Body Fluids Midterm Part I
1/123
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
124 Terms
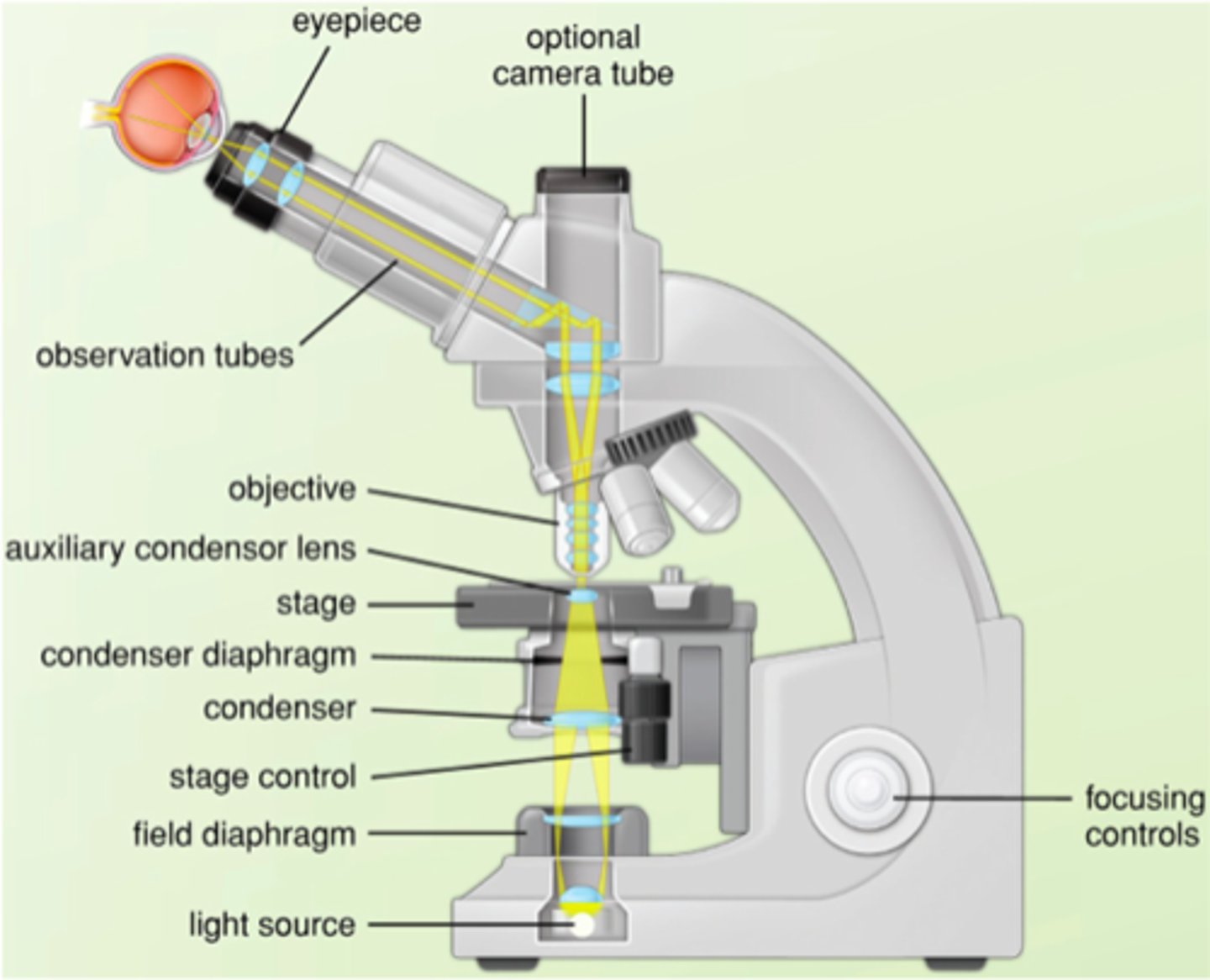
What are the steps of Kohler illumination?
1. Bring specimen into focus via coarse adjustment
2. Adjust fine focus knob
3. Close field iris diaphragm
4. Adjust condenser height knob
5. Center condenser with centering screws
6. Open field diaphragm just past field
7. Adjust condenser diaphragm until maximum contrast is obtained
MUST ADJUST WITH EACH NEW OBJECTIVE LENS USED
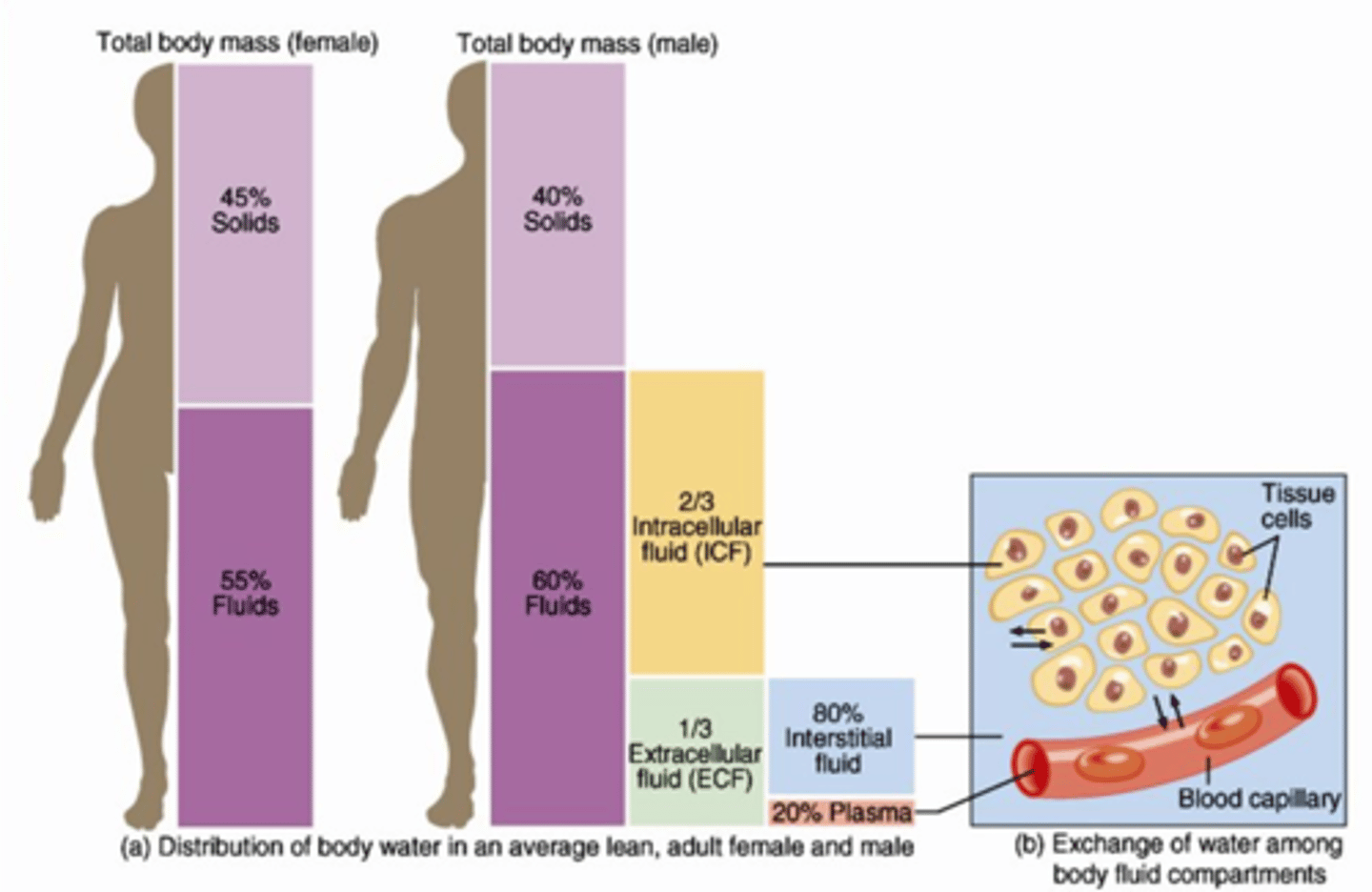
What is the normal distribution of water in the body?
60% of the body weight is water: 40% intracellular, 20% extracellular
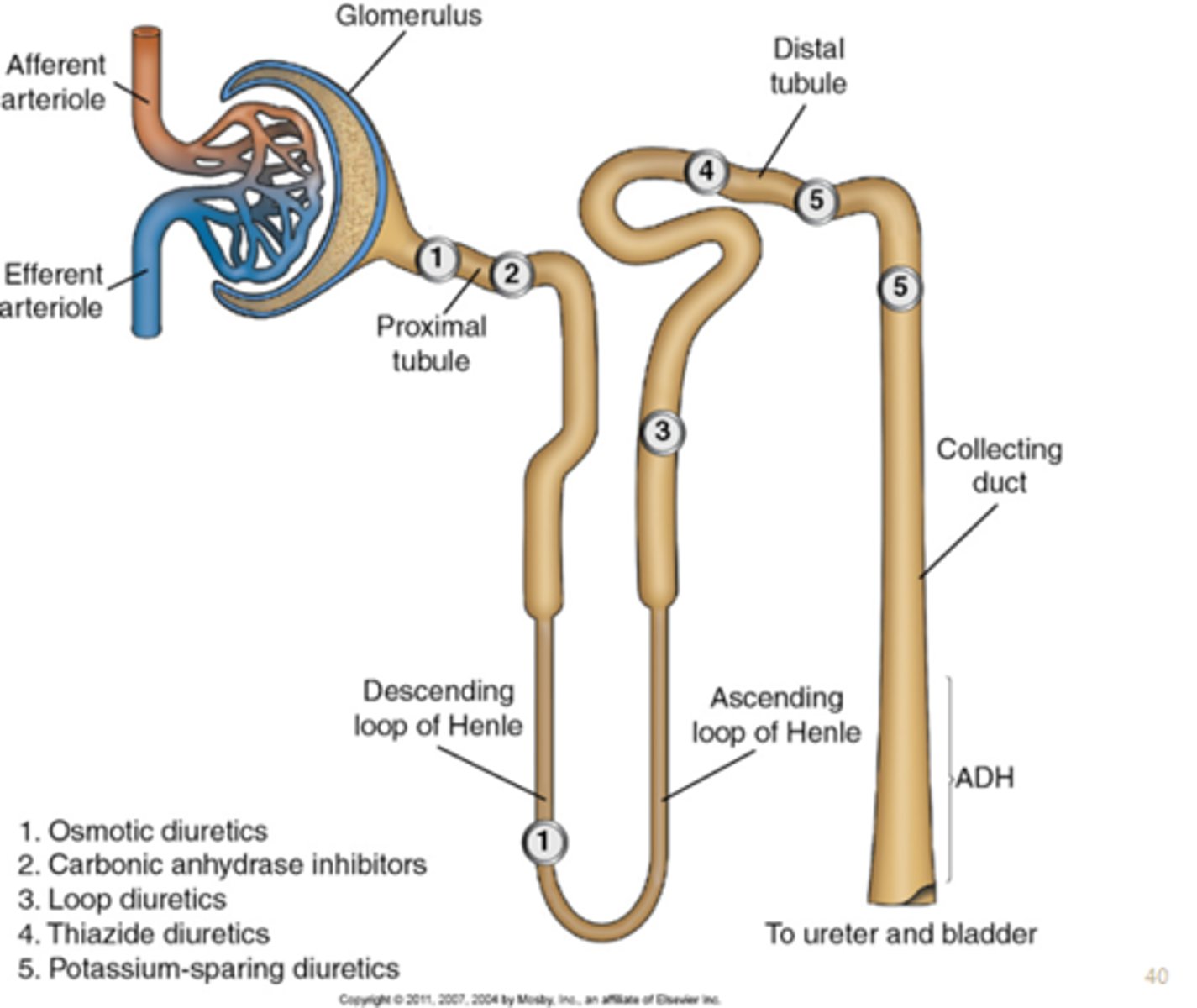
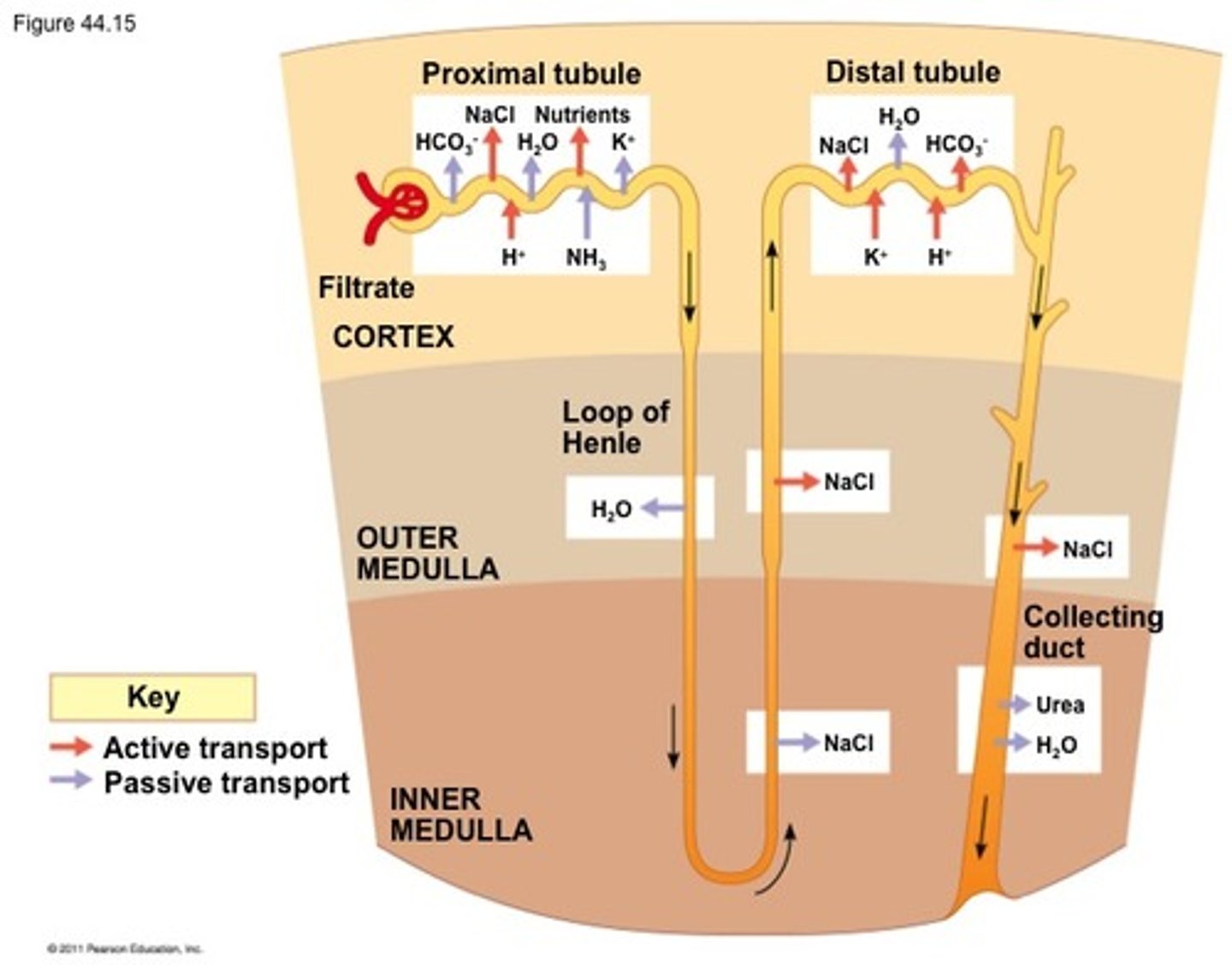
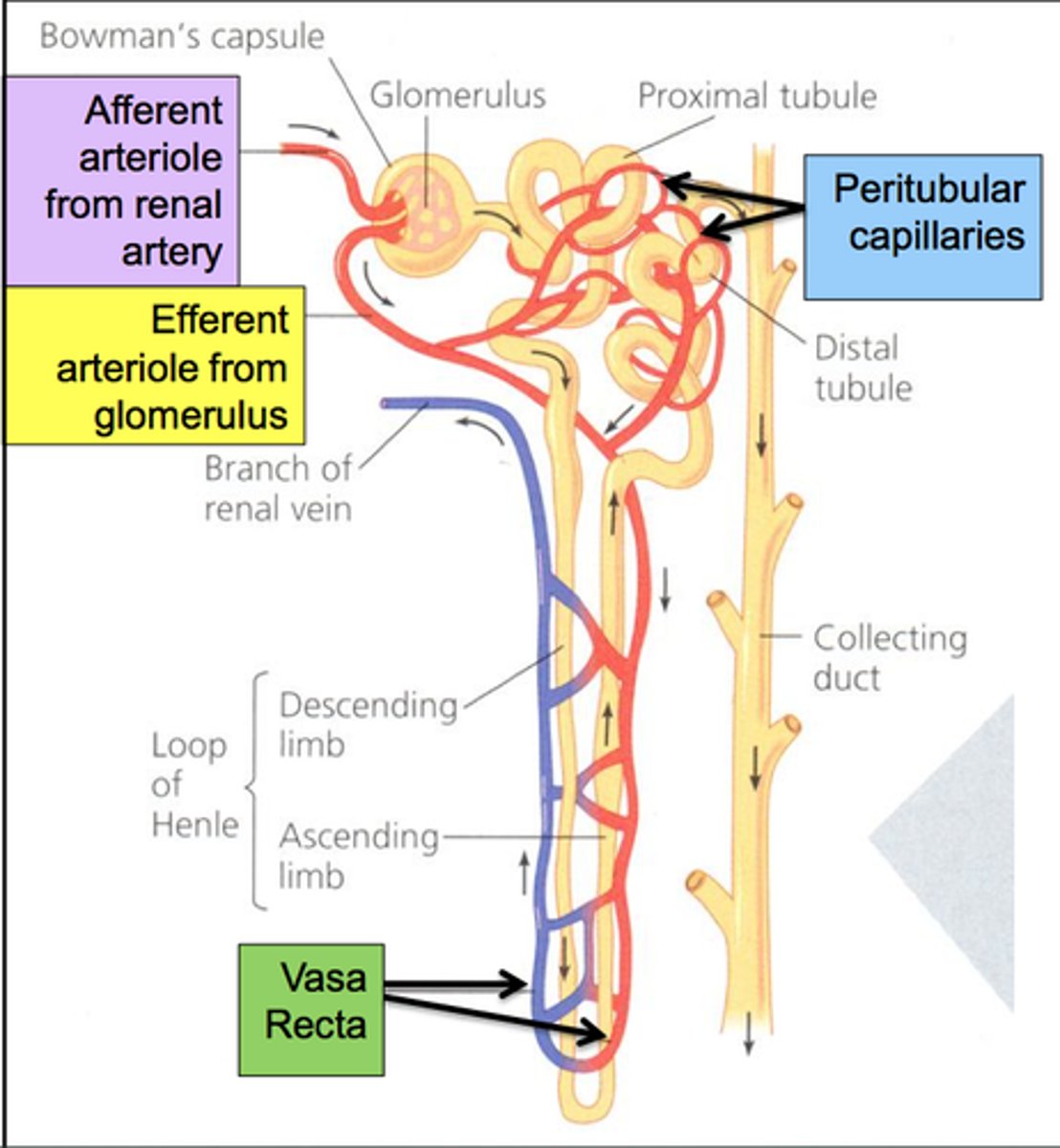
What is the path of water through the nephron?
From the Bowman's Capsule, filtrate passes through the proximal convoluted tubule, to the Loop of Henle, to the distal convoluted tubule,
and then to the collecting ducts.
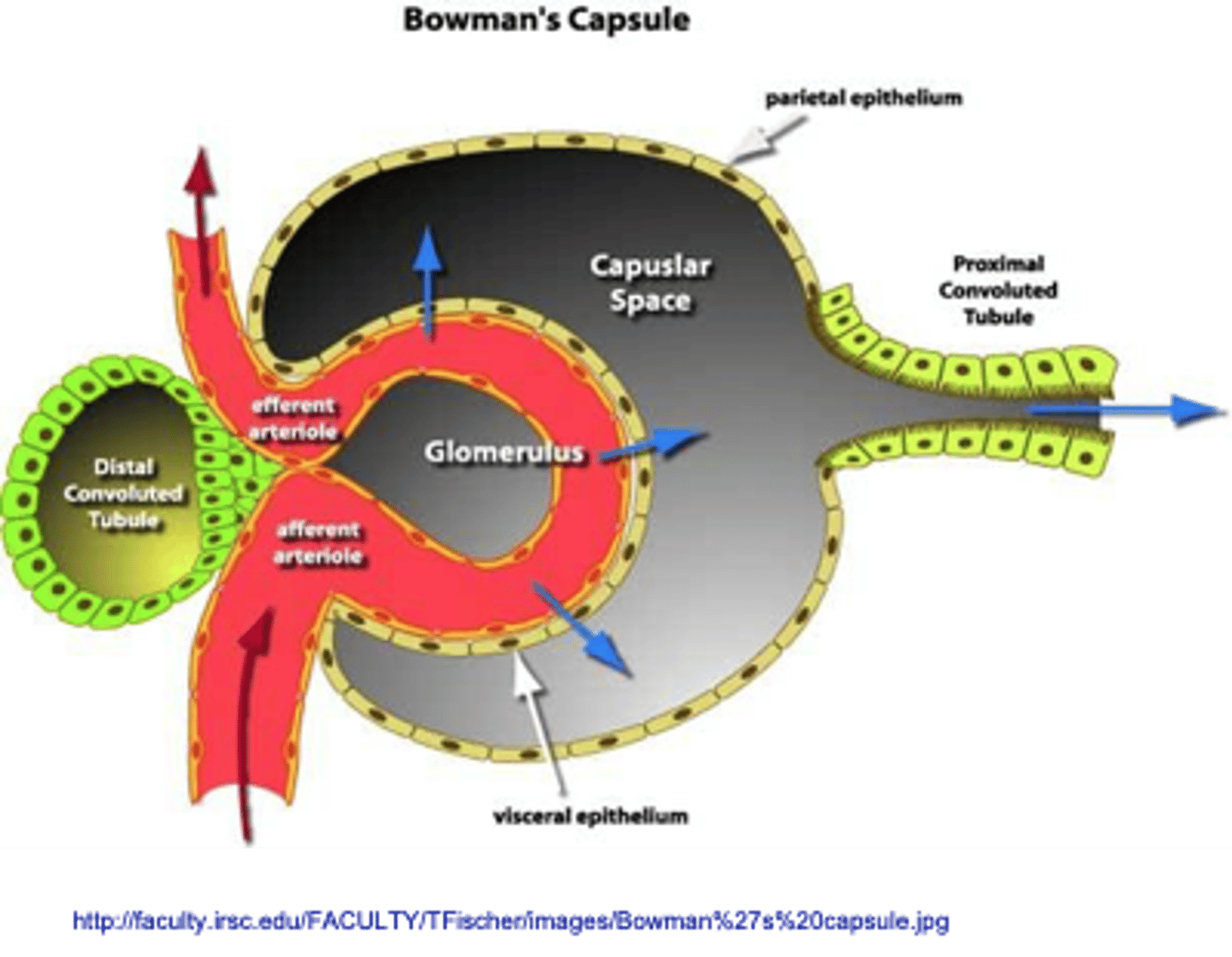
What is the function of Bowman's capsule?
Liquid plasma is filtered into a urinary ultrafiltrate
What are the three processes involved in urine formation?
Plasma ultrafiltration
Selected solute reabsorption
Selected solute secretion
What finding in urine is typically the first sign of glomerular damage?
Proteinuria (albumin)
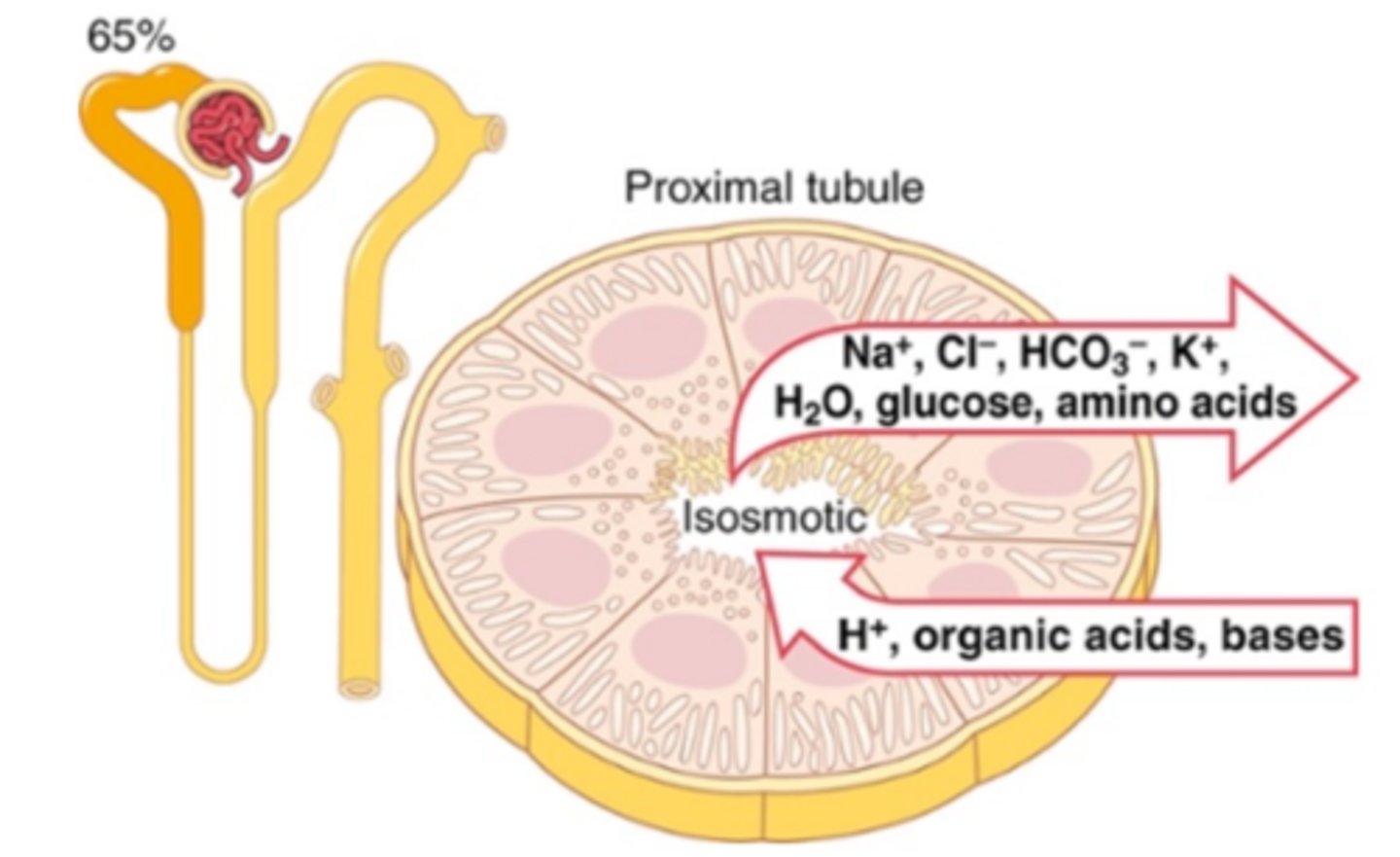
What is the function of the proximal convoluted tubule?
Reabsorption of Water, potassium, chloride, and urea by passive transport
100% of the glucose, amino acids and protein and 66% of sodium reabsorbed by active transport
Secretion of H+, NH3, weak acids and bases
What is the function of the Loop of Henle?
Passive resorption of water, urea, and sodium chloride ions.
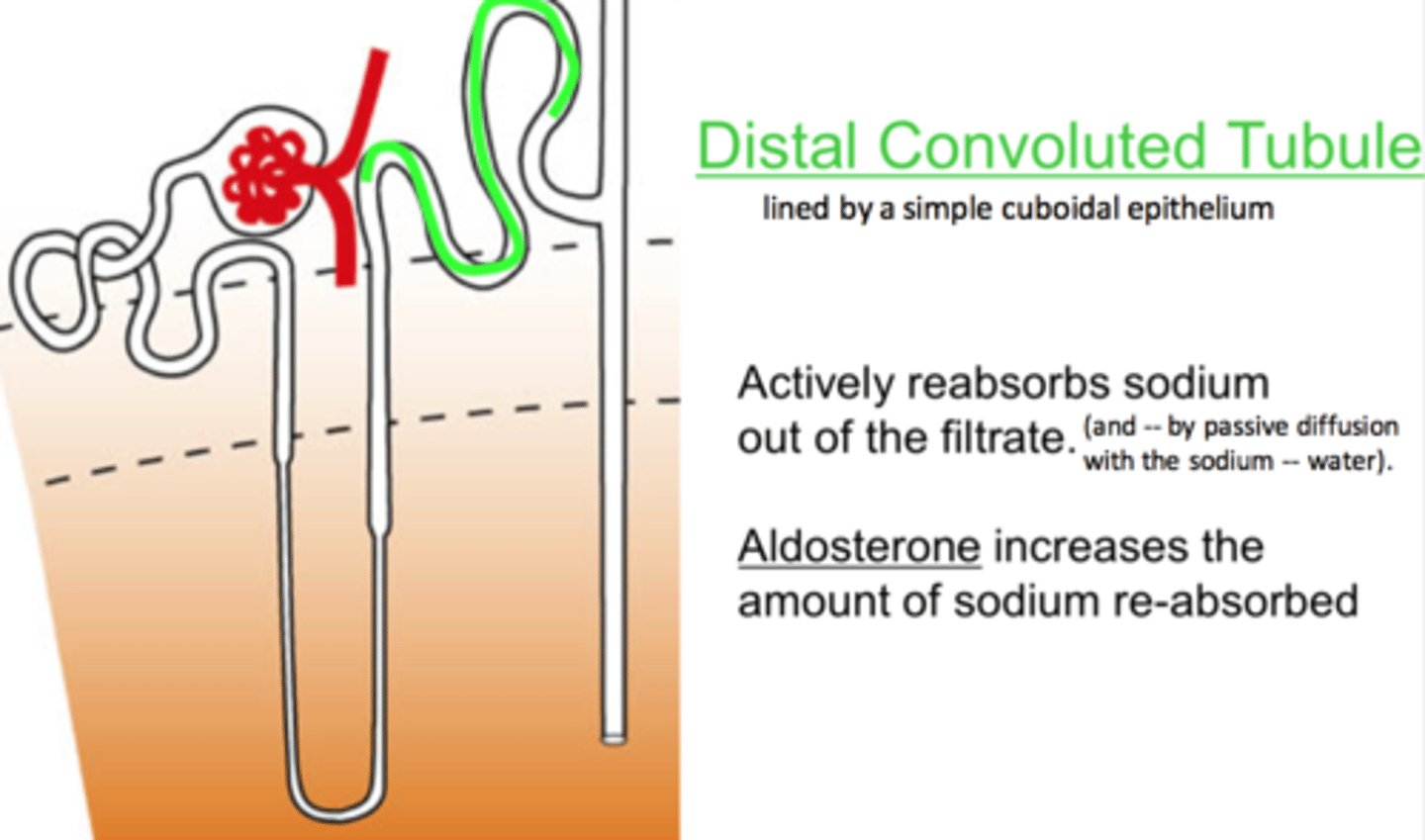
What is the function of the distal convoluted tubule?
Active transport back into circulation of sodium, chloride, sulfate and uric acid
Secretion of H+, K+, NH3, uric acid
What is the function of the collecting duct?
Final concentration of urine
Secretion of H+, K+, NH3
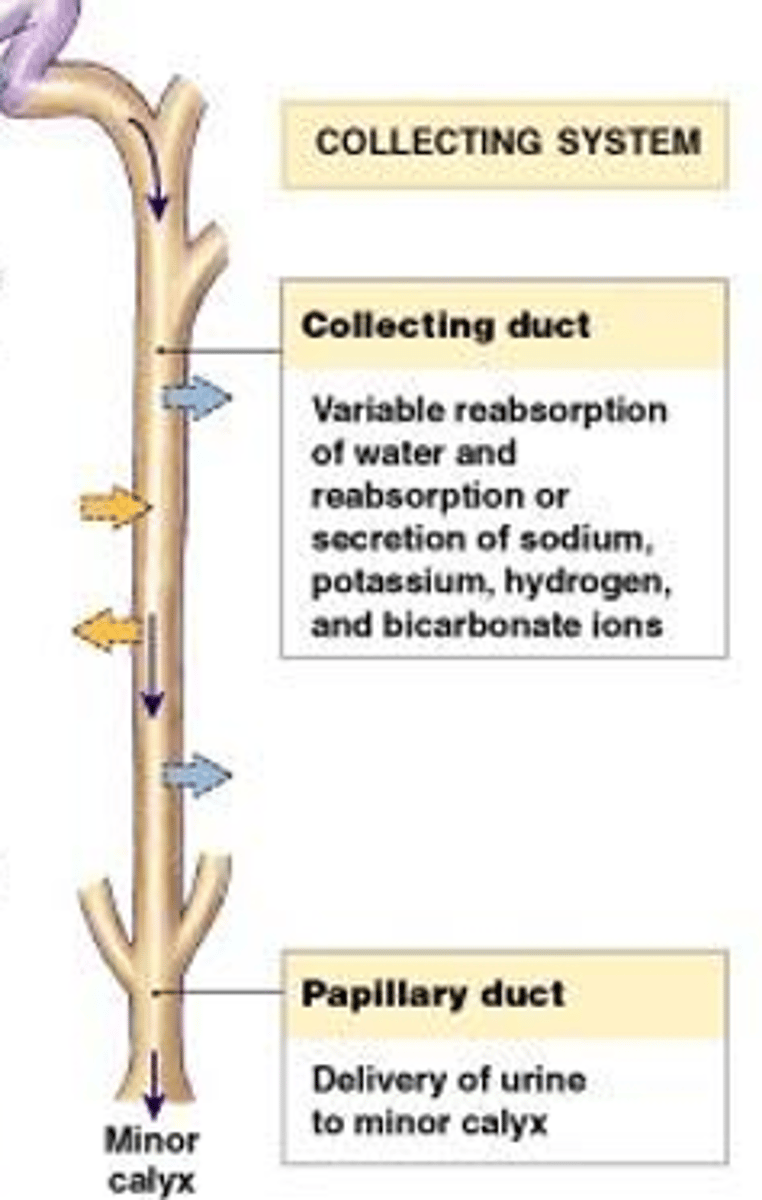
How is the kidney able to concentrate and dilute urine?
The collecting ducts pass through the renal medulla, and it is the hypertonicity of the interstitial fluid, maintained by the processes occurring in the Loop of Henle, that allow the collecting ducts to concentrate the urine into its final concentration.
What is the blood supply of the nephron?
The circulation of the kidney starts as an arteriole and then subdivides into a capillary bed, becomes an arteriole again, and then subdivides into second capillary network. It forms a specialized network of capillaries within the glomerulus. These capillaries are in direct contact with the Bowman's Capsule and it is here that the blood pressure must be high enough to result in the liquid plasma moving from the capillaries into the Bowman's space.
What is a random urine specimen and what is its clinical utility?
Occur randomly, like when at a doctor's office and are adequate for most routine urinalysis
What is a timed urine specimen and what is its clinical utility?
A timed urine is required when clearance rates are being determined. The bladder is emptied at the start of the collection period, and then all urine is collected over a specific time period. The volume of urine collected is determined at the end of the 24 hours, and the creatinine concentration in the urine can be determined.
What is a first morning specimen and what is its clinical utility?
The first morning sample is the most concentrated because it has usually been collected over a longer time period while the patient is sleeping and has not been diluted by the patient consuming liquids. More formed elements may also be present because of the longer time period that urine has been collecting in the bladder.
What is the difference between a routine void and a clean catch specimen?
Routine voids are adequate for most routine urinalysis, but often have contaminants. So the area must be clean prior to urine collection, especially if a UTI is suspected.
What is the time for processing of urine samples, fresh and refrigerated?
Fresh, left at room temperature - within 2 hours of voiding
Refrigerated, 2-6C - within 8-12 hours of voiding
What kind of physical changes can occur to unpreserved urine?
Color changes - oxidation of chemical components (Hgb, red, to methemoglobin, brown)
Clarity changes - as urine cools, crystals can form; bacteria can grow, these increase turbidity of sample
What kind of chemical changes can occur to unpreserved urine?
pH - falsely increased, typically
Nitrite - falsely increased
Glucose - falsely decreased
Ketones - falsely decreased
Bilirubin - falsely decreased
Urobilinogen - falsely decreased
What kind of microscopic changes can occur to unpreserved urine?
Casts can decrease due to dissolution
RBCs and WBCs shape can change, or cells can deteriorate
Bacteria continues to grow, falsely elevated
Trichomonas can die quickly in unpreserved urine
What are the colors used to describe urine and what compounds cause these colors?
Colorless - very dilute urochrome
Yellow - urochrome
Red/pink - hemoglobin, myoglobin, RBCs, beets, food dye
Brown - methemoglobin
Green - indican
Orange - pyridium
What solutes do not affect the clarity of urine?
Any molecule that will dissolve in urine - glucose, hemoglobin, bilirubin
What is the difference between hemoglobinuria and hematuria?
Hematuria (blood in urine) - intact RBCs, cloudy or turbid urine; many RBCs on microscopic
Hemoglobinuria (Hgb in urine) - there is hemolysis of RBCs; no/few intact RBCs on microscopic, clear clarity
Why does foam form on urine specimens and what are the causes of different colors of foam?
Foam is formed by increased of protein
When it is yellow, it is typically caused by increased bilirubin
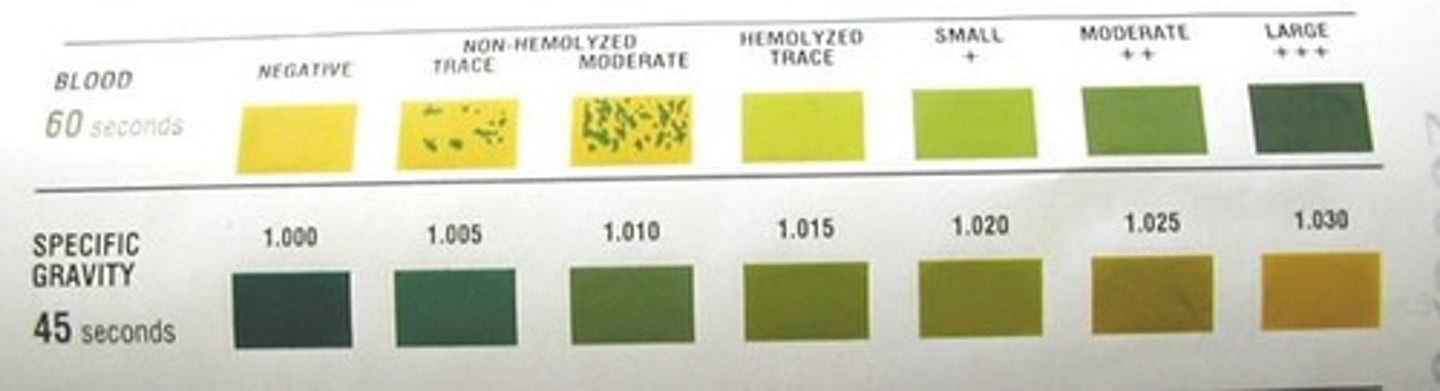
What is specific gravity?
the ratio of the density of a substance to the density of water
What affects the specific gravity of a urine sample?
The size and number of solutes present
What are the direct methods of specific gravity measurement and their principles?
Harmonic oscillation densitometry - sound waves of a fixed frequency are transmitted through the urine. The frequency changes in proportion to the specific gravity of the sample.
Urinometer/hydrometer (picture)- has a weight in the bottom, and a graduated stem. The stem is calibrated, so the level of the fluid on the stem will tell you what the density is of the fluid

What are the indirect methods of specific gravity measurement and their principles?
Reagent strip - relies on the fact that most healthy people will
not have glucose or protein in their urine, and it will only measure the ionic solutes present (not a true specific gravity, sometimes called ionic specific gravity)
Refractometer (picture) - as the light passes through the urine, it is bent to a certain degree depending on the amount of solutes present

What is oliguria?
Low urine volume output (<400mL/day)
How is a urine specimen prepared for microscopic analysis?
The urine is centrifuged for 5 minutes at 450rpm. The brake is not used because this could disturb the urine sediment. 1mL Kova pipette is used to carefully remove 11mL of the supernatant. The urine sediment is then gently resuspended in the remaining 1mL
Describe the color and clarity of a urine specimen that has hemoglobin present but no intact red blood cells
Pink/red and clear
Describe the color and clarity of a urine specimen that has both hemoglobin and intact red blood cells present
Pink to red and slightly cloudy, cloudy, or turbid, depending on the number of RBCs present
List at least three pathological and four non-pathological substances that can cause a urine specimen to be slightly cloudy or cloudy
Pathological: Red cells, bacteria, white cells, yeast, crystals, renal cells
Non-pathological: crystals, squamous epithelial cells, lotions/powders, bacterial contaminants
Describe the principle for determining specific gravity by reagent strip
The reagent strip measures ionic specific gravity, not a true specific gravity. The salts of the urine combine with a polyelectrolyte embedded in the pad. This releases hydrogen ions, as the salts take their place. The release of the hydrogen ions results in a decrease in pH. This results in a color change in the pH indicator embedded in the pad.
Why do urine sediment components such as RBCs, WBCs, and epithelial cells NOT affect specific gravity by any method?
Specific gravity is affected by dissolved compounds in the solution. The cells are not dissolved in the solution, only suspended.
List one substance that can cause the urine specific gravity to be greater than 1.050
Very dense dyes, like radiographic contrast
Differentiate test sensitivity and specificity
Specificity - the test's ability to react with only one compound, and not with closely related compounds.
Sensitivity - the smallest concentration that can accurately be measured by a test
What is a test's range of detection?
The range of results that can be accurately determined using a particular method
ie. Glucose assay from 50g/dL to 500g/dL
What are the minimum and maximum possible measurements of specific gravity and their physiology?
1.002 - the lowest concentration closest to pure water, as the kidneys are not able to excrete pure water
1.040 - equal to the concentration of the hyperosmotic renal medulla; greater than 1.040 is physiologically impossible, and indicate the presence of another compound, like contrast dyes
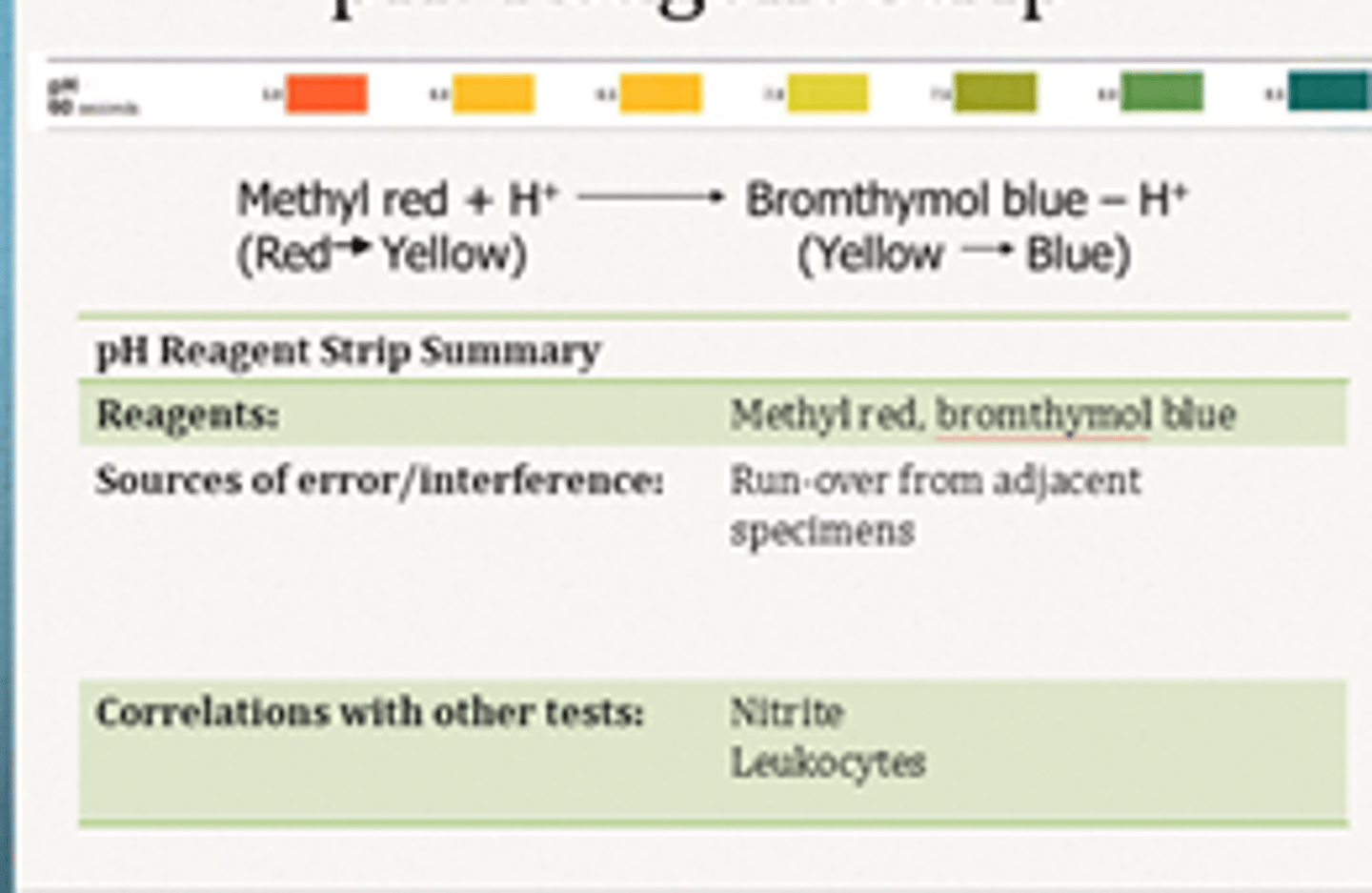
What is the principle of the reagent strip pH test?
Two different pH indicators, bromothymol blue and methyl red are embedded into the pad. The combined colors of the indicators produce a range of colors
What is the principle of the reagent strip blood test?
The heme portion of the hemoglobin molecule reduces
the peroxide present and oxidizes the chromagen tetramethylbenzidine that is present in the pad. The result is a color change from the yellow chromagen to the green, oxidized chromagen.
What can cause myoglobinuria?
Traumatic: muscle injury, extreme exercise
Atraumatic: muscle ischemia, acute overdose
What are some reasons that a reagent strip blood test could be falsely positive?
Urine has been contaminated with menstrual blood or blood from hemorrhoids
Presence of strong oxidizing agents
What are some reasons that a reagent strip blood test could be falsely negative?
High nitrites or specific gravity
Presence of ascorbic acid
What is leukocyte esterase?
An enzyme that is found in azurophilic granules of granulocytic leukocytes
If leukocyte esterase is negative on reagent strip, does this mean there is no patient infection?
No, if the white blood cells that are present are lymphocytes, the pad will not react because lymphocytes do not contain granules that have this enzyme
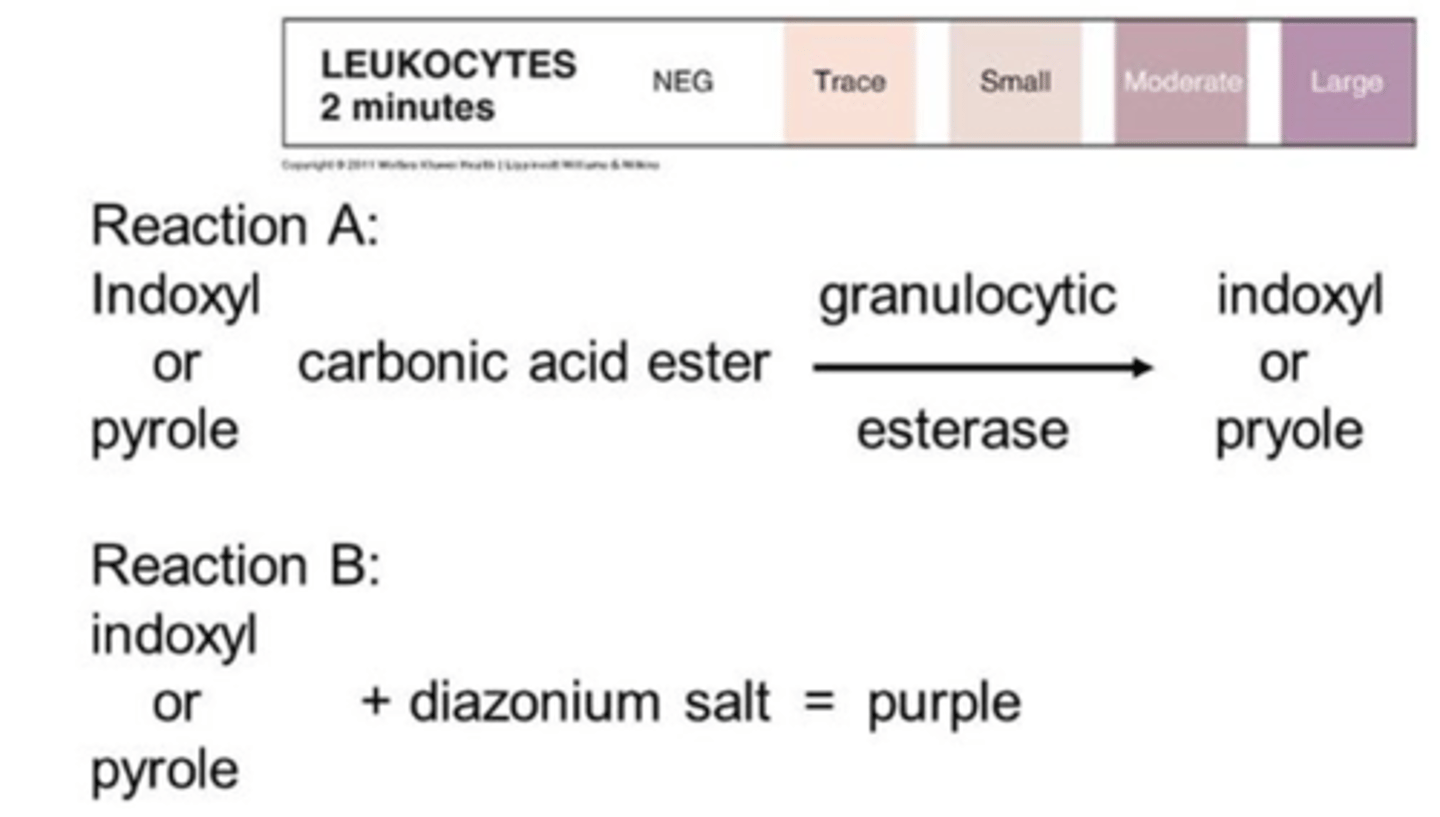
What is the principle of the reagent strip leukocyte esterase test?
Leukocyte esterase reacts with esters embedded in the pad to produce aromatic compounds. These aromatic compounds react with diazonium salts also present in the pad to produce a purple azo-dye, changing from beige to purple or violet
What are some reasons for false negative results on the reagent strip leukocyte esterase test?
Non-granulocytic WBC infection (mostly lymphs)
Strong oxidizing agents
Drugs
What are some reasons for false positive results on the reagent strip leukocyte esterase test?
Contamination - vaginal secretions, medications or foods that change color of urine
Does a negative nitrite rule out infection?
No, nitrite is simply a screening test used to detect nitrites produced by bacteria
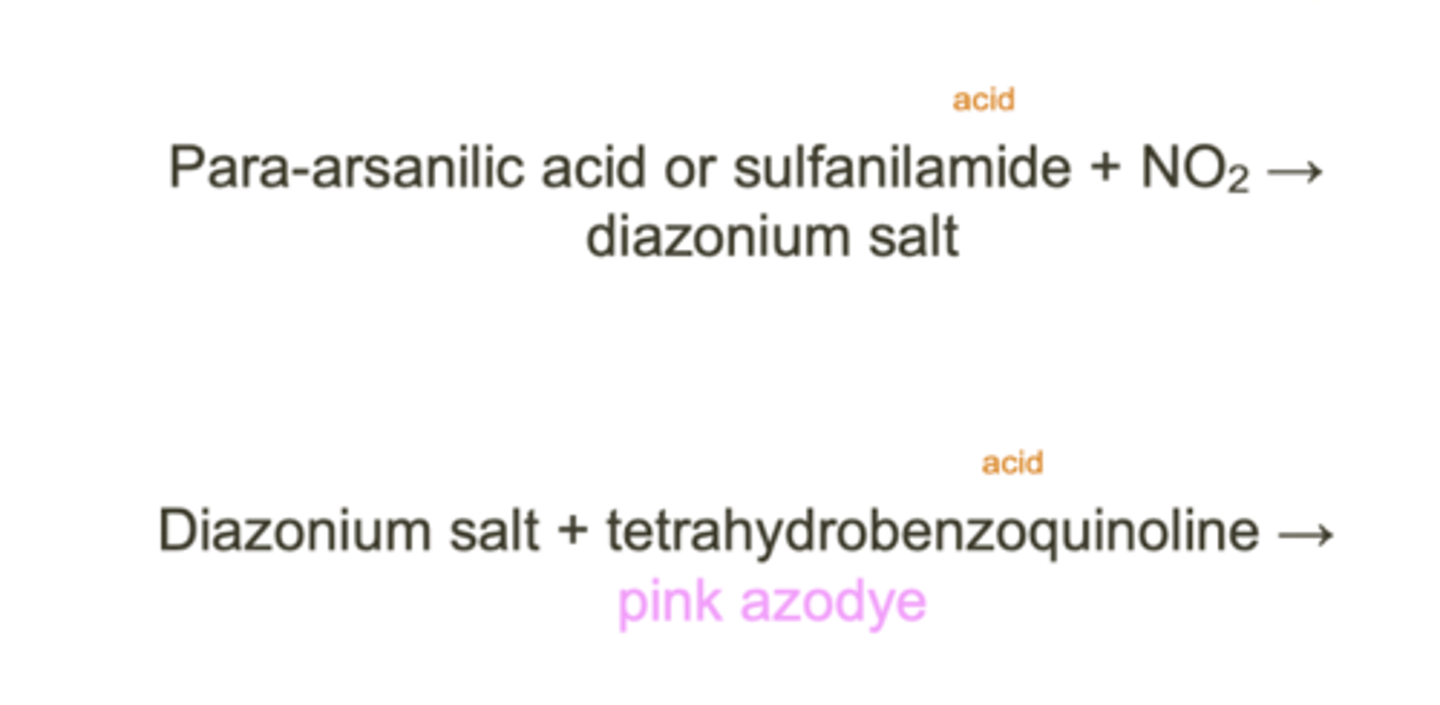
What is the principle of the reagent strip nitrite test?
If nitrites are present, they will react with an aromatic amine
embedded in the pad to form a diazonium salt. The diazonium salt will then react with another aromatic compound in the pad to form a colored (pink) azo-dye compound
What are some reasons for false positive results on the reagent strip nitrite test?
Colored substance interference (medications, beets)
Improper storage and bacterial proliferation
What are some reasons for false negative results on the reagent strip nitrite test?
Too fresh urine specimen (<4h)
Bacteria lacking nitrate reductase
Dietary nitrites
Ascorbic acid
What are some causes of acidic and alkaline urine?
Acidic - high protein diet, metabolic/respiratory acidosis
Alkaline - vegetarian diet, metabolic/respiratory alkalosis
What is pre-renal proteinuria?
AKA overflow proteinuria
Excess protein production leads to elevated concentration of proteins in the urinary filtrate. Because the concentration exceeds the renal threshold, small molecular weight proteins will end up in the urine
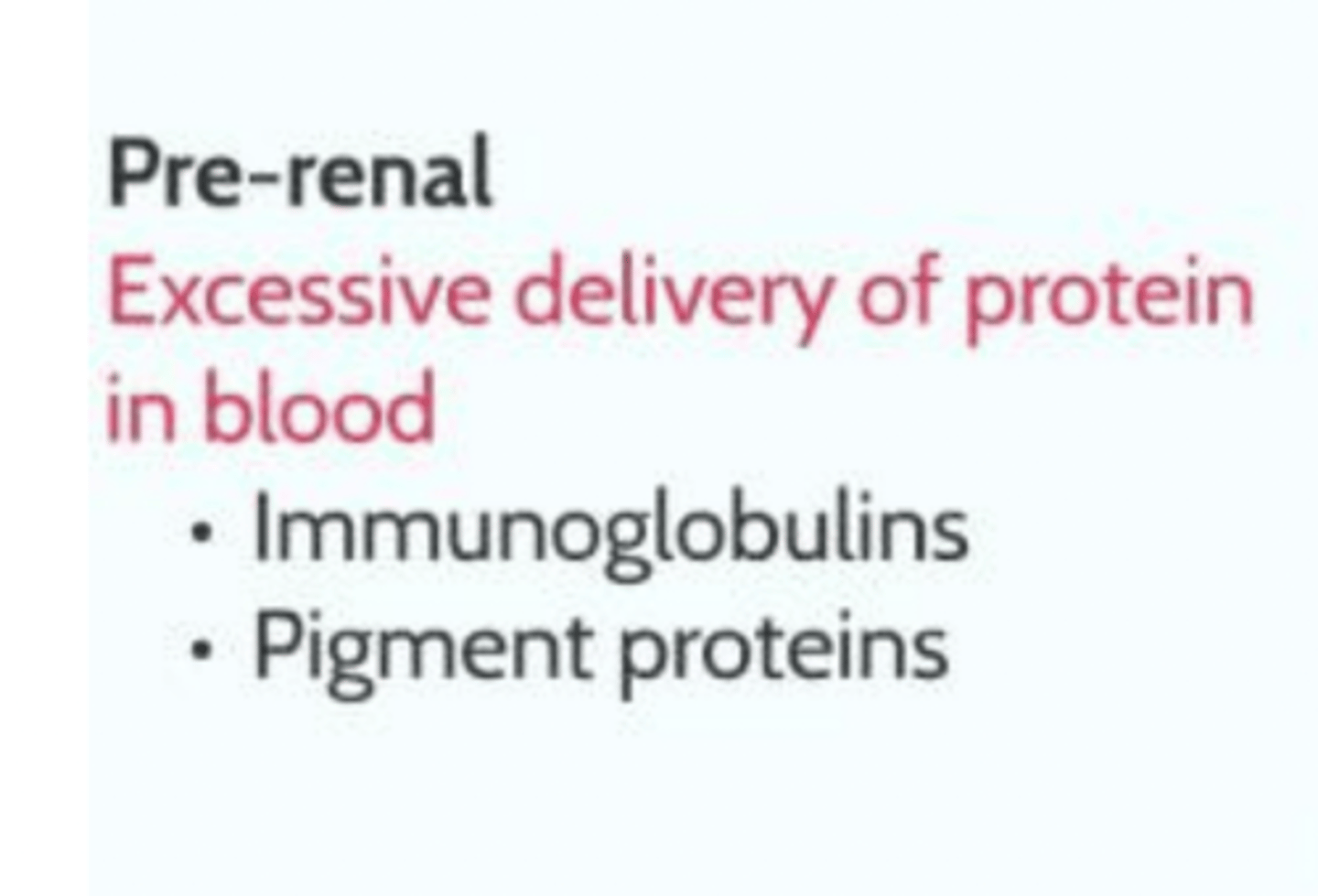
What are normal and abnormal proteins found in pre-renal proteinuria?
Normal: hemoglobin, myoglobin, acute phase proteins
Abnormal: immunoglobulin light chains
What is the difference between glomerular proteinuria and tubular proteinuria?
Glomerular - some type of damage to the glomerular filtration barrier, allowing proteins not normally able to pass through are now able to enter the urinary filtrate
Tubular - proximal tubules become damaged, and the proteins entering the urinary filtrate can no longer be absorbed. Because the glomerulus is functioning properly, it is only the low molecular weight proteins that are present
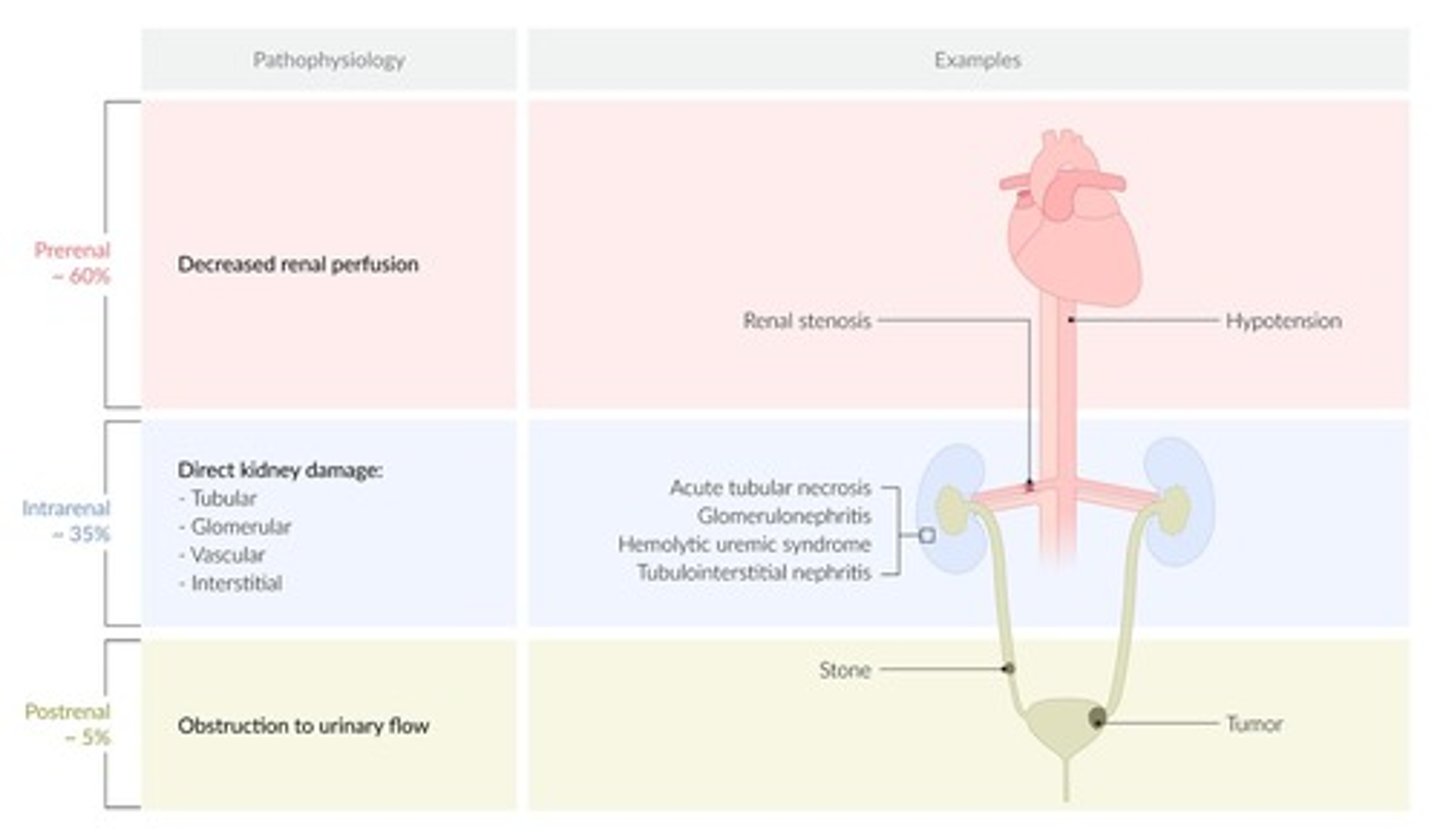
What are causes of glomerular and tubular proteinuria?
Glomerular - diabetes, lupus, sickle cell anemia, infectious disease
Tubular - heavy metal poisoning, hemoglobinuria, myoglobinuria
What is postural proteinuria?
Protein only gets into the urine when the patient is standing up. It is thought that being in an upright position increases the renal venous pressure, which results in the blood "backing up" which increases the pressure in the glomerulus
What is the principle of the reagent strip protein test?
Certain indicator dyes will release hydrogen ions when in the presence of proteins. The hydrogen ions are picked up by the proteins, so the pH of the pad isn't really changing, but the loss of the hydrogen ions by the indicator shows the presence of protein
What can cause false positive results in the reagent strip protein test?
Highly alkaline urine
Highly buffered urine
What can cause false negative results in the reagent strip protein test?
Non-albumin proteins present
What is post-renal proteinuria and what is its cause?
Proteins that enter the urine after it has already been formed
Due to infection, injury, kidney stones, or tumor
What are the causes of renal and pre-renal glycosuria?
Pre-renal - Glucose in the urine is not kidney related, and is the result of high glucose concentrations in the plasma (Diabetes, liver disease)
Renal - there is damage to the renal tubules so the glucose is not being resorbed into the blood (Fanconi's syndrome, pregnancy)
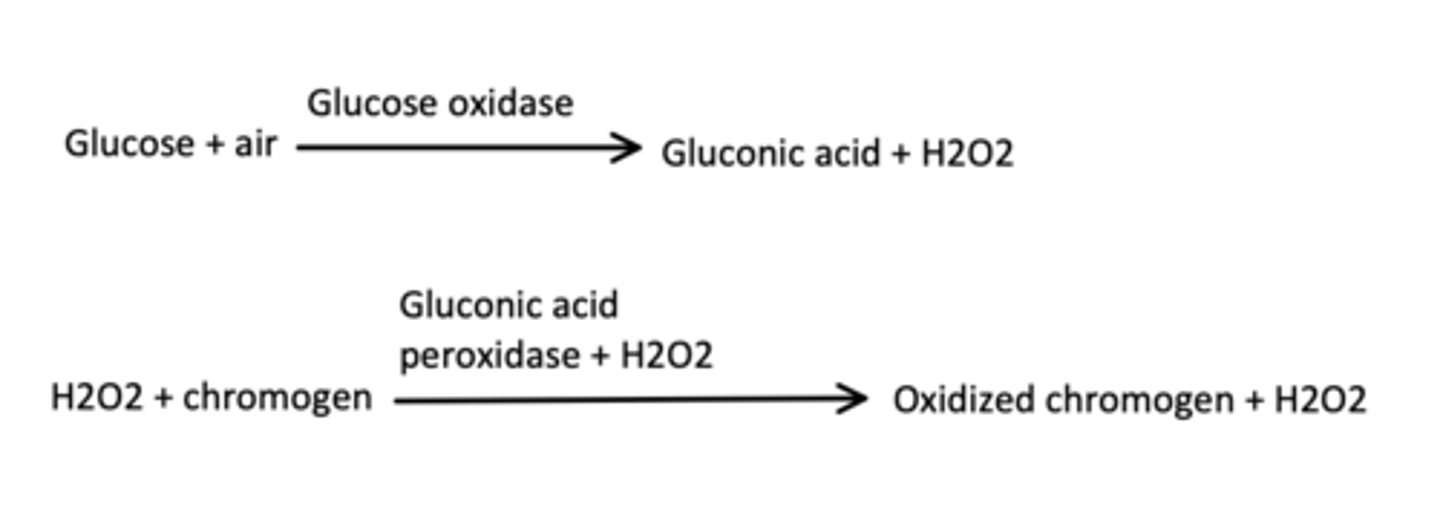
What is the principle of the reagent strip glucose test?
Glucose oxidase embedded in the pad reacts with glucose and oxygen to produce gluconic acid and peroxide. A second enzyme, peroxidase, will react with the peroxide and a chromagen that is also embedded in the pad to oxidize the
chromagen, producing a colored compound and water. Although the color develops because of the amount of peroxide present, the amount of color that develops is also directly related to the glucose concentration of the urine.
What can cause false positive results on the reagent strip glucose test?
Strong oxidizers, peroxide contamination
What can cause false negative results on the reagent strip glucose test?
Ascorbic acid
Improper storage
What is the principle of the reagent strip ketone test?
Acetoacetate reacts with nitroferricyanide (or nitroprusside) embedded in the pad to produce a purple color.

What can cause false negative results on the reagent strip ketone test?
Improper storage
What can cause false positive results on the reagent strip ketone test?
Compounds with free sulfhydryl groups (cancer drugs)
Highly colored urine
What is the principle of the Clinitest?
Reducing sugars (galactose, fructose, lactose) convert cupric sulfate to cuprous oxide
Detects larger quantities of glucose, but also other reducing sugars
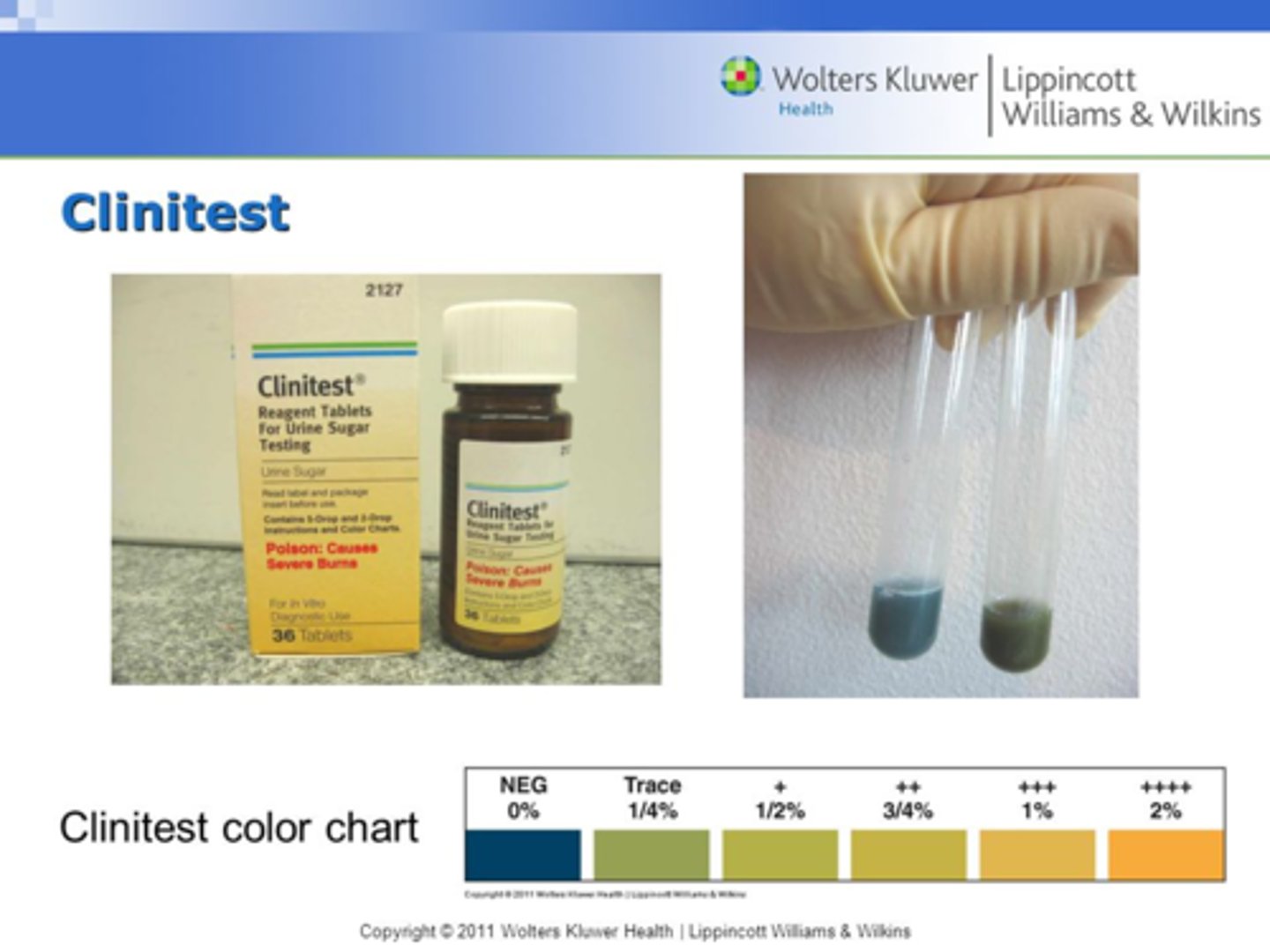
What is the pass through effect in the Clinitest?
The pass through phenomenon occurs when results are not read immediately at the correct time. When high concentrations of glucose or other reducing substances are present, the reaction "passes through" all of the colors, but the cuprous oxide form is then reoxidized to cupric oxide following exposure to room air after the CO2 gas above the mixture disperses. This results in the color changes back to a green color, indicating falsely decreased results when not read immediately.
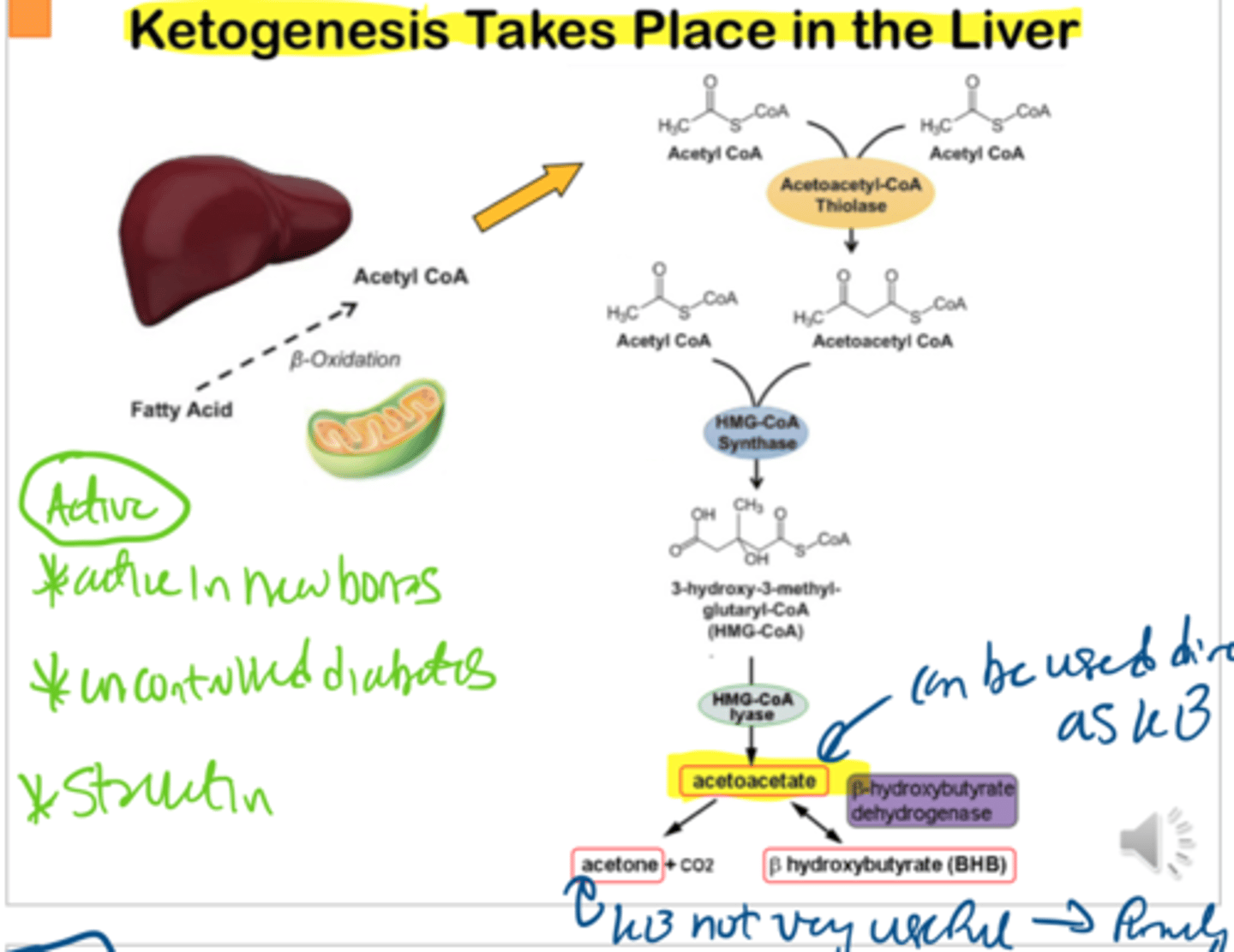
What are 3 causes of ketonuria?
Inability to utilize carbs available (diabetes mellitus)
Insufficient carb consumption (Starvation, diets, severe exercise)
Loss of carbs (Frequent vomiting, diarrhea, Fanconi syndrome)
What are the 3 major ketone bodies?
Acetoacetate (20%), acetone (2%), Beta-hydroxybutyrate (78%)
How are ketone bodies formed?
The liver converts glycerol on a triglyceride to acetyl-CoA, which are converted into ketone bodies in the TCA cycle
What is the Acetest?
A tablet that is used to detect ketones in urine, serum, and whole blood. Similar mechanism to reagent strip, except also uses glucine to aid in color change
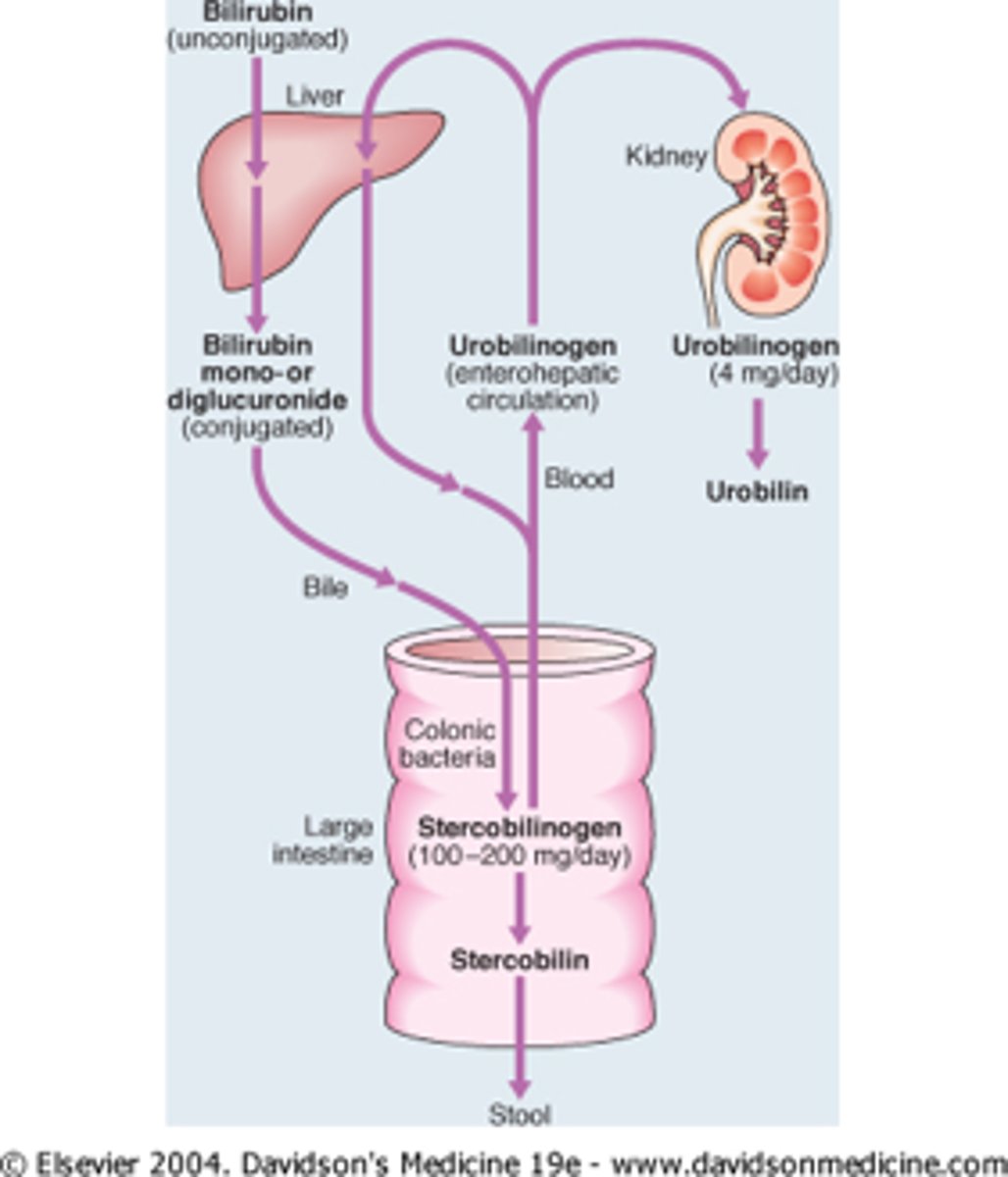
How is bilirubin formed?
Porphyrin ring is broken down into heme. Heme is converted to biliverdin and then unconjugated bilirubin
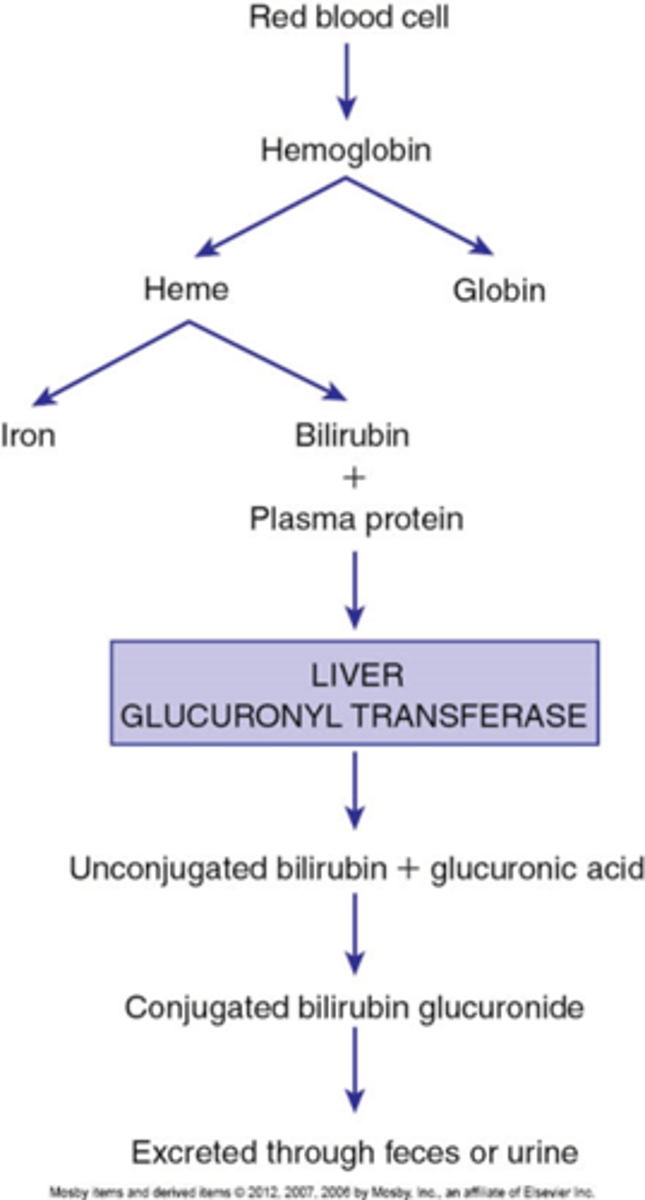
How is conjugated bilirubin formed?
Liver cells add a glucuronic acid to the unconjugated bilirubin, making it water-soluble and conjugated
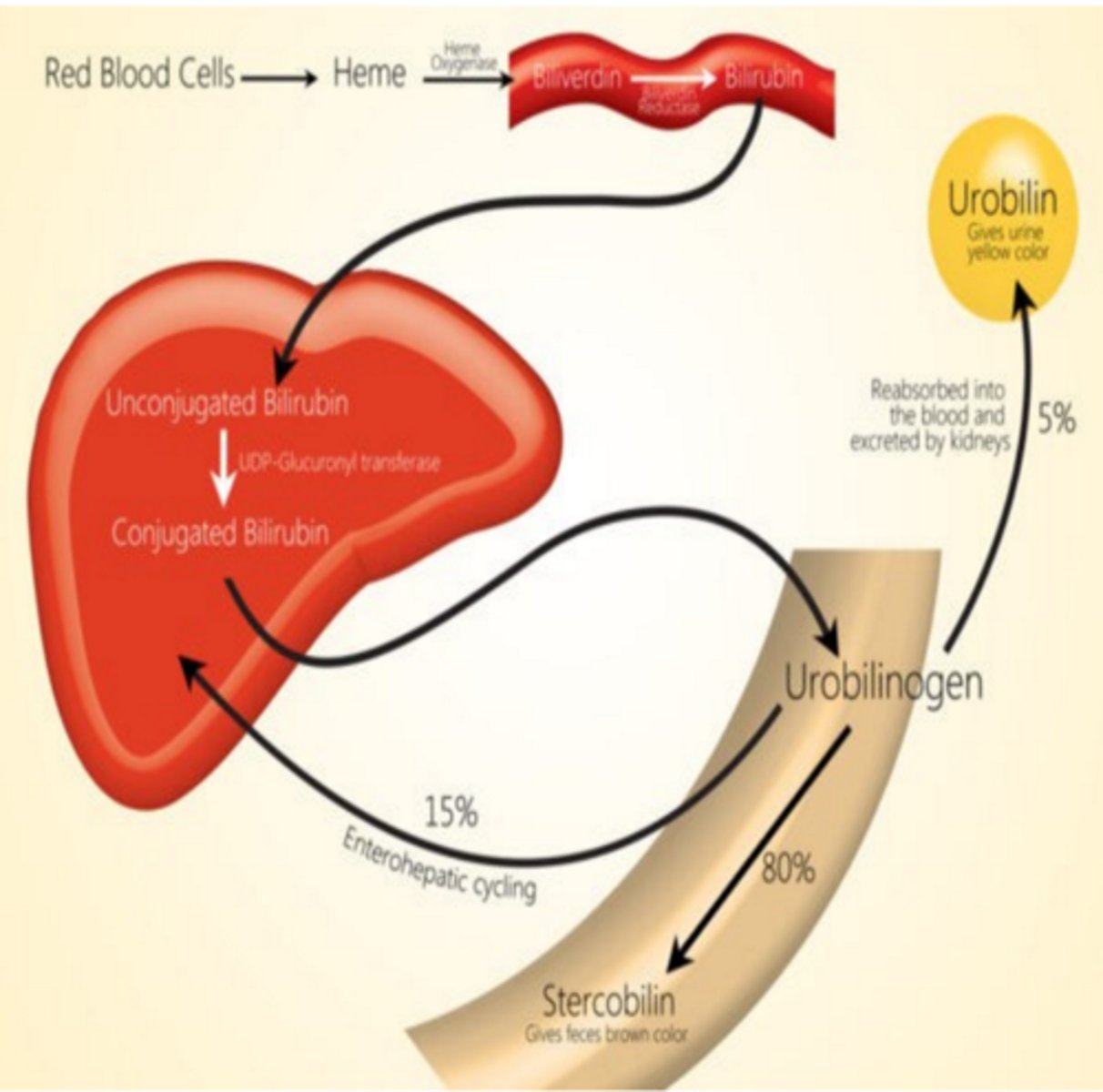
How is urobilinogen formed?
Intestinal bacteria convert conjugated bilirubin to urobilinogen
What is the principle of the reagent strip bilirubin test?
Bilirubin reacts with diazonium salt, to form azobilirubin, which can be brown to beige to pink in color, depending on the diazonium salt used and the amount of bilirubin present
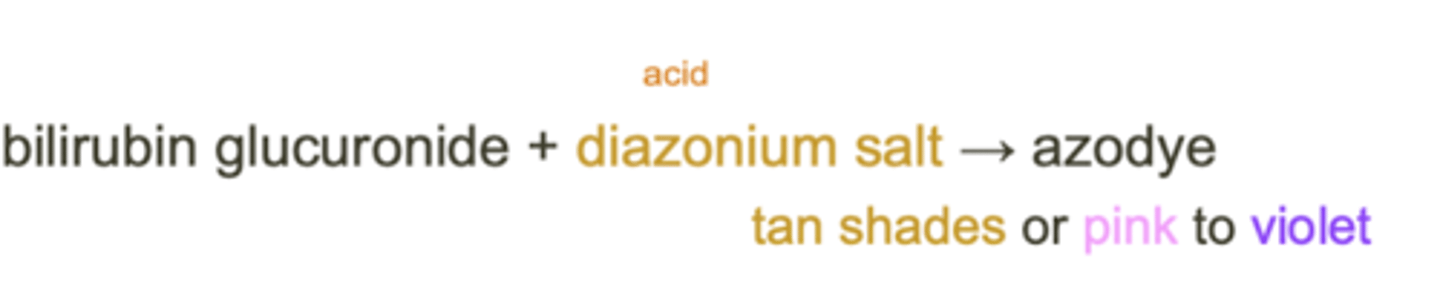
What can cause false negative results on the reagent strip bilirubin test?
Ascorbic acid
High nitrites
Improper storage
What can cause false positive results on the reagent strip bilirubin test?
Drug-induced (Pyridine)
What is the principle of the reagent strip urobilinogen test?
Urobilinogen reacts with an diazonium salt, causing red dye to appear
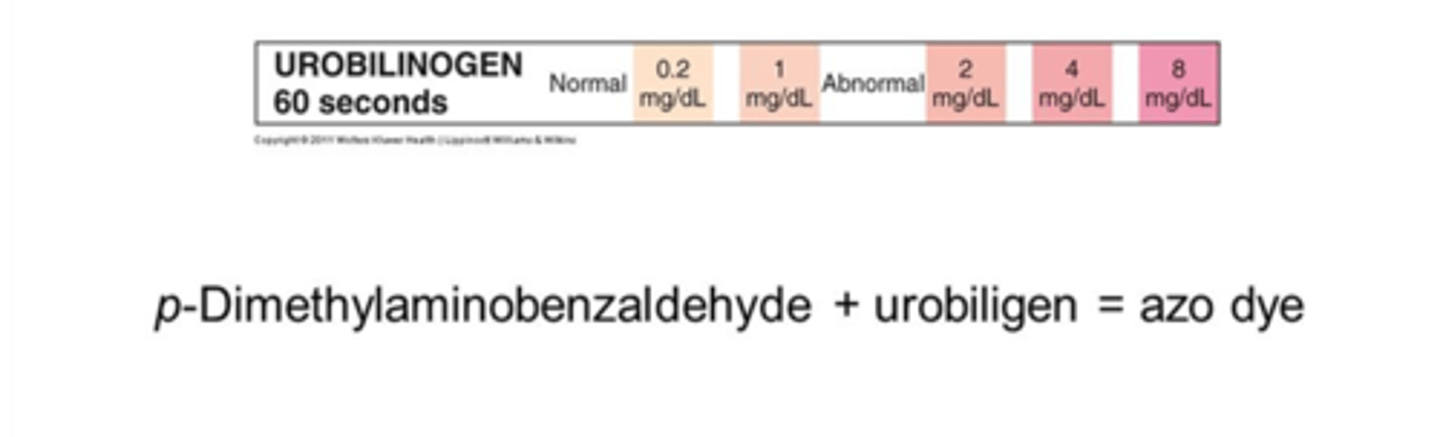
What can cause false positive results on the reagent strip urobilinogen test?
Highly colored urine
What can cause false negative results on the reagent strip urobilinogen test?
Improper storage
Formalin preservation
High nitrites
What is the principle of the reagent strip ascorbic acid test?
Ascorbic acid reacts with an oxidized chromagen, which will be reduced by ascorbic acid, changing the color
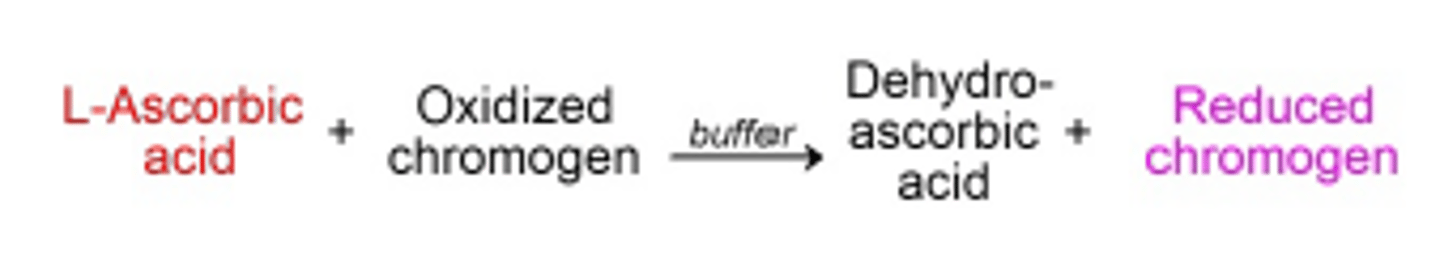
What is the significance of ascorbic acid testing in urine?
Vitamin C is a water soluble vitamin that is largely consumed and easily excreted in urine. It is a strong reducing agent and can cause interference in the reagent strip pads.
What tests may be affected by high concentrations of vitamin C?
Blood - > 9mg/dL
Bilirubin - > 25mg/dL
Nitrite - > 25mg/dL
Glucose - > 50mg/dL
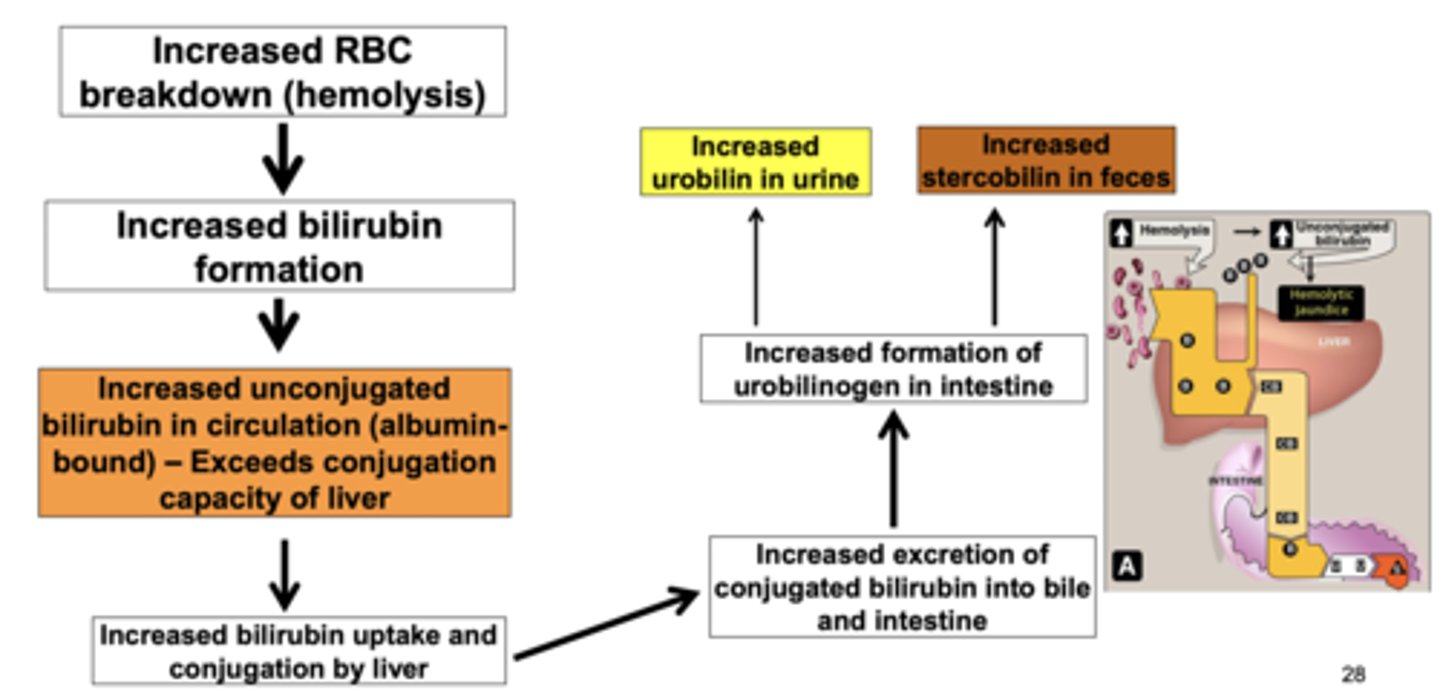
What are the metabolic changes in bilirubin and urobilinogen caused by prehepatic conditions?
Pre-hepatic = hemolytic conditions, thalassemia (typically no liver damage)
Bilirubin - Increased heme degradation, so increased unconjugated bilirubin; but urine bilirubin not increased (unconj. is not water soluble)
Urobilinogen - With no liver damage, the liver can handle the increased in unconjugated bilirubin, and converts it to conjugated bilirubin, but sends it straight into the small intestine via hepatic ducts to be broken into urobilinogen, which will be increased in the urine.
What are the hepatic metabolic changes in bilirubin and urobilinogen?
Hepatic = cirrhosis, hepatitis (damage to liver)
Bilirubin - Conjugated bilirubin enters intestines and bloodstream, allowing it to be filtered by the kidneys and excreted in the urine
Urobilinogen - may not be affected, could be slightly elevated in urine due to damaged liver's ability to resorb urobilinogen in the bloodstream
What are the posthepatic metabolic changes in bilirubin and urobilinogen?
Post-hepatic = blockage due to stones, tumors, or fibrosis
Bilirubin - blockage of the bile duct so conjugated bilirubin cannot enter the intestines, and will get "backed up" and leak into the bloodstream
Urobilinogen - Bilirubin is not able
to enter the intestines and no urobilinogen can be produced. This also means the feces will become acholic, which means they will be gray or clay colored
What factors can contribute to crystal formation in urine?
Solute concentration - when high specific gravity, higher likelihood of crystals
pH
Urine flow - less urine formed, glomerulus filters less, slow filtering causes increased formation
Temperature - cooling of the urine will initiate precipitation of crystals in urine
What is the etiology of amorphous crystals?
Rapid cooling of urine before compounds precipitate out and form an organized structure
How can you differentiate amorphous phosphates and urates?
Urates - pH 5.5 - 7.0 (acidic)
Phosphates - pH > 7 (alkaline)
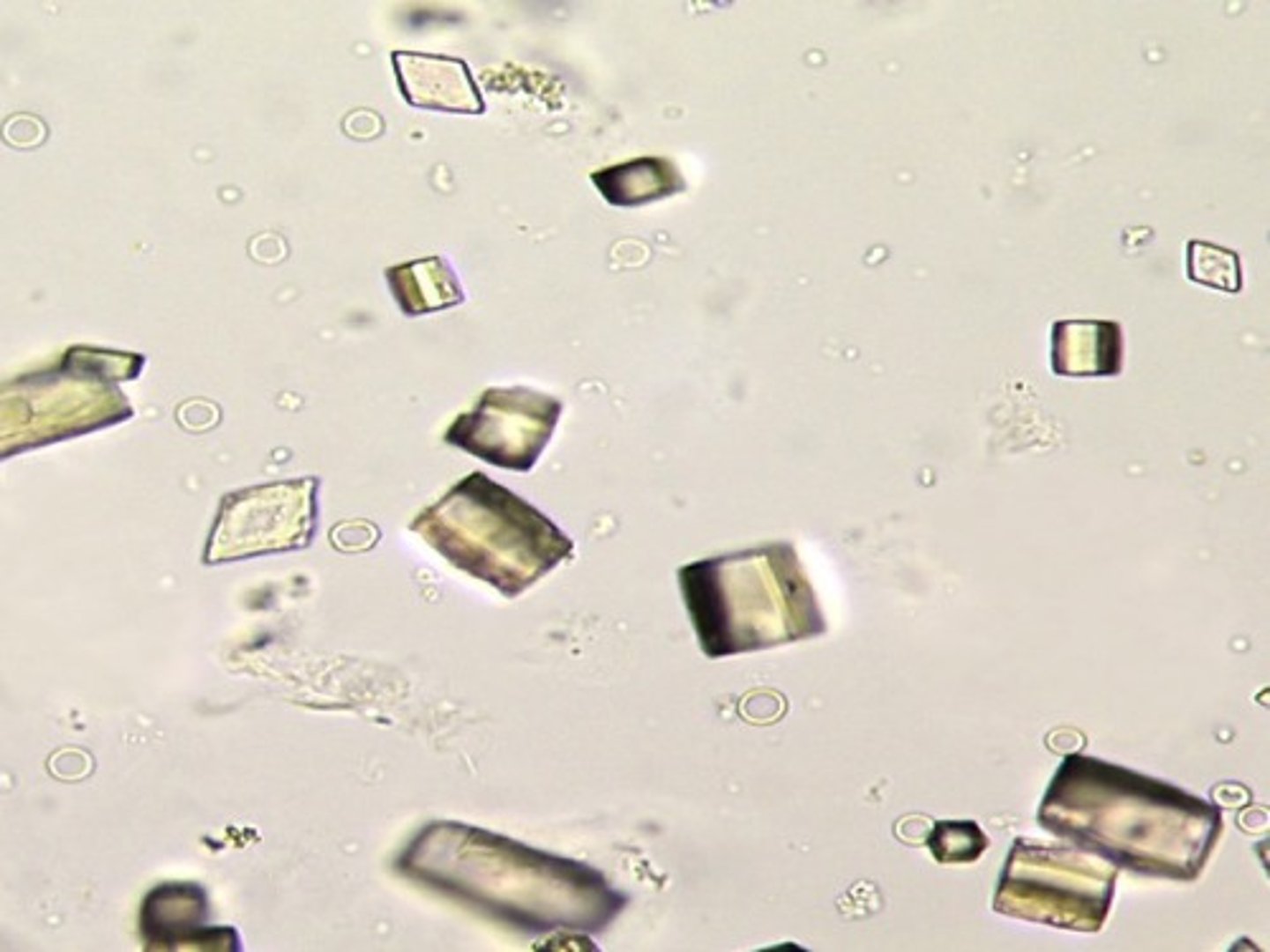
What are the two types of calcium oxalate crystals?
Monohydrate - round/ovoid, refractile; polarizes light
Dihydrate - envelope with X; more common
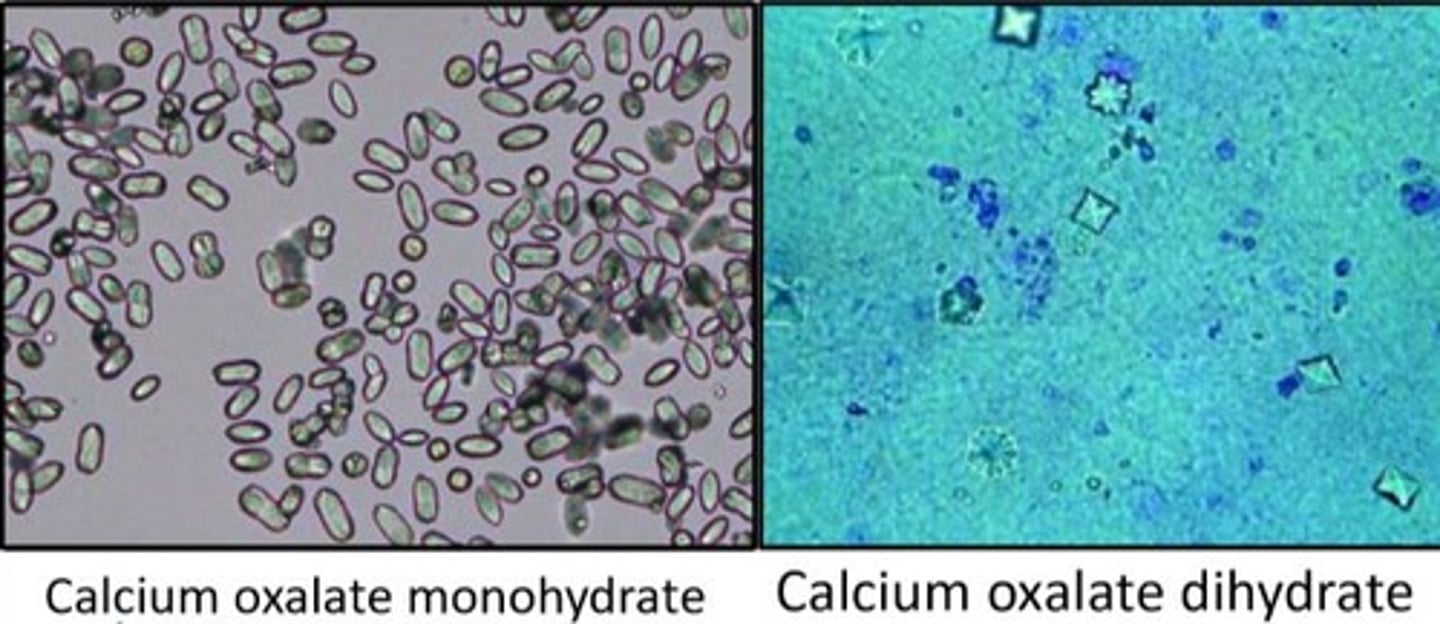
What causes calcium oxalate formation?
Metabolism of ascorbic acid
Cocoa, tea, coffee, and chocolate metabolism
Ethylene glycol poisoning
What pH do calcium oxalate crystals form at?
any pH
What pH do acid urates and monosodium urate crystals form at?
> 7.0
What pH do uric acid crystals form at?
5.5 - 7.0
What is the appearance of uric acid crystals?
Yellow-brown
Lemon, barrel, rosette, cubes