Musculoskeletal Pathology
1/15
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
16 Terms
Systemic Lupus Erythematosus (SLE)
Define
Pathogenesis
Clinical Features
A multi-system inflammatory disease
Pathogenesis: Antinuclear antibodies attack multiple organs
Positive ANA (antinuclear antibodies
Positive anti-dsDNA
Positive anti-Sm (smith)
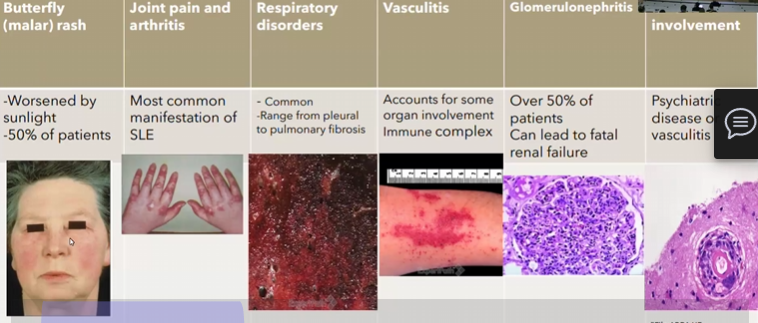
Clinical Features: butterfly rash, joint pain/arthritis, Respiratory disorders, vasculitis, glomerulonephritis
Relapsing-remitting disease
Systemic Sclerosis/Scleroderma
Pathogenesis
Clinical Features
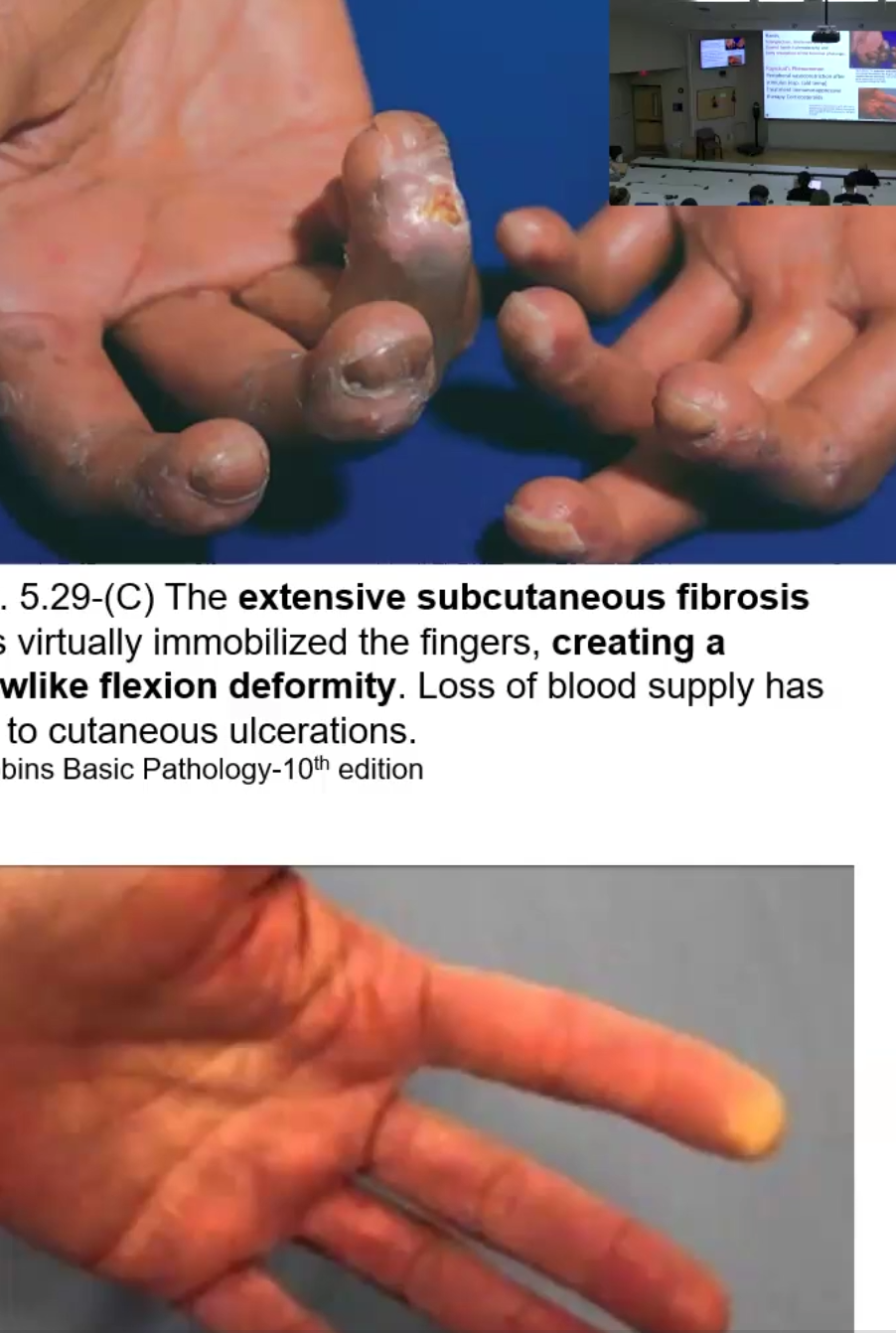
Multiple autoantibodies attack and cause deposition and fibrosis
Clinical features: Fixed facial expression, subcutaneous collagen hypertrophy and esophageal dysmotility, telangiectasis, sclerodactyly (claw hands)
Raynaud’s Phenomenon: peripheral vasoconstriction after stimulus
Ankylosing Spondylitis
Define
Genetic composition
Clinical Features
Autoimmune disease affecting the vertebral column and sacroiliac joints
Associated with HLA-B27 antigen
Clinical Features: Pain and stiffness in the spine and large joints, leads to spinal fusion

Reactive Arthritis
Define
Clinical Presentation
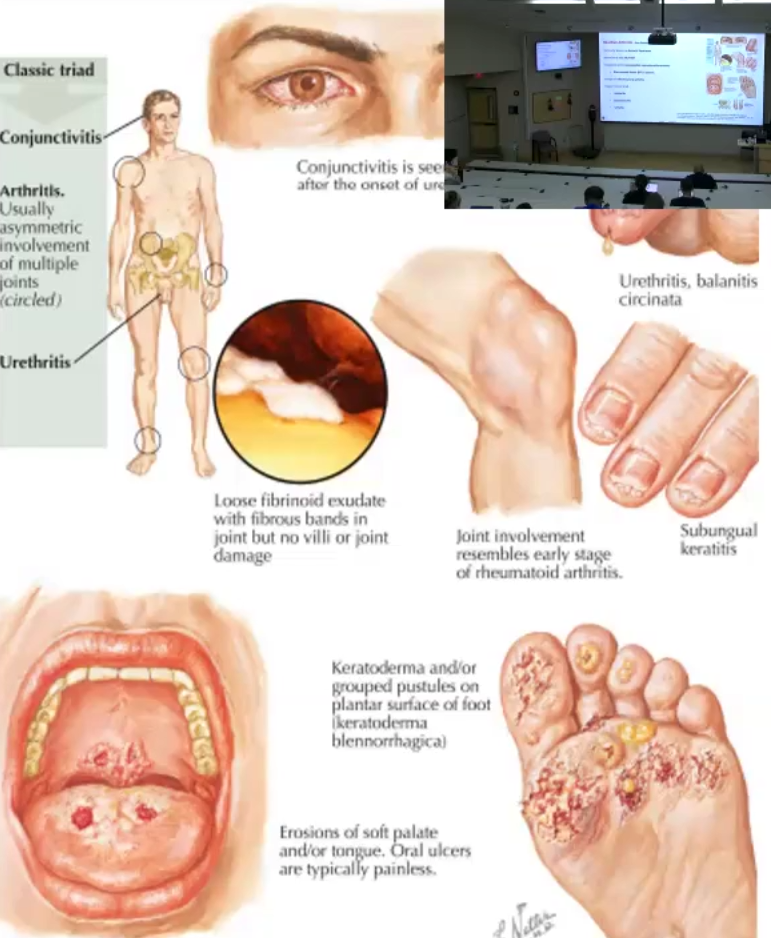
Inflammatory arthritis that lack the Rheumatoid Factor
Classic Triad Presentation: Urethritis, arthritis and conjunctivitis
Osteomalacia vs. Rickets
Etiology
Clinical Presentations
Etiologies for both:
Abnormal Vitamin D metabolism leads to increased PTH, which then causes phosphate deficiency
Can also be due to inadequate sun exposure, malabsorption or defective hydroxylation, low calcium or phosphate
Osteomalacia: Inadequate mineralization of the newly-formed bone matrix; predisposes to fractures
Nonspecific and can be asymptomatic for years
Muscle weakness, hypotonia
Labs show decreased phosphate and calcium, increased phosphatase
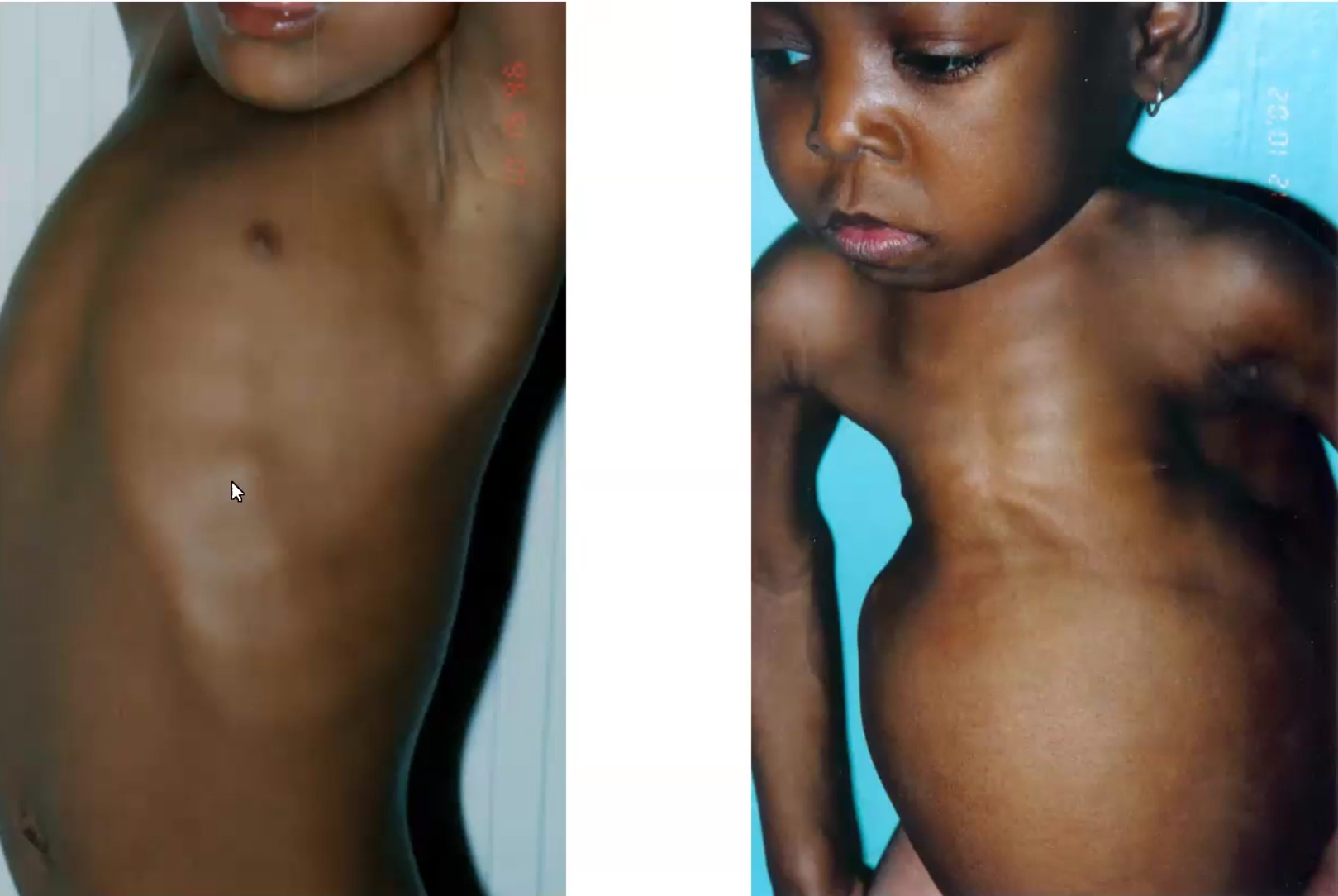
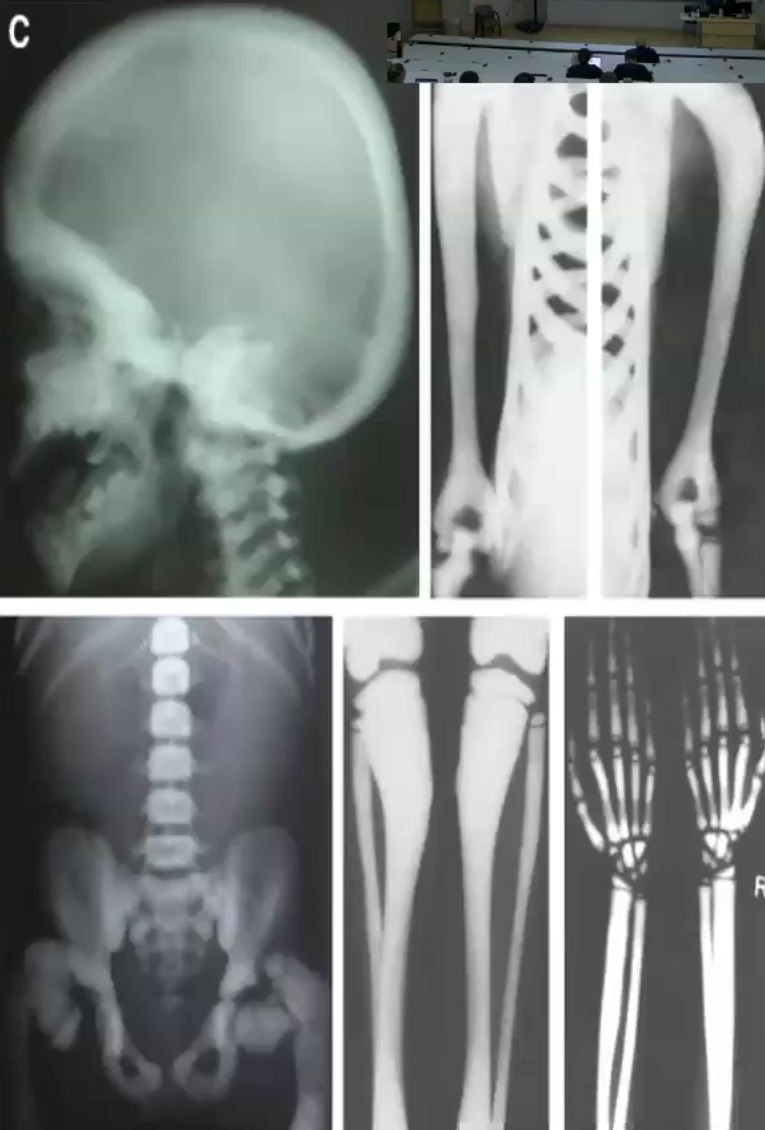
Rickets: Inadequate mineralization causes the growth plates to be open (children)
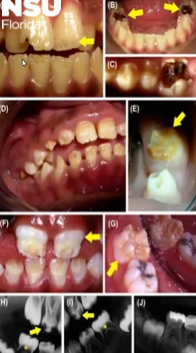
Rachitic rosary chest, pectus carniatum (pigeon breast), enamel hypoplasia
Apathy, irritability, sedentary, sort stature, flattening skull, abdominal muscle weakness, fractures and dislocations
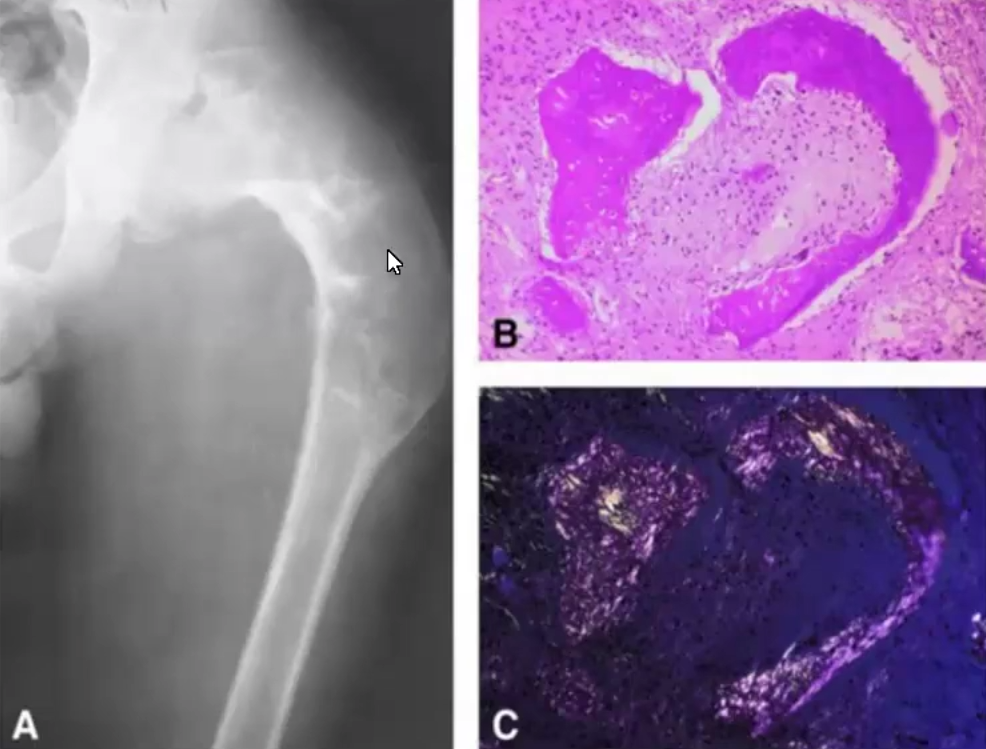
Primary Hyperparathyroidism/ Osteitis Fibrosa Cystica → BROWN TUMOR!
Etiology
What does it cause
Clinical Presentation
Most commonly due to parathyroid adenoma
Increased PTH leads to calcium conservation through bone resorption, thus osteoclast activity goes up
Clinical features: skeletal changes, kidney stones, psychiatric depression, gastrointestinal irregularities
Paget Disease of Bone ( Osteitis Deformans)
Pathogenesis
Localization
Clinical Presentation
What is the preferred diagnosis marker
Chronic Disorder of the bone remodeling where there is increased osteoblast activity (bone destruction) and disorganized regrowth
Localized to one or two bone sites, most commonly in the spine or skull because skull thickens
Clinical Presentation:
Skull thickening, which leads to hearing loss, platybasia (flattening of base of skull) and increased head size
Fractures and arthritis, anemia, high-output cardiac failure, neoplastic transformation
Preferred diagnosis marker is elevated serum phosphatase

Fibrous Dysplasia
Define
Types
Disease where bone is replaced by fibrous tissue, resembles ground glass on x-rays
Types
Monostotic: most common, one bone, can be asymptomatic, pathologic fractures
Polyostotic: multiple bones, painful, limb deformities and pathologic fractures
Ex; Mccune-Albright Syndrome: accompanied by endocrine dysfunction, precocious puberty, pigmented macules, short stature

Osteogenesis Imperfecta/ Brittle Bone disease
Etiology
Clinical Manifestations
Etiology: Autosomal dominant deficiency in collagen type I due to mutation in COL1A1 and COL1A2 (for alpha 1&2 chains of type I procollagen)
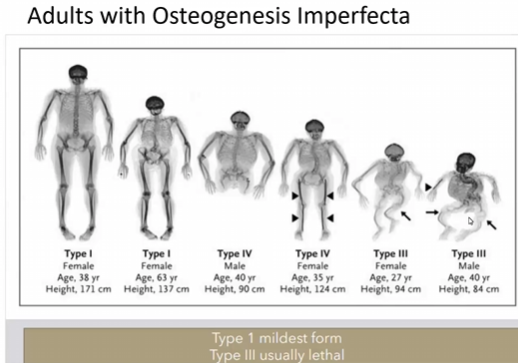
Clinical Manifestations: Low bone mass, increased bone fragility, gray-blue Sclerae

Osteoporosis and Osteopetrosis
Define
Etiology
Clinical Features
Osteoporosis: Decreased bone mass due to increase in osteoclast function and decrease in osteoblast function
Most common in females >50yo due to decreased estrogen
Results in weak brittle bones and pathologic fractures
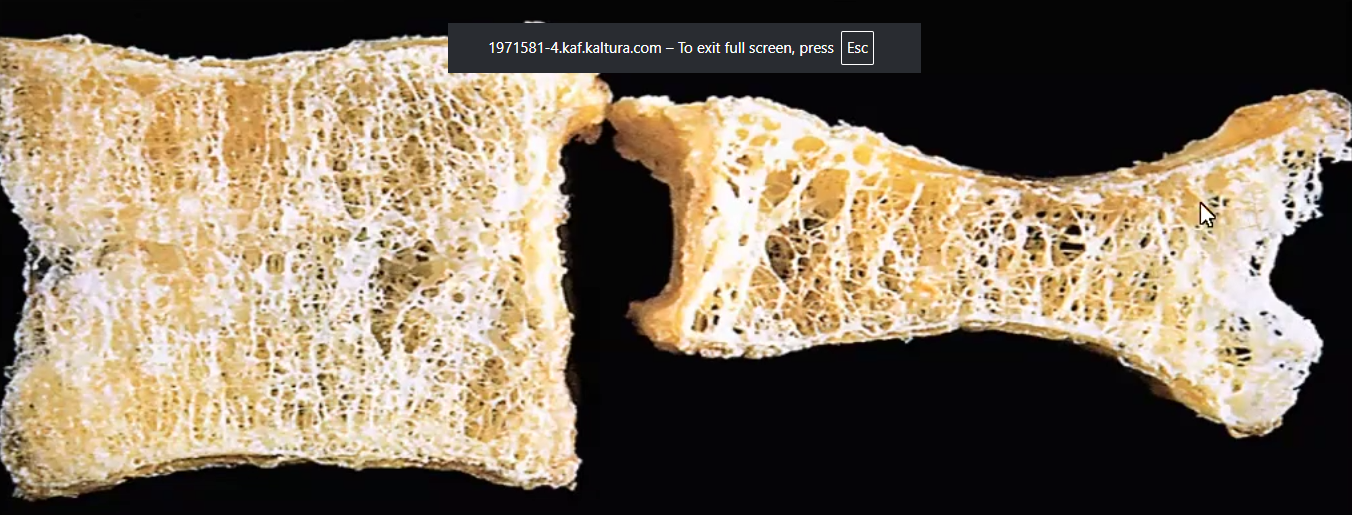
Osteopetrosis: Rare genetic disorder of osteoclast function and or development that results in impaired bone resorption and increased sclerosis
Leads to markedly dense bones, obliteration of bone marrow space, suppression of hematopoiesis, sclerotic bone is brittle
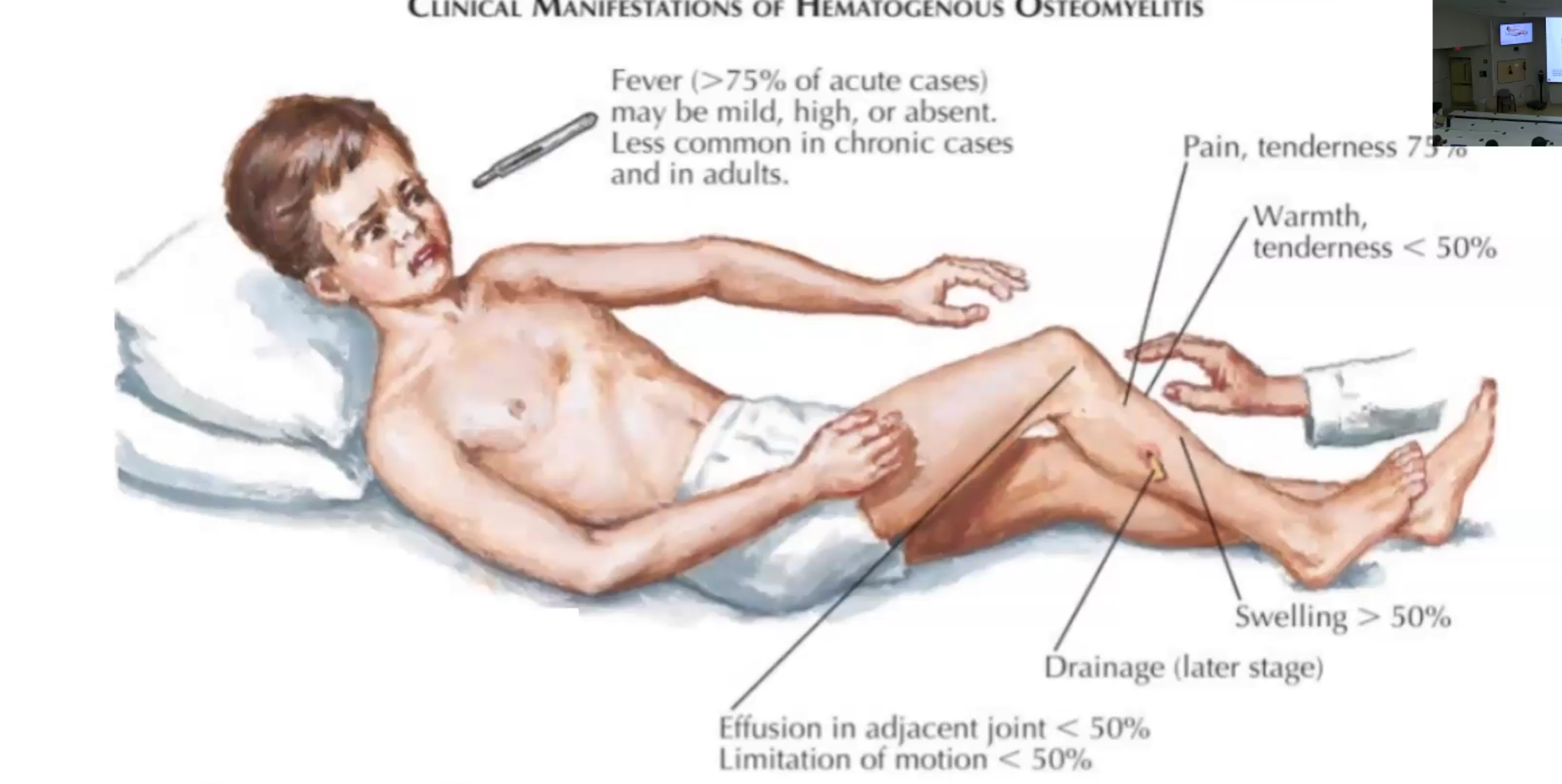
Acute Osteomyelitis
Definition
Routes
Risk Factors
Pathogenesis
Most Common sites affected by hematogenous spread
Clinical Manifestations
Complications
Inflammation of bone and marrow, almost always secondary to infection
Routes: direct penetration through wounds, open fracture or surgery, OR Hematogenous spread
Risk Factors: IV Drug use
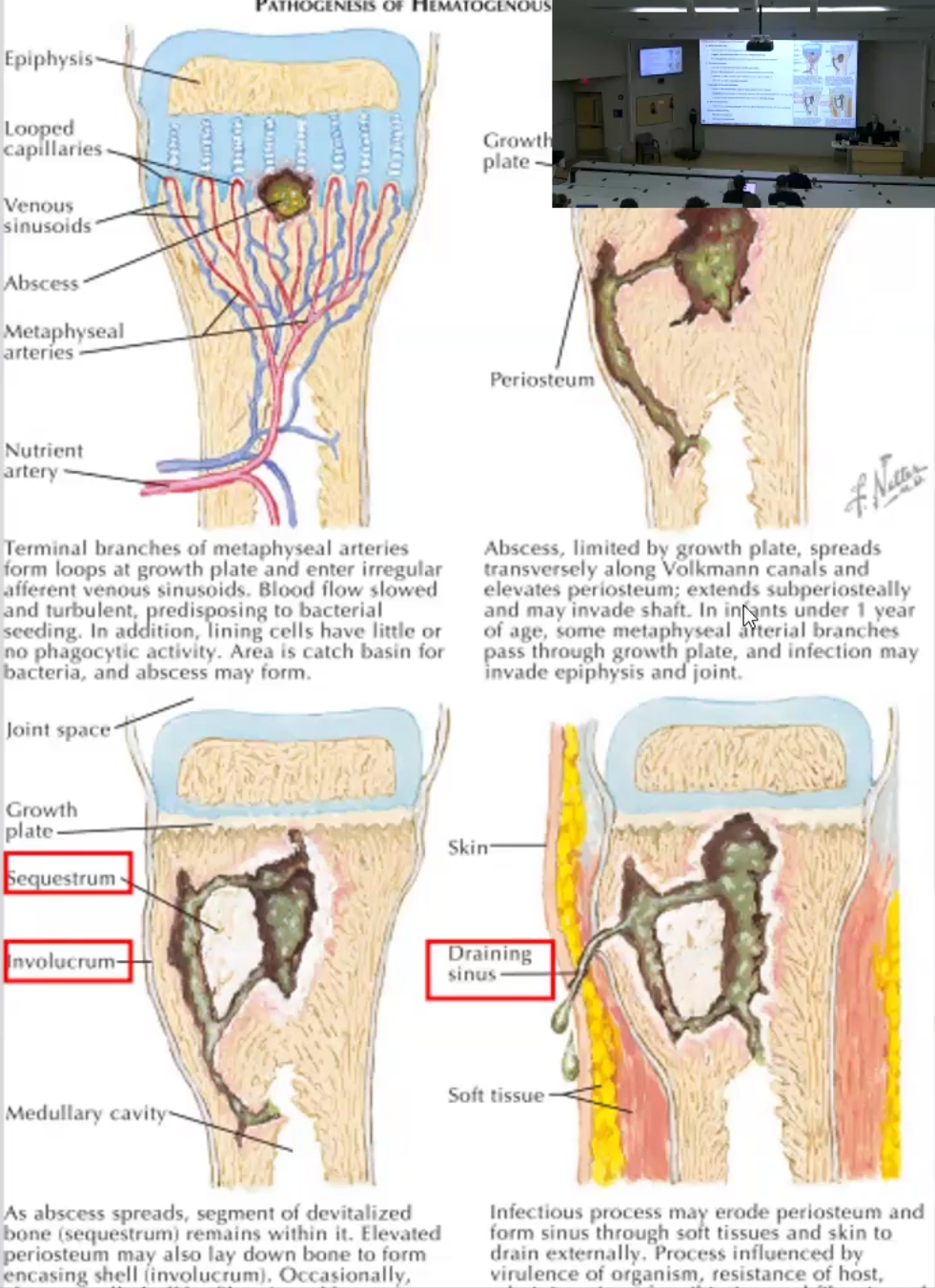
Pathogenesis:
Infection by Staph species occurs (80-90% of cases
Turbulent flow in terminal branches of metaphyseal plate and poor phagocytic activity contributes to infection spread
Abscess formation
Infection spreads through Volksmann canals and elevates periosteum and etends into shaft
In infants <1yo it reaches epiphysis and joints
Sequelae of Abscess Formation
Infection results in devitalized bone segment called sequestrum
Elevated periosteum may form new bone called involucrum
Infection can be walled off by fibrosis and sclerosis, this is called Brodie abscess
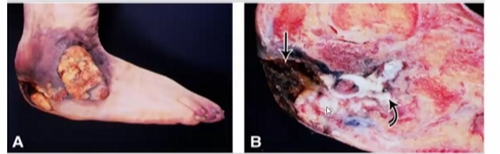
Chronic Progression: infection may erode periosteum, forming draining sinus through tissue and skin
Most Common sites affected: metaphysis of the long bones such as knee, ankle and hip
Clinical Manifestations: fever, pain, warmth, tenderness effusion to adjacent joint, limited motion, drainage
Complications: Septicemia, Acute bacterial arthritis, pathologic fractures, squamous cell carcinoma, chronic osteomyelitis
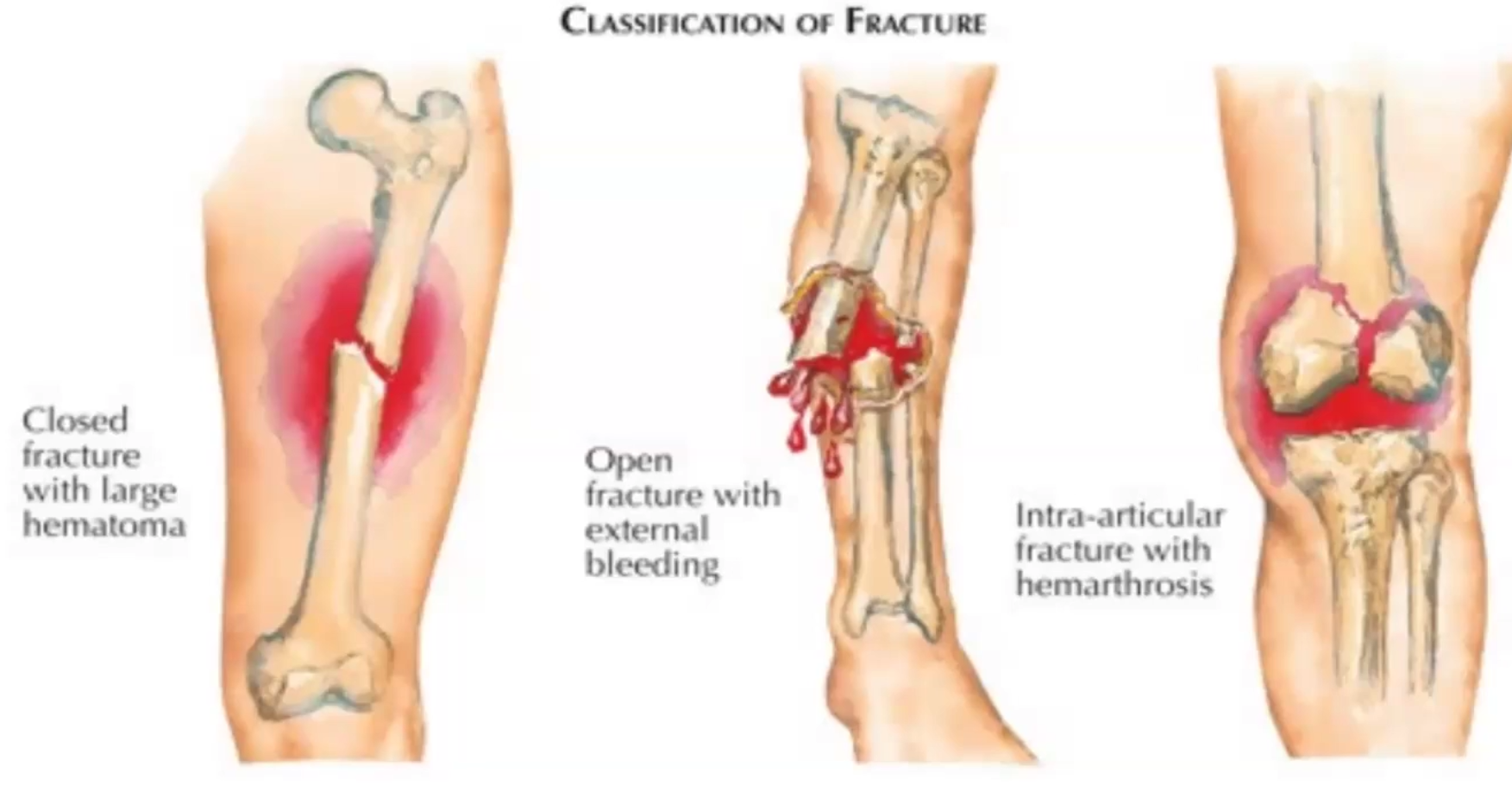
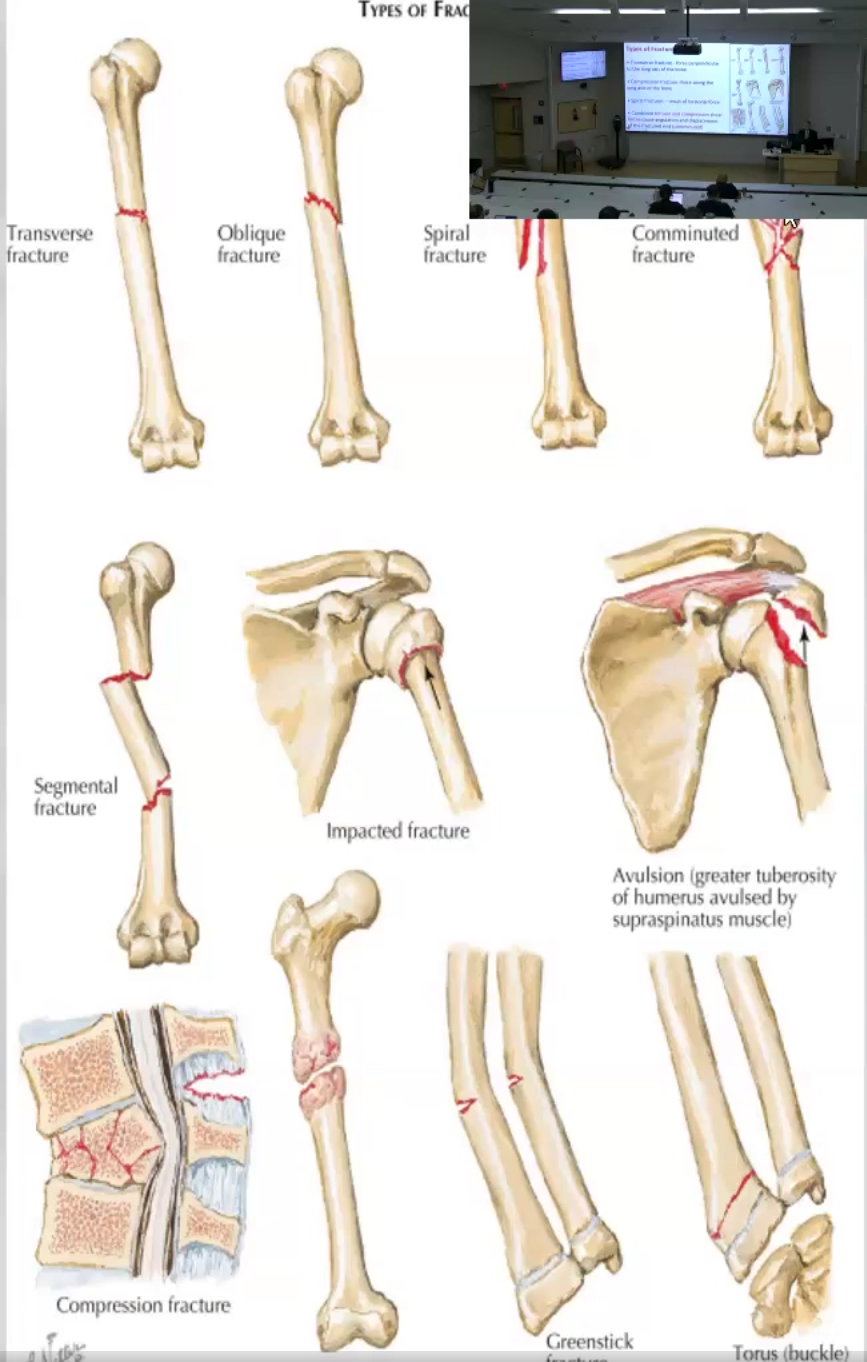
Fractures
Classifications
Types
Complications
Classifications: Open fracture, closed fracture and inter-articular fracture
Types: Transverse, Compression, Spiral, Combined
Complications:
Nonunion: an be due to ischemia, soft tissue interposition, infection or malnutrition
Malunion
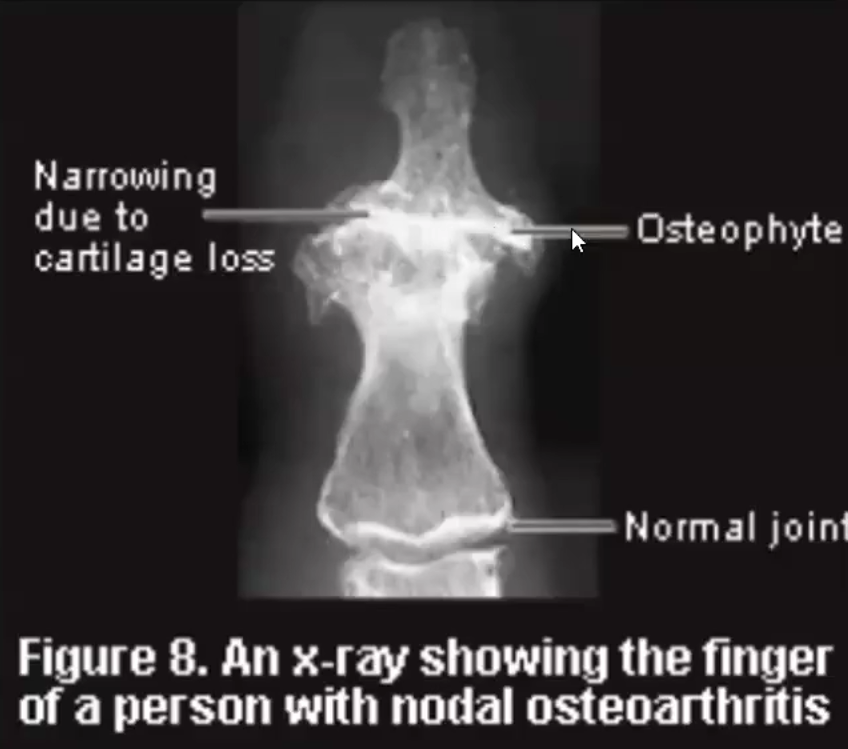
Osteoarthritis/ Degenerative Joint Disease (DJD)
Define
Most Common form of
Primary vs Secondary
Etiology
Pathogenesis
X-ray&Histology findings
Clinical Features
Slow and progressive destruction of articular cartilage especially weight-bearing joints and fingers of older adults
Most common form of Joint disease
Primary vs Secondary
Primary: Wear and tear arthritis which is aging-related or caused by intrinsic defects in articular cartilage
Secondary: due to trauma, crystal deposits, infection or Inflammatory diseases
Etiology:
Increased unit load and incongruities of the joint
Stiffness of subchondral cancellous bone
Biochemical abnormalities affecting type II collagen proteoglycans
Eg. Increased secretion of MMPs
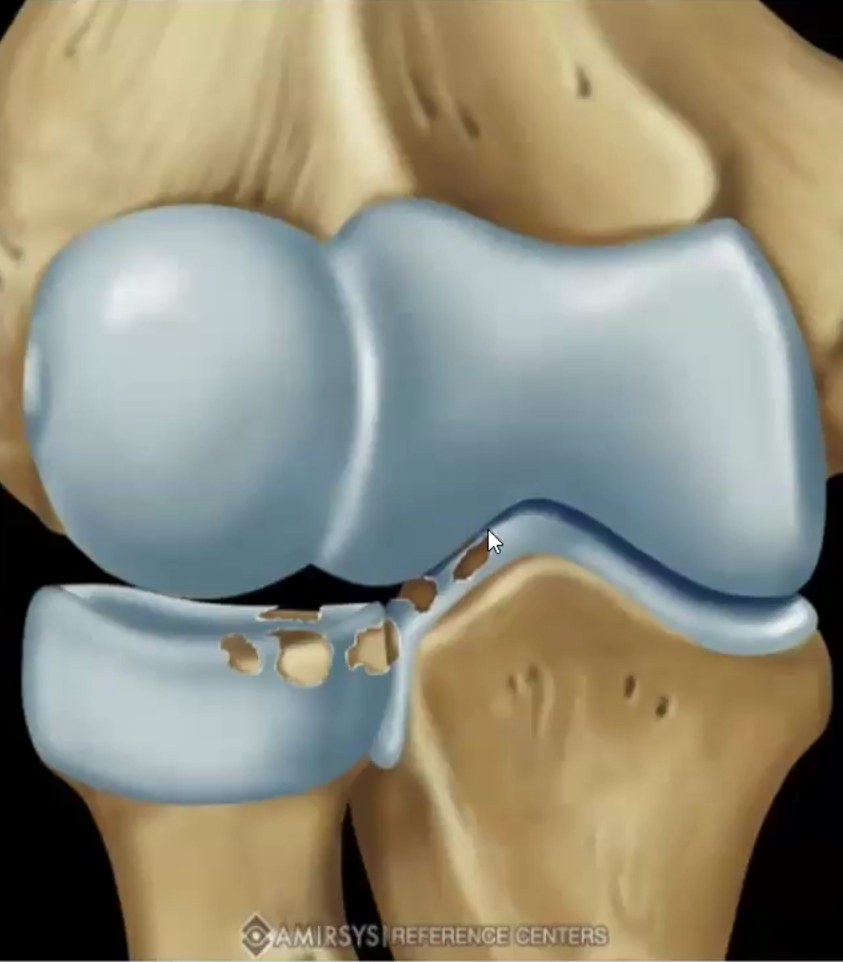
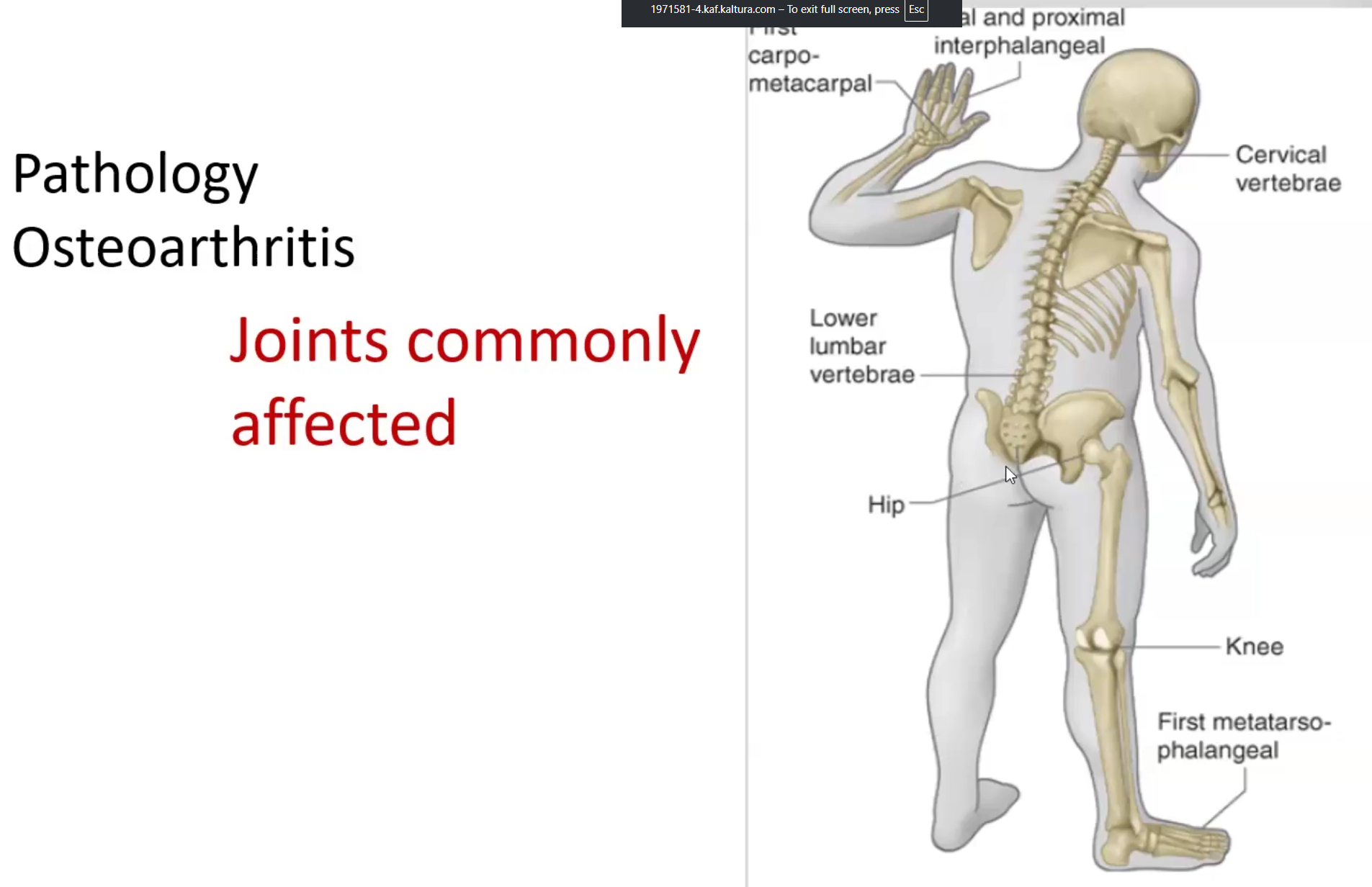
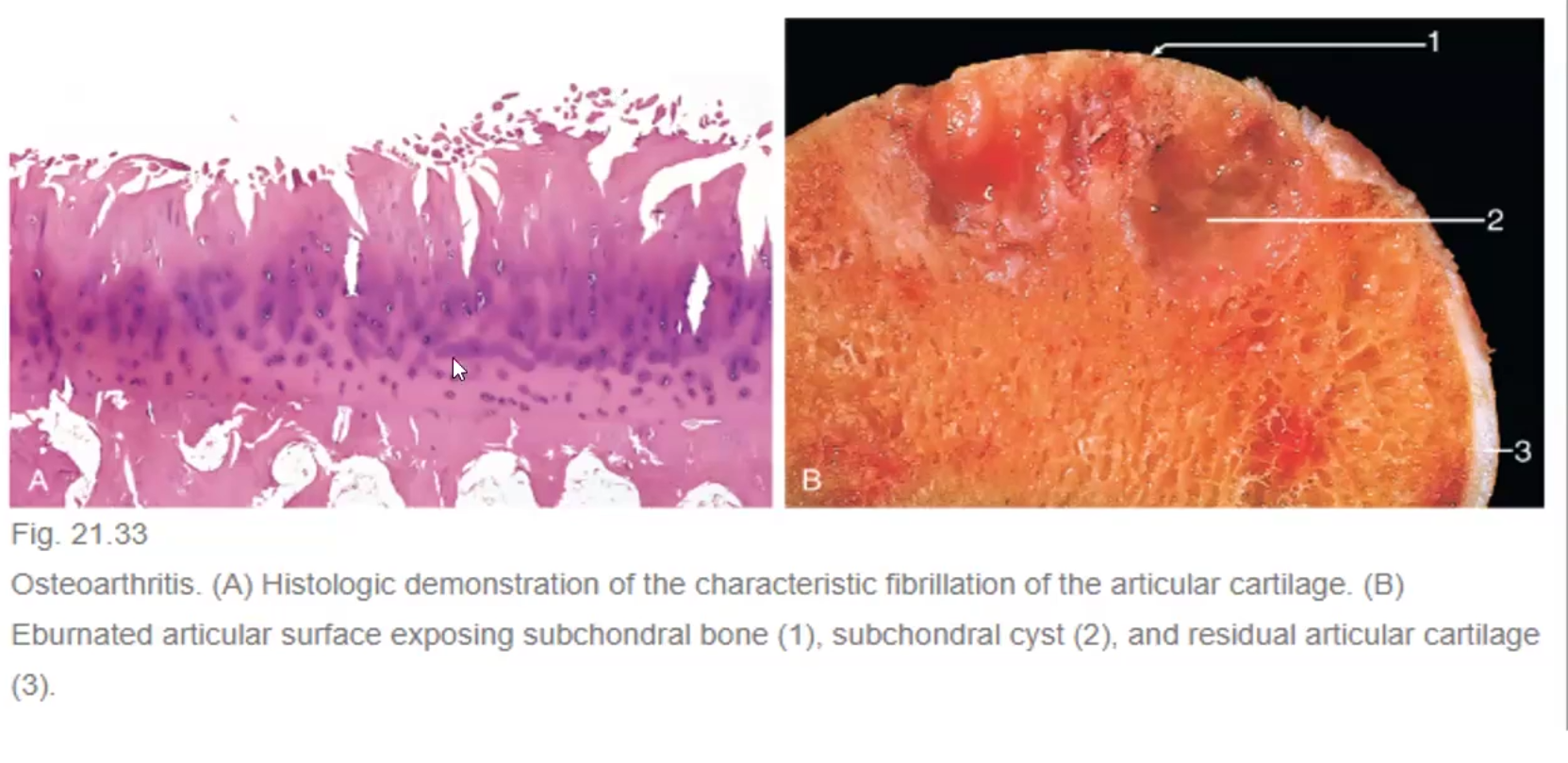
X-ray & Histologic findings: narrowing of joint spaces, large peripheral growth of bone and cartilage (osteophytes), fibrillation of articular cartilage and eburnated articular cartilage surface exposing subchondral bone
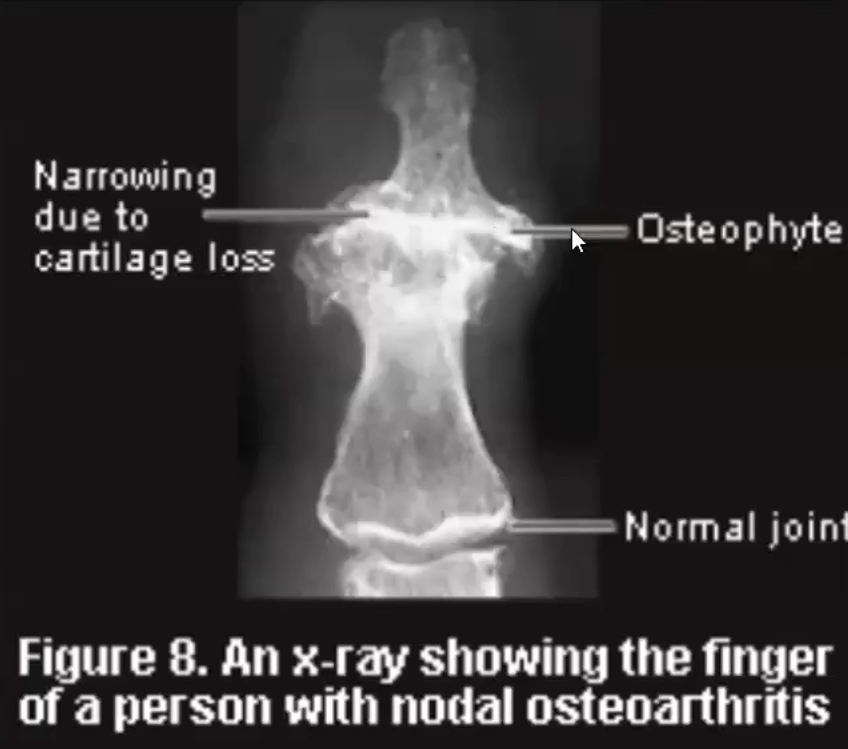
Clinical Features: Heberden Nodes (prominent osteophytes at the distal interphalangeal joints, common in women), deep, achy joint pain follows activity but relieved by rest
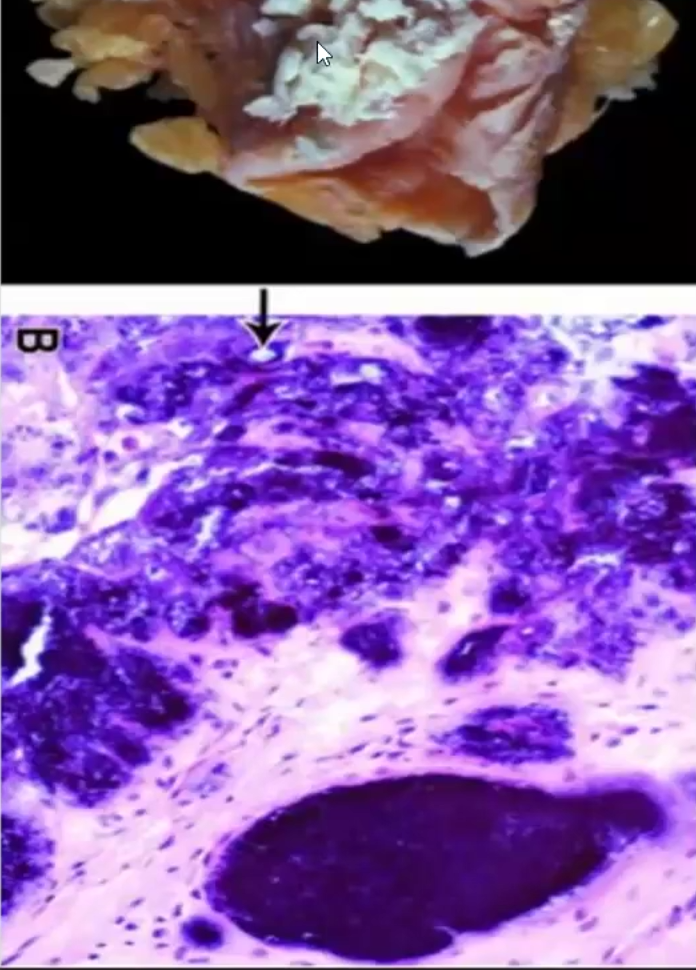
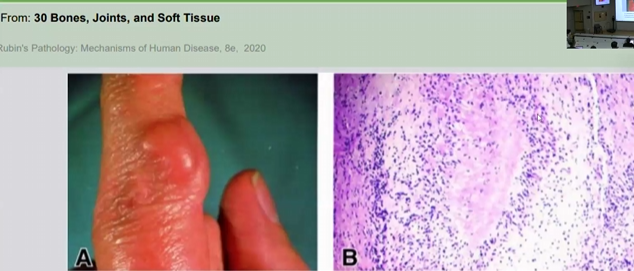
Gout
Primary vs Secondary
Pathogenesis
Clinical Features
Pseudogut
Primary vs. Secondary
Primary: due to hyperuricemia not associated with systemic disease; can be due to environmental habits such as diet or it can be due to genetic predisposition
Secondary: due to systemic disease such as diabetes, obesity, etc
Pathogenesis: overproduction of purines (inherited) OR overconsumption leads to increased catabolism of nucleic acids, which leads to decrease salvage of purine bases and decreased urinary uric acid excretion
Clinical Features: Gouty tophi of the hands (rubbery nodules), cross-section demonstrates toothpaste-like urate crystals, brownish monosodium urate crystals
Painful, swollen, warm, erythematous joint
Typically monoarticular but can be poly if chronic
Ankle, foot, knee, first MTP
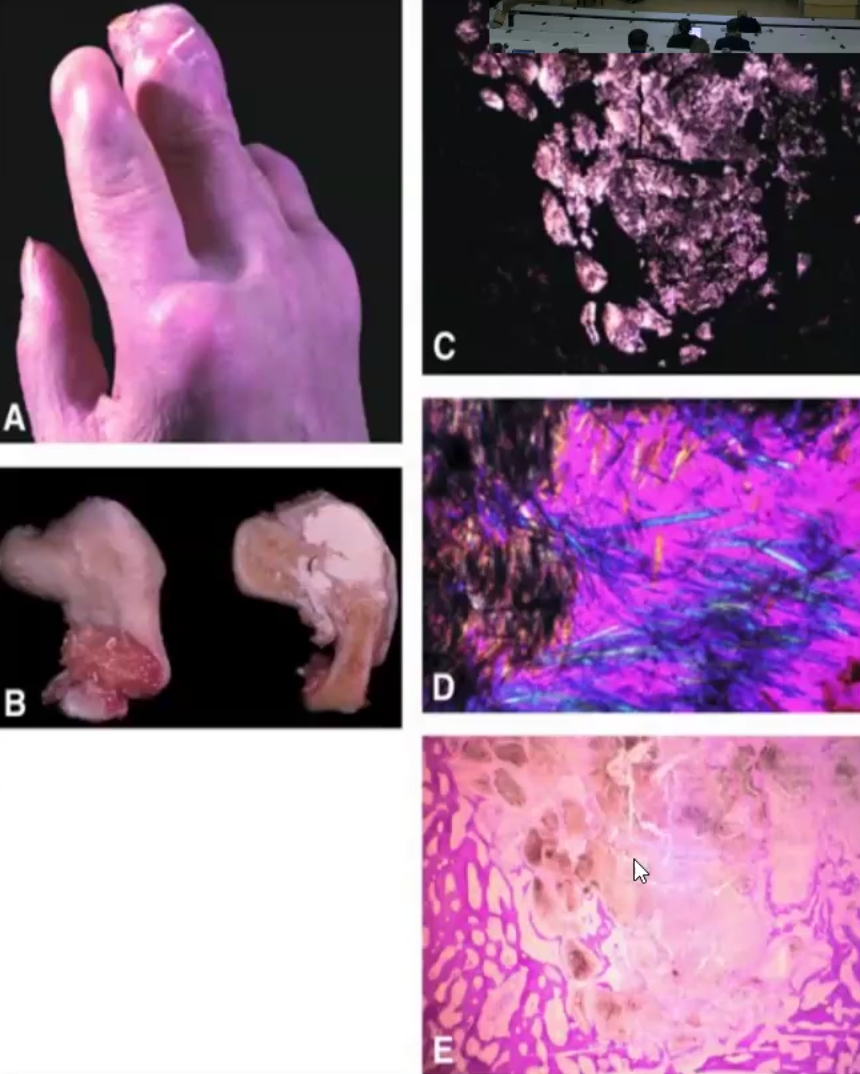
Pseudogout: Similar condition not caused by uric acid accumulation, but calcium pyrophosphate instead, gross specimen shows chalky-white calcific material
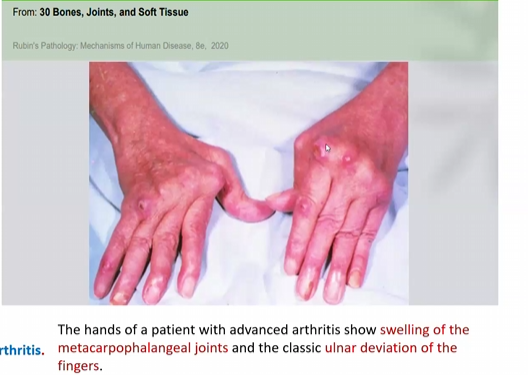
Rheumatoid Arthritis
Define
What are the 2 autoantibodies present
What increases risk
Clinical features
Chronic autoimmune systemic disease causing progressive damage to the joints
Autoantibodies:
Rheumatoid Factor (RF): IgM/IgA/IgG that are reactive against the Fc portion of IgG
Present in 80% of RA patients
Anti-citrullinated Protein Antibodies: target self proteins with citrulline residues
Present in 88-96% of patients and thus the most specific marker for RA
Risk increased by susceptibility genes HLA, or environmental factors such as smoking
Clinical Features:
Pannus: a mass of edematous synovium, inflammatory cells, granulation tissue and fibroblasts that grows over articular cartilage and damages it
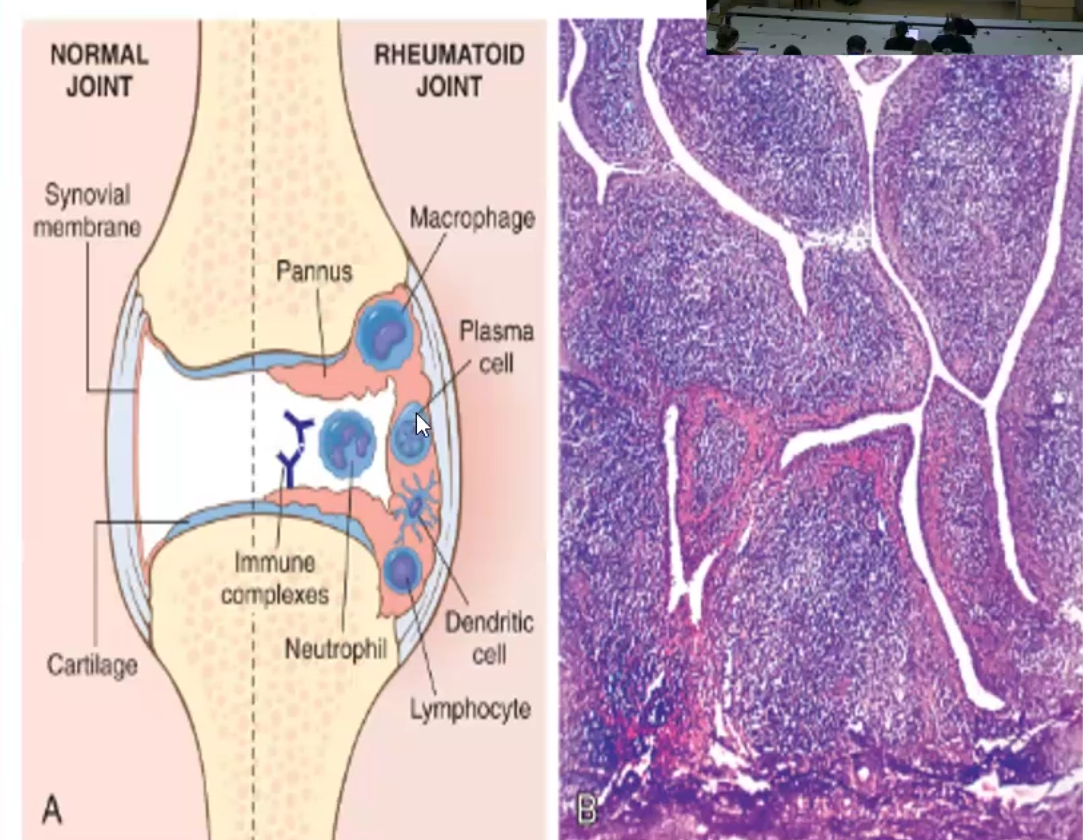
Joint pain, swelling, stiffness, loss of motion, nodules, and other extra-articular symptoms
Neoplastic Disease of Bone
Benign or Malignant?
Most affect what population?
Most common type and talk about it
Most are benign
Affect young people
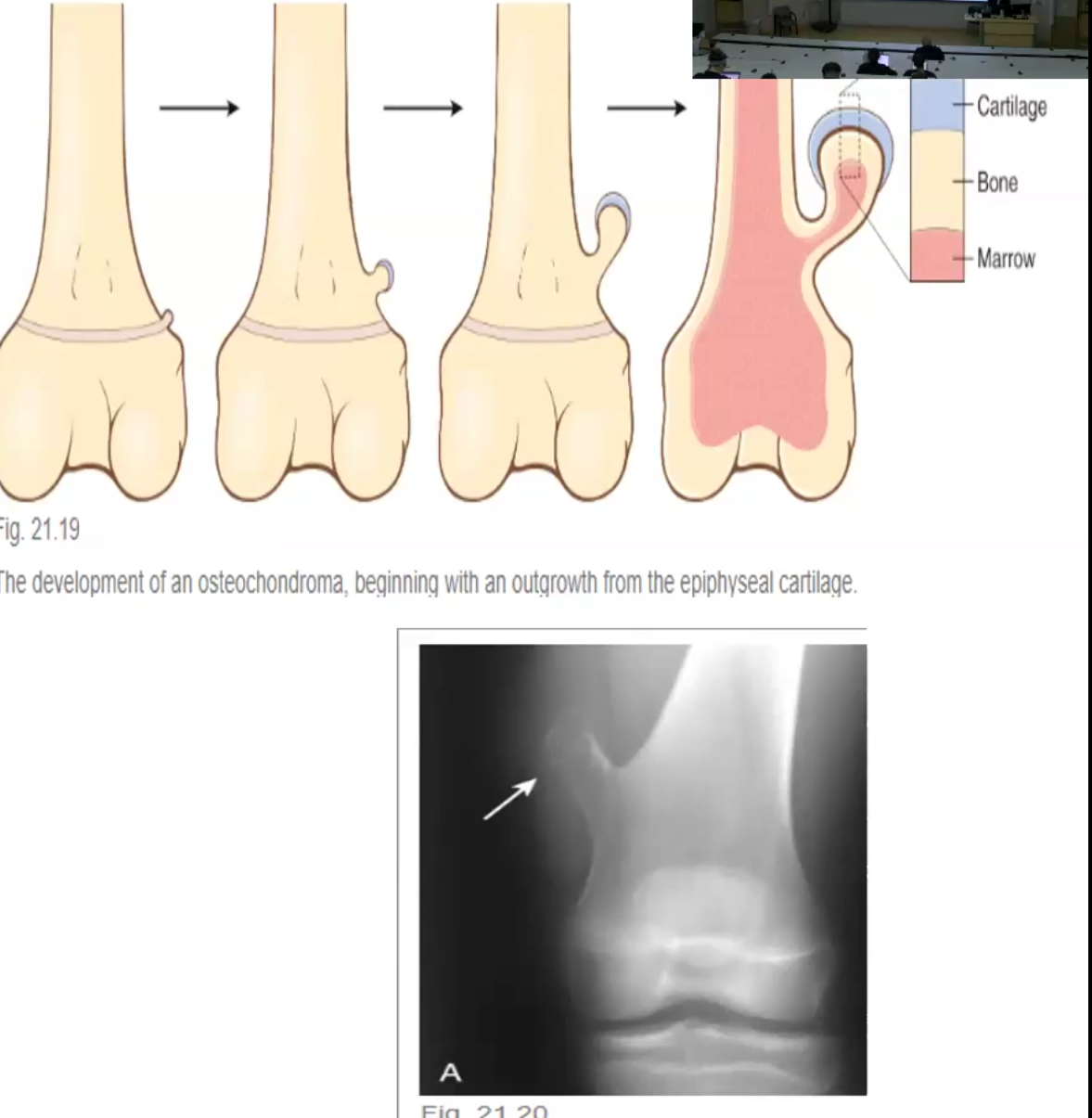
Most common type is osteochondroma:
Benign bony outgrowths with a cartilage cap in the metaphysis of long bones
Usually solitary