Eicosanoid Drugs and their Signaling
1/64
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
65 Terms
List Prostaglandins That Signal the Reproductive Tract
Misoprostol
Dinoprostol
Alprostadil
Carboprost thromethamine
List Prostaglandins That Signal the Glaucoma
Lantanoprost (Xalantan)
Bimatoprost (Lumigan)
Travoprost
Unoprostone
List Prostaglandins That Signal GI cytoprotection
Misoprostol
List Prostaglandins That Signal the Pulmonary Hypertension
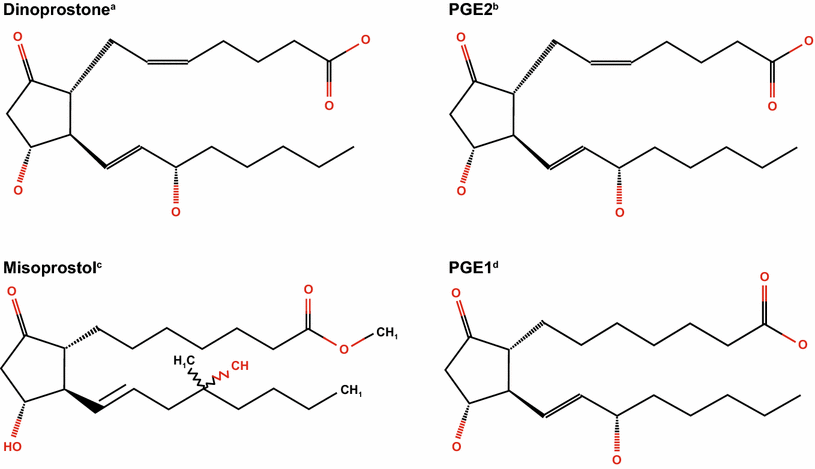
Iloprost
Treprostinil
Epoprostenol
List Prostaglandins That Signal the Ductus Arteriosus
Alprostidil
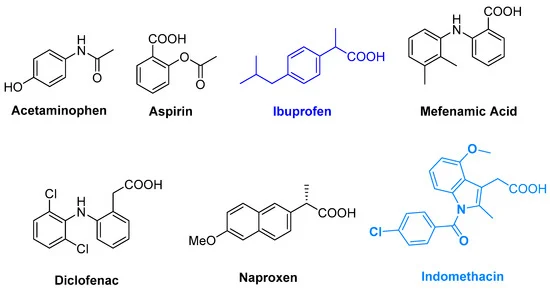
List NSAIDs and their indications
Ibuprofen, Naproxen, ASA, and indomethacin
Indications;
Anti- inflammatory
Analgesic
Antipyretic
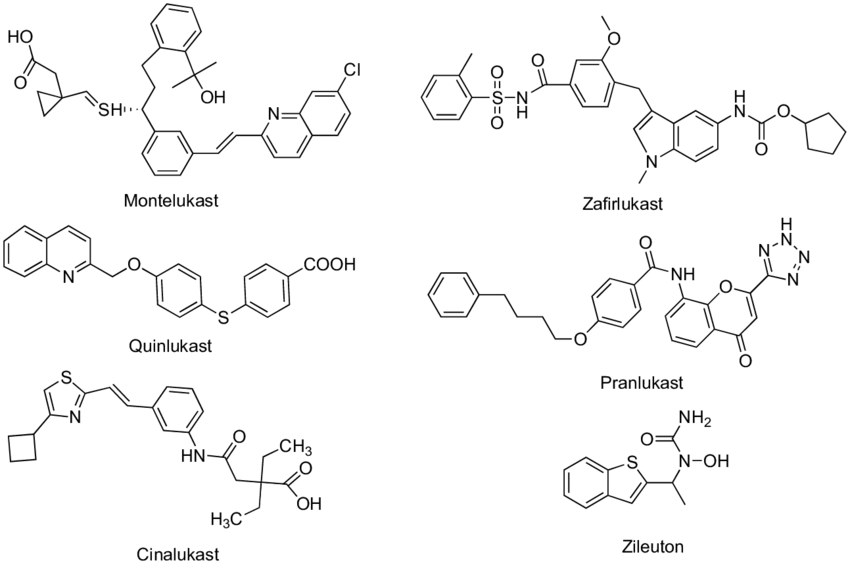
List Leukotrienene antagonist and their indications
Montelukast (Singulair)
Zafirlukast
Indication: Asthma
What’s an eicosanoid? What does it derive from? What is it’s main therapeutic function.
Lipid autocoid mediator ( or “ signaling Molecule”)derived from arachidonic acid.
Their main function is in the VASCULAR SYSTEM, regulating;
Vasoconstriction
Platelet Function
Capillary Permeability
Renal Function
Of course, Eicosanoids are also contributed to INFLAMMATORY RESPONSES
Chemotaxis
Immune Cell Actvation
GI Secretion
EYE Secretion
And our NERVOUS SYSTEM;
Fever ( CNS)
Pain Sensitivity. ( Both in central and peripheral)
List some pathological involvements eicosanoid can intervene with.
Asthma
Arthritis
Artherosclerosis
Thrombosis
Fever
Cancer
Chronic Inflammation
Etc.
What is the pathway of eicosanoid synthesis we DO NOT manipulate? Why?
P450 pathway; Cytochrome P450’s metabolize almost everything, so if we were t manipulate that pathway, we would be interfering with so many other processing that may not have favorable outcomes.
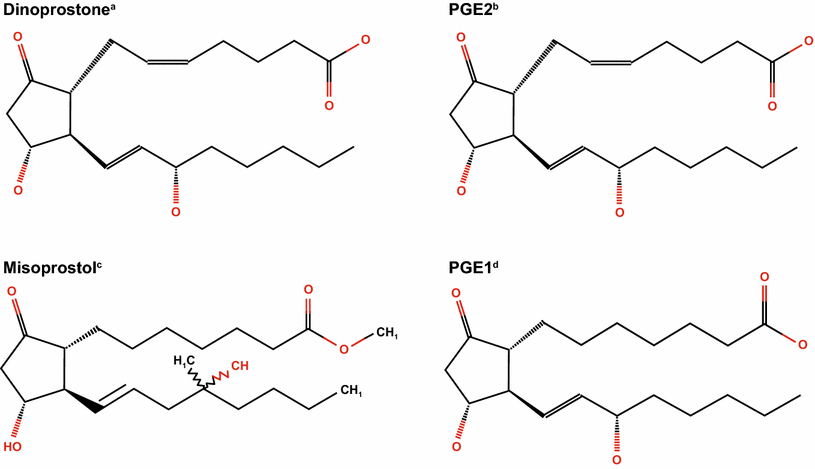
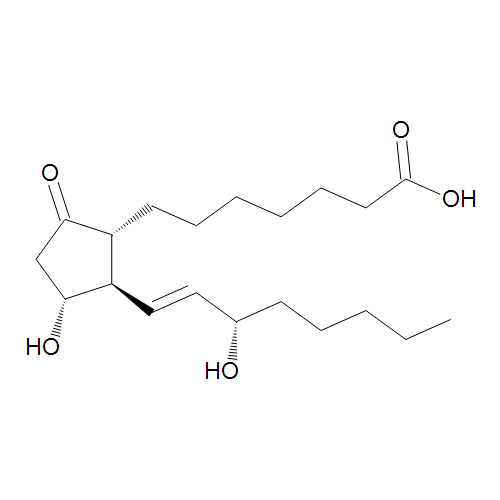
Describe the pathway of eicosanoid synthesis to produce specific Prostaglandins.
Arachidonic Acid is pulling from the cellular membrane to mediate an inflammatory Respinonse; the Enzyme to initiate this “ pulling” is phospholipase A2 or PL-A2.
Once the Acid is released, it can undergo the prostaglandin pathway or the Leukotriene pathway.
The Prostaglandin Pathways is Triggered by the Cyclooxyrgenase enzymes ( COX1/2) to produce Prostaglandin H2 or “PgH2”
The function of PgH2 now depends on the location:
If it’s effected directly on the platelets entering the hepatic portal vein, it will produce Thromboxane or "TxA2" to promote platelet aggregation and VC.
If PgH2 acts in the endothelium, it promotes prostacyclin which is the exact opposite of Thromboxane, promoting VD and platelet anti-coagulation.
If PgH2 acts in the gastric mucosa, it supports mucus production and cytoprotection.
T/F ASA is an irreversible inhibitor to TXA.
T
Describe the pathway of eicosanoid synthesis to produce specific Leukotrienes
Arachidonic Acid is pulling from the cellular membrane to mediate an inflammatory Response; the Enzyme to initiate this “ pulling” is phospholipase A2 or PL-A2.
Once the Acid is released, it can undergo the prostaglandin pathway or the Leukotriene pathway.
For the Lueukotriene pathway, the released Arachidonic Acid is metabolized by Lipoxygenase enzymes (LOX) to produce Leukotriene A4 (LTA4), which can further be converted into other leukotrienes like LTC4, LTD4, and LTE4, all of which are involved in mediating inflammatory responses that promote bronchoconstriction.
Dramamine is the _____ of Benadryl
Salt ( Diphenhydramate); Benadryl ( Diphenhyramine)
What is the only antihistamine drug that undergoes extensive metabolism in the liver?
Claritin
What enzyme degrades TxB2?
Prostaglandin (“11-hydro-TXB2”) dehydrogenase
What is the mechanism that Phospholipase A2 does to Arachidonic Acid?
Hydrolysis
List the degradation steps for PGE2
Prostaglandin Dehydrogenase
Reduction/ Beta-Oxidation/ Oxidation ( depends on the location)
What’s the enzyme that mediates the degradation for PGD2?
11- keto reductase
What does DP1-2 mean?
Prostaglandin D receptors 1 & 2
What does EP1-4 mean?
Prostaglandin E receptors 1-4
What does IP mean?
Prostaglandin I receptors or Prostacyclin
What does TPa,b mean?
Thromboxane receptor
What does BLT1-2 mean?
B Leukotriene receptors 1-2
What does CysLT mean?
Cysteinyl Leukotriene receptors 1 & 2
List the prostaglandin receptors that initiate a relaxant response.
IP- Prostacyclin Receptor ( I2)
EP2 - Prostaglandin E receptors 2
EP4 - Prostaglandin E receptor 4
DP1 - Prostaglandin D receptors 1
List the prostaglandin receptors that initiate a Contractile response
TP - Thromboxane receptors 1
EP1 - Prostaglandin E receptor 1
List the prostaglandin receptors that initiate an inhibitory response?
EP3 - Prostaglandin Receptor E 3
Name the Vascular Effects of the indicated Eicosanoid: TXA2
VC
Inducing platelets aggregation at low doses
Name the Vascular Effects of the indicated Eicosanoid: PGF2a
VC
Name the Vascular Effects of the indicated Eicosanoid: PGI2
VD
Inhibit platelet aggregation at high doses ( bind to IP)
Name the Vascular Effects of the indicated Eicosanoid: PGE2
VD
Induce platelet aggregation at low doses (EP3)
Inhibit platelet aggregation at high doses. (IP)
Name the Vascular Effects of the indicated Eicosanoid: PGD2
VD
Name the indicated Eicosanoid that mediates niacin-induced flushing
PGD2
Name the Vascular Effects of the indicated Eicosanoid:
Name the Vascular Effects of the indicated Eicosanoid: LTC4
Slow Hypotensive Effects:
decreased plasma volume
increased capillary permeability
Plasma exudation ( leakage)
What roles would each eicosanoid play?
PGI2:
Pulmonary Function
Uterine Contraction
Renal Perfusion ( GFR)
What roles would each eicosanoid play?
TXA2
Pulmonary Function
Uterine Contraction
Renal Perfusion ( GFR)
What roles would each eicosanoid play?
PGF2a:
Pulmonary Function
Uterine Contraction
Renal Perfusion ( GFR)
Decreased Pulmonary Function; Brochoconstriction
Increase Uterine Contraction
What roles would each eicosanoid play?
LTB4:
Pulmonary Function
Uterine Contraction
Renal Perfusion ( GFR)
-
List the Eicosanoids that will cause brochoconstricton
PGF2a
TXA2
CysLT
List the Eicosanoids that will cause Bronchorelaxation
PGI2
PGE2
List the Eicosanoids that will cause uterine contraction
PGF2a
TXA2
PGE2 @ low doses
List the Eicosanoids that will cause Uterine relaxation
PGE2 @ a high doses
PGI2
List the Eicosanoids that will cause increase GI motility
Prostanoids and Leukotrienes
List the Eicosanoids that will cause Chemotaxis
Leukotrienes, especially LTB4
List the Eicosanoids that will increase edema and leukocyte infiltration
PGE2
PGI2
List the Eicosanoids that will increase renal blood flow and cause renin excretion
PGE2
PGI2
List the Eicosanoids that will decrease renal blood flow and renin excretion
TXA1
List the Eicosanoids that will cause decrease intra-ocular pressure
PGF2a
List the Eicosanoids that will mediates pyrogenesis
PGE2
List the Eicosanoids that will sensitize peripheral nerve to pain sensation
PGE2 and PGI2 and LTB4
Glucocorticoids inhibit ______ activity, and block ___________
PLA2; prostaglandin synthesis
What;s a dietary modification to prostaglandin synthesis?
Replacing Arachidonic with Omega 3 Fatty Acids
Outline special populations for ASA
Those with asthma
Liver dysfunction
Under the age of 20
What’s an upside and downside to COX-2 selective drug
Decreases GI bleeding, increases cardiovascular issues like Myocardial Infarction, Angina, and Stroke
Prostanoids help maintain vasodilation of the _______ arteriole
afferent
What’s the lifetime of a platelet?
8 -12 days
The only direct antagonist for eicosanoids are_________
Leukotriene inhibitors
NSAID inhibit _________synthesis
Prostaglandin Synthesis
LOX inhibitors inhibit _______ synthesis
Leukotrienes