Session 10: Vaccinations
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
42 Terms
Active immunity
Protection produced by individual's own immune system and is usually long-lasting.
When body encounters antigen, the production of memory B and T cells allows protection against subsequent infection.
Active immune response can be triggered naturally or via vaccination.
Immunisation
Giving a vaccine that allows immunity to develop without exposure to the disease itself.
Process of inducing immunity to a disease
Immunisation can be obtained naturally, or by vaccination.
Features of a good vaccine
- Safe
- Few side effects
- Long lasting, appropriate protection
- Low in cost
- Stable with long shelf-life (no special storage required)
- Easy to administer
- Easy to store/transport
- Inexpensive
- Public must see more benefit than risk
Who should not be vaccinated
- Allergy
- Fever
- HIV infection
- Immunodeficiency e.g., cancer pts
- Neurological disorder
- Prematurity
- Reaction to previous vaccines
- Simultaneous administration of vaccines
- Thrombocytopenia
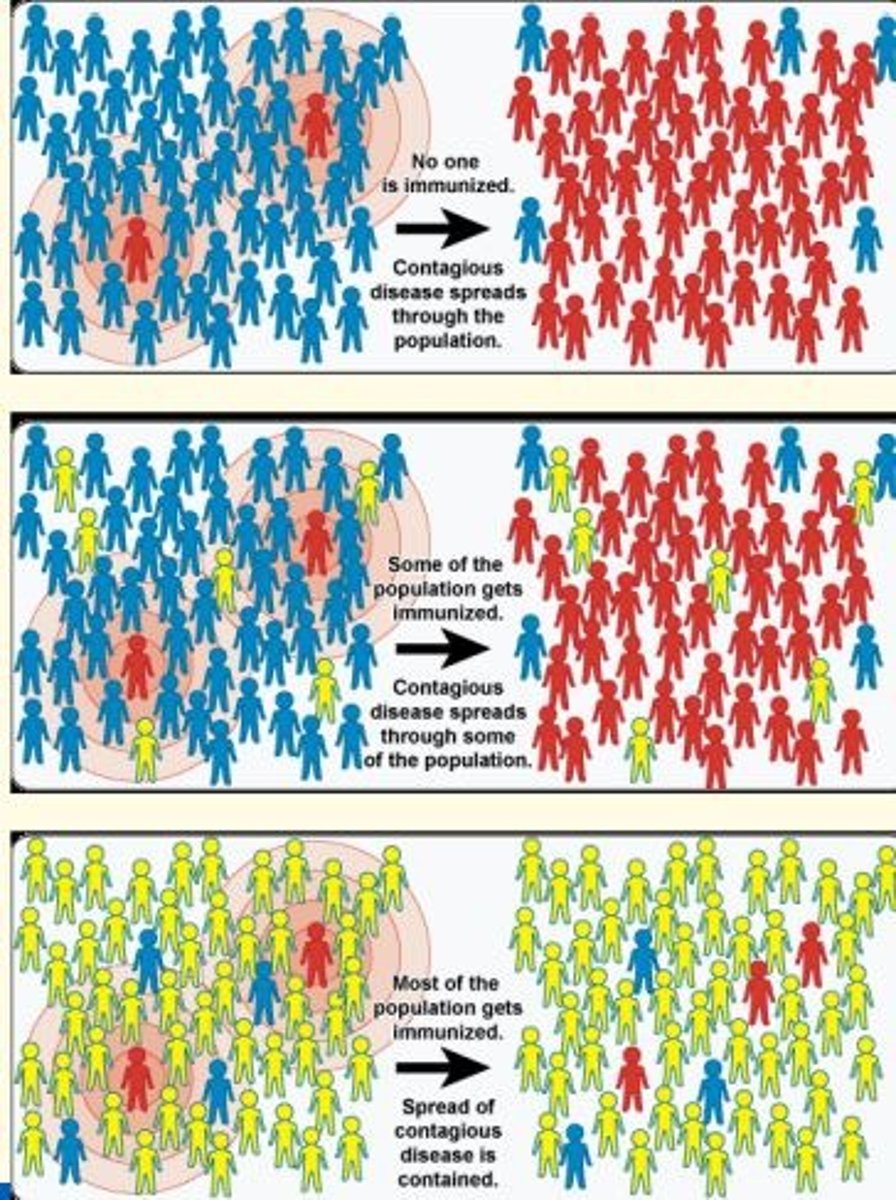
Herd immunity
The resistance to the spread of a contagious disease within a population that results if a sufficiently high proportion of individuals are immune to the disease, especially through vaccination.
This is achieved when immunisation programs reach sufficiently high coverage of target population to interrupt transmission in the community.
Herd immunity protects people who are unable to be vaccinated.
Herd immunity depends on...
- Vaccine efficacy
- Rates of transmission
- Length of protection
- Vulnerability of populations
- Environmental factors
What two prominent organisations are involved in vaccine distribution and global immunisation initiatives?
WHO
- Vaccine policy & guidance
- Vaccine research & development
- Vaccine procurement & distribution
- Technical support & capacity building
CDC
- Disease surveillance and outbreak response
- Immunisation recommendations & guidance
- Vaccine safety monitoring
- Vaccination coverage/education
- Global partnership & collaberation
Polio
Viral infection that may affect the spinal cord and cause muscle weakness and paralysis
Virus enters body via mouth, usually from hands contaminated of an infected person
Genus Enterovirus
Family Picornaviridae
Most virulent and common serotype of polio
P1
Inactive vaccines
Inactivated vaccines are produced when microorganisms have been killed by physical/chemical agents.
These vaccines are developed by treating microorganisms with heat, chemicals or radiation to render them incapable of causing disease, while still retaining ability to produce an immune response.
When introduced to the body, the inactivated pathogen or their components serve as antigens. The antigens are recognised by the immune system as foreign & trigger an immune response.
Once introduced into the body, they can cause an immune response, but the non-functional proteins cannot infect the cells.
Example
Inactivated polio vaccine (IPV) by Jonas Salk
How are inactivated vaccines produced?
1) Pathogen cultivation in lab under controlled conditions
2) Inactivation of pathogen by heat, chemicals or radiation. This disrupts pathogen's ability to replicate or cause disease while preserving its antigenic properties.
3) Vaccine formulation = inactivated pathogen is combined with other ingredients (stabilisers and adjuvants) to enhance immune response & improve efficacy of vaccine
4) Administration via injection (intramuscularly or subcutaneously). In some cases, boosters are needed to maintain immunity
Advantages and disadvantages of inactivated vaccines
Advantages
- Safe
- Cannot cause infection
- Good for immunocompromised patients (don't contain live pathogen)
Disadvantages
- May require boosters to maintain immunity
Other than the Inactivated Polio Vaccine (IPV) by Jonas Salk - what is the other vaccine produced for polio?
Sabin's attenuated oral polio vaccine (OPV)
Whole agent vaccines (attenuated)
Vaccine contains living, weakened (attenuated) pathogens
Designed to stimulate immune response similar to that of a natural infection - mild symptoms in vaccinated individuals.
Example
Sabin's Oral Polio Vaccine (OPV)
MMR
BCG
Mechanism of producing attenuated vaccines
Attenuation of viruses can be facilitated by passage through non-human cells...
1) Pathogenic virus isolated from patient, grown in human cells
2) Monkey cells are infected with cultured virus
3) Virus acquires many mutations that allow it to grow well in monkey cells. These mutations make the virus unable to grow well in human cells.
Advantages and disadvantages of attenuated vaccines
Advantages
- Strong, long-lasting immunity because vaccine contains live pathogens
- Single-dose efficacy (no need for boosters)
Disadvantages
- Potential to revert to virulent form and cause disease
- Unsuitable for immunocompromised patients (higher risk of causing disease in these individuals)
Toxoid vaccines
Type of vaccine that targets disease caused by bacterial endotoxins rather than the bacteria themselves.
Consist of exotoxins that have been inactivated (by heat or chemicals).
These vaccines produce immunity against TOXINS, but not the bacteria that produce the toxins.
Example
Whooping cough toxoid (Bordetella pertussis)
Diphtheria toxoid (Corynebacterium diphtheria)
Tetanus toxoid (Clostridium tetani)
Mechanism of toxoids vaccine
When person recieves toxoid vaccine, the inactivated toxoid is recognised as a foreign substance produced by the immune system.
This triggers the production of specific antibodies against the toxin.
These antibodies neutralise the toxin & prevent it from causing harm when the person is exposed to the disease-causing bacteria.
Immune response is generated by the toxoid vaccine, leading to the production of memory cells.
Advantages and disadvantages of toxoid vaccines
Advantages
- Compatability of toxoid vaccines with other vaccines. They can be combined with other vaccine components to create combined vaccines.
Disadvantages
- Limited protection = they do not provide protection against the bacteria producing the toxin, only the toxin.
- Multiple boosters/doses needed
- Potential side effects
- Limited efficacy against new toxin variants
Subunit vaccines
Subunit vaccines are made of only a fraction of the infectious agent (use antigenic fragments to stimulate an immune response).
Only a few proteins are used to make the subunit vaccine - no chance that the infection will occur.
Example
Hepatitis B vaccine (composed of only the surface proteins of Hep B)
Advantages and disadvantages of subunit vaccines
Advantages
- Safer (virus cannot reproduce because doesn't contain live components of pathogen)
Disadvantages
- Less effective than whole agent vaccines
- Can be costly
- Always requires boosters
Three types of subunit vaccine
1) Protein-based
2) Polysaccharide
3) Conjugate
Protein-based subunit vaccine
Contain specific isolated protein of pathogen
Disadvantage = if protein is denatured, the immune response may be inadequate
Examples
- Acellular pertussis vaccine
- Hepatitis B vaccine
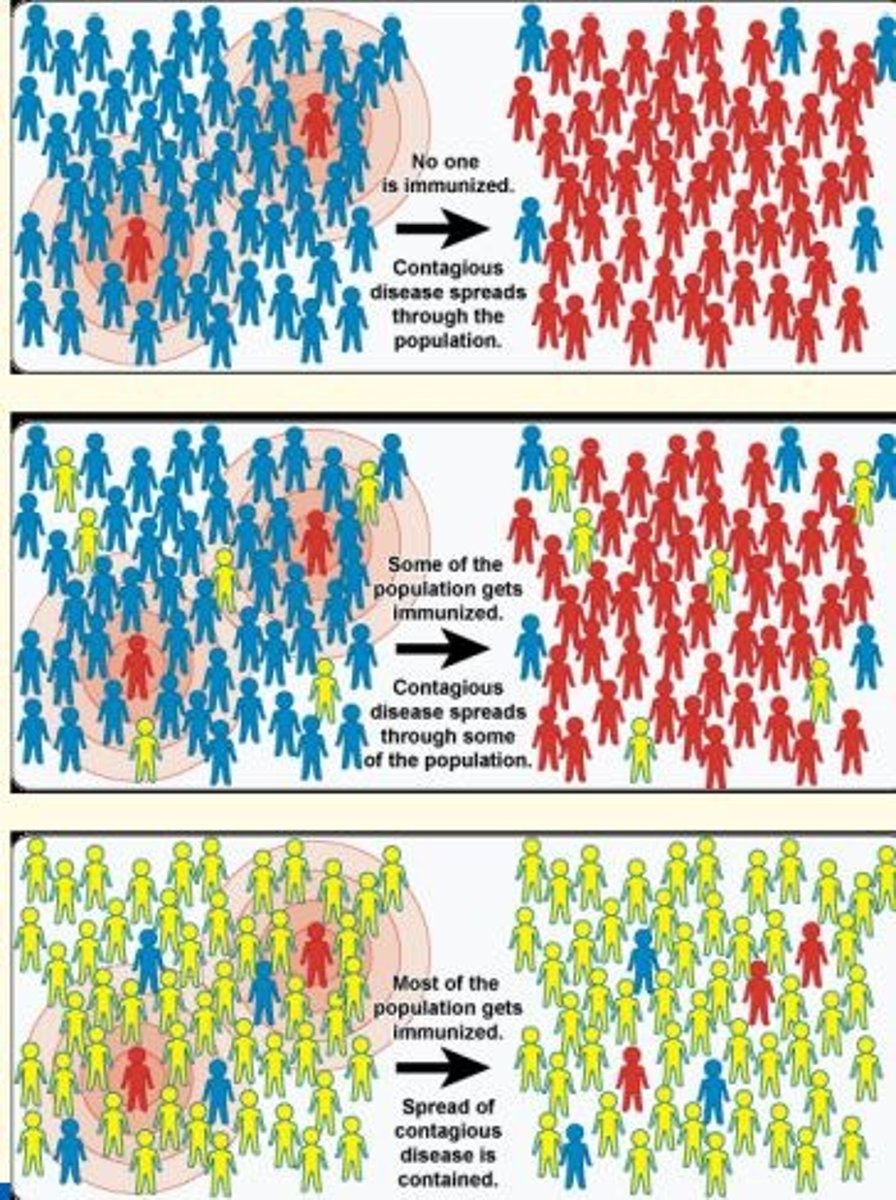
Polysaccharide subunit vaccine
Utilizes polysaccharide antigens from cell wall of bacteria.
Disadvantages
- T-cell independent (only B-cells stimulated)
- Poor immune response in <2 years of age
- Only provides short-term immunity
- No booster response even after repeated injections
Examples
- Typhoid Vi polysaccharide vaccine
- Pneumococcal polysaccharide vaccine
Conjugate subunit vaccine
Utilizes polysaccharide bound to carrier protein to induce long-term protection
Examples
- Pneumococcal Conjugate Vaccines (PCV-10, 13)
How can issues with subunit vaccines be overcome?
Multiple doses (booster shots)
Use of adjuvants given with vaccines to increase the efficacy of the vaccine
Adjuvant
A substance that enhances the body's immune response to an antigen.
Adjuvants are given together with vaccines to enhance the efficacy of the vaccine.
Vaccines prolong the stimulation of the immune response.
Adjuvants work by trapping the antigens in chemical complex & releasing them slowly.

Examples of adjuvants
Aluminum salts, monophosphoryl lipid A

Recombinant vaccines
Subunit vaccines that are produced using recombinant DNA technology (genetic modification).
Created by inserting specific genes from pathogens into another organism (e.g., yeast/bacteria) which then go on to produce the antigenic proteins of the pathogen.
These antigenic proteins trigger an immune response in the patient, leading to antibody production & development of immunity against the pathogen.
DNA vaccines
Microbial DNA is inserted into a plasmid vector (recombinant plasmid) and inoculated into a recipient
This creates a recombinant plasmid containing a gene which encodes a specific antigen.
Presenting of the antigen to T-cells provokes an immune response.
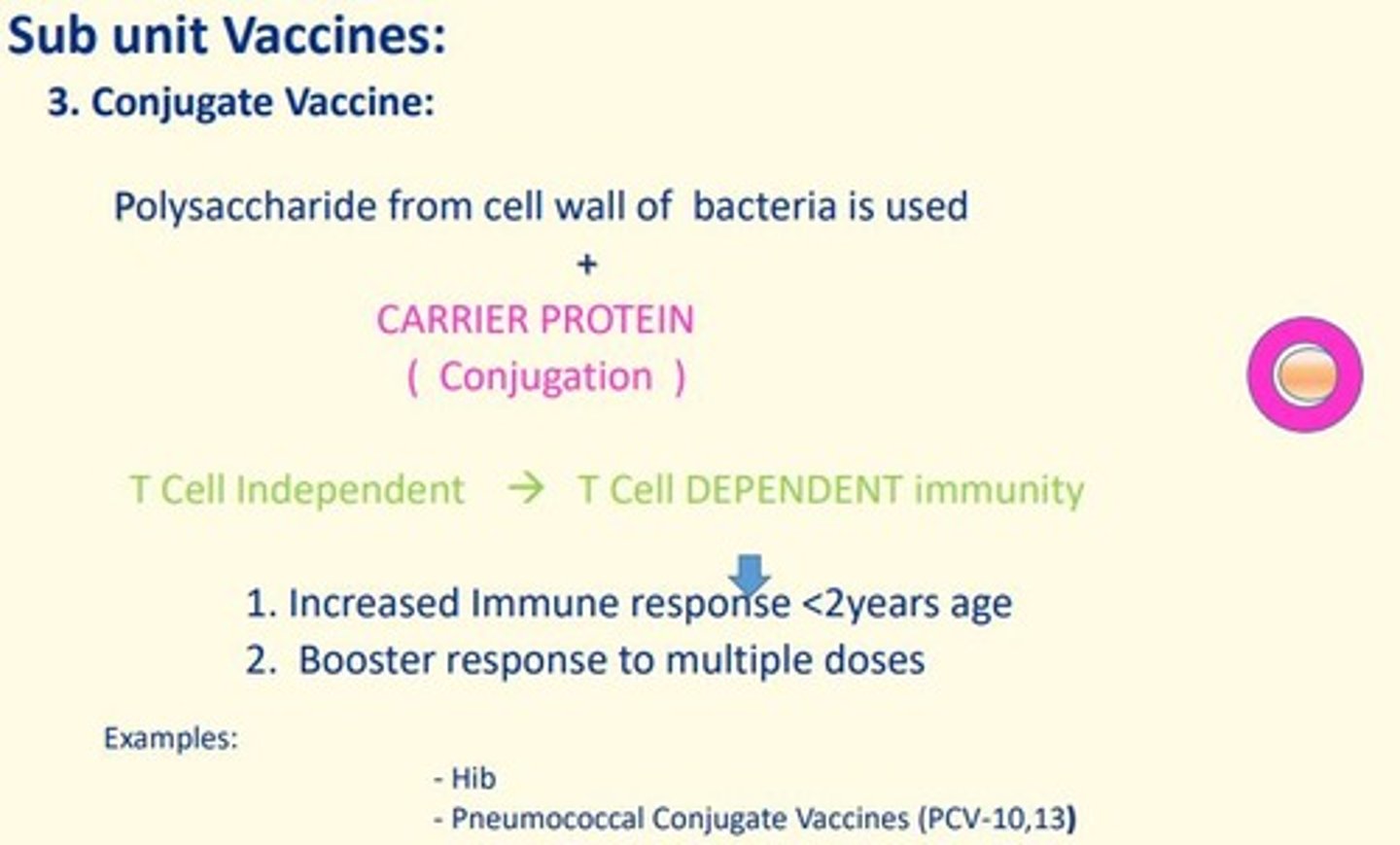
COVID-19 mRNA vaccine (Pifzer BioNtech)
mRNA vaccine
Contains genetic sequence (mRNA) for spike protein found on the surface of SARS-CoV-2 virus, wrapped in lipid envelope (nanoparticle) to allow it to be transported into cells in the body.
When injected, the mRNA is taken up by host cells which translate the genetic information and produce the spike proteins.
These spike proteins are then displayed on the surface of the cell. This stimulates an immune response to produce antibodies and activate T-cells which prepare immune system to respond to any future exposure to SARS-CoV-2 virus by binding to and disabling any virus encountered.
AstraZeneca COVID-19 vaccine
Viral vector vaccine which uses a weakened adenovirus as a carrier to deliver the SARS-CoV-2 antigen
Adenovirus has been modified so it cannot replicate in human cells (and cannot cause disease).
The genes that encode the spike protein on SARS-CoV-2 virus have been inserted into the adenovirus's genetic code to make the vaccine.
When the vaccine is injected, it enters the host's cells which then manufacture the spike protein.
This then stimulates the immune system which reacts by producing antibodies and memory cells to the SARS-CoV-2 virus without causing disease.
Advantages of recombinant vaccines
Recombinant vaccines are produced by using recombinant DNA technology.
- Produced quickly (and in large quantities) once gene is inserted into expression system
- They eliminate the need to cultivate the pathogen itself = reduce the risk of handling live pathogens
- Recombinant vaccines are safe and well tolerated as they do not contain live pathogens.
Routes of administration of vaccines
- Deep subcutaneous/intramuscular (most vaccines)
- Oral route (oral BCG)
- Intradermal route (BCG)
- Scarification (smallpox)
- Intranasal route (live attenuated influenza vaccine)
What is the importance of vaccines?
1) Disease prevention
2) Individual protection
3) Herd immunity
4) Eradication/elimination of disease e.g., smallpox
5) Public health and societal benefits = reduce burden on healthcare system, decrease healthcare costs & improve community wellbeing.
A patient’s pneumonia is to be treated with antibiotics with a quinolone. What is the mechanism of action of quinolone antibiotics?
Interference with separation of double-stranded DNA
Which are attenuated vaccines made from?
Live weakened bacteria
Which disease does the recombinant human papillomavirus vaccine offer protection?
Cervical cancer
Which is an advantage of live virus vaccines compared to inactivated vaccines?
Enhanced immune response
Which correctly defines an epitope?
Specific regions on antigens recognised by the immune system
What are possible complications for a pregnant woman of an untreated chlamydial infection?
Pelvic inflammatory disease (PID)
Reduced fertility
Ectopic pregnancy
Chronic pelvic pain
Reiter's reactive arthritis
Tubo-ovarian abscess
Adhesions
Perihepatitis
Salpingo-oophoritis
Hydrosalpinx
What possible problems could a neonate born to a woman with untreated chlamydial infection develop?
Premature birth
Conjunctivitis
Blindness
Pneumonia
Premature rupture of membranes
Low birth weight