dehydration, and Oral Replacement Therapy- Cruz
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
30 Terms
Define each of the following:
fever
hyperthermia
hyperpyrexia
fever: core body temperature >100ºF (37.8ºC)
caused by a regulated rise in body temperature, maintained by the hypothalamus in response to a pyrogen
hyperthermia: a malfunction of normal thermoregulatory processes at the hypothalamic level caused by excessive heat exposure or production
hyperpyrexia: body temp >106ºF (41.1ºC)—> associated with mental and physical signs of symptoms
What is the primary reason for treating a pediatric fever?
idk how important
To alleviate discomfort (should still find underlying cause)
Most accurate method of assessing fever is through a ____________.
thermometer
Which thermometer site is considered the gold standard?
Rectal temperature measurement.
Major risks associated with fever?
idk how imp
seizures, dehydration, change in mental status
Definition of a febrile seizure?
defined as seizure accompanied by fever in infants or children with no intracranial infection, metabolic disturbance, or an otherwise defined cause
2 most important RFs for febrile seizures?
severity of fever
rate of temp increase
True or False: Prophylaxis against simple febrile seizure with antiepileptic or antipyretic is recommended by the APP.
false—> not rec
NON-PHARM TX FOR FEVER:
adequate fluids
wearing light clothing
removing blankets
maintain comfy room temp (~68oF)
body sponging with tepid water (exclusions apply)
PHARM TX FOR FEVER:
APAP and Ibuprofen
State the dosing for pediatric acetaminophen for fever:
10–15 mg/kg every 4–6 hours; max 5 doses/day
State the dosing for pediatric ibuprofen for fever.
5–10 mg/kg every 6–8 hours; max 4 doses/day
Ibuprofen is only approved for fever in pts. >__ months of age
6
What 2 concentrations are available for Ibuprofen?
100mg/5ml
50mg/1.25ml
Does the AAP RECOMMEND ALTERNATING different antipyretics in the same regimen? why or why not?
DOES NOT RECOMMEND—> Increased risk of dosing errors, overdose, and adverse events
What are the exclusions to self-care with fever?
(sorry there’s so many.)
Patients >3 months of age with a rectal temperature ≥104.0ºF (40.0ºC) or equivalent
Children <3 months of age with a rectal temperature ≥ 100.4ºF (38.0ºC)
Severe symptoms of infection that are not self-limiting
Risk for hyperthermia
Impaired oxygen utilization (e.g., CV, pulmonary disease)
Impaired immune function (e.g., cancer, HIV)
CNS damage (e.g., head trauma, stroke)
Children with history of febrile seizures or seizures
Patients >2 years of age with fevers that persist >3 days with or without treatment
Child who:
develops spots or rash
refuses to drink any fluids
is very sleepy, irritable, or hard to wake up
vomiting and cannot keep down fluids
has repeated diarrhea
Children <2 years of age with fevers that persist >24 hours
Fever that repeatedly rises above 104.0ºF (40.0ºC) in a child of any age
Child with a stiff neck
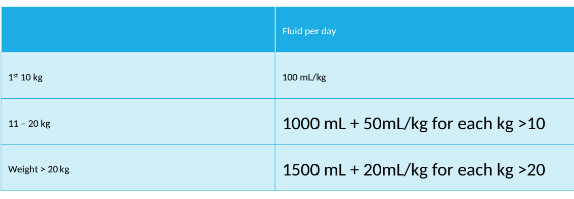
How do you calculate maintenance fluids using the Holiday-Segar Method?
NOTE*** WILL BE GIVEN EQUATIONS ON EXAM
JUST RECOGNIZE AND KNOW HOW TO SOLVE
100 mL/kg for first 10 kg
1,000 mL + 50 mL/kg for each kg >10 kg
1,500 mL + 20 mL/kg each kg >20 kg
PRACTICE:
What is the total fluid amount in milliliters to be given to a patient weighing 6 kg using the Holiday-Segar Method?
What is the fluid rate in milliliters per hour?
What is the total fluid amount in milliliters to be given to a patient weighing 17 kg using the Holiday-Segar Method?
What is the fluid rate in milliliters per hour?
What is the total fluid amount in milliliters to be given to a patient weighing 21 kg using the Holiday-Segar Method?
What is the fluid rate in milliliters per hour?
tbd
____________ is the mainstay of treatment for patients who are mildly or moderately dehydrated.
_____________ is recommended for patients who are severely dehydrated.
oral rehydration therapy (ORT) is the mainstay of treatment for patients who are mildly or moderately dehydrated.
note: ORT is not like soda or juice but fluid with Na+, Glu, etc.
IV replacement therapy is recommended for patients who are severely dehydrated.
Be able to solve problems using the % dehydration equation:
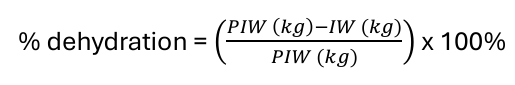
PIW= pre-illness weight
IW= illness weight
EQUATION GIVEN ON EXAM
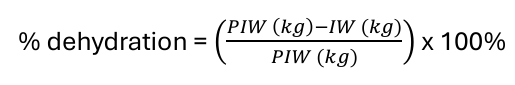
PIW= pre-illness weight
IW= illness weight
EQUATION GIVEN ON EXAM
Be able to solve problems using the total fluid deficit(TDF) equation:
TDF (mL) = (% dehydration)(weight kg)(1,000 mL/kg)
EQUATION GIVEN ON EXAM
TDF (mL) = (% dehydration)(weight kg)(1,000 mL/kg)
EQUATION GIVEN ON EXAM
There are 3 types of dehydration—>isonatremic, hypernatremic, and hyponatremic.
describe the serum Na+ levels of each.
iso: serum Na+ 130-150 mEq/L
hyper: serum Na+ >150 mEq/L
hypo: serum Na+ <130 mEq/L
Describe phase I, II and III of isonatremic dehydration:
Phase I: Rapid Phase
mild/mod: 20ml/kg bolus over 30-60min
severe: may repeat bolus
fluids: NS or LR
goal: restore circulation, re-perfuse brain/kidneys
Phase II: Replacement Phase
fluid type: D5W ½ NS or NS (±20 mEq KCl if voided)
amount: ½ deficit + 1/3 daily maintenance
time: 8 hrs
goal: replace deficit of fluids and electrolytes
Phase III: Stabilization Phase
fluids: D5W ½ NS or NS + 20 mEq KCl
amount: ½ deficit + 2/3 daily maintenance
time: >16 hours
goal: transition to maintenance fluids
The 3 phases of tx for isonatremic is similar to hypernatremic except for…
in hyper we treat slower
phase II: over 24 hrs
phase III: over 24-48 hrs
For hypernatremic dehydration, what is the maximum recommended Na⁺ correction rate?
No more than 10–12 mEq/L per 24 hours
Acute severe hyponatremia is a serum Na+ <____ mEq/L and causes what symptoms?
<120 mEq/L, CNS symptoms
What is the tx for acute severe hyponatremia?
fluid
how must it be infused?
bolus
what must be monitored?
Na+ deficit
max correction rate?
fluid:
administer 3% saline
MUST BE INFUSED VIA CENTRAL LINE
bolus
2-5 ml/kg over 20 minutes
monitor serum sodium 20 minutes after dose
can repeat up to 2 times
Na+ deficit
max correction rate: 0.5 mEq/L/hr or 10 mEq/L/24 hrs
What complication prompted ISMP’s warning about hypotonic fluids in 2009?
Hospital-acquired hyponatremia leading to neurologic dysfunction and deaths
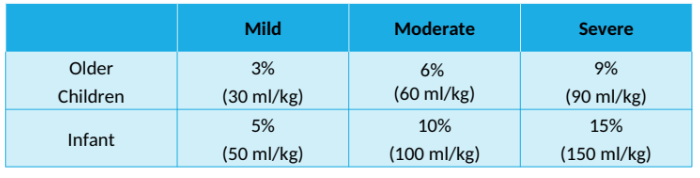
What are the degrees of dehydration?
A 10 kg patient presents with a 1-day history of vomiting and diarrhea. Serum sodium is within normal range. Based on symptoms he is 8% dehydrated. He received two 20 mL/kg boluses in the ER. Calculate the amount of fluid to be given the first 8 hours for the remaining deficit plus maintenance and the fluid to be given in the following 16 hours for the remaining deficit plus maintenance.