Renal Physiology
1/313
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
314 Terms
Kidney Regulation
Blood volume (plasma volume) and pressure.
Water concentration and fluid volume.
Inorganic ion composition.
These two factors keep pressure under homeostatic conditions.
Kidneys Balance
They help regulate the acid-base balance.
Kidneys Excretion
Urea, uric acid, creatinine, and bilirubin (breakdown product of Hb).
Removal of foreign chemicals (i.e. drugs, food addictives, pesticides.
Uric Acid
Produced from the breakdown of nitrogenous bases.
Creatinine
Byproduct of muscle metabolism.
Kidneys Synthesis
Glucose (gluconeogenesis).
Kidneys Secretion
Acts as a endocrine organ, secreting cytokines or hormones.
Erythropoietin (EPO) → synthesized in the kidney.
Renin.
1,25-dihydroxy Vitamin D (inactive form).
Fluid Compartments
Total body water: 42L, around 60% body weight.
Plasma is 3L, the interstitial fluid is 11L, and the intercellular fluid 28L.
Functions of the kidneys is to maintain the plasma volume within a narrow range.

Fluid Volume Changes
Fluid volume can be altered during various health disorders.
Changes occur through rapid water movement between compartments by osmosis.

Intracellular Fluid (ICF)
The fluid inside the cell.
Extracellular Fluid (ECF)
Fluid outside the cell.
Plasma + interstitial fluid + cerebrospinal fluid.
Plasma
Non-cellular part of blood, fluid inside blood vessels.
Kidney Regulates ECF
The ECF is made up of:
Plasma.
Interstitial fluid.
Cerebrospinal fluid.
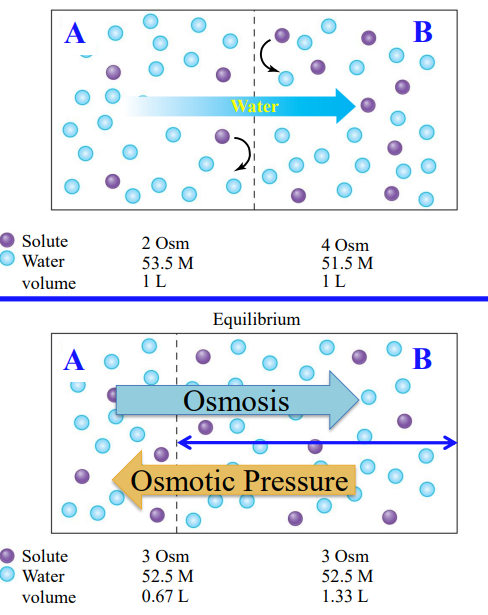
Dominant Ions in ECF
Na⁺, HCO₃⁻, Cl⁻.
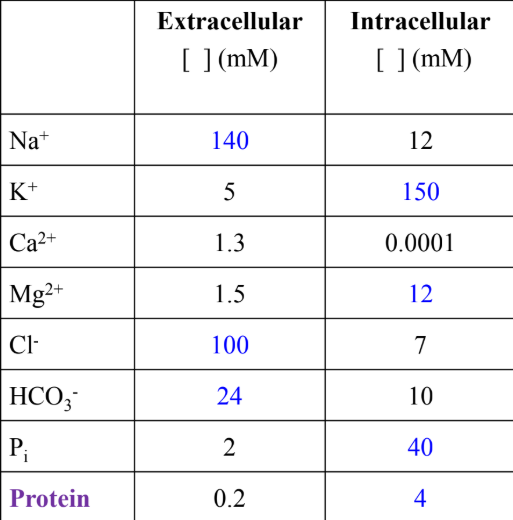
ICF Dominant in ICF
K⁺.
Diffusion
Rate of water diffusion that will affect fluid volume.
A low and finite degree of H₂O can diffuse through the tissues.
Aquaporins: water channels.
Osmoles
1 osmoles (osm) is equal to 1 mole of solute particles.
Osmolarity
Number of solutes per unit volume of solution expressed in moles per liter.
The addition of solute lowers the water concentration.
Addition of more solute would increase the solute concentration and further reduce the water concentration.
Diffusion
Is the movement of molecules from one location to another due to their random thermal motion.
Molecules initially move from a region of higher concentration to lower concentration.
Over time, solute molecules placed in a solvent evenly distribute themselves.
Diffusional Equilibrium
Is the result of diffusion.
Happens over time as solute molecules placed in a solvent evenly distribute themselves.
Osmosis
Net diffusion of water across a selectively permeable membrane from a region of high water concentration → lower water concentration.
Osmotic Pressure
The pressure necessary to prevent solvent movement (osmosis).
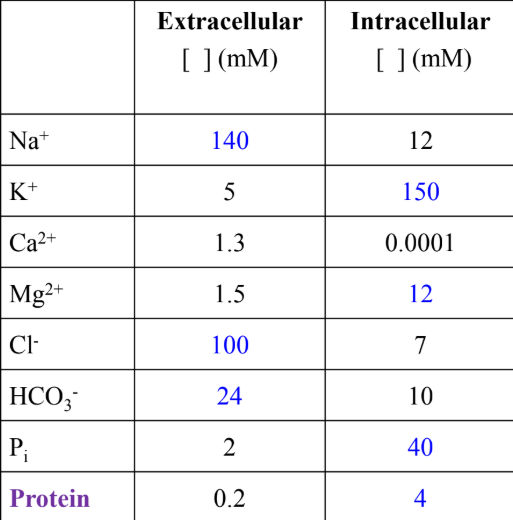
Reaching Diffusional Equilibrium
The partition between the compartments is permeable to water and solute.
After diffusional equilibrium has occurred, movement of water and solutes has equalized their concentrations on both sides.
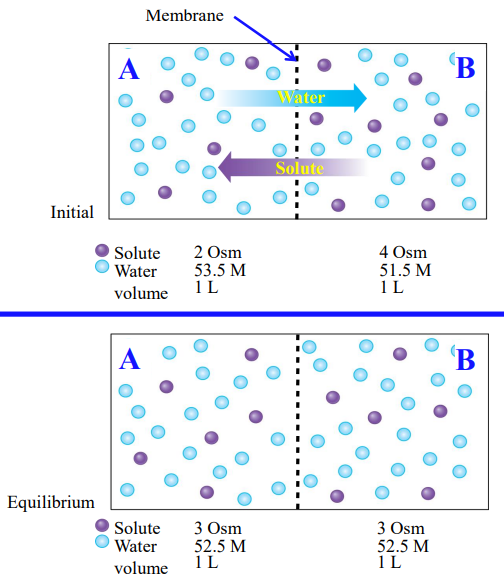
Reaching Osmosis
The partition between the compartments is permeable to water only.
After diffusional equilibrium has occurred, movement of water has equalized solute concentration.
The opposing pressure required to stop osmosis completely is equal to osmotic pressure.
Tonicity
Is determined by the concentration of non-penetrating solutes of an extracellular solution relative to the intracellular environment of a cell.
The solute concentrations may influence changes in cell volume.
Isotonic (Isoosmotic)
Same osmolarity outside and inside the cell.
Hypertonic (Hyperosmotic)
Higher osmolarity than inside of the cell.
Hypotonic (Hypoosmotic)
Lower osmolarity than inside of the cell.
Osmolarity Gradient
Water flows from osmolarity to higher osmolarity.
Normal osmolarity inside a cell is about 300mOsm/L.
Non-Penetrating Solutes
Solutes that cannot easily cross the cell membrane and establish osmotic gradients, thereby influencing cell volume and tonicity.
They are crucial for maintaining fluid balance.
i.e. Na⁺ and K⁺.
Penetrating Solutes
Solutes that can freely cross cell membranes, meaning they do not establish a sustained osmotic gradient.
Do not directly influence cell volume or tonicity.
i.e. urea.
Changes in Cell Volume
In a hypertonic solution the cell shrinks.
In a isotonic solution the cell volume does not change.
In a hypotonic solution the cell swells.
Absorption
Movement of solute/water into the blood (plasma).
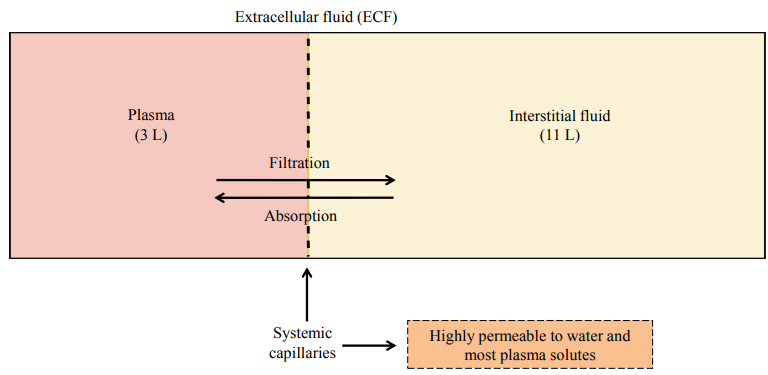
Filtration
Movement of solute/water out of blood (plasma).

Plasma Proteins + Movement
Plasma proteins in the blood create osmotic pressure.
This draws water into the capillary from the interstitial space.
Some plasma proteins may escape into the interstitial fluid.
Proteins
Big molecules that are sometimes charged.
Due to their size and charge, they cannot move in & out of capillaries easily.
Unable to cross capillary walls.
Capillary Hydrostatic Pressure (PC)
Pressure exerted on inside of capillary walls by blood.
Favors fluid movement out of capillary.
Interstitial Fluid Hydrostatic Pressure (PIF)
Fluid pressure exerted on the outside of the capillary wall by interstitial fluid.
Favors fluid movement into capillary; pressure is negligible & does not contribute.
Blood Colloid Osmotic Pressure (πC)
Osmotic pressure due to nonpermeating plasma proteins inside the capillaries.
Favors fluid movement into the capillaries.
Interstitial Fluid Colloid Osmotic Pressure (πIF)
Small amount of plasma proteins may leak out of capillaries into interstitial space.
Favors fluid movement out of capillaries; negligible.
Starling Forces
Net filtration pressure = PC + πIF - PIF - πC.
Govern the movement of fluid across capillary walls, determining whether fluid moves out of the capillary (filtration) or back into it (reabsorption).
Fluid Movement in Capillaries
At the arterial end, starling forces favour filtration. at the venous end, they favour reabsorption.
Filtration dominates at the arterial end; reabsorption at the venous end.
Overall, slightly more fluid is filtered than reabsorbed, with the excess drained by the lymphatic system.
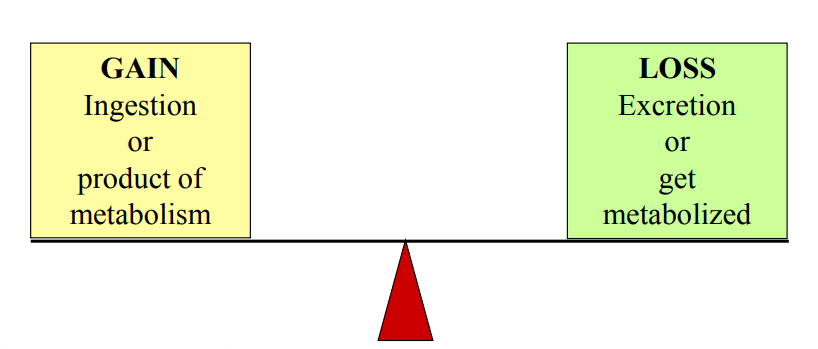
Homeostasis
Total body balance of any substance; keeping levels constant and maintained.
Urinary System
The kidneys are retroperitoneal (behind the peritoneum) in location.
Other structures associated with the urinary system include the ureters, bladder, and urethra.
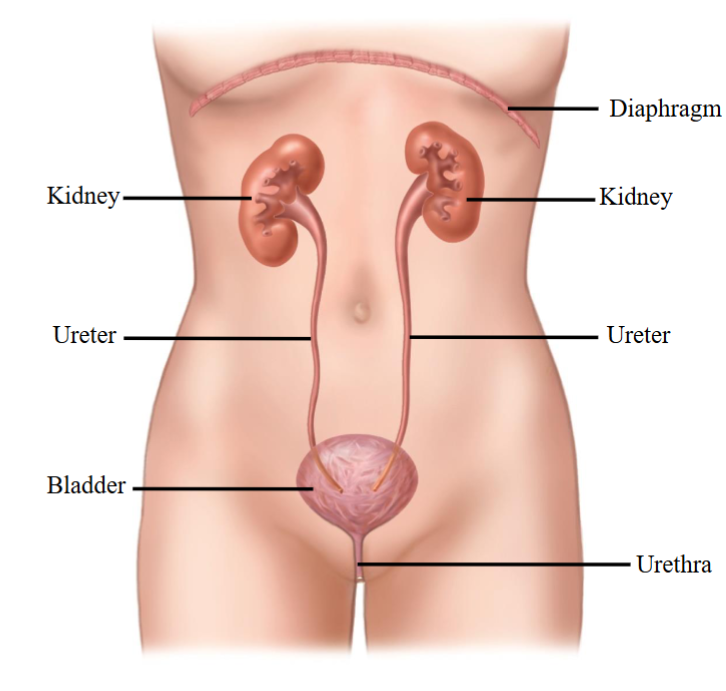
Ureters
Drain the formed urine from the kidneys.
Travel to the bottom of the abdominal cavity and empties into the bladder.
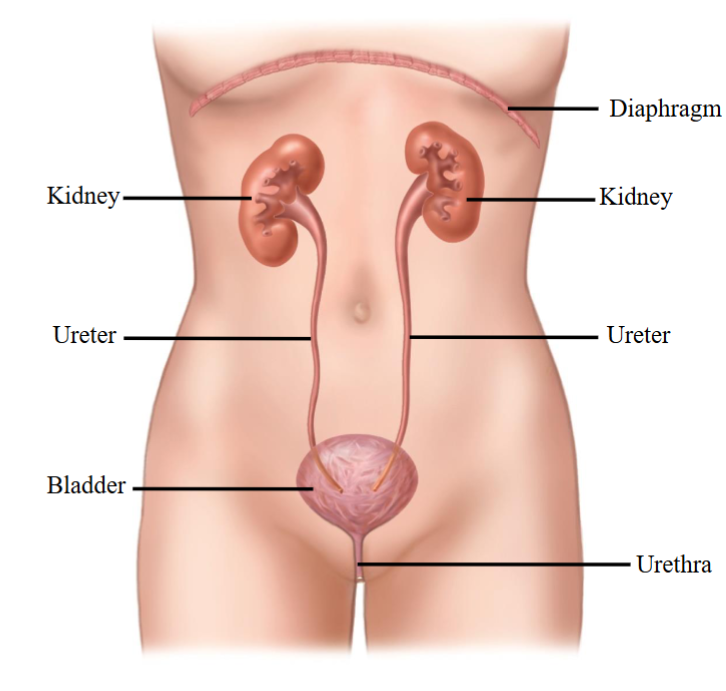
Bladder
Storage organ or sac.
Innervated by the ANS.
Voiding of the bladder is controlled by SNS/PSNS.
Bladder empties out of the body through the urethra.
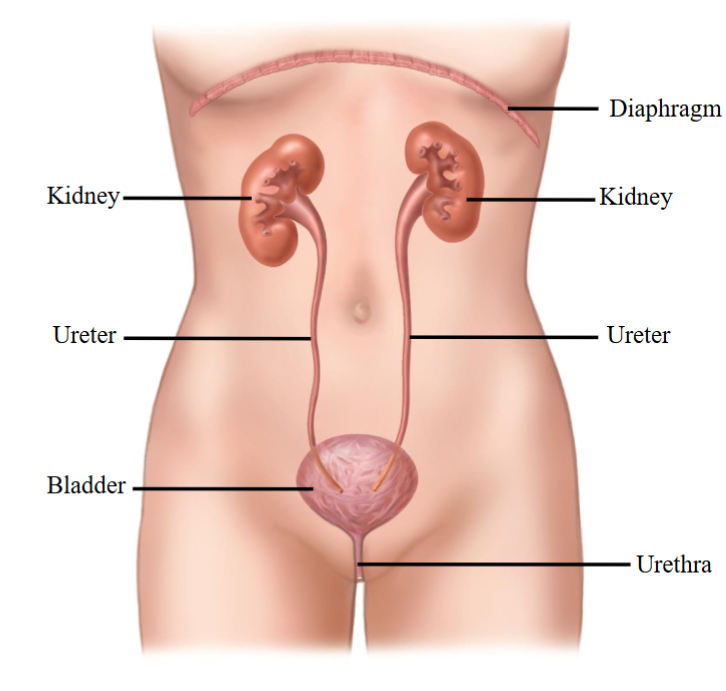
Hilum
Inner concave part of kidneys.
From the area two tubes emerge; these tubes are called ureters.
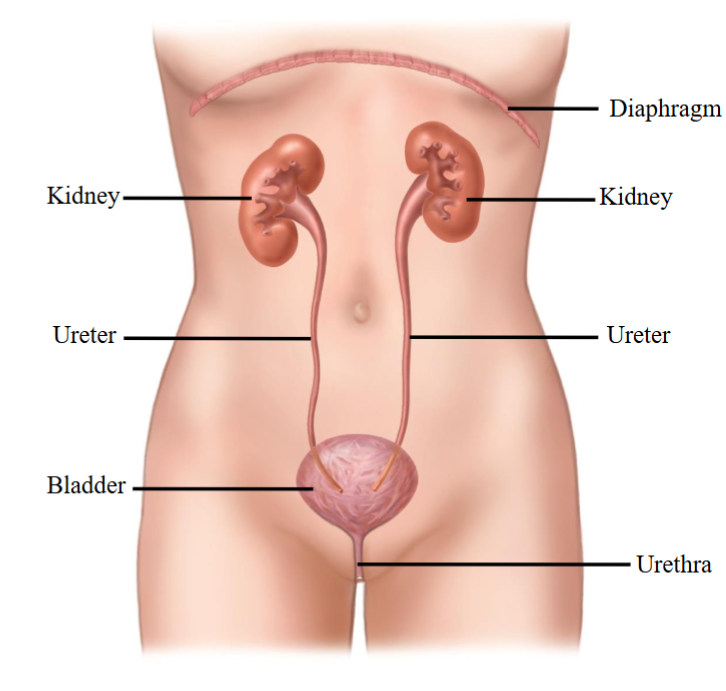
Micturition
The process of releasing the urine outside the body, or urination.
Bladder emptying with the help of autonomic control.
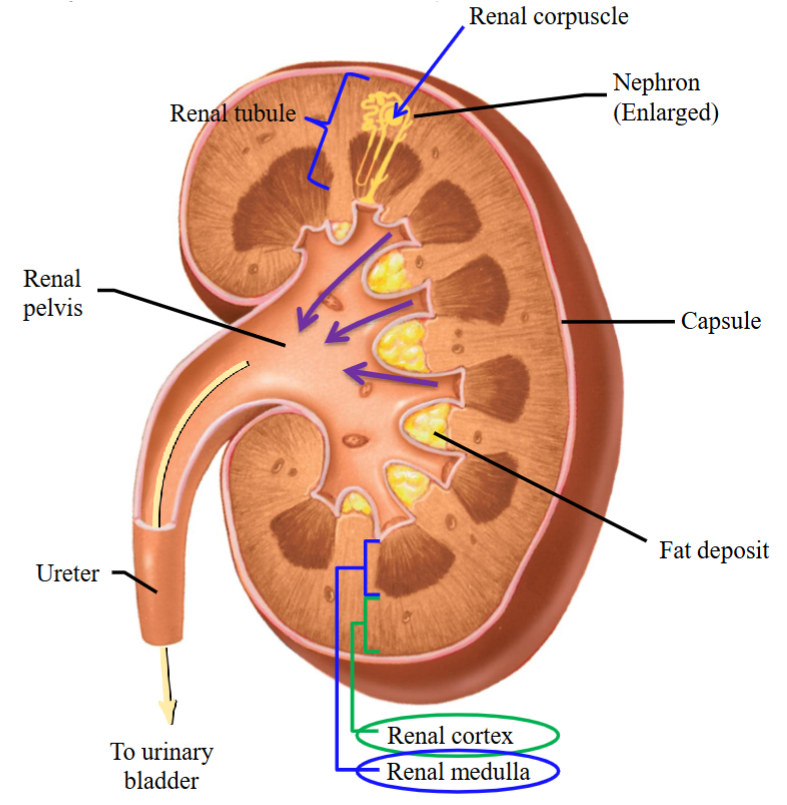
Kidney Anatomy
Covered with a capsule-like structure.
2 regions:
Outer portion: cortex.
Inner portion: medulla.
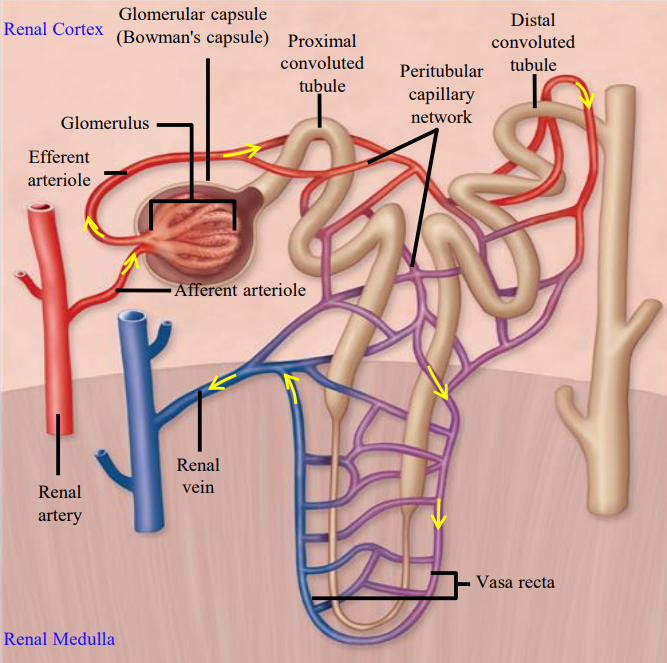
Nephron
Functional units of the kidney; where the urine is made.
1 million nephrons in your kidneys.
The parts of the nephrons form parts of the cortex and medulla.
Contains: renal corpuscle and renal tubule.
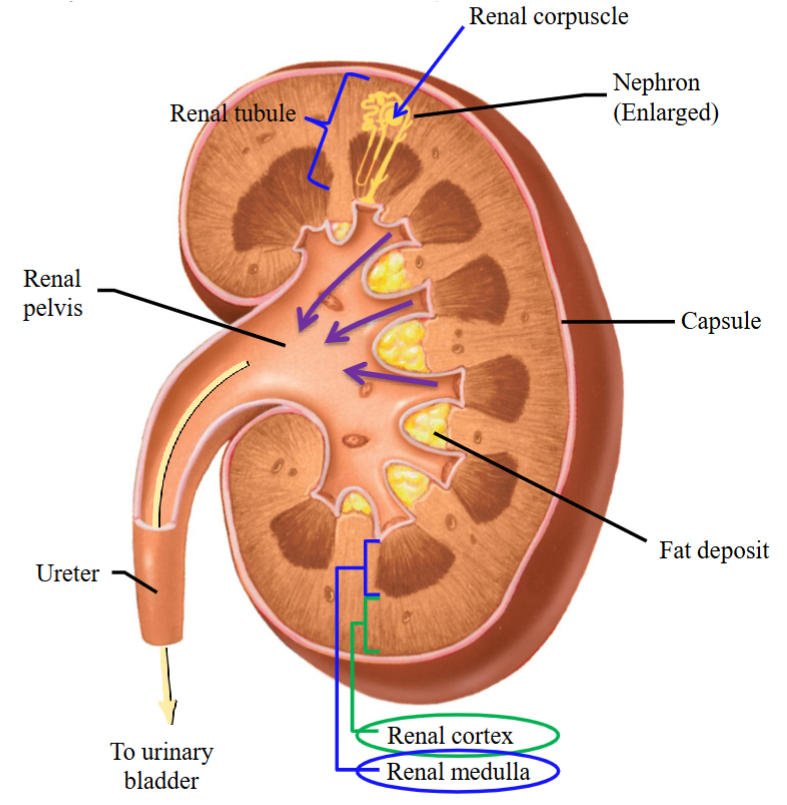
Renal Corpuscle
Bulb-like structure; attached to renal corpuscle is a long tube called the renal tubule.
A cup-like shaped structure with a tuft (loops) of capillaries.
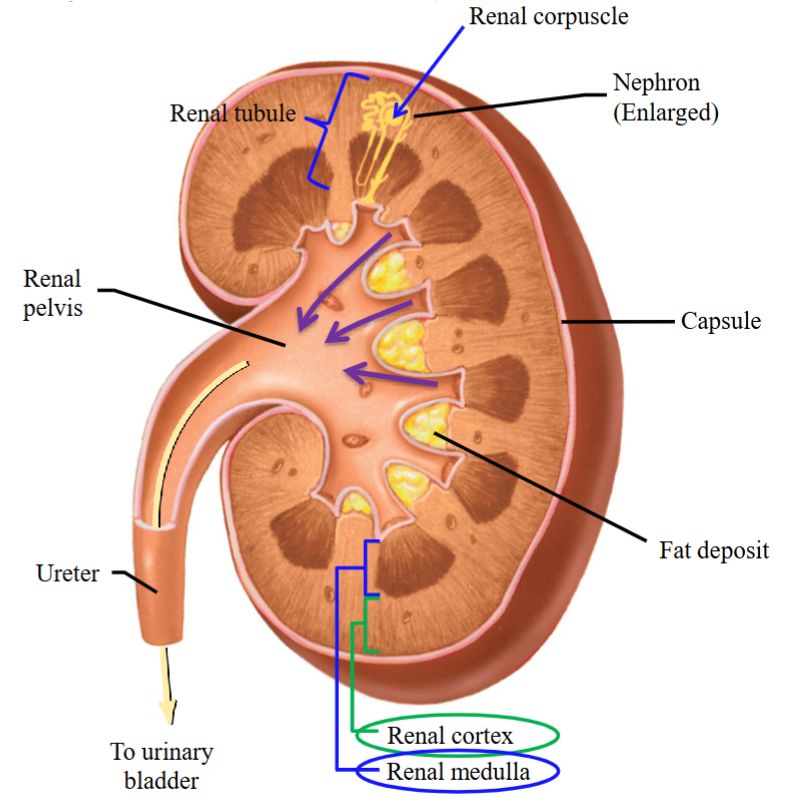
Renal Tubule
Attached to the renal corpuscle; a long tube.
Found mostly in the medullary portion.
Bowman’s capsule + glomerulus.
The formation of urine occurs through the different segments of the tubule.

Collecting Ducts
Each nephron has a renal corpuscle and a renal tubule that drains into a collecting duct.
Multiple nephrons drain into each collecting duct, which then empties the processed contents into the renal pelvis of the kidney.
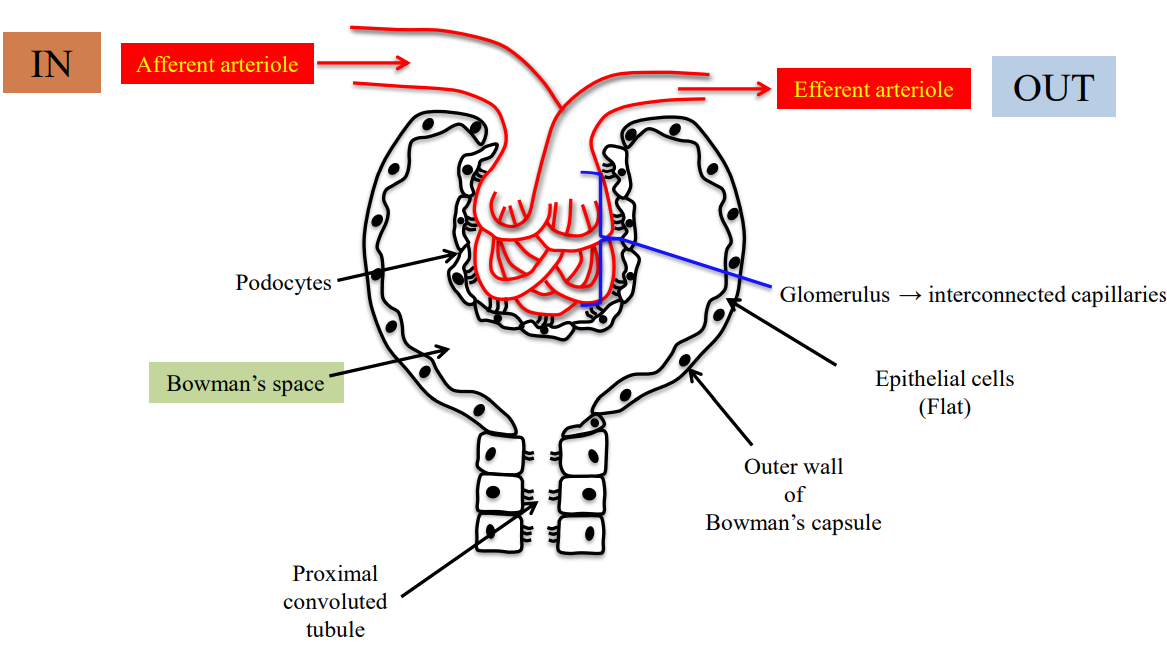
Glomerulus
A capillary tuft (loops).
Sits within the Bowman’s capsule (“cups” it).
Bowman’s Capsule
Leads into the renal tubule.
Renal Tubule Segments
Proximal convoluted tubule, Loop of Henle (descending and ascending limbs), distal convoluted tubule, collecting ducts.
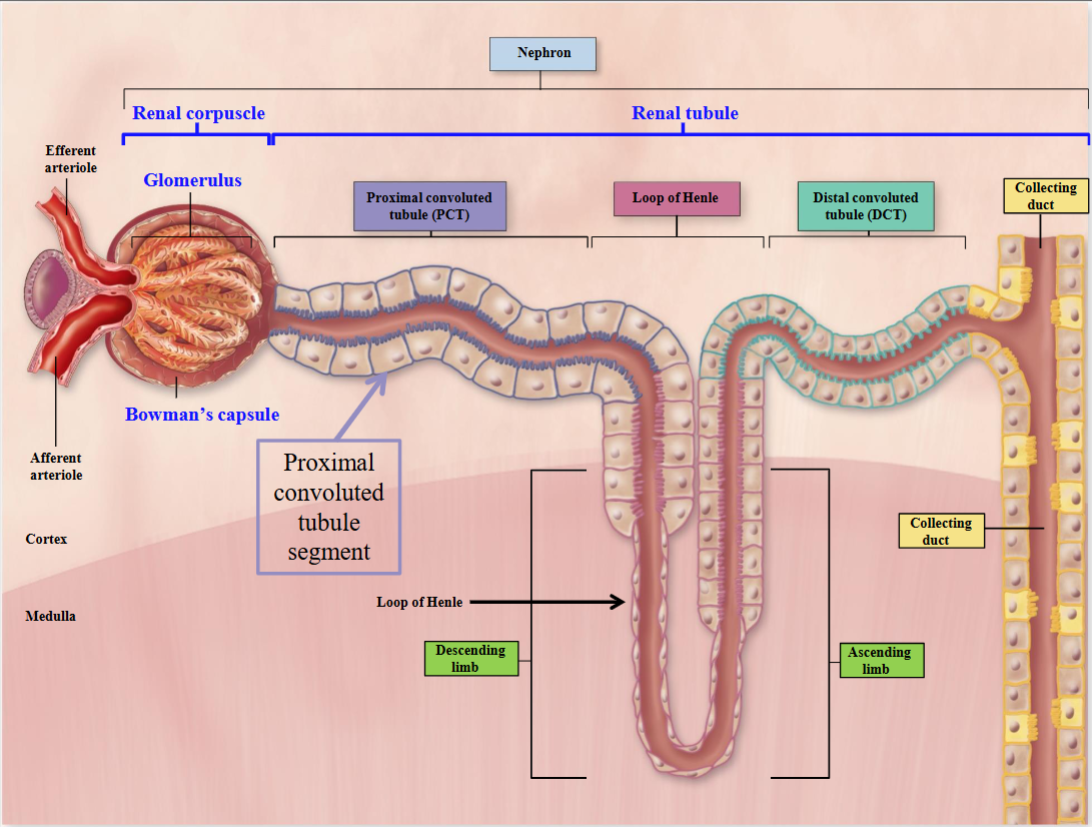
Distal Convoluted Tubule
“Distal” → far away from the renal corpuscle.
Drains its contents into a main tube called the collecting duct.
Major homeostatic mechanisms of fine control of water and solute to produce urine.
Proximal Convoluted Tubule
Proximal = close to the renal corpuscle.
Twisted.
Reabsorbs most of the water and non-waste plasma solutes.
Major site of solute secretion except K⁺.
Loop of Henle
Divided into descending limb and ascending limb.
Ascending limb has thick and thin segments.
Creates osmotic gradients that reabsorb large amounts of ions and smaller amounts of water.
Podocytes
The outer wall of the Bowman’s capsule is made of epithelial cells.
Flat cells continue on to form the tubules.
Cells in contact with the glomerular capillaries, called podocytes (podo = foot, cyte = cell), have foot-like processes.
Renal Corpuscle Filtering
Blood is brought in by the afferent arteriole and conducted towards the renal corpuscle.
The blood goes through several twists + turns.
Blood exits the renal corpuscle through the efferent arteriole.
Tubule Cell Variations
The cells forming the tubule are modified in structure.
As they approach the Bowman’s capsule, they slightly change in structure and function.
All are epithelial cells, but their type varies depending on the tubule segment.
Afferent
Conducted toward; blood is brought in by the afferent arteriole and conducted towards the renal corpuscle.
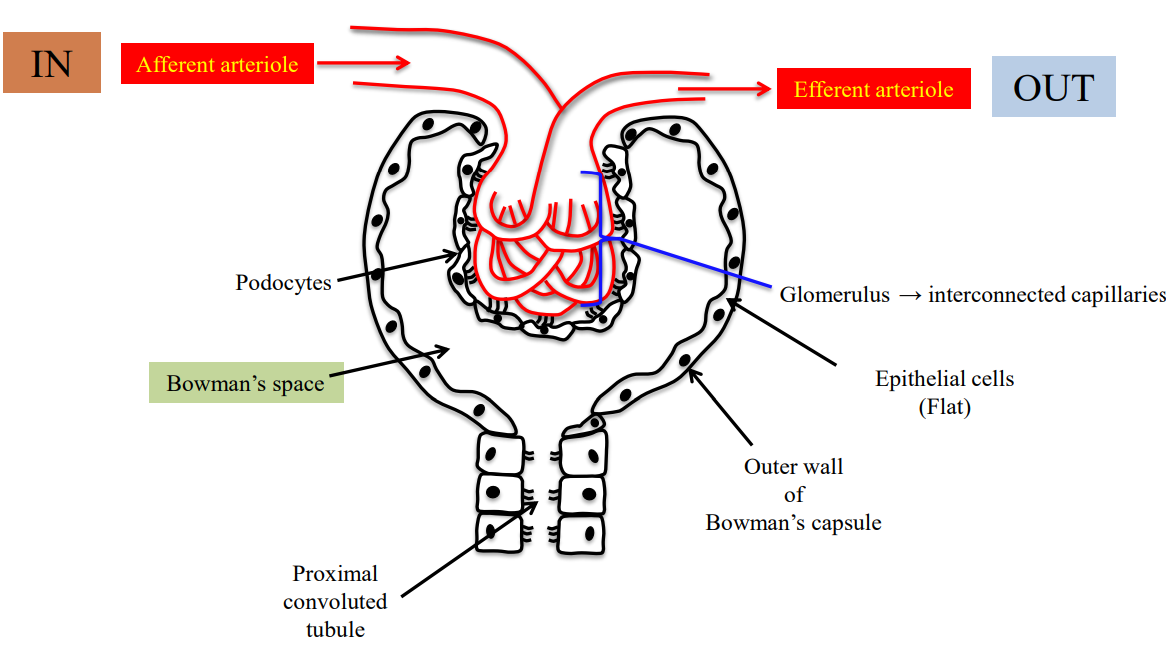
Efferent
Conducted away from; blood is being taken away from the renal corpuscle by the efferent arteriole.
Stage 1 - Renal Corpuscle Development Beginning
When the kidneys are forming fetal life.
A nephron will develop first as a blind-ended tube; there is no opening.
Tube is lined by a layer of epithelial cells sitting on a basement membrane.
Stage 2(1) - Renal Corpuscle Development Formation
A growing tuft of capillaries penetrates the expanded end of the tubules.
The tubule invaginates, bringing capillaries closer to the epithelial cell layer.
The basal lamina becomes trapped between the endothelial cells of the capillaries and the epithelial layer.
Stage 2(2) - Renal Corpuscle Development Structure
The epithelial layer differentiates into parietal (outer) and visceral (inner) layers.
The epithelial cells form a cup, and the tuft of capillaries forms the glomerulus.
Stage 3 - Renal Corpuscle Development Final
The outer layer does not fuse with the inner layer - there is a space between them.
Parietal layer eventually flattened to become wall of Bowman’s capsule; visceral layer becomes podocyte cell layer.
BC Parietal Layer
The outer layer of epithelial cells which forms the outer wall of the Bowman’s capsule.
BC Visceral Layer
The layer closest to the glomerular capillaries; these cells are the podocytes.
Glomerulus Functional Significance
The site where blood undergoes first filtration.
Interlocked Podocytes
Podocytes are arranged around the external surface of the glomerular capillaries.
The foot processes of one podocyte, which are cytoplasmic projections, interlock with those of another podocyte.
Between the interlocking foot processes of the podocytes are filtration slits.
Renal Corpuscle Capillaries
Blood is brought in through the afferent arteriole and flows through the capillaries of the glomerulus.
Capillaries are fenestrated.
Glomerular Capillary Layers
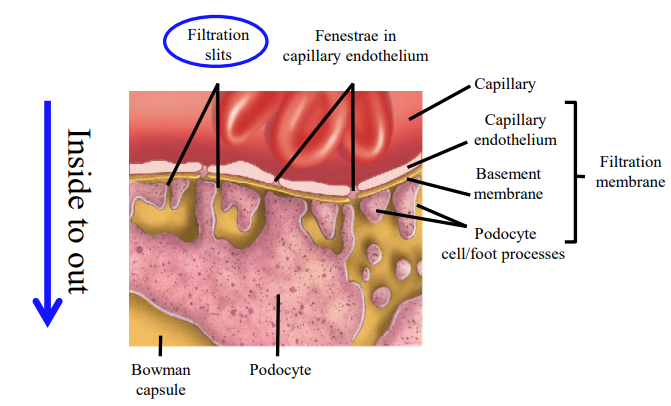
The glomerular capillary has three layers: the endothelial layer, the basement membrane, and the podocytes.
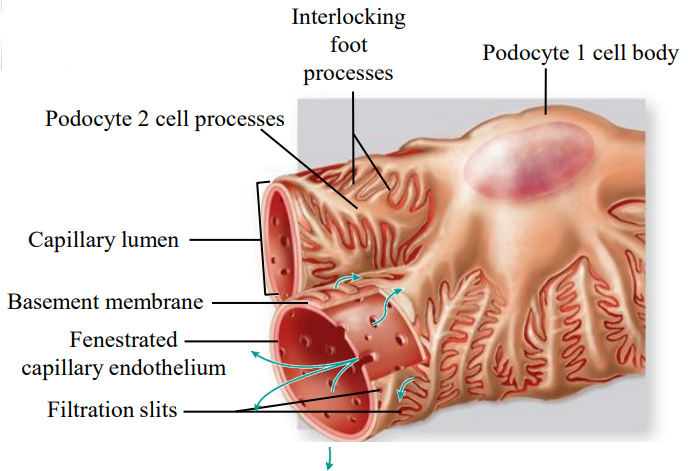
Endothelial Layer + Basement Membrane
The capillary endothelial cell layer is fenestrated to allow filtration.
The endothelial cells sit on a basement membrane, a gel-like mesh composed of collagen proteins and glycoproteins.
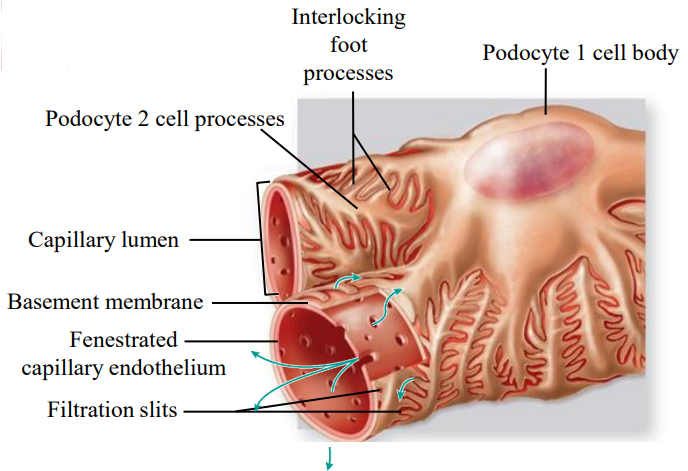
Filtration Slits
Podocytes are located outside the basement membrane, with filtration slits through which fluid moves.
Foot projections wrap around the capillaries, leaving slits between them.
Multiple foot processes increase the surface area for filtration.
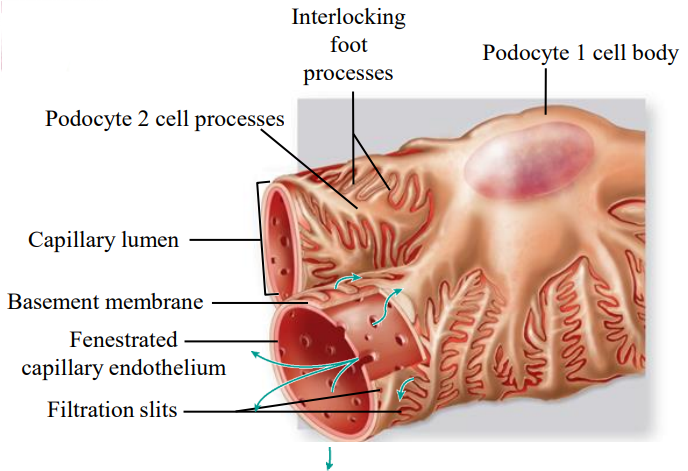
Basement Membrane
Gel-like mesh structure.
Composed to collagen proteins and glycoproteins.
Meshwork of collagen + other proteins which are negatively charged.
Prevents protein passage.
Filtration layer.
Multiple Foot Processes
Magnifies surface area for filtration.
Filtration Membrane
Capillary membrane.
Basement membrane.
Podocyte.
Two Types of Nephrons
The renal corpuscle is in the cortex for both.
One type of nephron (cortical) has their glomeruli in the outer cortex.
The other type (juxtamedullary) has their glomeruli closer to the medulla.
Cortical Nephrons
Make up 85% of all nephrons, with the renal corpuscle always in the cortex.
The collecting duct, distal convoluted tubule, and proximal tubule are mostly in the cortex, while loop portions may slightly dip into the medulla.
Juxtamedullary Nephrons
Juxta = close to; these nephrons sit closer to the medulla area.
Renal corpuscles sit in the cortex but are closer to the medullary area.
The loop of Henle and the ascending limb are found in the renal medulla.
15% of all nephrons.
Cortical Nephrons Function
Preforms the 3 basic functions.
Filtration, reabsorption, and secretion.
Juxtamedullary Nephrons Function
Perform the three basic functions and regulate urine concentration.
Create osmotic gradients in the interstitial space outside the Loop of Henle.
Regulate water volume and urine concentration.
Kidneys retain fluid when dehydrated and produce more urine when not dehydrated.
Blood Supply Kidney
Highly vascular organs.
They receive ~20% of the total cardiac output.
Blood enters through the renal artery via the hilum, a curved concave area, and begins branching.
The renal artery subdivides into arteries and arterioles; afferent arterioles bring blood to the nephrons.
Afferent Arteriole
Branches off from the renal artery and diverges into the capillaries of the glomerulus.
Arteriole that brings blood into the glomerular capillary network.
Blood travels through the Bowman’s capsule in the glomerulus or glomerular capillaries.
Efferent Arteriole
Blood exits the glomerulus through the efferent arteriole.
Efferent arteriole branches around to form a set of capillaries called the peritubular capillary network.
Types of Capillaries
Glomerular.
Peritubular.
Vasa Recta.
Peritubular Capillaries
Efferent arteriole branches around to form a set of capillaries.
Found around the proximal convoluted tubules.
Fuse together to form the renal vein.
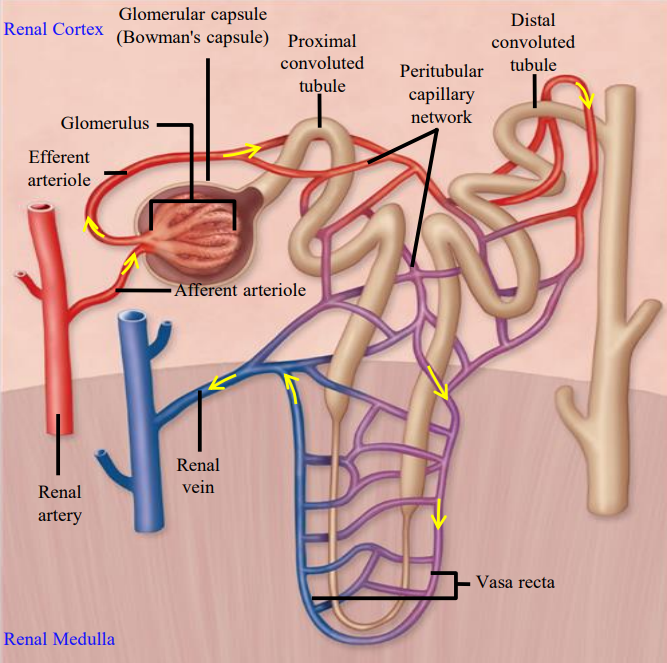
Vasa Recta
Capillaries that are found mostly associated with juxtamedullary nephrons in the medullary portion of the kidney.
Both the loop of Henle and this are important in forming the osmotic gradient.
Filter Load
How much slower the nephrons are getting each time the filtration process is occurring.
Glomerular Filtration
Fluid in the blood is filtered across the capillaries of the glomerulus and into Bowman’s space.
Blood is brought to the kidneys by the renal artery → enters the glomeruli through the afferent arterioles and is filtered.
Tubular Reabsorption
The movement of a substance from inside the tubule into the blood.
Glucose is reabsorbed by the body as it is very important as an energy source.
Tubular Secretion
Movement of nonfiltered substances from the capillaries into the tubular lumen.
Waste products that did not undergo filtration can be removed from the blood by tubular secretion.
Urinary Excretion
Blood is filtered at the glomeruli; substances are added/secreted to the tubules.
While other substances are reabsorbed urine containing unwanted products is excreted from our body.
Lumen Entry & Exit
Lumen entry via filtration and secretion.
Lumen exit via reabsorption and excretion.
Amount excreted = the amount filtered + amount secreted - amount reabsorbed.
Filtration Layers
Layers that substances move across from the lumen of the glomerular capillaries into Bowman’s space:
Capillary endothelial layer.
Basement membrane.
Podocytes with filtration slits.
Podocytes with Filtration Slits
Foot processes of the podocytes interdigitate and form filtration slits.
Slits remain covered with fine semiporous membranes.
Semiporous membranes are made up of proteins such as nephrins and podocins.
A filtration layer.
Capillary Endothelial Layer
Fenestrations (pores) in the capillary endothelium are not large enough to allow proteins to pass through.
Pores have negative charges that do not allow negatively charged proteins to pass through.
Filtration layer.
Holding Back Proteins
Large proteins or albumin are held back because:
Pore sizes are not large enough.
Pores and BM have negative charges and repel negatively charged proteins.
Podocytes have slits.