Psychopathology Exam 3 Study Set
1/103
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
104 Terms
What is the official definition of a mood disorder?
A group of mental health conditions characterized by persistent changes in mood, emotions, and behavior
Criteria sets for mood disorders require the presence of at least one mood episode. What are the mood episodes?
Major Depressive Episode
Manic Episode
Hypomanic Episode
What are the types of mood disorders?
Unipolar
Bipolar
What disorders fall under Unipolar?
Major Depression
Dysthymia
What disorders fall under Bipolar?
Bipolar 1
Bipolar 2
Cyclothymia
Major Depressive Episode (MDE) needs at least 5 of the following symptoms…
Depressed mood
Anhedonia
Appetite or weight changes
Sleep problems
Psychomotor changes
Loss of energy
Feelings of worthlessness or Inappropriate guilt
Concentration problems
Suicidal thoughts
What is Major Depressive Disorder?
Presence of a major depressive episode
Not better accounted for by another disorder
No history of a manic, mixed, or hypomanic episode
What is Persistent Depressive Disorder?
More chronic (can be less severe)
Depressed mood most of the day, more days than not, for 2 years
At least 2 of the following for at least 2 years
Appetite problems
Sleep problems
Low energy
Low self-esteem
Poor concentration
Feelings of hopelessness
What is the difference between Major Depressive Disorder and Persistent Depressive Disorder?
Major Depressive Disorder = depressed mood everyday for a short period of time
Persistent Depressive Disorder = depressed mood almost everyday, but not, for a long period of time
(LOOK AT SLIDES FOR GRAPH COMPARISON)
Major Depressive Disorder: Course & Prevalence
MDE last 6-9 months after no treatment
12 month prevalence of MDD is 7%
Ages 18-29 have 3x higher prevalence than ages 60+
~50% people will have recurrent MDE
Women 2x more common than men
Gender differences don’t emerge til puberty
Increase mortality (not just from suicide)
What is Seasonal Affective Disorder?
Major Depressive Episodes occur in a seasonal pattern
MDE starts same time every year
MDE ends same time every year
What is Premenstrual Dysphoric Disorder?
Symptoms appear the week before menstruation & improve during menstruation
5 symptoms total
One must be:
marked affective lability
marked irritability
marked depressive mood
marked anxiety
One must also be:
decreased interest
difficulty concentrating
lethargy
marked change in appetite
hypersomnia or insomnia
feeling overwhelmed
physical symptoms
Must be assessed prospectively
What are the biological theories of depression?
Genetics
Monamine theory of depression
Hypothalamic-Pituitary-Adrenal-Axis (HPA axis)
What are the GENETIC biological theories of depression?
If blood relatives have depression, then 2x more likely the person will have depression
Twin studies = 31-42% heritability
More severe, early onset, & recurrent depression = 70-80% higher heritability rate
Specific genes? - serotonin transporter gene (5HTTLP-R)
What are the MONAMINE biological theories of depression?
Depletion of serotonin & norepinephrine caused depression
We no longer think this is true
Limited evidence that serotonin is suppressed or low in people with depression; norepinephrine might actually be high for people with depression
Working hypothesis: complex interactions of neurotransmitters
What are the HPA biological theories of depression?
Activation ultimately releases cortisol
Depression associated with increased reactivity & failure of feedback mechanisms to turn the HPA axis “off”
Increased cortisol levels linked to memory impairments via damage to the hippocampus
Asymmetry in activity of the prefrontal cortex
Risk factor → predicts onset of first episode of depression
Smaller hippocampus
Important to memory
Low activation of the anterior cingulate cortex (acc)
Important in selective attention
Increased activation of the amygdala
Important for threat protection
What is the risk factor for asymmetry in activity of the prefrontal cortex?
Risk factor → predicts onset of first episode of depression
A smaller hippocampus is important to…?
Memory
Low activation in the anterior cingulate cortex (acc) is important to…?
Selective attention
Increased activation of the amygdala is important for…?
Threat protection
What are the psychological/behavioral/cognitive theories of depression?
Stressful life events
Developed depression = might have worsened problem solving skills
History of MDE = possibly sensitized to have more a response to less stressful event
May generate more stressful life events
Reduced positive reinforcers
Learn helplessness/hopelessness theories
What could be the possible learned helplessness/hopelessness theories?
Unpredictable negative events serve as punishers → cause behavioral withdrawal
Pessimistic attributional style → attributions that negative event was internal, stable, & global may underlie this effect
Response to rejection: “It’s my fault”, “Something has always been wrong with me”, “Nothing about me is likable”
Hopelessness relates to the stable part
Gender differences in depression rates = b/c women tend to be more likely to experience uncontrollable negative life events
What is the cognitive model of depression?
Internal (e.g. “It must be my fault”)
Stable (e.g. “I won’t ever be able to change”)
Global (e.g. “Nothing will work out for me”)
What the the cognitive (only) theories of depression?
Negative Cognitive Triad
Self (I’m incompetent and undeserving)
World (The world is hostile)
Future (I will always be in emotional pain)
Negative beliefs & schemas are developed in childhood & “latent” until activated by a stressful life event
Cognitive biases change people perception of the world & interpretation of events around them
What are the interpersonal theories of depression?
Rejection sensitivity
Excessive reassurance seeking
Both could lead to more stress being generated
What is Rumination?
Repetitive and relatively passive mental activity
What are the biological treatments for depression?
Monamine Oxidase Inhibitors (MAOIs)
Tricyclic antidepressants
Selective Serotonin Re-uptake Inhibitors (SSRIs)
Selective Serotonin and Norepinephrine Re-uptake Inhibitors (SSNRIs)
Electroconvulsive therapy (ECT)
Transcranial Magnetic Stimulation (TMS)
Deep brain stimulation
Light therapy
How long does it take for pharmacological treatments to have effect?
3-5 weeks
What is the relapse rate during the maintenance phase?
About 25%
6-9 months to relapse
Pharmacological treatments are more effective for _____ depression, and are less effective for _____ & _____ depression.
severe; mild; moderate
What are the problems with Monoamine Oxidase Inhibitors (MAOIs)?
Dangerous + potentially fatal interactions with other medications and certain foods
What are the problems with Tricyclic antidepressants?
Only about 50% have clinically significant improvement
Unpleasant side effects
Higher toxicity
What are the facts with Selective Serotonin Re-uptake Inhibitors (SSRIs)?
Relief within a couple of weeks
Side effects better tolerated, but can be unpleasant (sexual side effects, insomnia, GI distress)
Equally (or maybe less) effect that tricylic antidepressants
What are the fact(s) with Selective Serotonin and Norepinephrine Re-uptake Inhibitors (SSNRIs)?
Similar advantages as SSRIs, but has more stimulant effects
What is Electroconvulsive therapy (ECT)?
brief seizures
treatment-resisted major depression disorder (MDD)
memory loss
high relapse rate
What is Transcranial Magnetic Stimulation (TMS)?
noninvasive brain stimulation with electromagnet
treatment-resistant depression
Small effects? 14% remitted with rTMS compared to 5% in placebo
What is deep brain stimulation?
electrodes placed within brain
under investigation for intractable depression
infection risk
What is light therapy used for?
Seasonal Affective Disorder
What are the psychological treatments for depression?
Behavioral activation
Cognitive therapy
Interpersonal therapy (IPT)
What is behavioral activation for psychological treatments?
targeting positive reinforcers
schedule enjoyable and meaningful activities
What is cognitive therapy for psychological treatments?
identify maladaptive beliefs or thinking traps
challenge thoughts/core beliefs
often includes some behavioral activation (CBT)
What is interpersonal therapy (IPT) for psychological treatments?
Goal: Identify & address 1 of 4 interpersonal sources of depression.
grief, loss
interpersonal role disputes
role transitions
interpersonal skill deficits
What is the success difference between medication & therapy for treatment of depression?
Therapy has less relapse than medication.
What is a Manic Episode?
distinct period of elevated or irritable mood for at least 1 week
marked impairment
often results in hospitalization
can have psychotic symptoms
grandiosity
talkativeness
distractibility
racing thoughts
reduced need for sleep
impulsive activities
increased goal directed activity
What is a Hypomanic Episode?
distinct period of elevated mood or irritability for a least 4 days
some impairment, but not marked
no psychotic symptoms
no hospitalization
What is Bipolar 1?
marked impairment or hospitalization required
episodes at least 7 days
Major Depressive Episodes = NO
Full Manic Episodes = YES
Hypomanic Episodes = OK
What is Bipolar 2?
no marked impairment or hospitalization required
episodes at least 4 days
present depressive episode
Major Depressive Episodes = YES
Full Manic Episodes = NO
Hypomanic Episodes = YES
What is Cyclothymia?
Cyclical mood changes between high & low over a 2 year period
No manic, hypomanic, or major depressive disorder
Potentially a precursor to Bipolar 1 or Bipolar 2
What is a Mixed Episode?
meets criteria for a manic & major depressive disorder
duration of at least 1 week
present in at least ¼ of patients w/ bipolar 1
associated w/ a worse course
What is the lifetime prevalence for Bipolar 1 & Bipolar 2?
Bipolar 1: 1%
Bipolar 2: 2-3%
What is the onset for Bipolar Disorder?
Late adolescent & Early adulthood
Bipolar 2 has an _____ onset, _____ depressive episodes, & _____ risk of suicide than Bipolar 1.
earlier; more; greater
What is the gender prevalence for Bipolar Disorders?
No gender differences in prevalence
What is the cycle of episodes for Bipolar Disorders?
4 episodes in a year
What is the heritability/genetic theories for Bipolar Disorders?
1st degree relative of someone w/ Bipolar 1, then 8-10x more likely to have bipolar disorder
Heritability = 60-90%
Shared & unique genetic factors for Bipolar 1 & Bipolar 2
Bipolar 1 is more strongly genetically related to schizophrenia than Bipolar 2
What is the Neurotransmitter & Hormone theories for Bipolar Disorders?
Serotonin may be low during both depressive & manic episodes
During manic episodes there may be an increase in Norepinephrine & Dopamine
HPA axis dysregulated during depressive episodes/ when remitted from depressive episodes
HPA axis dysregulation may be decreased during manic episodes
What is the difference between depression & manic episodes?
Activity in the prefrontal cortex decreased during depressive state, increased during manic state.
What regions of the brain increase in activity?
Emotional Processing from the thalamus & amygdala.
Why are there disruptions in circadian rhythms in Bipolar Disorder?
Sensitive to circadian rhythm disruptions
More likely to have evening chronotype
Some evidence problems in sleep entrainment/regulating wakefulness
Sleep disruption predicts manic episode onset for some
What are the psychosocial theories of Bipolar Disorder?
Positive or negative stressful life events predict episodes
Perhaps by changing biological rhythms?
Poorer social support linked to worse outcomes
Increased sensitivity to reward
Difficulty regulating responses/emotions to reward and goal-related events
Set more ambitious goals
Positive life events predict mania onset
What are the biological treatments for Bipolar Disorder?
Lithium
Anticonvulsants
Atypical Antipsychotics
Antidepressants might increase manic epsiodes in those with bipolar disorder
Patient often remain on medication to prevent recurrence.
What are the psychological treatments for Bipolar Disorder?
Interpersonal and Social Rhythm Therapy
Combine interpersonal and behavioral techniques to helpmaintain routine
Cognitive Behavioral Therapy
Address problematic cognitions to reduce vulnerability todepression and mania
Self-referential, positive cognitions
e.g., “I feel good, I must be GREAT.”
Suicide vs. Self-harm:
Self-inflicted Unintentional Death
Outcome = Fatal injury
Intent = No intent to die
Suicide vs. Self-harm:
Death by Suicide
Outcome = Fatal injury
Intent = Intent to die
Suicide vs. Self-harm:
Self-harm (NSSI)
Outcome = Non-fatal injury or no injury
Intent = No intent to die
Suicide vs. Self-harm:
Suicide Attempt
Outcome = Non-fatal injury or no injury
Intent = Intent to die
Suicide rates _____ by 37% between 2000-2018 & _____ by 5% between 2018-2020. However, rates returned to their peak in _____.
increased; decreased; 2022
What are the most common methods in attempts in suicide?
Firearms
Suffocation
Poisoning
Other
What is the ratio of suicidal attempts by gender?
3:1
(women:men)
What is the ratio of suicidal deaths by gender?
4:1
(men:women)
What age group was their an increase in suicidal ideation?
Adolescents
What are the top 5 risk factors for suicidal ideation?
Prior suicidal ideation
Hopelessness
Depression diagnosis
Abuse history (any kind)
Anxiety diagnosis
What are the top 4 risk factors for suicide attempts?
Prior non-suicidal self-injury
Prior suicide attempt
Personality disorder
Prior psychiatric hospitalization
What are the top 5 risk factors for death by suicide?
Prior psychiatric hospitalization
Prior suicide attempt
Prior suicide ideation
Lower socioeconomic status
Stressful life events
What are additional risk factors for suicide?
Genetics
Low serotonin levels (independent of psychiatric diagnosis)
Psychache
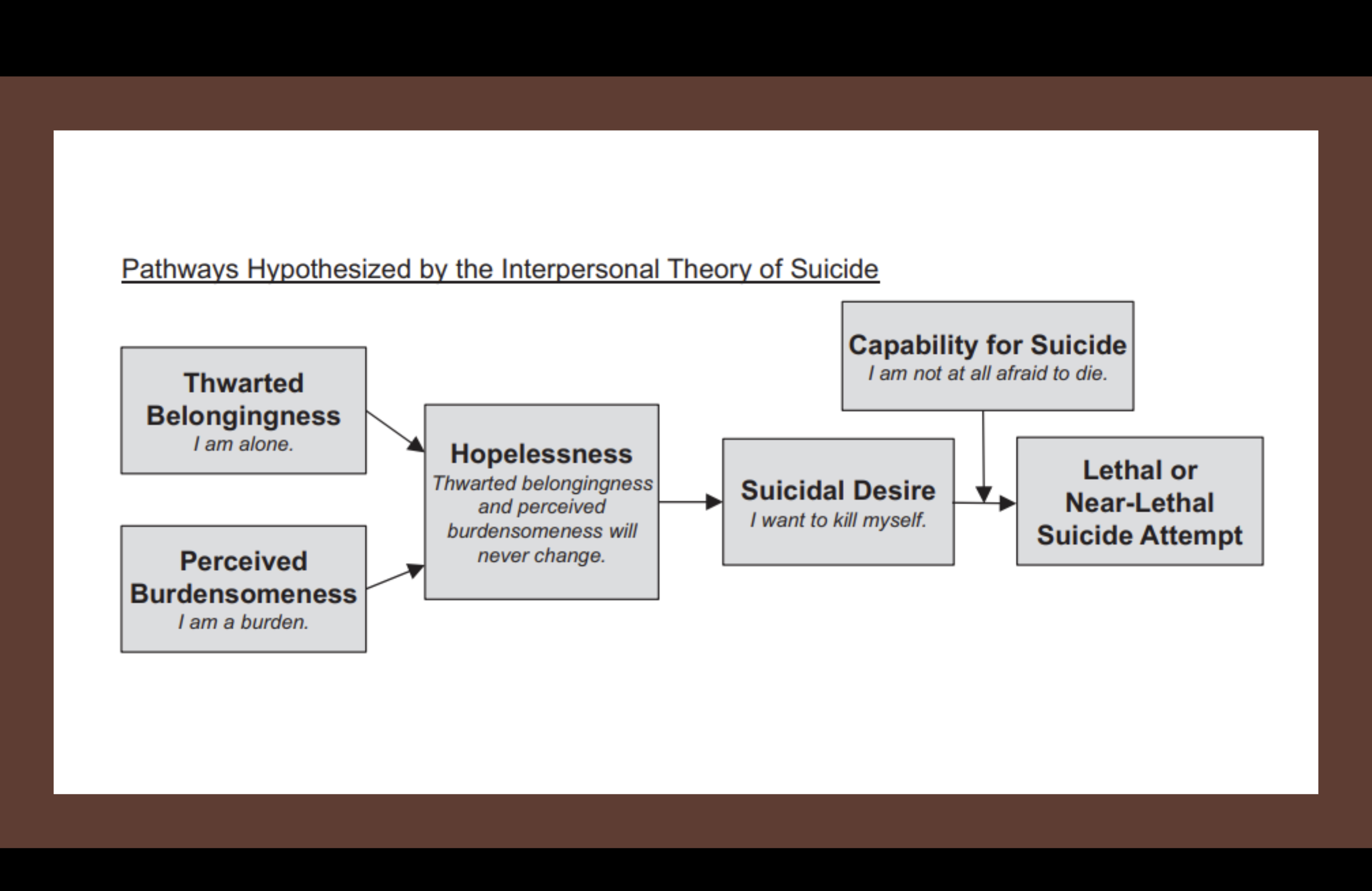
What is the interpersonal theory of suicide?
What are the treatments & preventions for suicide?
Interpersonal Therapy
Crisis intervention
Addressing underlying concerns
What is interpersonal therapy for suicide treatments & preventions?
Decrease burdensomeness and increase belongingness
Interpersonal coping skills
Challenging distorted beliefs
Activities that foster connectedness, effectiveness, & feelings ofself-efficacy
What is the crisis intervention for suicide treatments & preventions?
Hospitalization (stabilization)
Suicide Hotlines
Means safety/restriction
What is a social issue that leads to suicide?
Access to Guns
What is the definition of a personality?
styles of thinking, feeling, & behaving that make each of us unique.
includes sense of self & how you relate to others
What are the Big 5 Personality Traits?
O - Openness
C - Conscientiousness
E - Extroversion
A - Agreeableness
N - Neuroticism
What are the facets of Openness?
Fantasy
Aesthetics
Feelings
Actions
Ideas
Values
What are facets of Conscientiousness?
Competence
Order
Dutifulness
Achievement Striving
Self Discipline
Deliberation
What are facets of Extroversion?
Warmth
Gregariousness
Assertiveness
Activity
Excitement Seeking
Positive Emotion
What are facets of Agreeableness?
Trust
Straightforwardness
Altruism
Compliance
Modesty
Tendermindedness
What are facets of Neuroticism?
Anxiety
Hostility
Depression
Self consciousness
Impulsiveness
Vulnerability to stress
What is Personality Disorder?
A long standing pattern of problematic attitudes, thoughts, & feelings
onset in adolescents/early adulthood
Can affect relationships, identity, &/or behavior
Present in a variety of contexts
Ex: romantic relationships, work settings, friendships
Causes significant functional impairment or distress
Sometimes referred to as “Axis 2”
What makes people want to seek treatment for personality disorder?
Comorbid Psychopathology
Romantic relationship at a breaking point
Vocational problems
Arrested or Hospitalized
What are the Personality Disorder Clusters?
Cluster A: odd/eccentric
Cluster B: dramatic/emotional
Cluster C: anxious/fearful
What is Cluster A Personality Disorder
Odd/Eccentric
unusual behaviors or perceptual experiences
sub-threshold psychotic symptoms
no full-blown psychosis, delusions, hallucinations
What are the Cluster A Personality Disorders?
Paranoid Personality Disorder
Schizoid Personality Disorder
Schizotypal Personality Disorder
What is Paranoid Personality Disorder?
mistrust & suspiciousness of others
motives interpreted as malevolent
may accuse others of mistreating them
What is the prevalence & course of Paranoid Personality Disorder?
2-4% of general population
In treatment, 3x more likely in men than women
Chronic cause
Transient psychotic symptoms (minutes or hours)
Often comorbid with other disorders
What are the theories of Paranoid Personality Disorder?
Biology: Moderate heritability
Environmental: Parental neglect/abuse may increase risk.
Cognitive: Maladaptive beliefs that others are malevolent & deceptive
Describe the biological theory of Paranoid Personality Disorder.
Moderate heritability
somewhat more common for folks with family history of schizophrenia, although data are mixed
Describe the environmental theory of Paranoid Personality Disorder.
Parental neglect/abuse may increase risk
traumatic brain injury and chronic cocaine use may increase risk