Parathyroid Hormone, Calcitonin and vitamin D
1/40
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
41 Terms
What are the three hormones that regulate calcium and phosphate metabolism?
Calcitonin (from the thyroid)
Parathyroid hormone (PTH, from the parathyroid), and
1,25-dihydroxyvitamin D₃ (from the kidneys).
What are the main physiological roles of calcium in the body?What are the main physiological roles of calcium in the body?
Calcium is essential for building bones, blood clotting, muscle contractions, and heart function.
calcium is poorly absorbed from the intestinal tract, while phosphate is easily absorbed, except when calcium intake is excessive.
What effect does vitamin D have on calcium and phosphate absorption?
Vitamin D enhances absorption of calcium and phosphate from the gastrointestinal tract and affects bone deposition and resorption.
What form of vitamin D is biologically active in calcium regulation?
1,25-dihydroxycholecalciferol (also called 1,25-dihydroxyvitamin D₃), which is produced in the kidneys.
lipid soluble and promotes calcium and phosphate absorption.
it must be actived in the kidney for use.
What role does parathyroid hormone (PTH) play in the formation of 1,25-dihydroxycholecalciferol?
PTH is necessary for the formation of 1,25-dihydroxycholecalciferol, the active form of vitamin D that helps regulate calcium levels.
1,25-dihydroxycholecalciferol (the active form of vitamin D) increases calcium absorption from the intestines.
How does the body regulate calcium levels when plasma calcium concentration is too high?
Formation of 1,25-dihydroxycholecalciferol is downregulated to reduce calcium absorption from the intestines, bones, and kidneys, preventing further increase in blood calcium.
Mechanism of 1,25-dihydroxycholecalciferol in intestinal calcium absorption
It increases production of calcium-binding proteins and activates calcium transporters (like the Ca²⁺/ATPase pump) in intestinal cells, moving calcium into cells and then into the bloodstream by facilitated diffusion.
ultimately promoting calcium absorption
How is calcium concentration regulated in the blood?
Blood calcium is tightly regulated around 2.4 mMol/L, mainly by parathyroid hormone (PTH), which raises calcium levels.
What are the three forms of calcium in the blood and which is biologically active?
~1.0 mMol/L bound to plasma proteins (inactive, can't cross membranes)
~0.2 mMol/L unbound but non-ionized (diffusible but inactive)
~1.2 mMol/L ionized and free (diffusible and biologically active)
these make up the blood calcium 2.4
Relationship between PTH, vitamin D, and calcium absorption
PTH activates vitamin D to its active form, which increases calcium absorption in the intestines by boosting calcium transport proteins; high blood calcium reduces active vitamin D production to prevent excess absorption.
Why must calcium levels be tightly controlled in the body compared to phosphorus?
Calcium levels must be tightly controlled because both high and low calcium levels can cause serious effects, while changes in phosphorus usually don’t cause major problems.
What happens when calcium levels drop too low in humans?
Nerves become more excitable, causing uncontrollable muscle contractions or twitching, and if calcium drops to half normal, muscles can go into tetany (involuntary spasms).
How does low calcium cause increased nerve excitability and muscle spasms?
Normally, calcium controls how easily sodium enters nerve and muscle cells. Low calcium allows sodium to flow in more easily, triggering spontaneous action potentials and muscle contractions.
How does hypocalcemia typically present in cows compared to humans and dogs?
In cows, muscle twitching during hypocalcemia is brief or absent, and they usually develop paralysis instead of tetany.
this is because calcium is needed at the neuromusclar junction to trigger neurotransmitter release; without it, muscles lose their restign tone and become paralyzed.
What normally maintains muscle tone in voluntary muscles like skeletal muscles?
Signals from muscle spindles and brain pathways, especially the extrapyramidal tracts from the motor cortex.
Hypercalcemia
A condition with too much calcium in the blood, which slows the nervous system and heart function, causing delayed reflexes and disrupted normal brain activity due to impaired nerve cell repolarization (going back to being negative in cell)
How does high calcium affect the heart's function?
It prolongs the heart's action potentials, especially the plateau phase, delaying repolarization and potentially causing the heart to stop while contracted.
PTH, vitamin D and Calcitonin functions
What effect does abnormal increased activity of the parathyroid glands have?
It causes rapid absorption of calcium from bones, leading to hypercalcemia (high blood calcium).
if there is a defisicicy of PTH it results in hypocalcemia
Effect of PTH on phosphate levels
PTH decreases blood phosphate by increasing phosphate excretion in the kidneys, despite pulling phosphate from bones.
How does PTH affect osteoclasts and calcium levels in the blood?
PTH increases the number and activity of osteoclasts, which break down bone and release calcium and phosphate into the blood.
How does PTH normally work?
PTH usually works slowly by increasing the number and activity of osteoclasts, which are cells that break down bone and release calcium and phosphate into the blood. After osteoclasts weaken bone to break it down, osteoblasts (cells that build bone) are activated to repair it. However, PTH has a stronger effect on osteoclasts, so overall more bone is broken down than rebuilt, leading to bone demineralization.
What happens to bones when PTH activates both osteoclasts and osteoblasts?
Osteoblasts repair bone after osteoclasts break it down, but because PTH has a stronger effect on osteoclasts, more bone is broken down than rebuilt, leading to demineralization.
Osteolysis
A rapid, damaging release of calcium and phosphate from bone triggered by PTH; it's less understood but contributes to bone loss.
PTH and how kidneys handle ions
PTH it increases the absorption of magnesium and hydrogen ions, but decreases the resorption of sodium, potassium and amino acids by blocking their transport systems.
PTH and gut
PTH increases calcium and phosphate absorption from intestines by boostign kidney’s production of 1-25-dihydroxycholecalciferol (active form vitamin d)
vitamin D3 excess and in small amounts
In large amounts, it can cause bone breakdown, similar to excess PTH.
in small amounts, it helps build bone b increasing calcium and phosphate absopriton from the gut.
in small amounts it also helps bone mineralization deposition.
Control of PTH secretion by calcium ions
When calcium levels in the blood slightly drop the parathyroid glands respond by releasing more PTH. If low calcium levels continue for a long time, the glands enlarge (called hypertrophy) to keep up with the demand. This enlargement usually happens during pregnancy or breastfeeding when calcium levels are lower.
When calcium levels are too high - maybe when taking too much calcium or vitamin D or from lack of bone use leading to breakdown, the parathyroid glands reduce PTH secretion and may shrink (hypotrophy).
calcitonin
Calcitonin lowers blood calcium levels by reducing osteoclast activity, encouraging calcium to stay stored in bones.
in young animals t quickly reduces osteoclast activity and slows the formation of new osteoclasts, decreasing bone breakdown.
When is calcitonin released and how fast does it act?
Calcitonin is released when blood calcium rises and acts faster than PTH, creating a second feedback system for calcium regulation.
Role of Calcitonin vs. Parathyroid Hormone in Calcium Regulation
Despite its role, calcitonin is not the main long-term regulator; if the thyroid gland is removed, calcium levels stay normal due to PTH's dominant regulation.
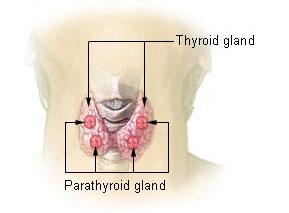
Paraythroid glands
parathyroid hormone (PTH) is produced by the parathyroid glands, which are separate small glands located behind or near the thyroid gland, not inside it.
- So even if the thyroid gland is removed, the parathyroid glands usually remain intact and keep producing PTH to regulate blood calcium levels
Hypoparathyroidism
Condition where parathyroid glands produce insufficient hormone, lowering blood calcium by reducing calcium release from bones.
Bone strength remains normal despite low blood calcium levels.
removed parathyroid gland leading to untreated hypoparathyroidism symptoms
Muscle spasms (tetany) and death due to low calcium.
Treating with actual PTH isn't ideal because it's expensive and the body can develop antibodies against it.
Instead patients are usually given very high doses of vitamin D (100000 units a day) and 1-2 grams of calcium a day to keep calcium levels in the normal range.
Hyperparathyroidism
Condition where parathyroid glands produce excess hormone, often due to tumor, leading too much calcium and phosphate levels decrease.
when its mild, the body builds bone fast enough to balance breakdown, but extra calcium and phosphate in the blood may cause kidney stones.
when its severe, Bone is broken down faster than rebuilt, leading to weak bones prone to fractures. Blood calcium becomes very high leading to slowed reflexes and heart problems.
Rickets
Childhood disease caused by vitamin D deficiency leading to low calcium and phosphate in blood, resulting in bone problems.
Role of parathyroid hormone in rickets
Maintains blood calcium by releasing calcium from bones but increases phosphate loss through urine.
Adult Rickets (Osteomalacia)
A bone disease in adults caused by vitamin D or calcium deficiency, often due to fat malabsorption.
vitamin D is fat soluble and is lost with fat in feces and calcium also lost bc it binds to unabsorbed fats
might be caused by too much castor oil intake
Renal rickets
Caused by long term kidney damage, the kidneys fail to produce the active form of vitamin D, which is needed for absorption of calcium and phosphate.
Osteoporosis
Happens when there is a loss of the bone's structural framework (the organic matrix) not because of problems with calcium levels, in this condition osteoblasts arent working as much as they should so new bone isnt made fast enough.
Causes of osteoporosis
lack of physical activity, poor nutrition (need more protein), vitamin C deficiency (needed for cells to make material between cells like bone), postmenopause (estrogen levels drop so less stimulation of osteoblasts), Aging (growth hormone declines), cushing’s disease (high levels of stress hormones reduce protein production and bran down existing protein)