HBP 310 - Musculoskeletal & Autoimmune Diseases
1/96
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
97 Terms
Musculoskeletal System: Overview:
Bones: Structural scaffold
Ligaments: Connect bone to bone
Tendons: Connect muscle to bone
Muscles: Drives movement
Joints: Allows directional movement
Functions of the Bone:
Support: the framework for the body
Protection: skull, spine and ribs protect vital organs
Movement: attachment point for skeletal muscles
Storage of Minerals: calcium (99%) and phosphorus (85%)
Blood Cell Formation: bone marrow
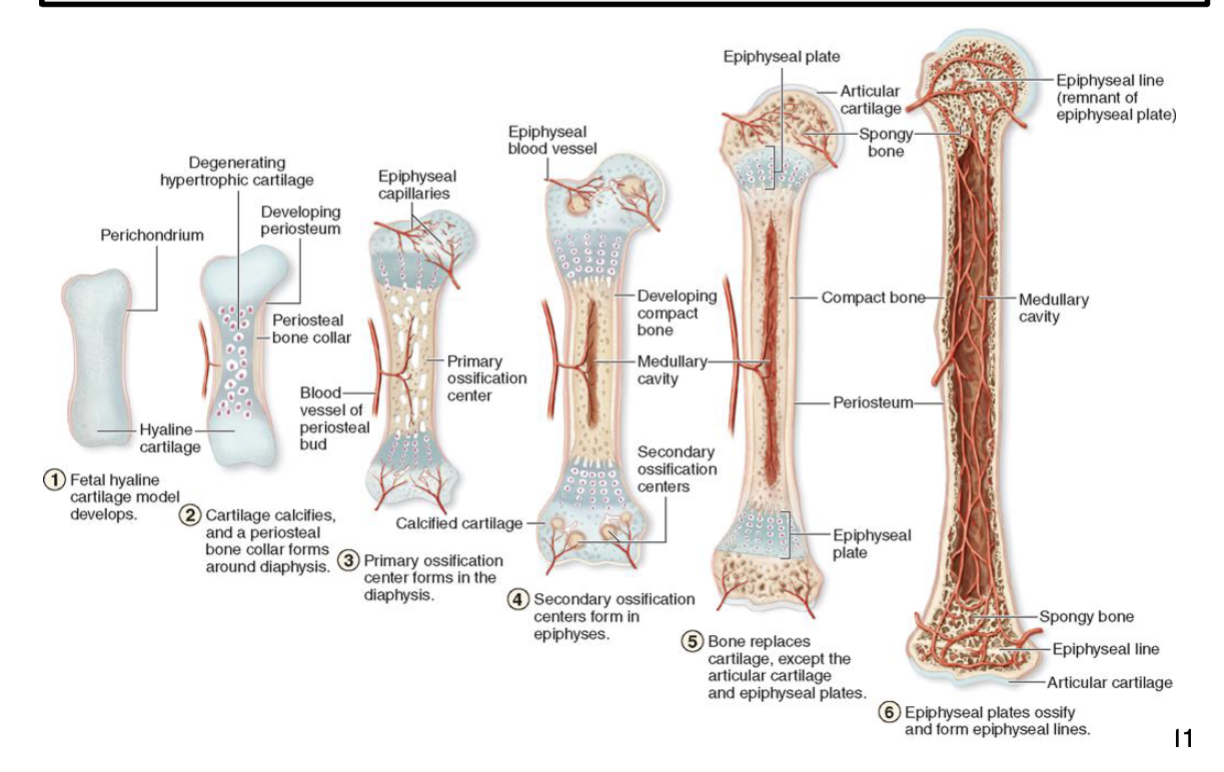
Types of Bone: Long Bones:
Arms, legs
Epiphysis (ends of bones)
Growth plate (epiphyseal line)
Metaphysis
Diaphysis (shaft)
Types of bone: Short Bones:
Wrist, ankle
Types of bone: Flat bones:
Sternum, skull
Types of bone: Irregular Bones:
Sacrum
Types of bone structure: Compact (cortical) bone:
The exterior part of bone, very dense, solid bone that resists deformation, this accounts for 80% of total bone mass (weight)
Types of Bone Structure: Trabecular Bone:
Interior part of bone, also called cancellous bone or spongy bone characterized by a meshwork, provides mechanical strength
Structure of bone: from outside to inside:
Cartilage: fits in joint cavity
Periosteum: outer coating, serves as attachment for tendons, contains nerves and blood vessels
Cortex: cortical (compact) bone, very strong and rigid
Endosteum: Vascular tissue that lines the inner side of the cortex
Medullary cavity
Trabecular (cancellous) bone: Meshwork that provides strength
Bone marrow
Bones:
Structural scaffold
Ligaments:
Connect bone to bone
Tendons:
Connect muscle to bone
Muscles:
Drives movement
Joints:
Allows directional movement
Support:
The framework for the body
Protection:
Skull, spine, and ribs protect vital organs
Movement:
Attachment point for skeletal muscles
Storage of Minerals:
Calcium (99%) and phosphorus (85%)
Blood cell formation:
Bone marow
Cartilage:
Fits in joint cavity
Periosteum:
Outer coating, serves as attachment for tendons, contains nerves and blood vessels
Cortex:
Cortical (compact) bone, very strong and rigid
Endosteum:
Vascular tissue that lines the inner side of the cortex
Trabecular (cancellous bone):
Meshwork that provides strength
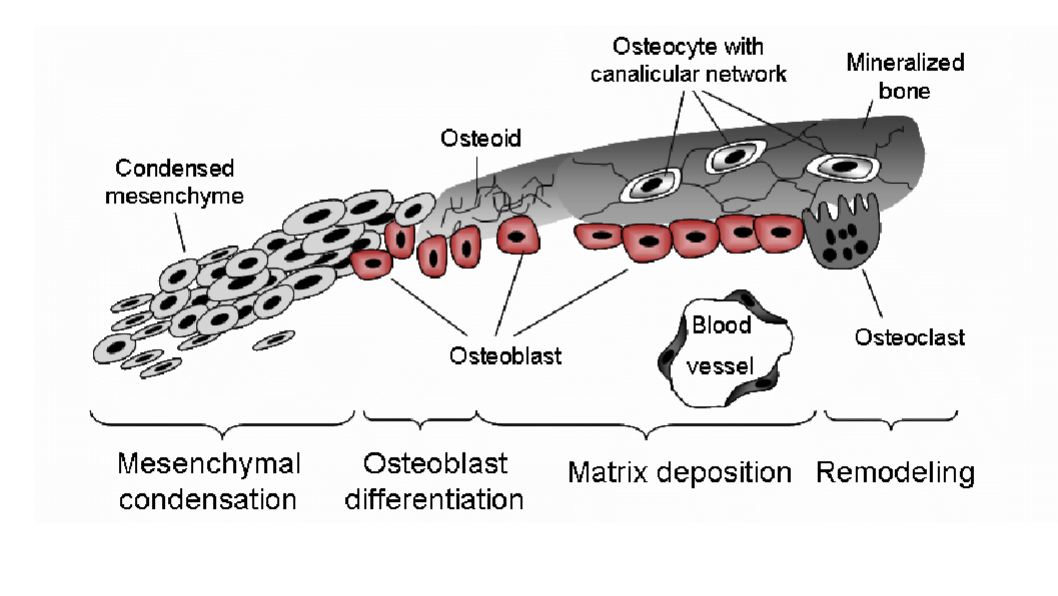
Osterochonroprogenitor cells:
mesenchymal stem cells that give rise to all cells
Chondrocytes:
produce and maintain cartilage matrix, and the only cell type in cartilage
Osteoblasts:
synthesize bone matrix (collagen, other bone proteins), deposit minerals in bone
Osteocytes:
mature osteoblasts embedded in matrix they secrete, they maintain the bone
Bone lining cells:
flattened inactive osteoblasts that cover bone surfaces
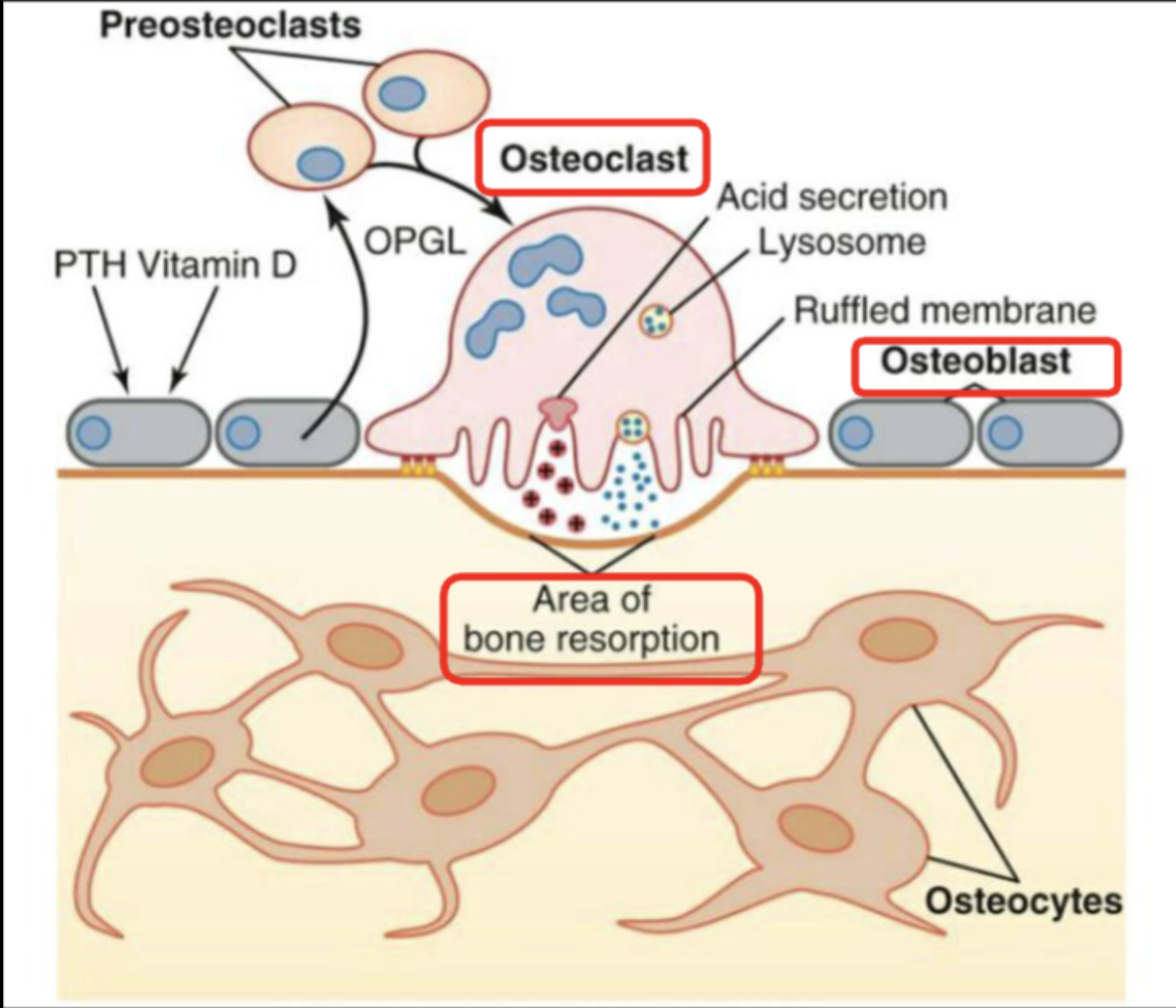
Osteoclasts:
essentially bone macrophages, they resorb and remodel bone
Bone matrix has both Organic & Inorganic components: Organic
called Osteoid, composed largely of type I collagen (>90%) and other proteins made by the osteoblasts
Bone matrix has both Organic & Inorganic compounds: Inorganic:
almost entirely composed of calcium and phosphorust hat form crystals known as Hydroxyapatite
Mineralization:
As bone develops the matrix transitions from a largely protein-based composition (osteoid) to a mineral-based (hydroxyapatite) composition as calcium and phosphorus is added to strengthen the bone, this process produces the characteristic solid and dense bone
Osteogenesis: Formation of Bone:
also known as Ossification
Important factors needed for bone formation: calcium, phosphorus, vitamin D, parathyroid hormone (PTH), calcitonin
Endochondral ossification:
Long bones
Cartilage “template” is progressively degraded and converted into bone
Intramembranous ossification:
Flat bones
Connective tissue “template” of mesenchymal cells condenses, and cells begin to synthesize bone
Bone formation: Two Histological patterns of Bone Formation:
Woven bone
Lamellar bone
Woven bone:
Newly formed immature bone
Osteoblasts produce osteoid rapidly
Characterized by a haphazard organization of collagen fibers
All bones in the fetus, replaced later in development by lamellar bone
Occurs at fracture sites during rapid osteoid synthesis
Lamellar bone:
Characterized by highly organized parallel alignment of collagen into sheets (lamellae), fiber arrangement produces high tensile strength
Lamellar bone is very strong
Virtually all adult bone is of the lamellar type
Bone remodeling: Wolf’s law:
Bone adapts to loads placed on it
Bone in athletes’ dominant arm is stronger than bone in the non- dominant arm (i.e., tennis players, baseball pitchers, etc.)
Astronauts lose bone mass while in space, this is caused by the reduced weight load due to the micro-gravity of space
Bone is constantly remodeled: needed to regulate calcium homeostasis, repair bone damage, adapt to changing stresses
Osteoblasts form bone, while Osteoclasts resorb bone, these processes need to be coordinated for proper bone health
Bone mass peaks at about age 25-30, but after age 40 bone mass begins to decline slowly
Overview of Bone Disorders
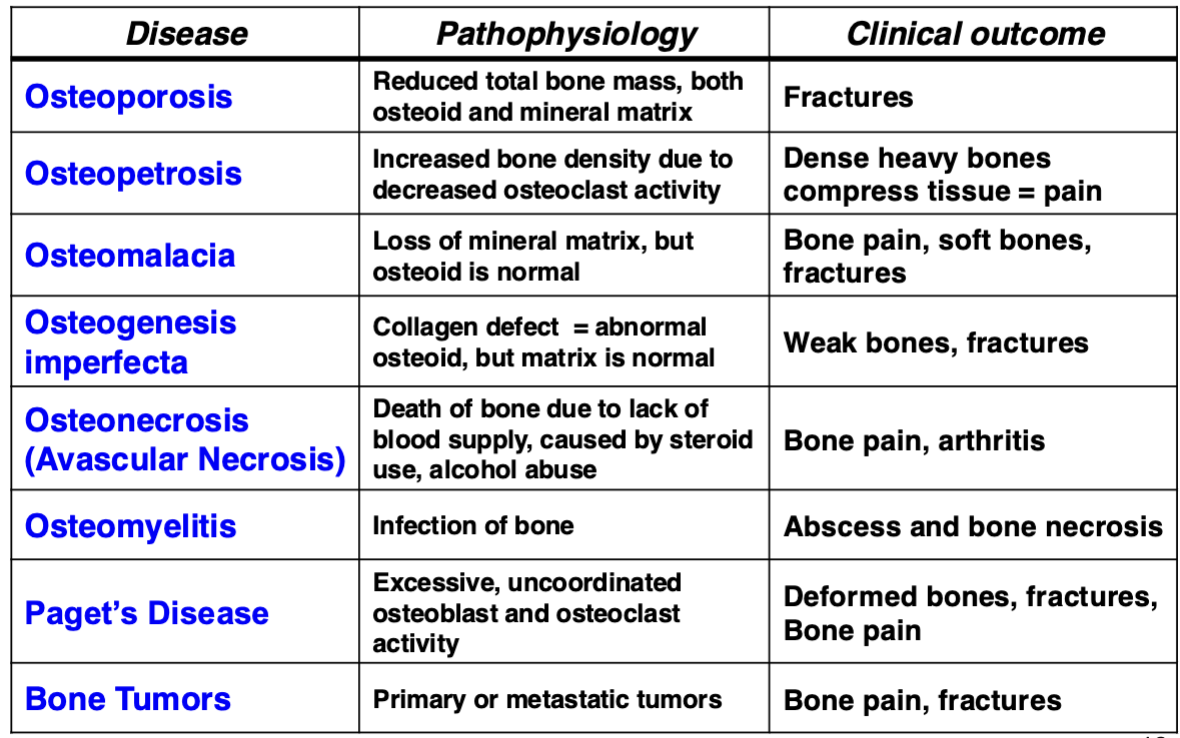
Osteoporosis:
Reduction in bone mass due to loss of both osteoid and mineral matrix
But the bone composition (% of osteoid and mineral) is normal
2 major types of osteoporosis:
Primary (Senile) osteoporosis
Secondary osteoporosis
Primary (senile) osteoporosis:
A disease of the elderly
Also called post-menopausal osteoporosis since the incidence increases significantly in women following menopause
Secondary osteoporosis:
Drug-induced: Glucocorticoid-induced (steroids), long-term cigarette smoking, heavy chronic alcohol use
Diseases: Cushing’s Syndrome, Hyperparathyroidism, Multiple Myeloma (cancer of plasma cells), Chronic Renal Failure
Osteoporosis clinical manifestations:
Silent until a fracture occurs, and then PAIN! Most common fracture sites:
Spontaneous fracture: Lumbar and lower thoracic spine (compression fracture), sacrum (sacral insufficiency fracture)
Loss of height from vertebral collapse, causes spinal curvature (kyphosis)
Trauma-induced fracture: Wrist and hip due to accidental falls
Osteoporosis diagnosis:
Bone Mineral Density test (BMD)
Dual-emission X-ray absorptiometry (DXA)
Scores compared to 30-year old gender-matched controls (T score)
Osteopenia: mild loss of BMD (T: -1.0 to -2.4 S.D. below the mean)
Osteoporosis: significant loss (T: -2.5 or greater S.D. below the mean)
Osteoporosis preventative treatment:
Correct the underlying causes, must start early before significant bone loss occurs:
Proper nutrition and adequate exercise
Daily intake of calcium (600-1000 mg) and vitamin D (>1000 units)
Avoid cigarette smoking and heavy alcohol consumption
Osteoporosis pharmacological treatment:
Relatively new approach
Drugs that inhibit bone resorption by osteoclasts
Bisphosphonates (Fosamax, Zometa, Boniva, Atelvia
● Denosumab (Prolia): a biologic Rx (monoclonal antibody to RANKL)
Drugs that promote bone formation by osteoblasts
Teriparatide and Abaloparatide: a modified form of PTH that has osteoblast stimulating activity (with little osteoclast activity)
Osteopetrosis:
Do not confuse with osteoporosis
Rare condition caused by defect in chloride channel gene (CLCN7), also called Albers-Schonberg disease
Causes decreased bone resorption by osteoclasts
Largely affects spine, pelvis and base of skull, dense bones cause pain by compressing tissue and sensory nerves
Results in characteristic dense bone in vertebral bodies known as “sandwich vertebrae”
Osteomalacia:
Reduction in bone mineral matrix due to lack of vitamin D and/or calcium. Bone composition (% mineral vs. osteoid) is abnormal
Results in soft bones that are prone to fracture, leg bones will deform (bow outward since soft bones can’t support the body weight, more often occurs in children)
Early stages are often asymptomatic, but as condition progresses bone pain will develop and risk of fracture increases
Rickets: Osteomalacia in children, usually due to poor nutrition
Major causes of osteomalacia:
Diet: Deficiency of vitamin D and/or calcium
Celiac disease: can produce secondary osteomalacia because the damaged intestine can’t absorb nutrients
Chronic Liver and/or Kidney disease: can’t activate vitamin D
Certain Medications: for seizures can cause vitamin D deficiency
Osteogenesis Imperfecta:
Genetic defect in Type I collagen
Defect produces abnormal osteoid that results in weak bones that are prone to fracture, this is also called Brittle Bone Disease
Several variants (at least 8) range from mild to severe depending on the gene alteration
Osteonecrosis (Avascular Necrosis):
Long-term use of corticosteroids
Death of bone cells due to decreased blood supply (bone is very vascularized)
Causes localized areas of necrosis with dead bone cells, results in weak regions of bone that can collapse and fracture, this can cause degenerative (osteo) arthritis
Osteomyelitis:
Bone infection, usually bacterial (Staph is most common) or fungal (usually in the immunocompromised)
Symptoms are typical of an infection (pain, fever, pus at wound site, etc.)
May require surgical intervention to clean the wound followed by IV antibiotics
Can result in necrosis at the affected area of bone that is prone to fracture
Paget’s Disease:
Accelerated and uncoordinated bone remodeling
Mostly a disease of those > 60 years old, usually affects skull, spine, pelvis, femur. Causes bone pain and produces deformed bone that is prone to fracture
Treatment is drugs that inhibit osteoclast activity (often Bisphosphonates)
Bone tumors: benign:
often detected as a ”bump” on a bone that may slowly grow larger
Osteoma (osteoblasts/osteocytes)
Non-Ossifying Fibroma (fibroblasts)
Chondroma (chondrocytes)
Bone tumors: malignant:
Rare!
Osteosarcoma (Osteogenic Sarcoma) is the most common type
Chondrosarcoma
Giant Cell tumor (tumor of osteoclasts, borderline benign/malignant)
Ewing’s Sarcoma (largely a bone cancer in children)
Bone tumors: Metastatic:
from cancer in other organs is the most common bone tumor (10-fold more common than primary bone tumors)
Most common primary cancers that metastasize to bone: prostate, lung, breast, kidney
Diseases of joints:
Types and structure
Osteoarthritis
Rheumatoid arthritis
Other arthropathies
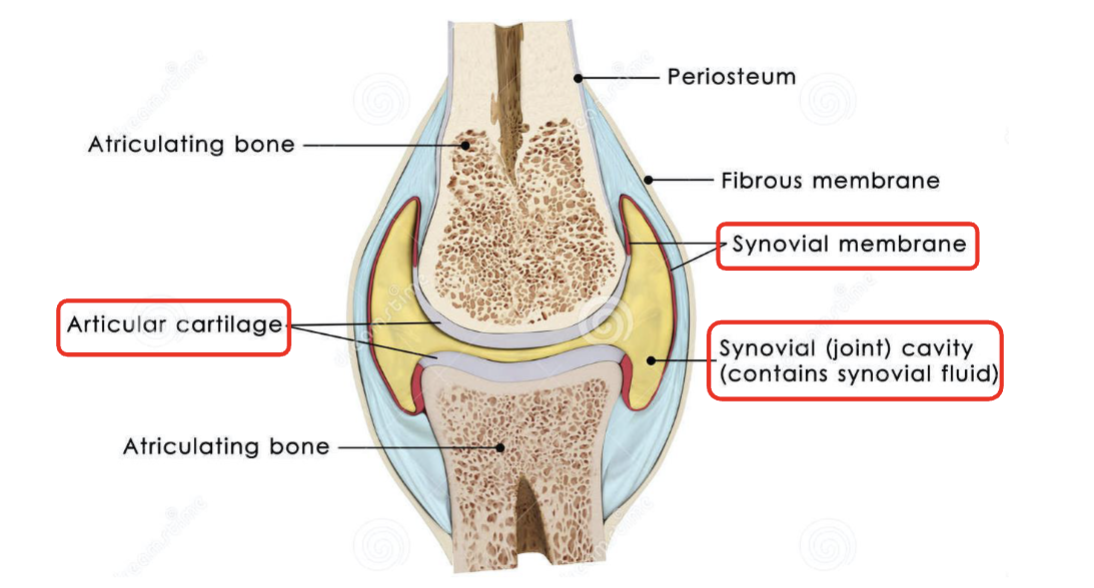
Synovial joint structure:
Cartilage + Synovial Fluid allows for smooth joint movement with little or no frictional resistance
Osteoarthritis: (OA):
Characterized by loss of cartilage and formation of bone spurs (known as Osteophytes)
Also called as Degenerative Arthritis
This is a “Wear and Tear” disorder of repetitive stress on joints:
Common in older athletes and individuals who sustained joint injury
Occupational overuse of joints, obesity and weak muscles can cause OA
The disease incidence increases with age:
10% of men and 13% of women over age 60 have symptomatic OA
Slightly more prevalent in females
OA is a world-wide disorder observed in all populations
Genetic link is uncertain, but OA can occur in families
Greater than 50% of elderly have OA, if you live long enough, you’ll get OA!
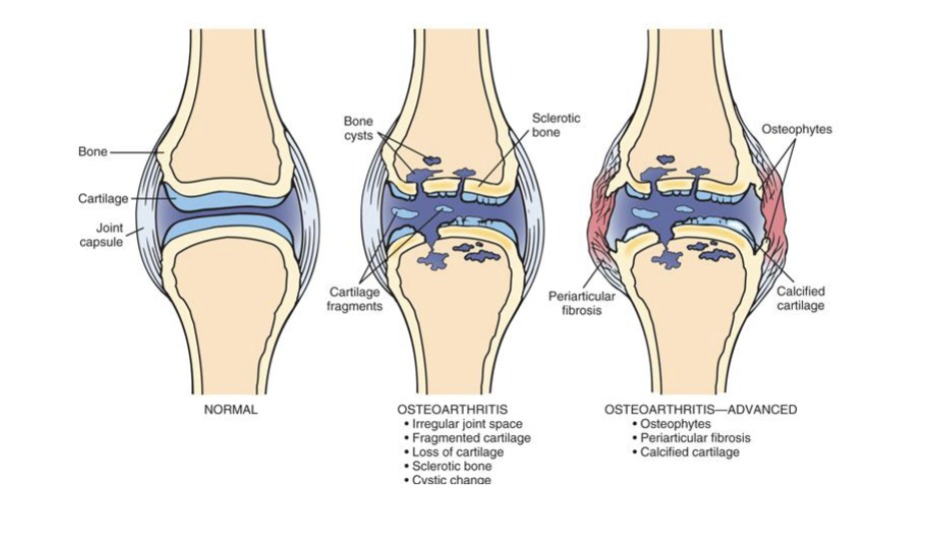
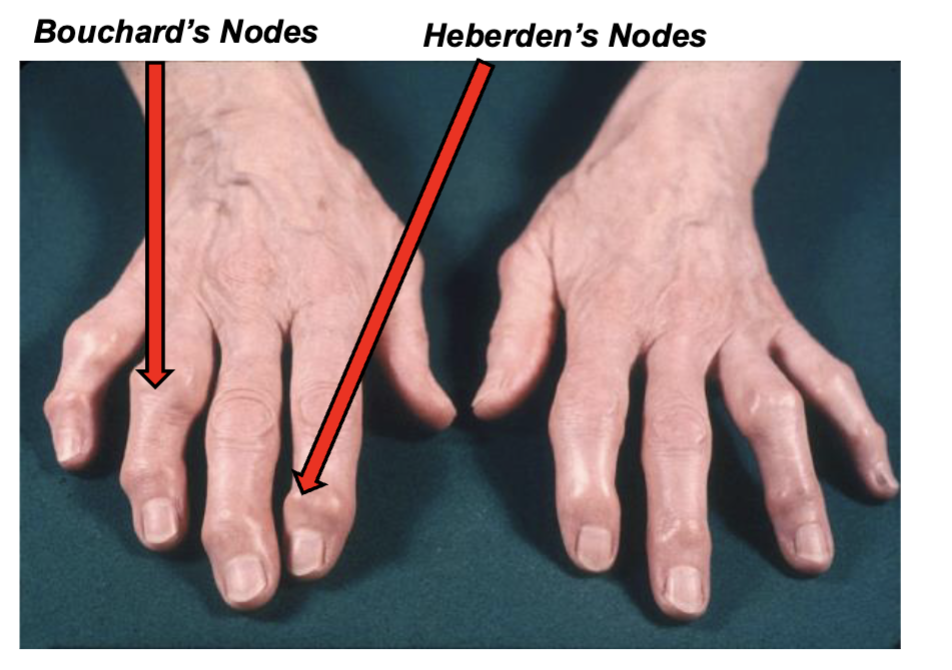
Osteoarthritis tends to affect certain joints:
Spine: neck (cervical spine), lower back (lumbar spine)
Hips, knees, feet
Hands: last 2 rows of finger joints; all joints of the thumb
Heberden’s Nodes: bony spurs in distal interphalangeal (DIP) joint.
Bouchard’s Nodes: bony spurs in proximal interphalangeal (PIP) joint
OA less often affects shoulders, wrists, elbows and ankles
Osteoarthritis (OA): Symptoms:
PAIN! Restricted motion & loss of function
Osteoarthritis: Diagnosis:
History, physical, and X-rays
Osteoarthritis: Treatment:
No treatment to reverse cartilage loss but:
Symptom relief with NSAIDS (aspirin, ibuprofen, naproxen)
Physical Therapy, Occupational Therapy
Joint Replacement Surgery
Rheumatoid Arthritis (RA):
Systemic inflammatory autoimmune disease
A common disorder world-wide, affects ~ 1% all humans
Affects individuals at any age but most often seen in middle-aged adults (age 40-65), more often in women (female/male ratio is 3:1)
Major symptoms: Joint inflammation and Pain
Genetic link is moderately strong, with an association with specific immune receptors: MHC class II (remember the Immunology lecture!)
The typical clinical presentation is a slow insidious onset of pain, stiffness and joint inflammation, but there are several variations
A progressive chronic inflammatory disorder, but can have flare-ups (flares) of painful acute inflammation of joints
Symptoms can improve (remission) but can relapse again, and cycle through this pattern of relapse/remission
Clinical features of RA:
Almost always affects joints in the extremities (arms, legs, hands, feet) in a symmetrical pattern (both hands, feet, etc.)
In about 25-30% of cases can involve joints in the axial skeleton (spine)
Primary disease manifestation is inflammatory arthritis
Secondary issues can involve the eyes, heart, blood vessels and lungs
Rheumatoid Factor (RF) is found in the plasma of almost all RA patients, but it is NOT specific for RA and is seen in other autoimmune diseases.
Rheumatoid Factor is IgM or IgG autoantibodies against the Fc region of IgG
Anti-cyclic citrullinated peptide antibodies (anti-CCP): more RA specific
Diagnosis is made by history, physical and blood tests that show autoantibodies, increased markers of inflammation (cytokines, CRP, sed rate)
Treatment is anti-inflammatory Rx and anti-cytokine biologics, anti-TNF alpha is the most common anti-cytokine Rx (Enbrel, Humira, Remicade, etc.)

Mechanism of Immune-Mediated Joint Damage in RA:
Classic pattern shows inflammation of the synovial membrane with an inflammatory exudate and cells
Immune cells: B and T lymphocytes, macrophages and neutrophils
Inflammation causes synovial cells to proliferate and cover the surface with Pannus, an inflammatory membrane
Pannus is the classic pathological finding in an RA joint
Immune cells and osteoclasts in Pannus secrete enzymes that destroy cartilage and erode underlying bone, Bone Erosions
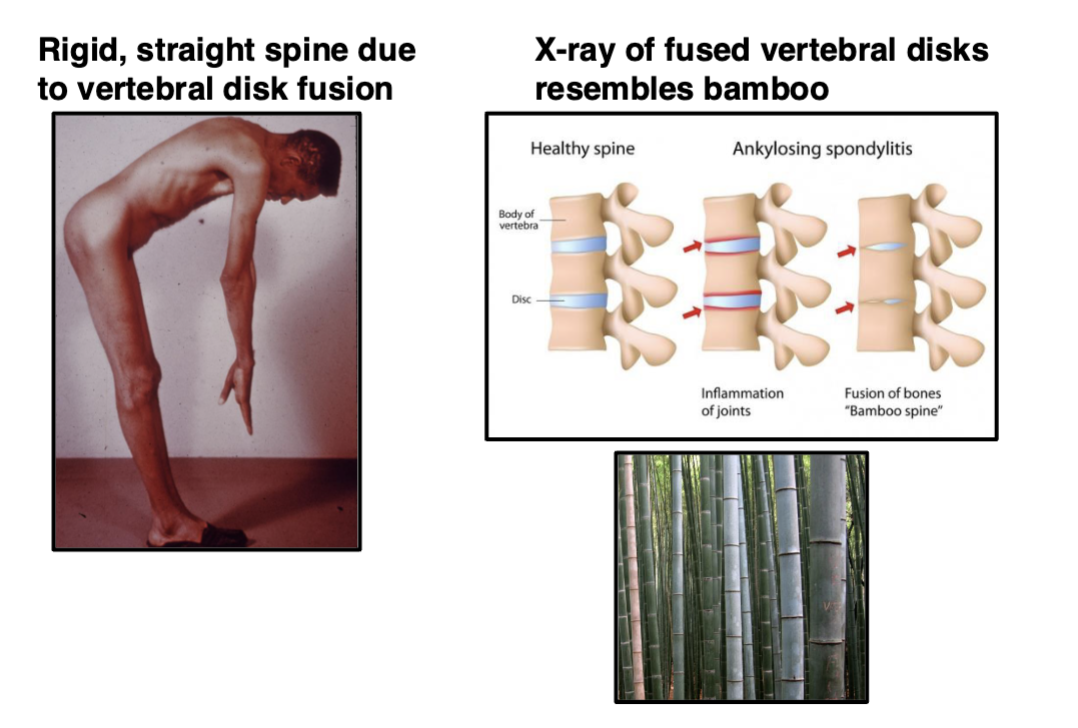
Spondyloarthropathy:
Spinal Arthritis
A group of different conditions that all result in a spinal arthritis, all these disorders are seronegative for Rheumatoid Factor and anti-CCP
Ankylosing Spondylitis:
Usually presents in late teens to 20’s and is 2-3x more frequent in men. Highly associated with tissue type HLA- B27. Causes fusion of vertebral bodies resulting in a rigid spine and spinal immobility, known as Bamboo Spine
Psoriatic Arthritis:
About 20%+ of individuals with the autoimmune skin disease Psoriasis develop a spinal arthritis (and other joints)
Crohn’s disease:
About 3% of Crohn’s patients develop arthritis
Reactive Arthritis:
Formerly called Reiter's Syndrome, this is arthritis that occurs in response to an infection, BUT not directly caused by the microbe, but rather the immune response to the infection.
For example, Streptococcus infection can produce antibodies that cross-react with joint tissue and induce an arthritis
Crystal-Induced Arthropathies:
crystals that precipitate out of solution in distal joint spaces (hands, feet), due to lower temperatures. Crystals induce VERY PAINFUL inflammation. Often, a temporary condition that is reversible once treated
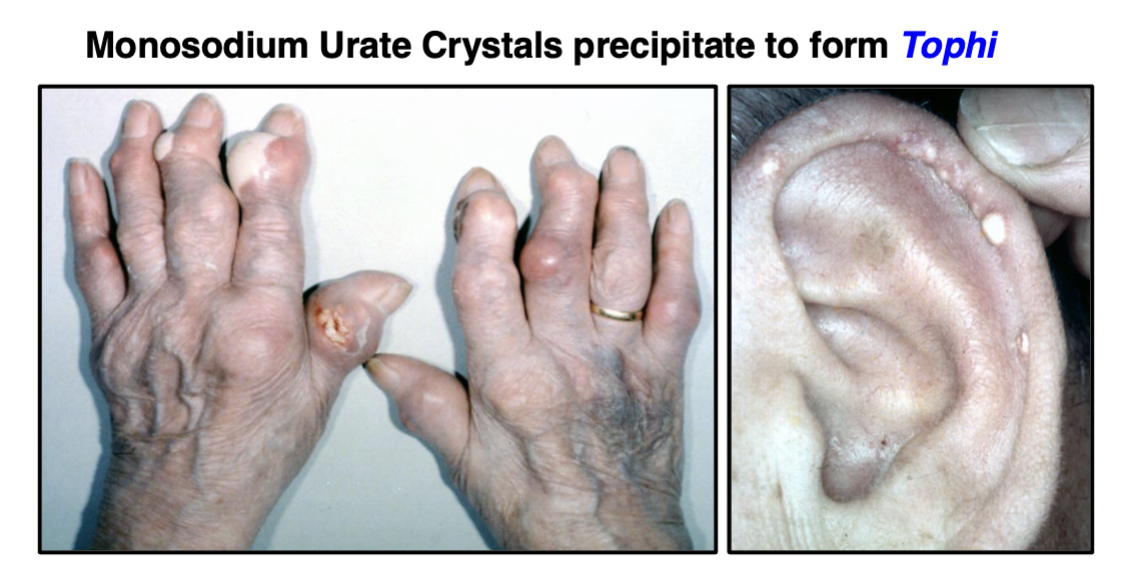
Gout:
caused by monosodium urate (MSU) crystals, large collections of MSU crystals are called Tophi, very common in big toe and outer part of the ear. Tophaceous Gout: gout with tophi
Pseudogout:
Caused by calcium pyrophosphate crystals
Infectious Arthritis:
Infectious organism can directly trigger arthritis at the site of infection:
Lyme Disease bacteria cause Lyme arthritis
Tuberculosis (most often involves the spine)
Other systemic (blood-borne) infections can “seed” joint spaces with infectious organisms resulting in an arthritis
Diseases of Muscle (Myopathies):
Muscular Dystrophy
Polymyositis
Dermatomyostitis
Polymyalgia rheumatica (PMR)
Muscular dystrophy:
A genetic defect in muscle gene dystrophin causes progressive muscle weakness beginning in early childhood which results in the inability to move, swallow and breath. There is no effective treatment
Polymyostitis:
Autoimmune attack on skeletal muscles resulting in symmetrical weakness causing difficulty in climbing stairs, getting up from a seated position and lifting objects overhead
Usually affects people aged 30-50, and more frequently in females
Symptoms slowly progress over weeks to months
Treatment is to reduce pain and inflammation, also physical therapy
Dermatomyositis:
Autoimmune condition that affects both skin and skeletal muscles, much like polymyositis but also has rashes on the face and hands
Usually affects people aged 40-60, and more frequently females
Can also affect young children (Juvenile Dermatomyositis)
Symptoms and treatment same as polymyositis
Polymyalgia Rheumatic (PMR):
Relatively common condition of people over age 60, but most cases are in late 70s to 80s. Characterized by inflammatory muscle pain (myalgia) and weakness, particularly in the shoulders and hips. Treatment is low-dose corticosteroids
Connective Tissue:
Composed of collagen, elastin and other glycoproteins that form the extracellular matrix (ECM) that surrounds and supports all organs and tissues. The ECM composition varies among different tissues.
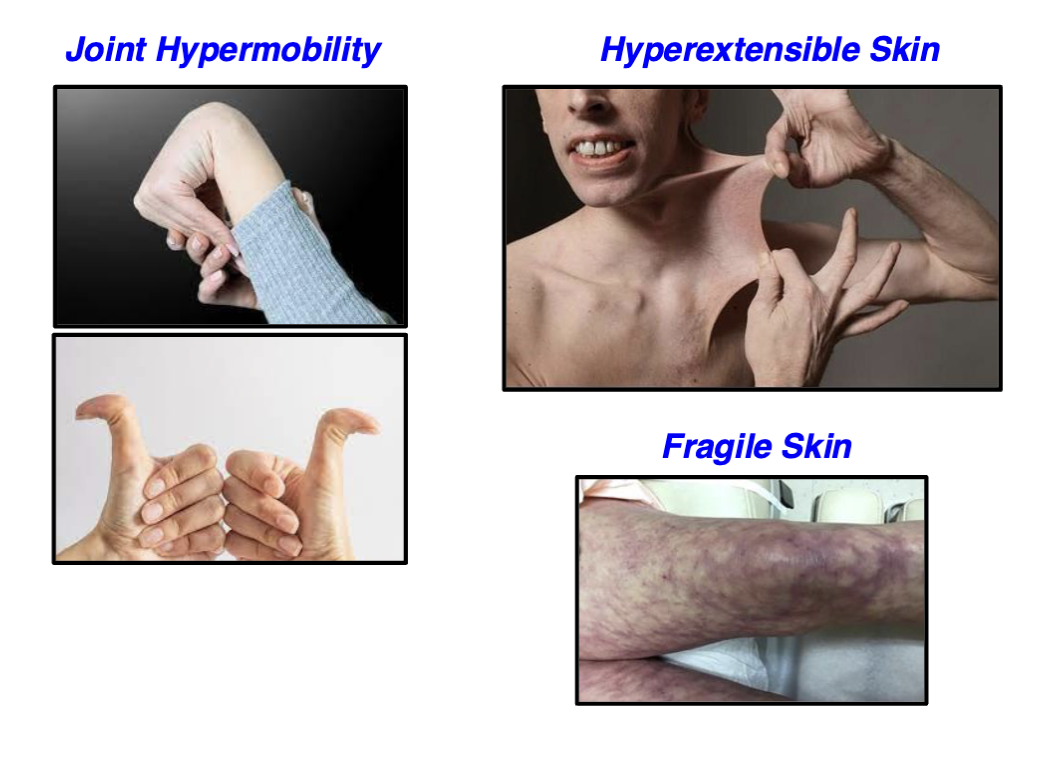
Ehlers Danlos Syndrome (EDS):
This syndrome comprises 13 different genetic mutations involving connective tissue, but most often affects the genes for different types of collagen
Generally is a rare disease, but some variants are more common
More often affects females
Lifespan can vary from near normal to reduced depending on mutation
Genetic mutations involving connective tissue, most
often the genes for collagen
Most mutations result in:
Hypermobility of the joints
Hyperextensible skin
Thin and fragile skin
Some mutations have an increased risk of heart valve disease and/or arterial rupture
Marfan Syndrome (MFS):
Somewhat common disease (1:5000 persons) usually caused by gene mutations in connective tissue protein Fibrillin-1
Fibrillin-1 maintains the structure of connective tissue, particularly in elastic tissue found in blood vessels, lungs, tendons and ligaments
Equally affects females and males
Patients usually have reduced life-span due to aortic rupture and other cardiac problems
Autosomal dominant inheritance, severity is variable depending on the gene mutation (i.e., some mutants are worse than others)
Defect in Fibrillin-1 gene produces multiple anomalies:
Tall and thin with long arms and legs
Long thin fingers and toes
Anomaly in the sternum (chest bone)
Eye problems include retinal detachment
Aorta and heart valve defects are the most serious complications
Systemic Autoimmune Diseases:
more than 100 diseases:
All are characterized by autoantibodies and/or autoreactive T-cells to “self antigens”
Most diseases largely affect one tissue or organ, but all display some level of systemic pathology
DO NOT CONFUSE Autoimmune Diseases with the recently described Autoinflammatory Diseases
Autoinflammatory Diseases present with systemic symptoms much like autoimmune diseases BUT there are NO autoantibodies or autoreactive T-cells. The defect are mutations of intracellular immune sensor molecules in the innate immune cells (macrophages, neutrophils). These defective cells target the body’s own healthy tissues by mistake. This can cause intense episodes of inflammation that result in fever, rash, and/or joint swelling.
Systemic Autoimmune Diseases:
Polymyositis and Dermatomyositis: Discussed earlier
Rheumatoid Arthritis: Discussed earlier
Vasculitis: Inflammation of blood vessels, briefly mentioned in Cardiovascular
Inflammatory Bowel Disease: Discussed in GI lecture
Autoimmune Atrophic Gastritis: Discussed in GI lecture
Graves’ Disease: Discussed in Endocrine lecture
Hashimoto’s Thyroiditis: Discussed in Endocrine lecture
Addison’s Disease: Discussed in Endocrine lecture
Type 1 Diabetes: Discussed in Endocrine lecture
Psoriasis: Briefly mentioned earlier
Sjögren’s Syndrome: Decreased secretions (tears, saliva, lung and GI tracts)
Multiple Sclerosis: Neurological disease
Myasthenia Gravis: Neuromuscular disease, discussed in Immunology lecture
Sarcoid: ??? Discussed in Lung lecture: has characteristics of an autoimmune disease and an infectious disease but is neither. It is in a class by itself!
Systemic Lupus Erythematosus (SLE):
The prototypic autoimmune disease
Highly heterogeneous disease manifestations and highly variable disease activity, it has been stated that “patients are like snowflakes, no two cases are alike”
● is often just called Lupus (Latin word for Wolf)
● Chronic condition with relapsing and remitting disease activity
● Genetic association with specific MHC class II genes
● Disease triggers: UV light, cigarette smoking, estrogen levels
● Disease incidence:
● Female: Male = 10:1
● Can affect a person at any age, but average age of onset is 25 years
● SLE shows world-wide distribution, prevalence of 0.1% in global population
● Disease is more common and severe in African, Asian, Hispanic populations
● Very challenging to treat, best to refer to a Rheumatologist
Clinical Features of SLE: Disease Onset:
At any age from infants to elderly! Symptoms are variable ranging from acute (rapid) and very severe to very slow and insidious
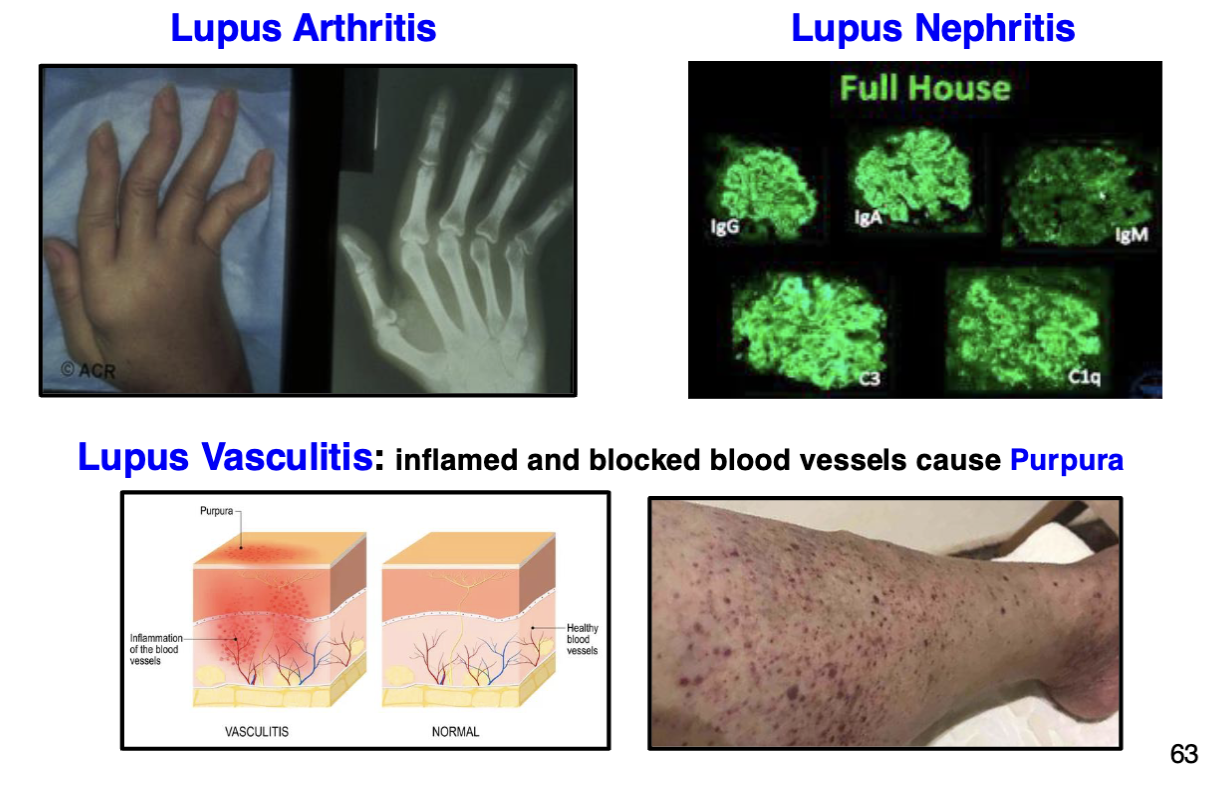
4 Major Disease Manifestations: SLE:
Inflammatory Arthritis (similar to Rheumatoid Arthritis)
Nephritis (Membranous Glomerulonephritis, Nephrotic Syndrome)
Vasculitis (Purpura)
Lupus (Malar) Rash: Rash forms after exposure to UV light and presents as a distinct butterfly pattern across the bridge of the nose and both cheeks
Triggered by exposure to sunlight (UV wavelengths)
Usually occurs on face and hands, but can appear on any part of the body exposed to UV light
Rash can persist for many days to weeks depending on severity
Secondary Manifestations of SLE:
Heart and lung disease (Note: that SLE can affect ANY organ)
Pathological Features of SLE: Pathological Findings:
Anti-nuclear antibodies (ANA) to DNA and DNA-associated molecules are a consistent finding in SLE
SLE: Mechanisms of Tissue Injury:
Autoantibodies deposited in tissue form immune complexes that activate the complement system and innate immune cells (neutrophils, macrophages, etc.) that cause tissue damage
SLE: Treatment:
Varies from patient to patient
NSAIDs (aspirin, ibuprofen, etc.) to reduce pain and inflammation
Corticosteroids for more severe cases
Hydroxychloroquine is usually prescribed for most SLE patients since it is effective in reducing the Lupus malar rash
Systemic Sclerosis:
Multisystem disease characterized by vascular dysfunction and progressive fibrosis of skin and internal organs
Also known as Scleroderma
Primarily affects the skin, but also lung, heart, kidneys, GI tract
Has variable disease manifestations and activity
Autoantibodies to various intracellular antigens are detected in blood
Raynaud’s Disease (Phenomenon): Constriction of cutaneous blood vessels in hands and feet is almost always found
10-20% of global population is thought to have some form of Raynaud’s
However, most people with Raynaud’s do not have SSc
Disease Incidence: Overall global incidence is about 0.03% in all populations
Gender incidence is about 5:1 female:male, females often have a younger age of onset (age 20-40), but the disease is less severe than in males
Disease Subsets:
Limited Cutaneous: fibrosis limited to skin of arms, legs, face and neck
Diffuse Cutaneous: more rapid disease progression with lung fibrosis
New Potential Treatment for Autoimmune Diseases?:
Clinical trial of 15 patients with severe autoimmune disease (8 SLE, 4 SSc, 3 Myositis) who were not responding to treatment.
Follow-up 15 months after single dose of CAR T-cells: All patients were in remission and no autoantibodies detected!