Drugs, Anxiety & Schizophrenia
1/151
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
152 Terms
What is the lifetime incidence of MDD and Schiz?
MDD = ~15-20%
Schiz = 1%
Name 3 drugs that has been used historically?
Iproniazid - first MAOI introduced 1957 which was developed for TB in the early 1950's
Imipramine - first TCA introduced in 1957/8 first developed for schizophrenia
Reserpine (antihypertensive and antipsychotic): an indole alkaloid which depletes monoamines via its action on vesicular monoamine transporters (VMAT's)
This therefore causes depression as it reduces amount of monoamines in the synapse
Whole basis around treatment = monoamine transmission
What are the risk factors of depression?
Gender - females, even higher during reproductive years
Age - Younger onset, shorter duration. Oldies less prevalence but increasing
Marital status - Highest in separated, then widowers, then divorced females
Socio-economic factors: social class 3 has a higher incidence than social class 1 and 2. Higher in rented accommodation, highest in homeless.
Ethnicity - Highest in asian females then white then black
Males - No difference between race
Depression definition
Refers to a wide range of mental health problems characterised by:
The absence of positive effect (anhedonia: loss of interest and enjoyment in ordinary things and experiences.),
Low mood
A range of associated emotional, cognitive, physical and behavioural symptoms
What are 3 elements contributing to depression severity?
3 elements
Symptoms (which may vary in severity and frequency)
Duration of the disorder
The impact on personal and social functioning
Personal functioning - when an individual is able to effectively engage in normal activities of daily living and can react to experiences
Social functioning is the ability to interact with other people, develop relationships and gain from and develop these interactions.
Classification of Depression severity
Sub-threshold - less than 5 symptoms
Mild - Excess of 5 symptoms and minor functional impairment
Moderate - Symptoms of functional impairment are between mild and severe
Severe - Most symptoms and they interfere with functioning
How are new episodes of depression defined/scored?
Less severe - encompasses sub-threshold and mild depression (<16 on PHQ-9 scale)
More severe - encompasses moderate and severe depression (>16 on PHQ-9 scale)
What are 3 key symptoms?
Lowered mood
Anergia - lack of energy
Anhedonia - No longer enjoys previously enjoyed
What are other symptoms? Sam Smith Sucks Willy For Anxiety, Praise Liam
Sleep pattern interference
Self-harm
Sexual dysfunction
Weight changes
Feelings of guilt
Anxiety
Psychotic features
Loss of self-confidence
3 things that can cause depression
Physical
Causative or exacerbated from depression
Organic causes like chronic pain
Latrogenic - Prescription drugs
BB
Opioids
Corticosteroids
Loss and regret
Jobless, homeless, no bitches yute
Treatment considerations for depression:
Carry out assessment of need
Develop a treatment plan
Take into account physical health problems and coexisting mental health problems
Discuss what factors would make a person more likely to engage with treatment - positive/negative experiences
Account for previous treatment history
Address any barriers to the delivery of treatments because of any disabilities, language or communication difficulties
Ensure regular liaison between healthcare professionals (as well as specialist support if the patient is receiving this)
When prescribing what info must be provided to pt.?
SE from first few doses and what they are
How long it takes to see an effect (~4 weeks)
When their first review will be (usually within first 2 weeks)
Importance of following instructions and how to take the medication
Why regular monitoring is required and how often they need to attend reviews on their medications
Treatment for 6 months after remission but reviewed regularly
Persisting SE throughout treatment
Withdrawal symptoms and how to minimise them
What is the stepped care for depression (NICE guidance)?
Depending on the severity and duration of their depression, there is stepped treatment for increasing risk
All known and suspected presentations of depression
Treatment of persistent sub-threshold depressive symptoms, mild to moderate depression
Persistent sub-threshold or mild to moderate depression that has failed to respond to initial interventions;’ moderate or severe depression
Severe and complex depression; risk to life; severe self-neglect
Step 1
Screen individuals for depression using validated assessment tools such as the Patient Health Questionnaire-9 (PHQ-9)
Establish a diagnosis of depression based on clinical criteria and severity of symptoms
Step 2
Mild patients: watchful waiting
Patient does not want treatment or may recover without further intervention, re-assess in two weeks
CBT
Encourage therapy
Some Antidepressant use
Not recommended as SE likely but efficacy maybe = risk
Step 3
AD routinely offered to all patients
Key Medication counselling points
Addiction
Potential SE
Discontinuation symptoms
Delay in full benefit
Consider referral
Monitoring risk
Pts. at high risk of suicide or younger than 30 - follow up weekly
Prescribe limited AD
Monitor for increased signs of anxiety, agitation and akathisia
Step 4
HIGH RISK PTs.
Assess symptoms, suicide risk, treatment history
Refer to specialist mental health services
STAR*D treatment for TRD patients
Treatment of depression 1st line and something not recommended by NICE
First line - SSRIs (Citalopram, Sertraline and Fluoxetine)
similar effectiveness to TCA (Amitriptyline) and less chance of SE and toxicity
St John’s Wort not recommended by NICE due to lack of evidence and efficacy in severe MDD
Induce CYP450 for toxicity of drugs like anticonvulsants
How to treat relapsing pts.?
50-80%
Therefore medication should be continued for 2 years for people who have had 2 or more episodes in the recent past and have suffered functional impairment during these episodes
Patients on maintenance treatment should then be revaluated after two years (taking into account age, co-morbidities and other risk factors)
Maintenance dose = the dose that achieved remission
MOA of AD (In detail further down in anxiety)
Almost all antidepressants increase either
Seratonin
Noradrenaline
Reuptake inihibition in post-synapse
So more to bind to receptors
Common side effects of SSRIs/SNRIs
Nausea
Vomiting
Agitation
Akathisia
GI upset
Hyponatraemia
Sexual dysfunction
Panic attacks
Serotonin syndrome
Common side effects of TCAs
Dry mouth
Anticholinergic
BP disturbances
Hyponatraemia
Discontinuation/serotonin syndrome
Sedation
Common side effects of NARIs (Reboxetine)
Dry mouth
Constipation
Sweating
Insomnia
Anxiety
Agitation
MAOIs food interaction problem
Food and drug interactions which can result in HTN crisis
What to do when pt. fails to respond to initial AD?
Ensure it was taken as prescribed
If so and SE were tolerable, increase dose
If no response after a month consider switch in AD
Choices for second-line AD:
Another SSRI
SNRI - Duloxetine
MAOIs
TCAs
Other treatments due to limited pharmacological response
Adding a group exercise intervention
Switching to psychological therapy
Changing to a combination of psychological therapy
CBT
Interpersonal psychotherapy (IPT)
Medication
What is treatment refractory depression?
Diagnosis made when a patient is unresponsive to two or more medications, given sequentially
70% will respond to the initial AD
30% - half of these people will respond to a second AD
Treatment refractory sub-population = 15%
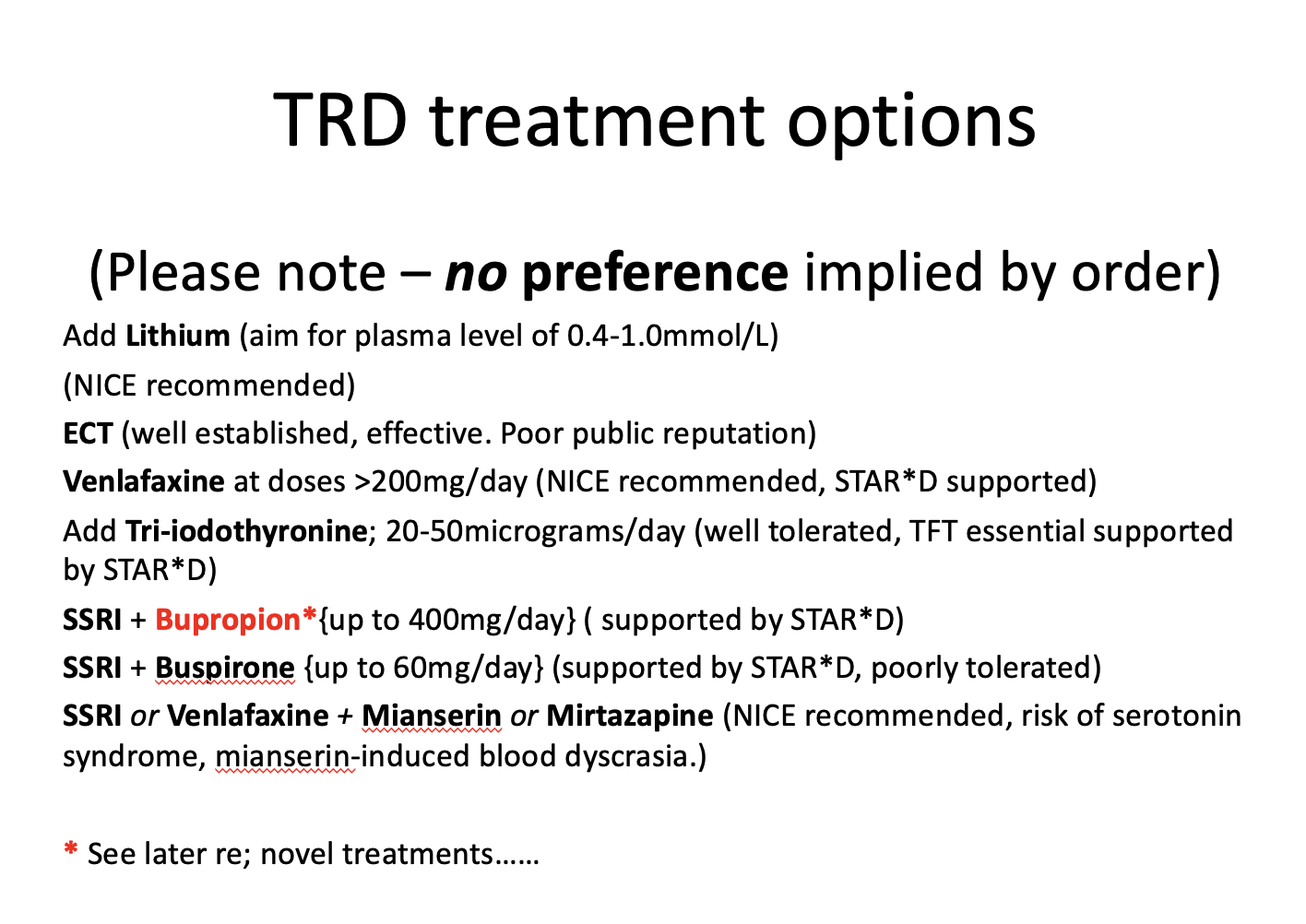
What are TRD treatment options?
MOA of Buspirone
Neuromodulator of serotonin
Presynaptically, buspirone's partial agonism at 5-HT1A receptors inhibits release of serotonin regulating serotonin levels in the brain, preventing excessive serotonin release
Postsynaptically, buspirone's partial agonism at 5-HT1A receptors enhances serotonin neurotransmission in certain brain regions = antidepressant & anxiolytic effects
Why is the serotonin theory obsolete?
Tryptophan depletion does not cause/worsen depression
Levels of HIAA do not correlate with depression
Patients with depression do not have reduced levels of 5HT in plasma
No. of post-synaptic 5HT-1a receptors is not increased in people with depression
Genetic polymorphism with subjects having variations in SERT molecules has no effect on depression
Which is the best antidepressant?
No singular AD is better than any other
Best antidepressant is the one that works best for individual patient, differs from person to person
Also depends on willingness
Which AD work the fastest?
Esketamine
Ketamine
Dextromethorphan + Bupropion
DMX is an uncompetitive antagonist of the NMDAR and a sigma-1R agonist
Bupropion inhibits DMX metabolism as DMX alone is rapidly and extensively metabolised
How do AD’s work?
Increase amount of certain chemicals that influence working of CNS
This is monoamine theory of depression as chemicals involved are monoamine neurotransmitters
Are they AD’s addictive?
Not addictive from a point of fixation or dose adjustment, however when patient stops they can experience withdrawal symptoms
AD discontinuation syndrome
Flu like symptoms
Gastrointestinal effects
Anxiety
Sleep disturbance
Panic attacks
Manage by reducing therapy gradually and reassure patients symptom won’t persist and not indicative of relapse
Can you drink alcohol on AD?
Alcohol can potentiate sedative effects of certain AD
CNS depressant
Consumption strongly associated with suicide
How is libido affected in depression?
Decrease in libido could be emergent symptom
Need to get baseline to double check if this could have been caused by AD
What do you give to a patient with Closed angle glaucoma? What is contraindicated in CAG?
Cannot give TCA as contradicated
Give SSRI instead like citalopram as first line and safest
What can a lack of asthma control and steroid use lead to?
Depression
Name types of anxiety disorders and subtypes and lifetime prevalence of GAD
Specific phobia - Marked fear or anxiety about something specific 6/12
Agoraphobia - Marked fear or anxiety about situations where escape is difficult
Leads to avoidance of situations like being alone in or outside home
Social anxiety disorder - Persistent fear about 1 or more social situations 6/12
Selective mutism - consistent failure to speak in social situations when there is expectation to do so
GAD - Excess worry about number of events or activities and difficulties controlling this 6/12
Panic disorder - Recurrent unforeseen panic attacks
Repeated unpredictable attacks of severe anxiety occurring without warning unrelated to specificity
Can be combined with GAD
Separation anxiety disorder - Excessive fear or anxiety focussed on separation from home or figures 1/12 children, 6/12 adult
5% lifetime incidence
Why is differentiation between disorders difficult?
Can be a co-morbidity with other anxiety disorders or depression and other affective disorders
Like depression, NICE adopts stepped care model
What is step 1 of the stepped care model?
All known and suspected presentation of GAD, identification and assessment
Education about GAD
Treatment options
Active monitoring
What is step 2?
Diagnosed GAD that has not improved after education and active monitoring in primary care
Individual non-facilitated self help
Individual guided self help
Psychoeducational groups
What is step 3?
GAD with inadequate response to step 2 interventions or marked function impairment
Choice of high intensity psychological intervention
Drug treatment
What is step 4?
Complex treatment refractory GAD and very marked functional impairment such as self neglect or high risk of self harm
Highly specialist treatment
Crisis services
Day hospitals
Inpatient care
What 3 groups of adults are likely to be affected by GAD?
Aged between 35-54
Divorced or separated
Living alone or as lone parent
Anxiety risk factors: Poor Cuban Families Find Young Children Personally Stressful
Family history
Childhood adversity
Stressful life events
Personality traits like excessive worrying
Certain parenting styles
Over protectiveness
Lack emotional warmth
Younger age
Female, unmarried or unemployed
Poor physical or mental health
What are 6 presenting symptoms? PPI Claims Are Annoying
Apprehension
Cued or spontaneous panic attacks
Irritability
Poor sleep
Poor concentration
Avoidance
What is Agoraphobia?
Anxiety about being in places or situations from which escape may be difficult or embarrassing, or where help may not be available in the event of a panic attack.
This type of anxiety usually leads to a pervasive avoidance of a verity of situations
Being alone outside the home
Being home alone
Being in a crowd full of people
Travelling by car, bus or plane
Being on a bridge or in a lift.
What is Panic disorder?
Repeated unpredictable attacks of severe anxiety occurring without warning, unrelated to a specific situation
Can peak within 10 minutes with many somatic or physical symptoms
Can be combined with GAD or phobic disorders
What is GAD?
A persistent, excessive anxiety, apprehension or worry present for at least 6 months
Chronic condition with acute episodes
Often begins in early adulthood
Twice as common in women than men
Explain Phobic disorders
Irrational fear out of all proportion to situation or object
Recognised as excessive but cannot be reasoned away
Sub-divided into agoraphobia, social phobia
What is OCD?
Obsessive compulsive disorder
Time consuming obsession and compulsion
Males and females equally effected
Prevalence = 2%
What is PTSD?
Intense and prolonged, can be delayed response to specific traumas
Characterised by emotional numbness, flashbacks, recurring memories and vivid dreams
Symptoms in anxiety
Symptoms in anxiety
Dry mouth
Hyperventilation
Palpitations
Difficulty breathing
Thoughts of worry
Fatigue
Dizziness
Sweating
Sleep disturbances
GI discomfort
Anxiety relationship with stress
Anxiety naturally exists as means of overcoming or responding to stress
An optimal level of anxiety allows us to perform at high level
In disorders, anxiety remains after stress has ceased
2 brain systems involved in fear and anxiety
Defence system: responds to both learned and unlearned threats, initiates fear, fight, flight, freeze behaviour
Behavioural inhibition system: Responsible for avoidance behaviour, a neurobehavioral system thought to regulate negative affect and avoidance behaviour in response to threats or punishment
Neuro aspects of anxiety
Techniques such as PET-scanning have demonstrated altered neuronal pathways especially in limbic regions
E.g. increased activity in the amygdala (fear response)
Hippocampus (memory regulation including stressful memories)
Note also that there is a dense concentration of serotonergic and noradrenergic synapses and systems within limbic regions.
What happens in the brain with patients with GAD?
Exhibit increased metabolic rates in occipital, temporal and frontal lobes as well as cerebellum and thalamus compared with healthy individuals
What is the general management of anxiety disorders?
Shared decision making between patient and HCP helps promote concordance and optimises outcomes
Appropriate and usable information should be given to patients, carers and family - including med info
Patients family should be informed of all appropriate self-help
What are 3 treatment options?
Self help
Psychological therapy
Pharmacological therapy
What is the pharmacological treatment?
SSRI
Consider giving sertraline first as cost effective
Informed consent must be obtained and documented
Monitor closely for adverse reactions
What is Sertraline licensed and indicated for the treatment of?
MDD
Panic disorder
OCD in adults
Social anxiety
PTSD
What if Sertraline is ineffective?
Offer alternative SSRI/ SNRI
Can produce withdrawal syndrome e.g. venlafaxine
SE profile and potential for drug interactions
Increases risk of suicide and likelihood of toxicity in overdose e.g. venlafaxine
Persons prior experience of treatment with individual drugs
What pharmacological treatment options are there?
BDZ
SSRIs
Pregabalin
Antipsychotics
Beta-blockers
Antihistamines
How do BDZ work and how they are used responsibly ?
Act on GABA-A receptors
Short term relief (2-4 weeks) for anxiety that is severe, disabling or causing extreme distress NOT PRIMARY CARE
Used as immediate care for patients awaiting other treatments
How do SSRIs work?
Inhibits reuptake of serotonin at post-synaptic membrane
Increases central serotonergic activity
Onset of action may not appear for 6 weeks and full response from drug may take 12 weeks
How do ADs work in anxiety?
Serotonin facilitates defensive responses to potential threat which is related to presentation of anxiety - basal forebrain (amygdala)
Desensitises 5-HT2c receptors and increased stim of 5-HT1a receptors resulting in less activation of amygdala, medial PFC and insula
Other treatments for anxiety
Beta blockers - only to treat somatic or physical symptoms
Buspirone - complex MOA (partial 5HT 1A agonist, acts on both Noradrenergic and Dopaminergic pathways)
takes time to work (1/12 minimum)
better than placebo, worse than BDZ in terms of efficacy and tolerability (drug interactions with CYP450 3A4 inducers + inhibitors)
Sedating antihistamines - e.g. high dose hydroxyzine (not recommended)
Antipsychotics - specifically used in PTSD and occasionally OCD
E.g. olanzapine, risperidone, quetiapine (not used routinely in GAD)
Social anxiety disorder and PTSD - valproate and carbamazepine (rarely used)
How does Pregabalin work?
Binds to a2-∂2 protein of v-g Ca channels in CNS, causing conformational changes and reducing excitatory transmission
Rapid onset of action
Reduced dose in renal impairment
Use when SSRI/SNRIs aren’t tolerated
Monitor for misuse
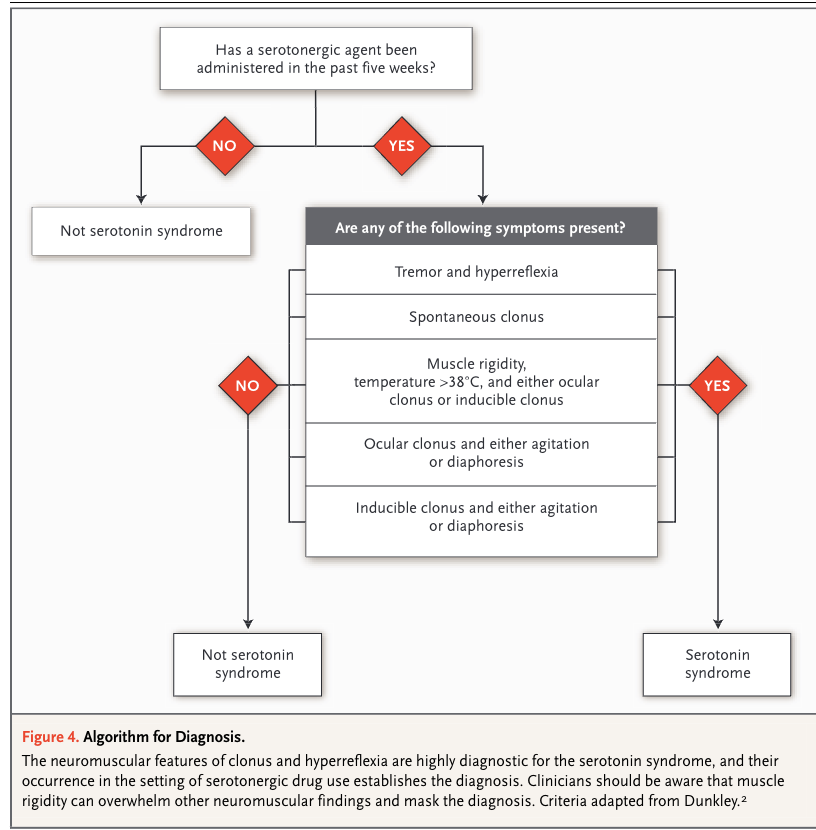
How to diagnose Serotonin syndrome
What is Schizophrenia
Signs and symptoms can include disorders of perception(hallucinatation), inferential thinking(Deluluuu), goal-directed behaviour and emotional expression
No single symptoms or signs can be considered as specifically characteristic or indicative of schizo
All pts. experience different symptoms
Chronic illness that may progress through several phases
Aetiology of Schizophrenia
Alteration in brain structure
Enlarged cerebral ventricles
Cortical thinning
Decreases size of anterior Hippocampus
Changes in neurochemistry - change in neurotransmitter activity
Recently demonstrated genetic risk factors
Explain neurodevelopmental vulnerability and its relation to schizophrenia
Schizophrenia occurs more often in patients with changes/ difficulties in their cognitive/ memory/ social/ focus skills and the combination of these with environmental stressors can cause schizophrenia.
What childhood factors can influence disease onset in adulthood?
Genetic predisposition
Intrauterine, birth or postnatal complications
Viral CNS infections
Childhood trauma and neglect
Genetic predisposition (chances)
First degree relative with schizo have 10-12% risk of developing schizo
Monozygotic twins = ~45%
Environmental Stressors
Can trigger emergence or recurrence of psychotic symptoms in vulnerable people
May be mainly pharmacologic
Can be social
Environmental events can initiate epigenetic change that could influence gene transcription and disease onset
Types of protective factors
Strong psychosocial support
Well-developed coping skills
Antipsychotic medication
When do patients display psychotic symptoms
8-15 months before presentation in medical care
Can be recognised earlier now
What do symptoms of schiz impair
Ability to perform complex and difficult cognitive and motor functions.
This means they usually interfere with work, social relationships and self-care
Common outcomes can include:
Unemployment
Isolation
Deteriorated relationships
Diminished quality of life
5 Phases of Schizophrenia
Prodromal phase
Advanced prodromal phase
Early psychosis
Middle phase
Late illness phase
Prodromal Phase
Individuals may show no symptoms or may have
Impaired social competence
Mild cognitive disorganisation
Perceptual distortion
Anhedonia
Other general coping difficulties
Advanced prodromal phase
Subclinical symptoms may emerge
Withdrawal or isolation
Irritability
Suspiciousness
Unusual thoughts
Perceptual distortions
Disorganisation
Onset can be sudden or very slow
Here <40% pts. convert to full schizo
Early psychosis
Symptoms are usually active and at their worst
Middle phase
Symptomatic periods may be episodic
Can also be continuous where functional deficits tend to worsen
Late Illness Phase
Illness pattern becomes more established but there is considerable variability
Disability may stabilise, worsen or diminish
Symptom categories in schizophrenia
Positive: Hallucinations and delusions
Negative: Diminution or loss of normal function and affect
Disorganised: Thought disorder and bizarre behaviour
Cognitive: Deficit in memory, info processing and problem solving
Positive Symptoms of schizophrenia
Delusions: Erroneous beliefs that are maintained despite clear contradictory evidence
Persecutory: Tormented or followed, tricked or being spied on
Delusions of reference: patients believe that passages from books, on-line posts, TV, radio, newspapers, song lyrics or other environmental cues are directed at them
Delusions of thought withdrawal or thought insertion: patients believe that others can read their mind, that their thoughts are transmitted to others
Hallucinations
Sensory perceptions that are not perceived by anyone else
Auditory, visual, olfactory, gustatory or tactile
Auditory hallucinations are most common
Negative symptoms of schizophrenia
Blunted affect: patients face appears immobile, poor eye contact and lack of expressiveness
Poverty of speech: patient speaks little and gives terse replies to questions, creating impression of inner emptiness
Anhedonia: Lack of interest in activities and increased purposeless activity
Asociality: lack of interest in relationships
Disorganised symptoms
Thinking is disorganised with rambling, non-goal directed speech that shifts from one topic to another
Speech can be incoherent and incomprehensible
Bizarre behaviour may include childlike silliness, agitation and inappropriate appearance, hygiene or conduct
Catatonia
Cognitive Symptoms
Attention
Processing speed
Working and declarative memory
Abstract thinking
Problem solving
Understanding of social interactions
Subtypes of schizo
Classified into
Deficit
Non-deficit
Based on presence and severity of negative symptoms such as:
Blunted affect
Lack of motivation
Diminished sense of purpose
Deficit of schizo
Negative symptoms unaccounted for by other factors e.g
Depression
Anxiety
Under-stimulating environment
Drug adverse effects
Non-deficit of schizo
May have delusions, hallucinations and thought disorders
Relatively free of negative symptoms
How is schizo diagnosed
Clinical criteria (ICD-11, DSM-5)
Earlier diagnosis = better outcome
No definitive test for schizophrenia
Combination of history, symptoms and signs
Info collected from close sources
During what time period and under what conditions for diagnoosis
For 1 month, one of the below:
Positive symptoms (hallucinations, delusions, thought disorders)
Negative symptoms (reduced self-care, motivation, anhedonia, alogia, affective blunting)
Reduced social functioning
There should be an absence of mood disorder ~mania/depression
Clinical aspects of schizophrenia in terms of prognosis
For first year after diagnosis, Prognosis is closely related to adherence to prescribed psychoactive drugs and avoiding recreational drug use
15% of all patients fully return to pre-illness level of functioning
1/3 of patients achieve significant improvement
1/3 improve somewhat but have relapses and residual disability
1/3 severely incapacitated
Factors associated with GOOD and BAD prognosis:
GOOD | BAD |
Good premorbid functioning | Young age at onset |
Late and/or sudden onset of illness | Poor premorbid functioning |
Family history of mood disorders other than schizophrenia | Family history of schizophrenia |
Minimal cognitive impairment | Many negative symptoms |
Few negative symptoms | Longer duration of untreated psychosis |
Short duration of untreated psychosis |
Age and Sex
Women respond better to treatment with antipsychotic drugs
Peak incidence of onset in
Males = 15-25yrs
Females = 25-35yrs
How do we manage schiz?
Address psychological, social and emotional components for best prognosis
Pharmacological treatment is 1st line in ALL CASES