Chapter 2: Electrical Activity of the Heart
1/109
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
110 Terms
Cell Membrane Potentials
What is resting membrane potential?
Electrical potential of a resting cell
measured with a microelectrode
outside of the cell is 0 mV
Cell Membrane Potentials
What is the resting potential of a ventricular MYOCYTE (Em)?
90mV
Cell Membrane Potentials
How was the resting membrane of a ventricular myocyte determined by?
the concentration of + and - ions across the cell
relative permeability of the cell membrane to these ions
ionic pumps that transport ions across the cell membrane
Cell Membrane Potentials
What are the movement of ions in and out of the myocyte?
high concentration of K+ inside the cell diffuses out
high concentration of Na+ outside the cell diffuses in
high concentration of Ca++ outside the cell and diffuses in
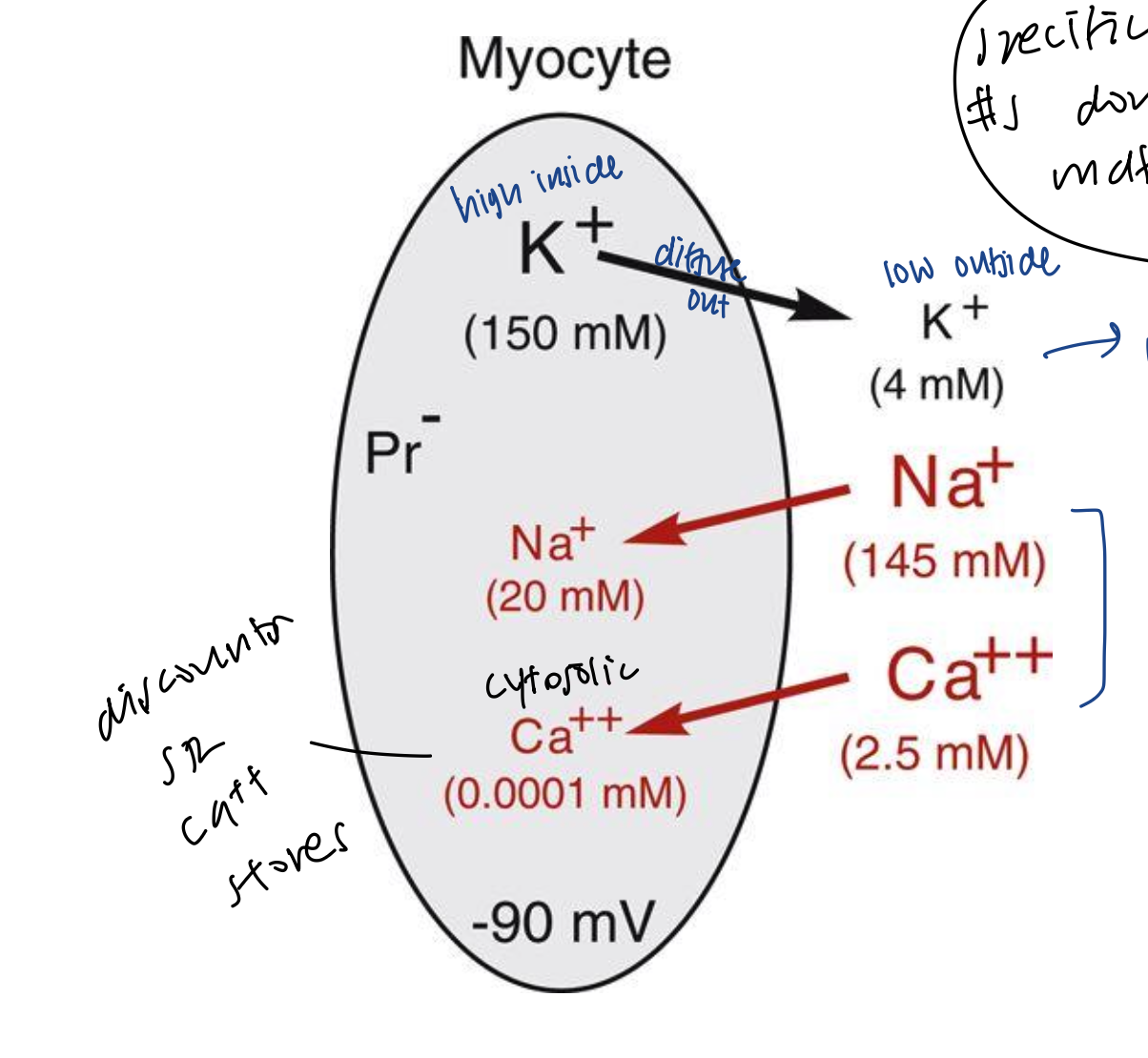
Cell Membrane Potentials
Why is K+ important?
It is the most important ion in determining the resting membrane potential
Cell Membrane Potentials
What directs the concentrations of ions?
Activity of energy-dependent ionic pumps and semi-permeable membrane
Cell Membrane Potentials
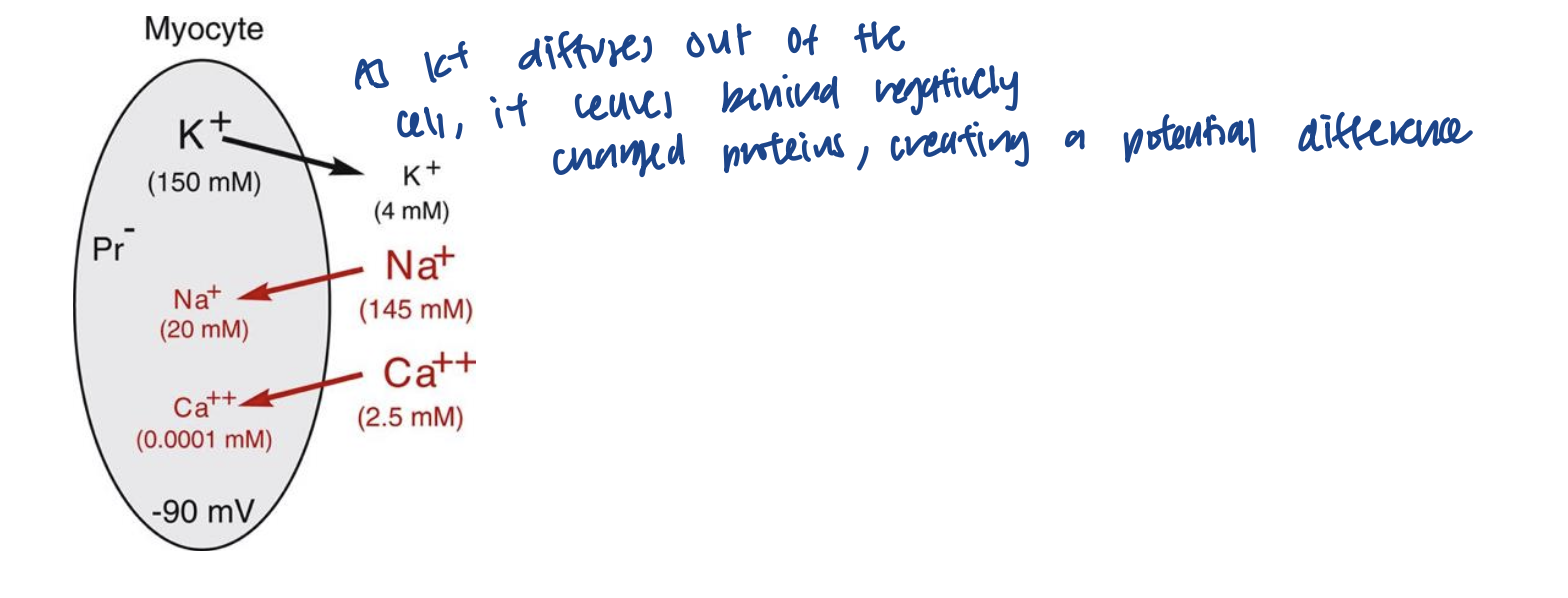
When K+ diffuses out, what happens to the cell?
As K+ diffuses out of the myocyte, it leaves behind negatively charged particles, creating a potential difference
Cell Membrane Potentials
Why is the equilibrium potential important and what is it dependent on?
It is the membrane potential that is necessary to oppose the outward movement of an ion down its gradient
most important is the equilibrium constant for K+ because it keeps the K+ from diffusing down its chemical gradient and out of the cell
Cell Membrane Potentials
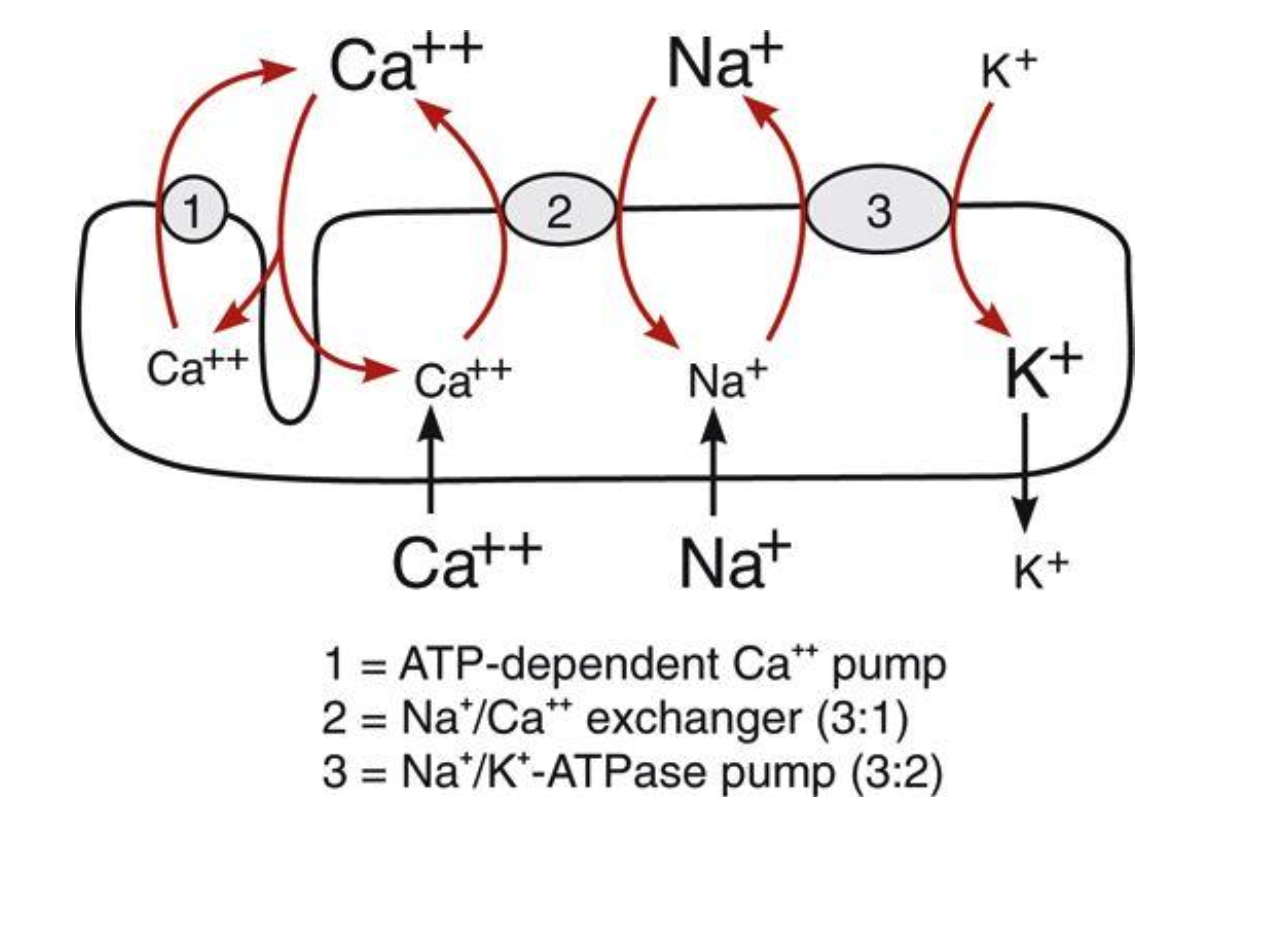
How are ionic gradients maintained?
concentration gradients maintained via energy-using ionic pumps
require ATP
the Na+/K+ pump is electrogenic and pumps 3 Na+ for every 2 K+ (pumping more positive out of the cell turns it into a negative potential within the cell)
Cell Membrane Potentials
What happens if the Na+/K+ pump stopped working?
If pump inhibited by diogoxin, the Na+ accumulates within the cell and intracellular K+ falls, resulting in a less negative resting membrane potential
Cell Membrane Potentials
What must be removed from the cell following a depolarization and how?
Ca2+ needs to be extracted from the cell via 2 mechanisms
ATP-dependent Ca++ pump that actively pumps Ca++ out and generates a small negative potential
NA+/Ca++ antiporter exchanger that can be flipped depending on membrane potential, and exchanges 3 Na+ for every 1 Ca+
Ion Channels
What are the 2 types of ion channels?
voltage-gated: respond to changes in membrane potential (ex: Na+, K+, and Ca++ during cardiac action potentials)
receptor-gated: respond to chemical signals through membrane receptors (ex: ACh binding to open special K+ channels)
Ion Channels
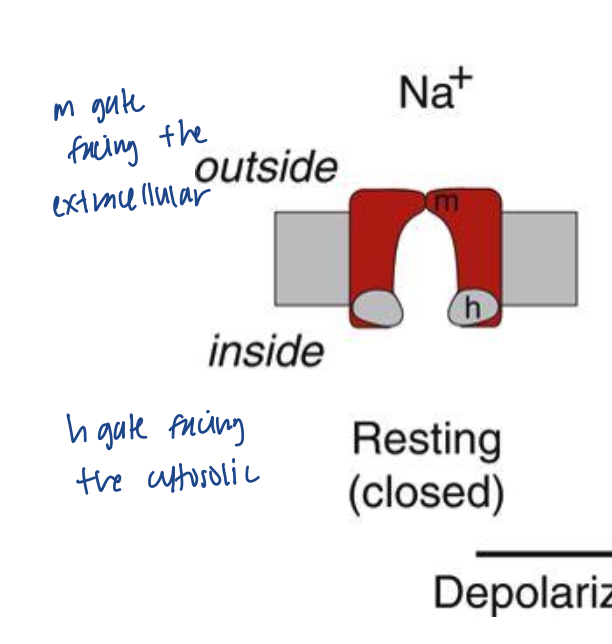
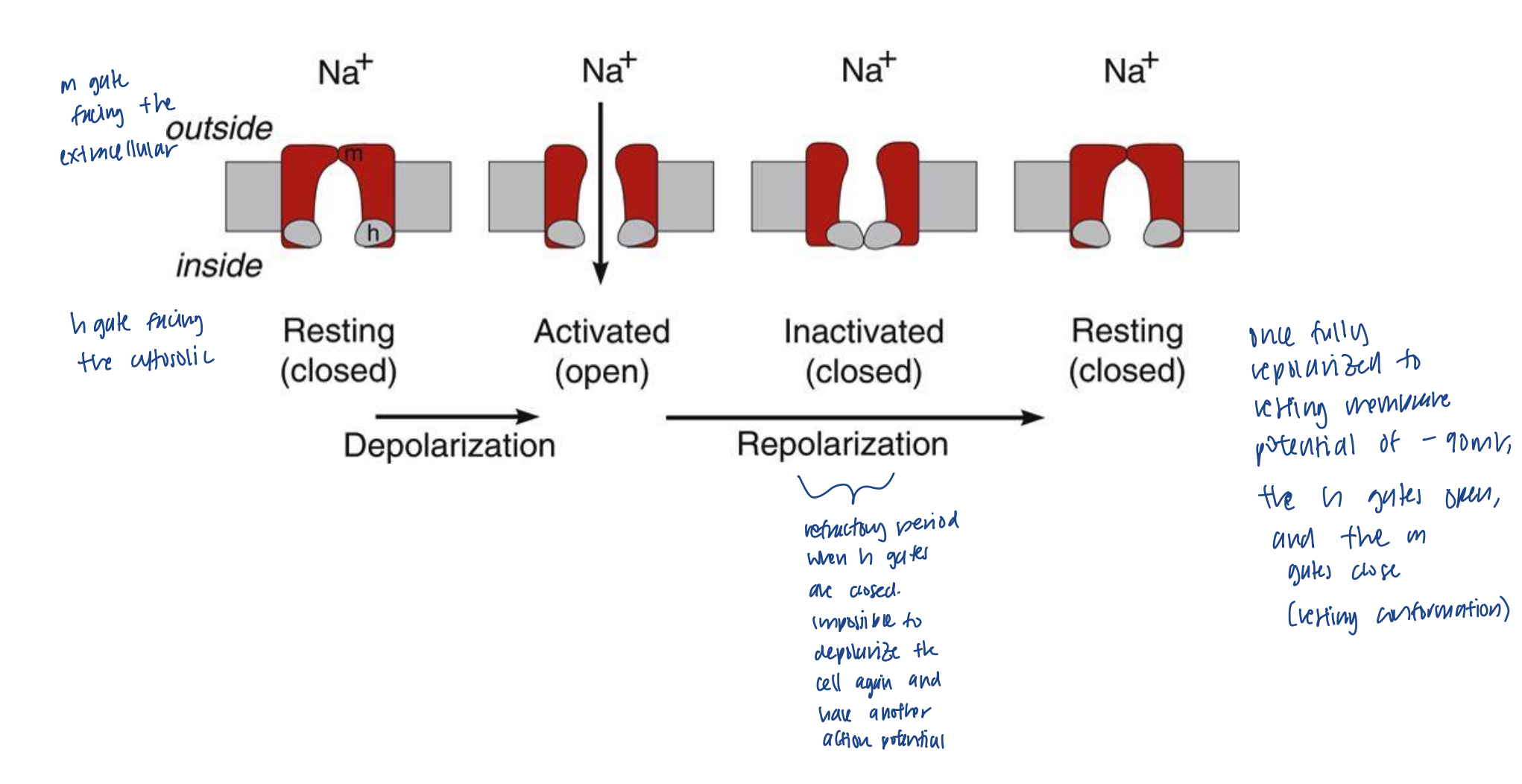
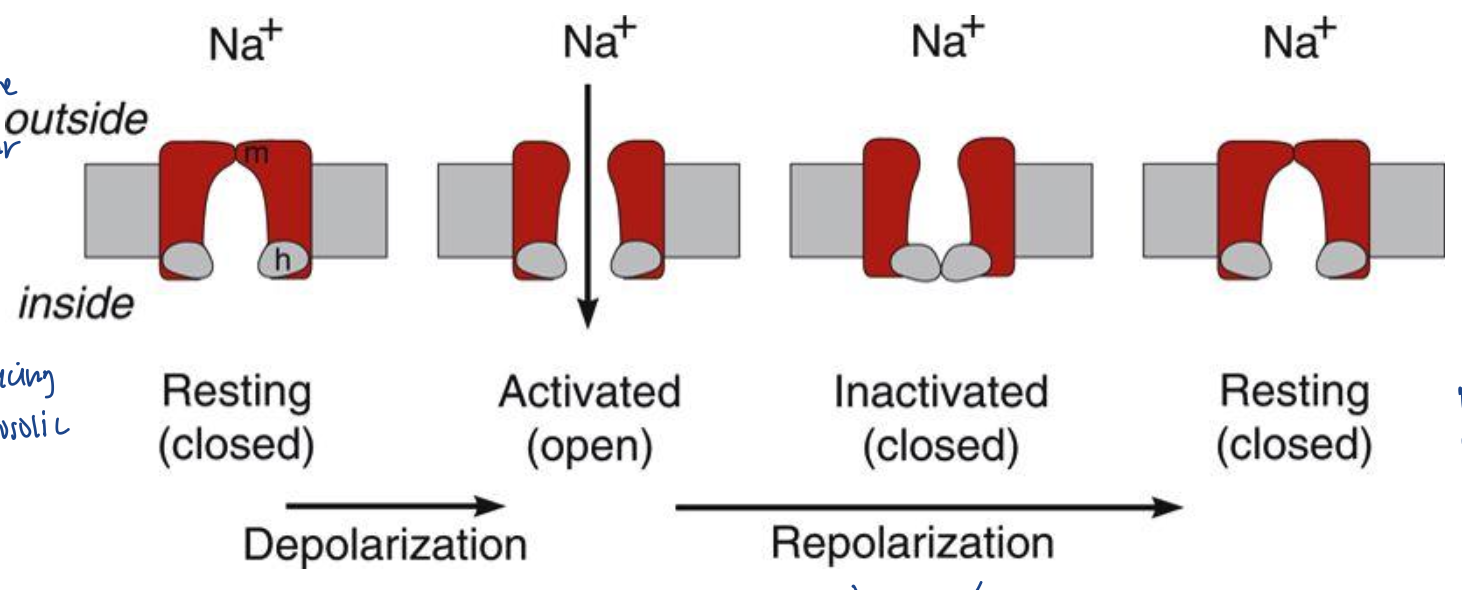
At resting membrane potentials, what happens to the ion channels?
Na+ gates are closed
m gate (activation gate) is blocking the opening on the membrane
h gate (inactivation gate) is open during this time
Ion Channels
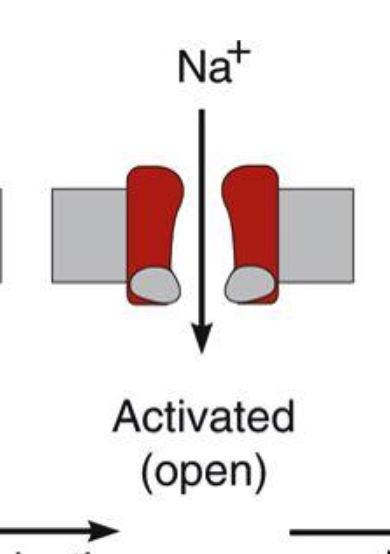
When there is a disruption in voltage (depolarization), what happens?
m gates become rapidly activated and open, allowing Na+ in through its chemical gradient
as the m gates open, the h gates begin to close slowly (m gates open more rapidly than h gates closing so this allows Na+ to briefly enter the cell)
Ion Channels
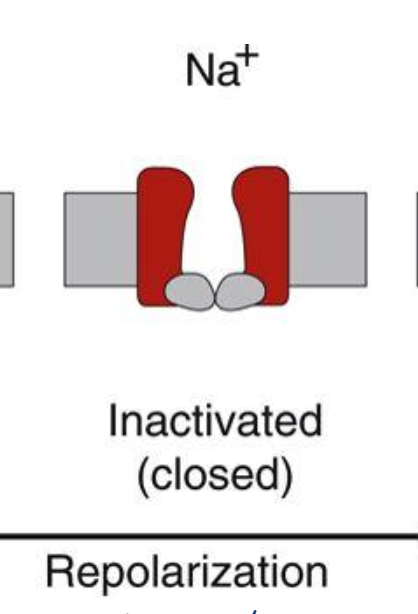
After a few milliseconds, what happens to the channels?
the h gate closes and the flow of Na+ stops
Ion Channels
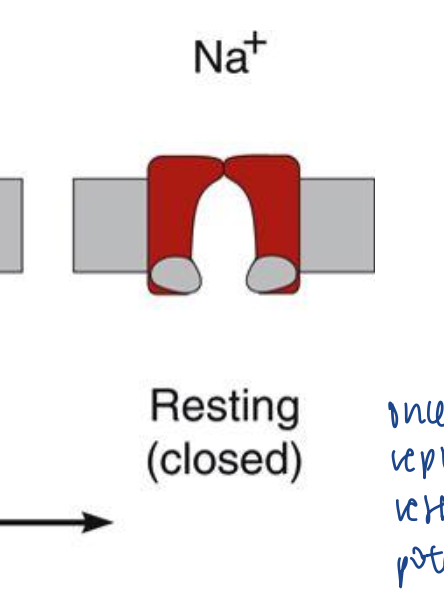
What happens finally to the ion channels?
at the end of repolarization, the m gates close, and the h gates open again
Ion Channels
When is the refractory period here?
during the inactivated stage when h gate closes. this is when it is impossible to depolarize the cell again to have another depolarization
Ion Channels
What happens to ion channels during partial depolarization?
fast Na+ channels respond differently
partial depolarization causes the closing of h-gates, inactivating the Na+ channel
the more the cell depolarizes (partially), the more inactivation of the Na+ channels
so during these slow depolarizations, more time allows for the closing of h gates as the m gates open
go from straight from resting to inactivated
Action Potentials
When does action potentials occur?
when the membrane potential suddenly depolarizes, and then repolarizes
Action Potentials
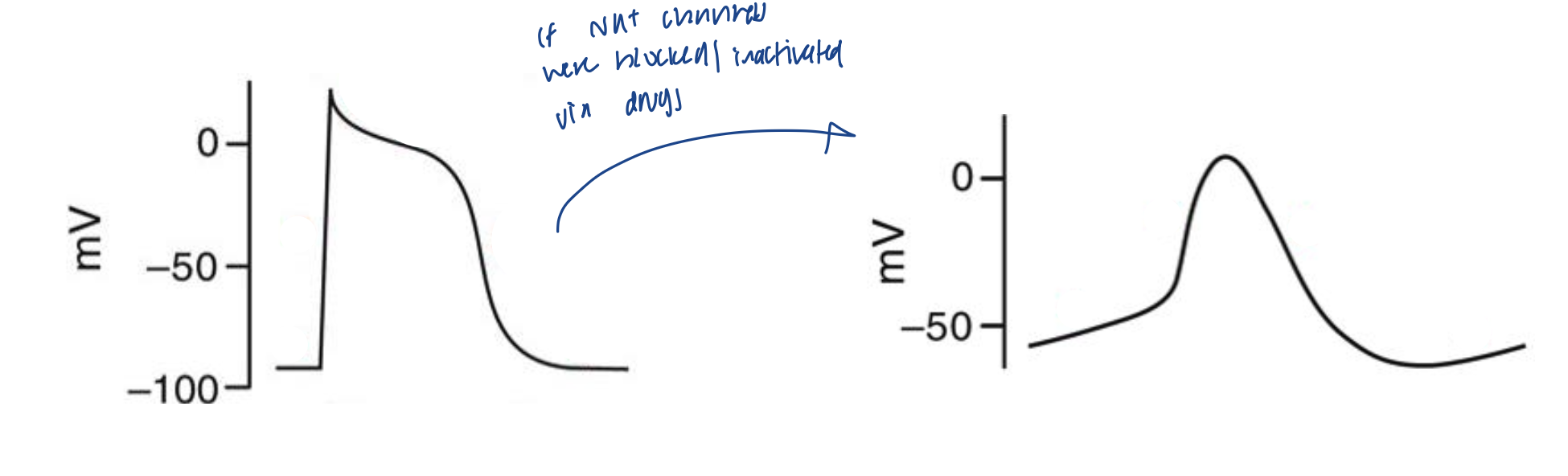
What are the two types of cardiac action potentials?
non-pacemaker
triggered by nearby cells (not spontaneous)
cardiac myocytes
pacemaker
spontaneous
nodal cells (SA and AV node)
Non-pacemaker Action Potentials
Do non-pacemaker cells have a true resting membrane?
non-pacemaker cells have a true resting membrane potential that remains near the equilibrium potential for K+
Non-pacemaker Action Potentials
What are the different phases?
phase 4: resting membrane potential
phase 0: rapid depolarization caused by the conductance of Na+
initiated by the increasing Na+ into the cell, and moves the membrane potential away from the K+ equilibrium membrane potential, and closer to the Na+ equilibrium membrane potential
phase 1: initial repolarization
caused by the opening of special (outward) K+ channels
also caused by inactivation of Na+ channels
phase 2: plateau phase
delayed repolarization due to slow influx of Ca++ which occurs through long-lasting L-type Ca+ channels
phase 3: repolarization
K+ conductance increases and Ca++ conductance decreases
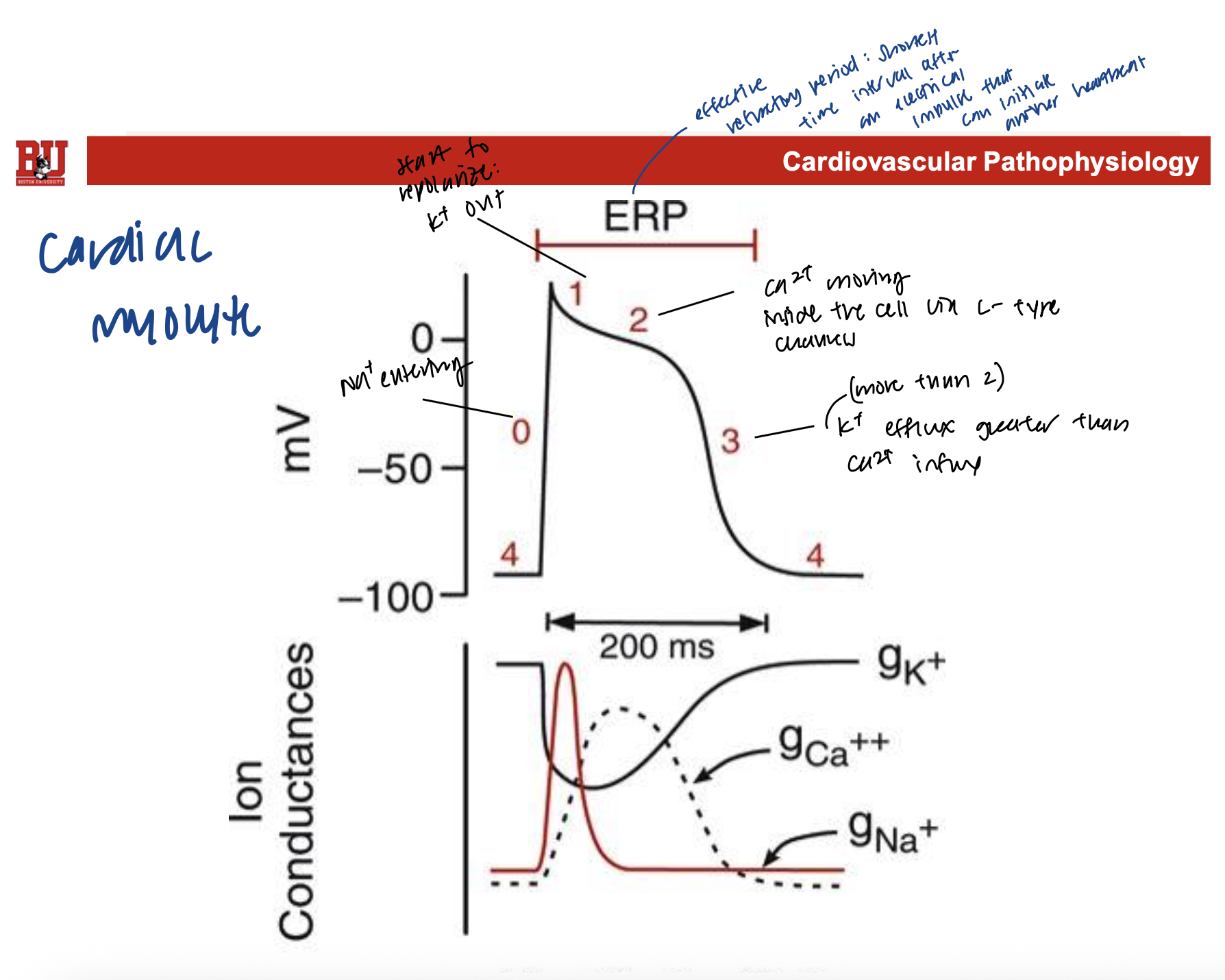
Non-pacemaker Action Potentials
Label the curve with what is happening at the phases in simple terms. What is ERP and when is that?
phase 4: -90 mV resting
phase 0: rising above 0 mV and is when Na+ enters
phase 1: dips closer to 0, and starts repolarization with K+ exits
phase 2: delay in repolarization as Ca2+ moves into the cell
phase 3: dips all the way down and near -90 mV because K+ efflux is greater than Ca+ influx
phase 4: back to -90 mV resting
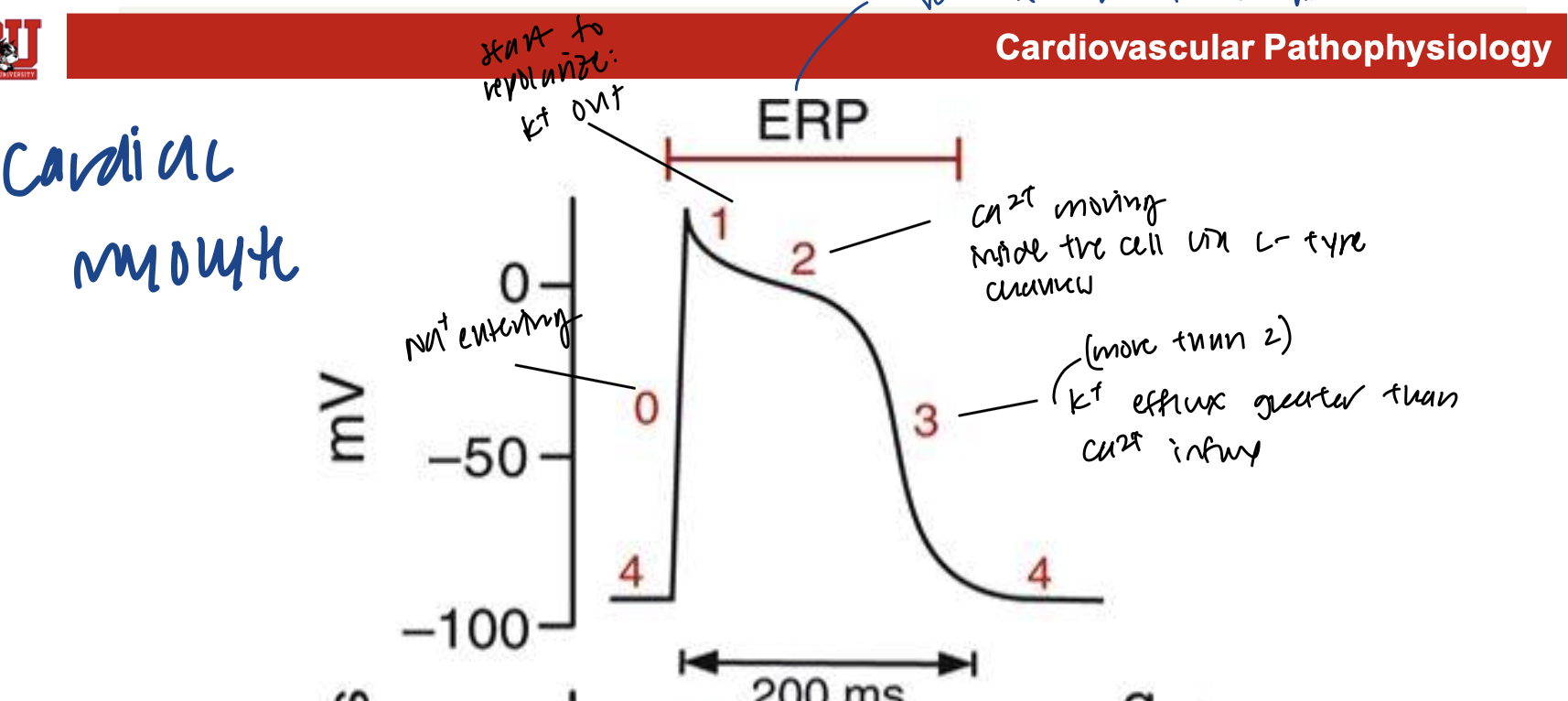
Non-pacemaker Action Potentials
What is ERP and when is that?
ERP is the effective refractory period, which is stages when a new action potential cannot be initiated
phases 0, 1, 2, and part of 3 = unexcitable
Non-pacemaker Action Potentials
What is ARP and when is that?
absolute refractory period
phases 0, 1, and most of 2
h-gates are closed, so no new action potentials can be produced
this serves to limit the amount/duration of action potentials
also allows the heart to have adequate time to fill and eject blood
Non-pacemaker Action Potentials
What is RRP and when is that?
relative refractory period
final part of phase 3 and part of 4
myocytes are capable of new action potentials, but a lot of stimuli are required
Na+ channels are not fully recovered (only when Na+ channels are fully recovered can the cells become excitable by normal depolarization magnitudes)
Non-pacemaker Action Potentials
Why would you prescribe calcium channel blockers to someone with a high HR?
high HR means there are short action potentials, meaning more heart beats are fitted in a minute
this drug can change the length of time that the action potential lasts
by blocking Ca++ channels, it prevents Ca++ rush and makes phase 2 slower because Ca++ doesn’t enter as much but enters for longer
thus, they can fit less action potentials/contractions per minute
Pacemaker Action Potentials
Do pacemaker cells have a true resting membrane?
no, pacemaker cells do not have a true resting membrane due to leak channels
Pacemaker Action Potentials
What is the rate of depolarization in comparison to non-pacemaker cells? Why?
pacemaker action potentials driven by the slow, inward Ca2+ currents (L-type Ca2+ channels)
so, it is slower compared to the “fast response” from non-pacemaker cells’ fast Na+ currents
Pacemaker Action Potentials
What sets the pace?
Cells in the sinoatrial (SA) node
Pacemaker Action Potentials
What else can set the pace, but…?
Atrioventricular (AV) node is also capable
this happens when SA node is slow/fails to reach the AV node
normally, there is “overdrive suppression” where SA node inhibits the AV by firing faster
but, if SA node slows/ fails, then overdrive suppression is gone, and secondary pacemakers can take over the heart’s main pacemaker
Pacemaker Action Potentials
What is ectopic focus?
when the AV node takes over SA node and becomes the heart’s main pacemakers
Pacemaker Action Potentials
What are the phases of pacemaker action potentials?
phase 0: upstroke of action potential
voltage opens the L-type Ca++ channels, allowing increased Ca++ to flow (slowly) into the nodal cells
phase 3: repolarization
depolarization from phase 0 causes voltage-gated K+ channels to open, and K+ leaves the cell
depolarization also causes Ca++ channels to become inactivated, decreasing Ca++ conductance
phase 4: spontaneous depolarization
phase of repolarization is restricted because K+ channels start to become
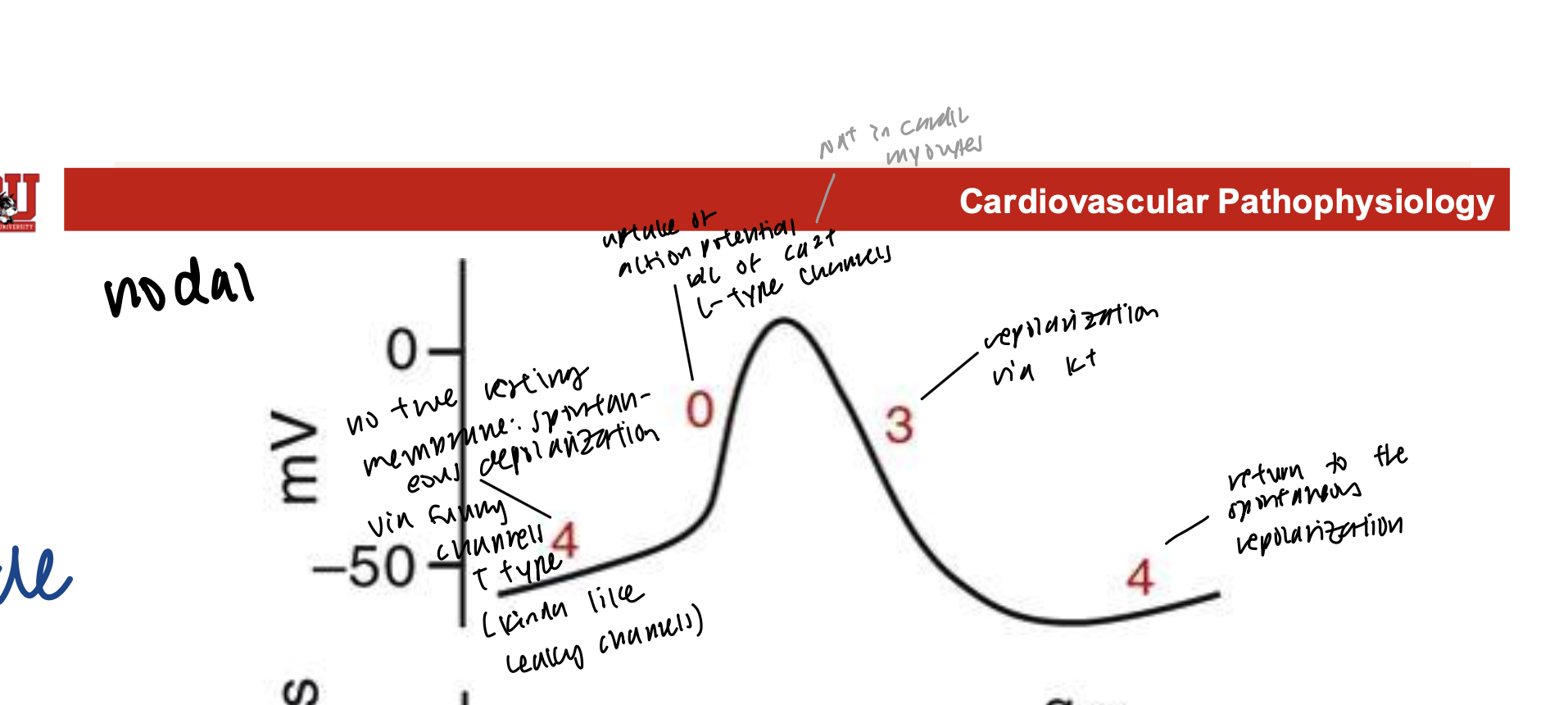
Pacemaker Action Potentials
In the repolarized states (phase 4), how is there a slow tick of depolarization?
these funny currents are from the slow inward movement of Na+ throughout the whole phase 4
movement of Na+ into the cell contributes to depolarization
in second half of phase 4, there is a small increase in Ca++ conductance through T-type Ca++ channels
Pacemaker Action Potentials
What is the importance of T-type Ca++ channels?
if T-types are blocked, there will be no beating, and will die
it opens briefly at a very negative voltage
cannot be blocked by classical L-type Ca++ channels
Pacemaker Action Potentials
How do calcium channel blockers affect pacemaker cells?
since pacemakers’ depolarization depends on Ca++, with low concentration of Ca++ influx, the phase 0 will take a long longer
so, there will be fewer potentials per minute, and shorter rate of conductance means slower HR
Ca++ Channel Blockers
What is dromotropy and chromotropy?
dromotrophy: slow conductance rate
chromotropy: rate of depolarization of nodes
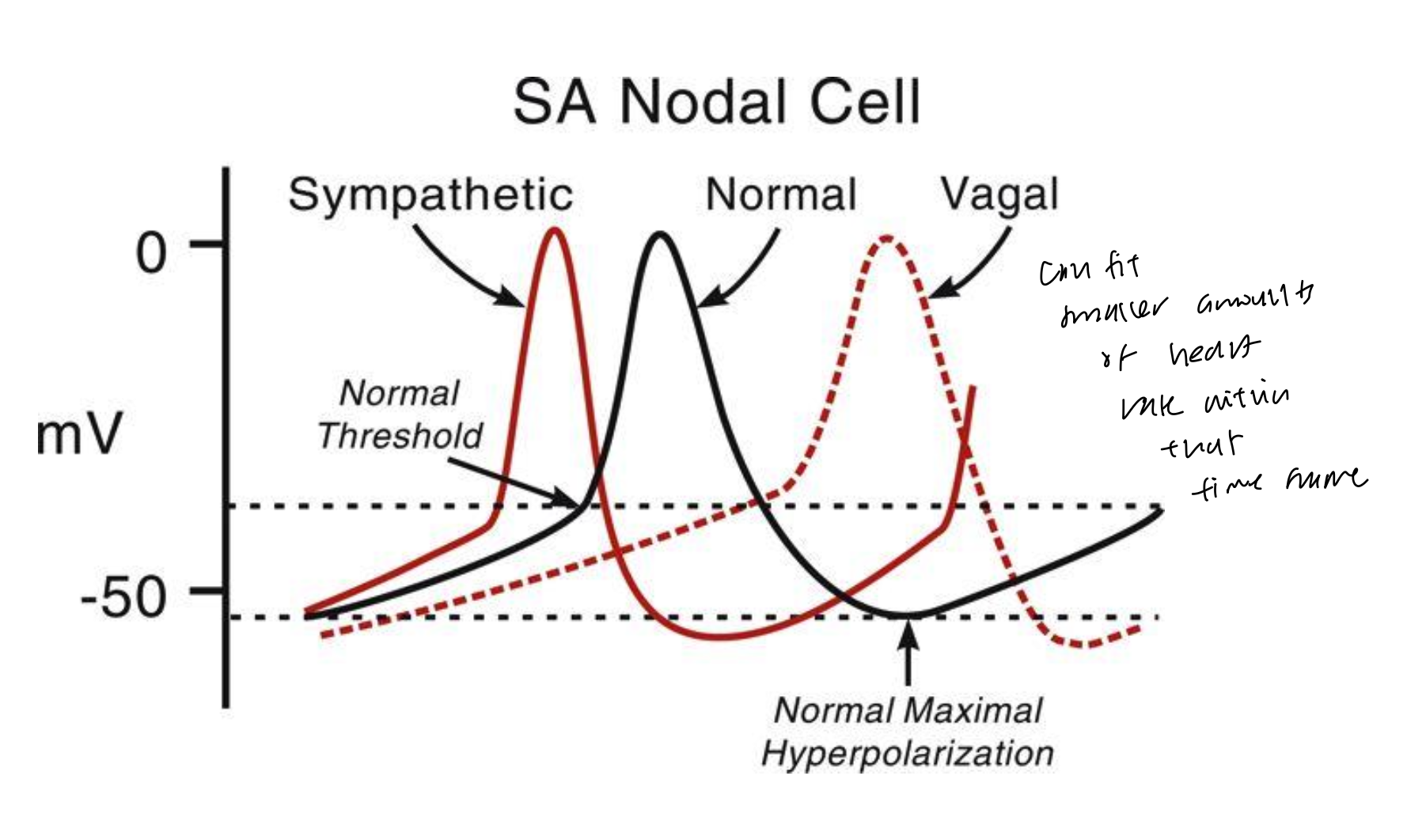
Regulation of SA Nodal Pacemaker Activity
Without any external factors, what is the intrinsic firing from the SA node?
100 bpm
Regulation of SA Nodal Pacemaker Activity
However, HR can range below 50 and to more than 200. How?
adjustments are made by the autonomic nerves acting on the SA node
vagal tone HR <100, happens at low resting HR and it is more dominant than the sympathetic influences
vagal withdraw + sympathetic activity: HR > 100 happens when increased sympathetic activity (such as NE binding to beta-adrengeric receptors to increase Ca++ and make depolarizations faster)
Regulation of SA Nodal Pacemaker Activity
What is chronotropy?
chronotropy is the adjustment in HR
+ chronotropy = increased HR
- chronotropy = decreased HR
Regulation of SA Nodal Pacemaker Activity
Autonomic control of HR can be influenced by what factors?
increase/decrease of the slope of phase 4
alter the threshold voltage for triggering phase 0
alter the degree of hyperpolarization following phase 3
Regulation of SA Nodal Pacemaker Activity
What happens if NE is released from sympathetic nerves?
binds to beta-adren receptors and activates the G-protein signaling pathway to ultimately increase Ca2+ influx
this increases slope of phase 4 and lowers threshold to depolarize in phase 0
increased chronotropy due to accelerated depol and repol, and shortens the overall cycle length
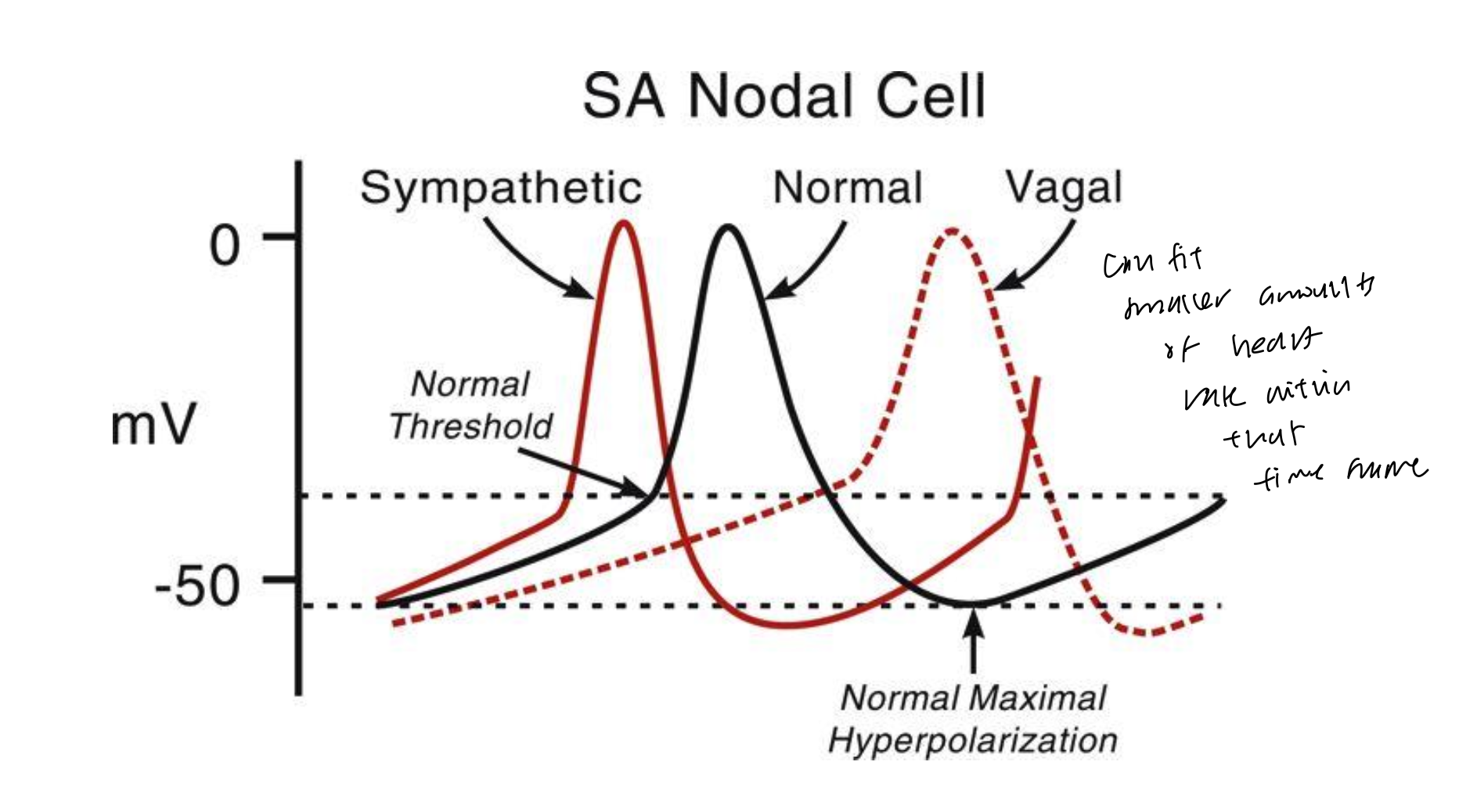
Regulation of SA Nodal Pacemaker Activity
What happens if ACh is released by vagal nerves?
binds to M2 receptors and decreases G-protein signaling pathway, which ultimately decreases Ca2+ influx
this decreases slope of phase 4 because it inhibits “funny currents,” and also makes threshold to depolarize in phase 0 higher
decreased chronotropy due to slower depol and repol
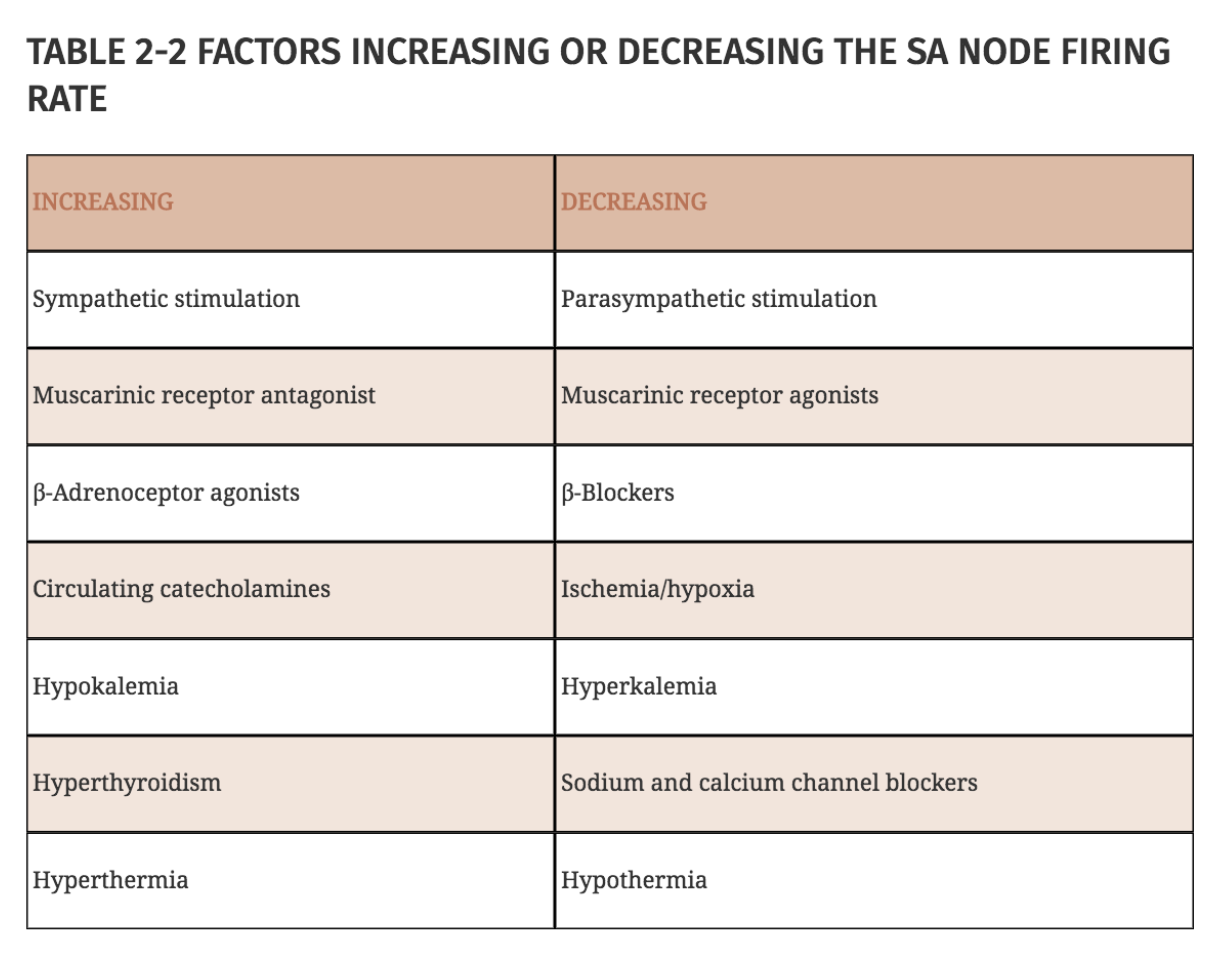
Factors increasing or decreasing SA node firing
Arrhythmias: Abnormal Automaticity
What happens if fast Na+ channels are somehow blocked in cardiac myocytes?
if blocked, cardiac myocytes can behave similarly to nodal cells
slope and amplitiude of phase 0 are depressed
depolarization is brought on by L-type Ca++ channels
could result in spontaneous action potential generation
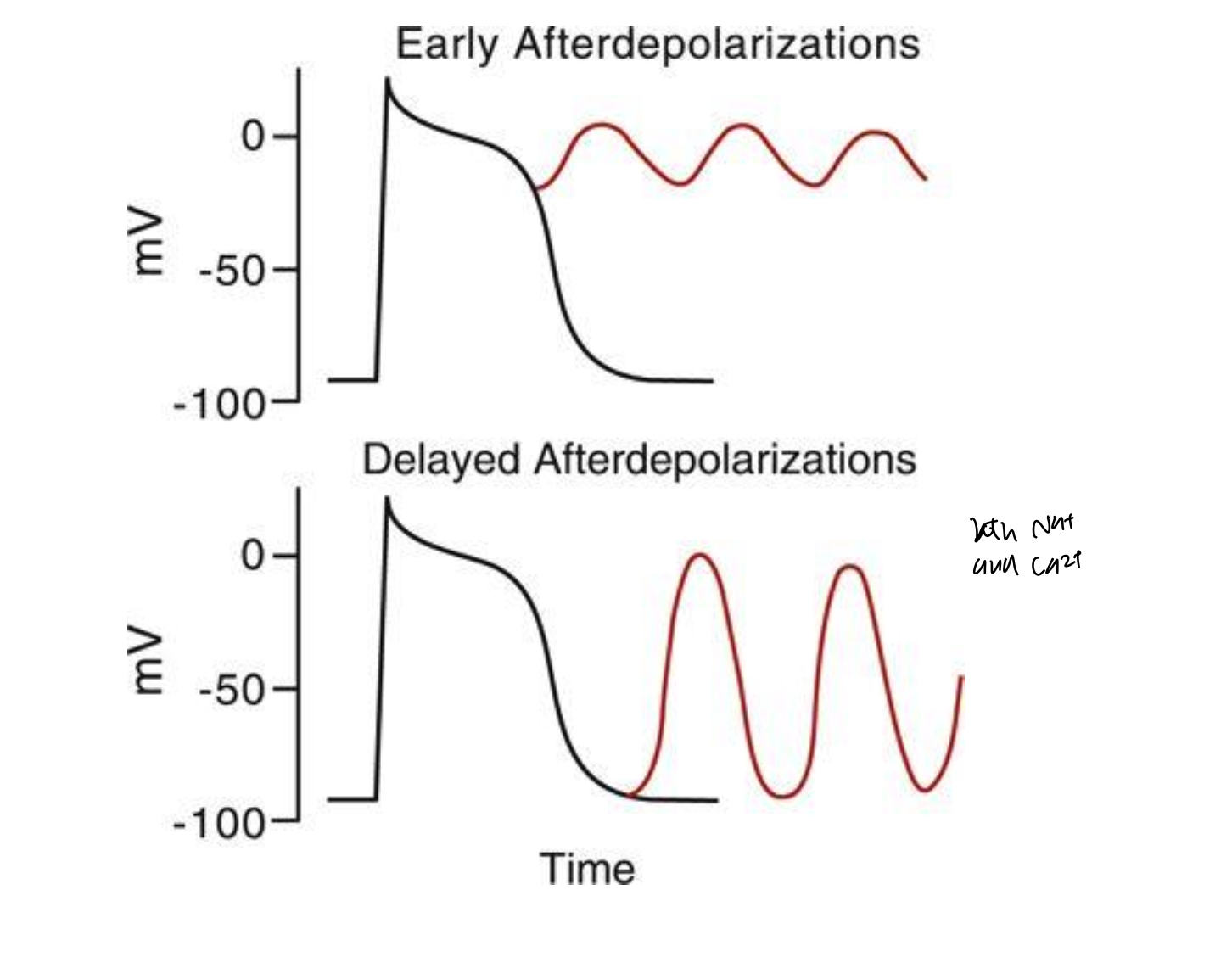
Arrhythmias: Triggered Activity
How does triggered activity happen?
nonpacemaker cells can generate action potentials during abnormal times (phase 3 or 4)
early afterdepolarization happens in phase 3 and occurs bc of the slow Ca2+ influx (since Na+ channels are inactive here)
delayed afterdepolarization happens later in phase 3/early phase 4
Electrical Conduction within the Heart
How are action potentials spread within the heart?
via cell-to-cell conduction
cells joined together by low-resistance gap junctions located at intercalcated disks
leads to cell progagation
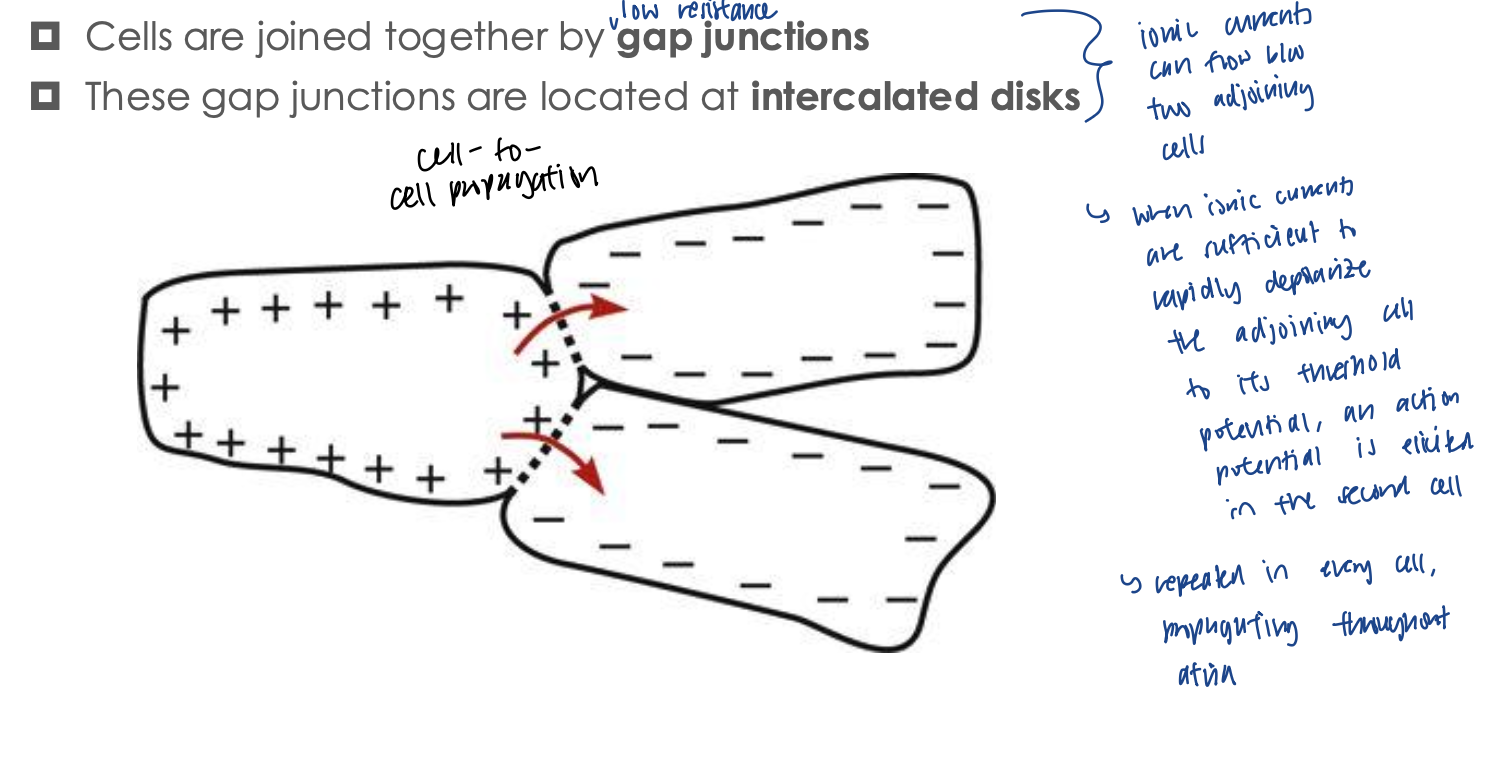
Electrical Conduction within the Heart
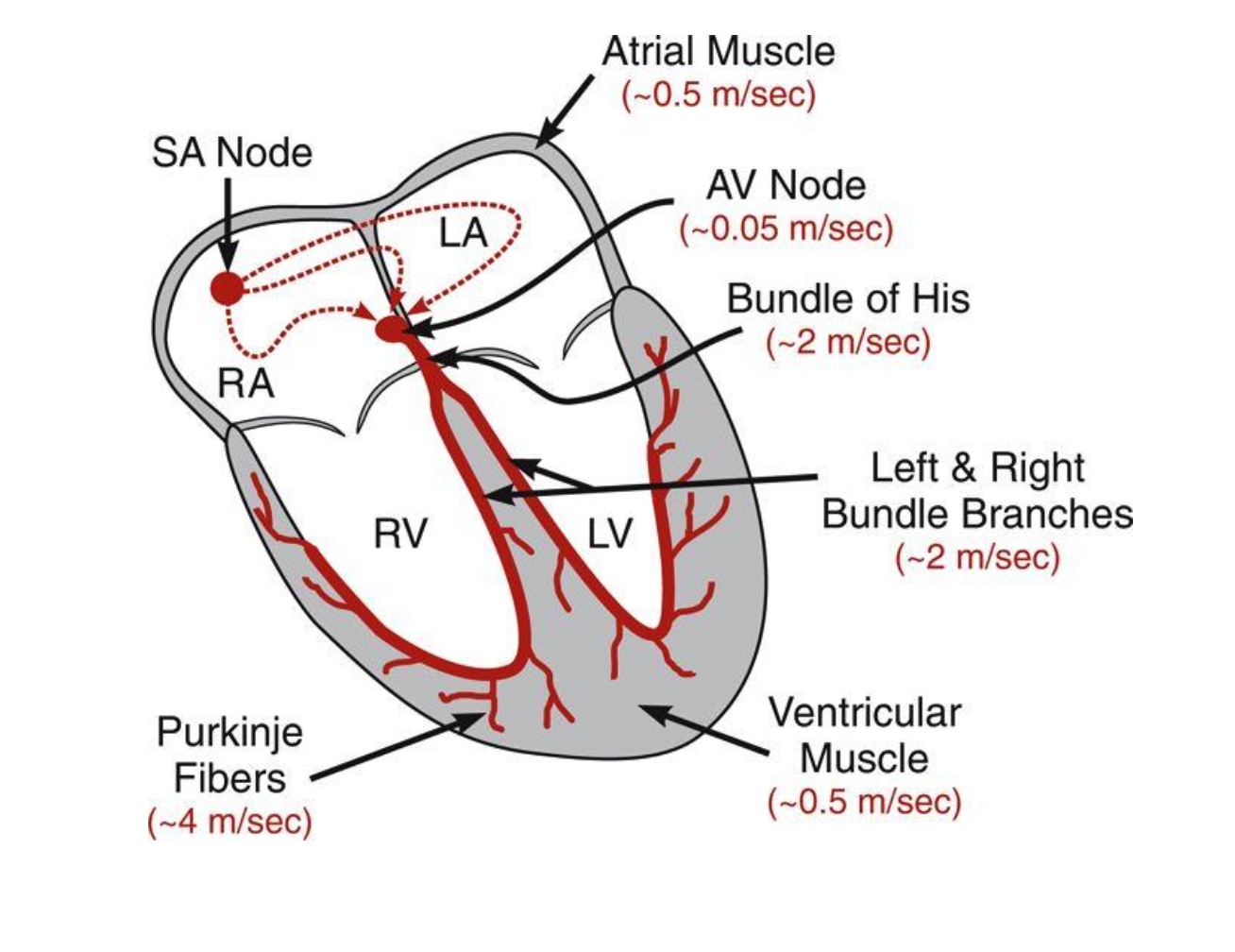
1 → 2 → 3 → 4 → 5 → 6
atria: depolarizes rather fast (0.5)
atrial muscle: connective tissue separates atria from ventricles (not a good conductor)
AV node: action potentials can only enter the ventricles through the AV node
action potential is slowed down to 0.05 to allow sufficient time to complete atrial depol, contraction, and emptying of blood into ventricles before ventricular depola/contraction
Bundle of His: action potential leaves AV node to the ventricle base called the bundle of His at a high speed (2) and splits into right and left bundle branches
Ventricular muscle
Purkinje fibers: branches from bundle of His divide into a system of purkinje fibers, which is the final site for cell-to-cell conduction. has the highest speed of 4
purkinje fiber cells connect with ventricular myocytes
Electrical Conduction within the Heart
What are cell-to-cell conduction regulated by?
Intrinsic and extrinsic factors
Intrinsic
electrical resistance between cells
nature of the action potential (rate of depolarization in phase 0 because the more rapidly a cell depolarizes, the quicker the adjoining cell will too)
Problem 2-2
even though the Na+ channels are partially inactivated, the Na+ will still attempt to reach threshold for depolarization
with less Na+ channels, there are less Na+ entering the cell, which will lead to a prolonged phase 0
it will thus take longer than normal and decrease conduction velocity within the ventricle
Abnormal Conduction
What happens if electrical activation of the heart doesn’t follow the normal path?
arrthythmias and inefficiencies will appear
ex of ineffiency if problem is AV node is blocked: ventricular depolarization will have to rely on slow cell-to-cell conduction between myocytes
Electrical Conduction within the Heart
What is an ectopic beat?
one that occurs (originates) in a location other than the SA node
Tachycardia Caused by Reentry
When does reentry occur?
when conduction pathway is stimulated prematurely by a previous action potential
leads to a rapid, cyclical reactivation
Tachycardia Caused by Reentry
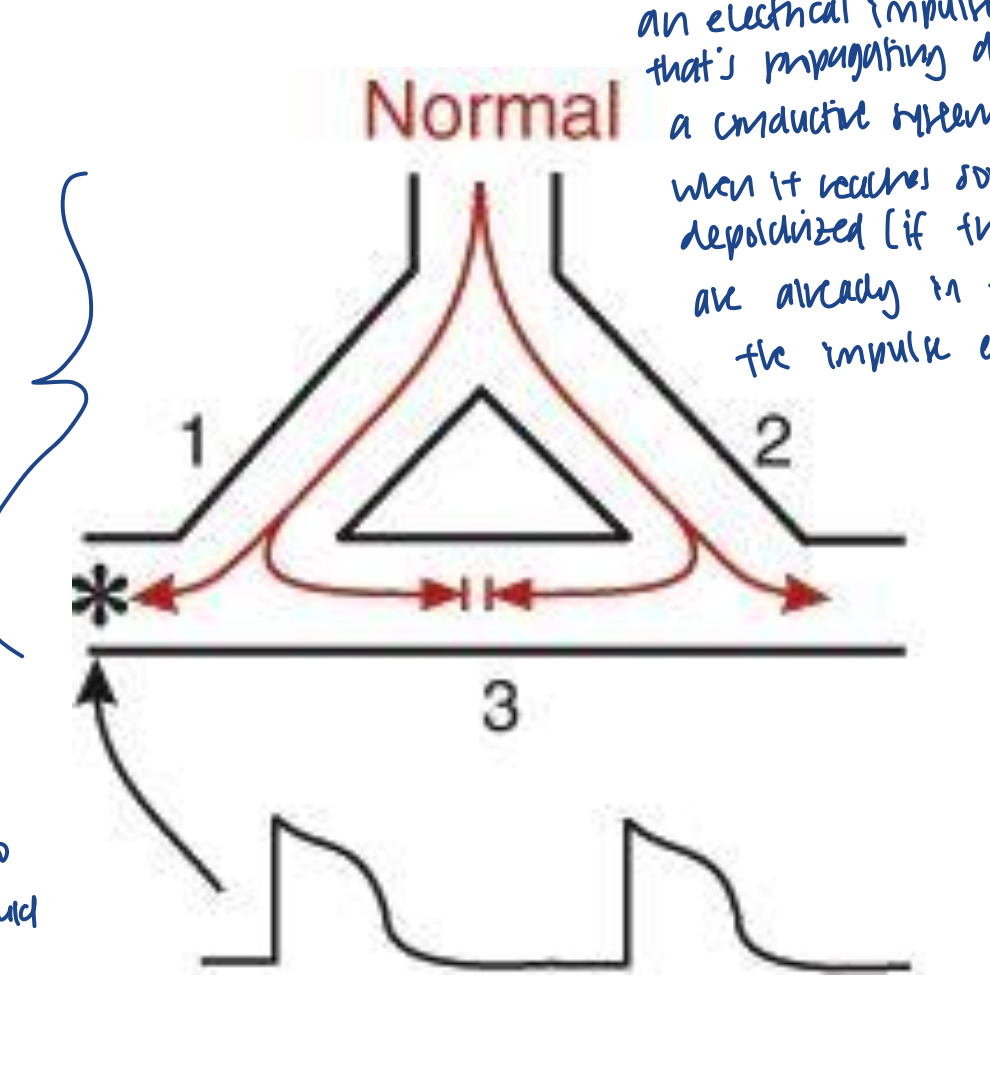
What should happen normally?
in a single purkinge fiber, it has 2 branches (left and right)
the action potential would divide into 1 and 2, and travel down
some of the action potential would travel to the left or right to excite myocytes
some of the action potential from left and right would meet at a common ground (3) to cancel each other out so that a reentry loop would not occur
Tachycardia Caused by Reentry
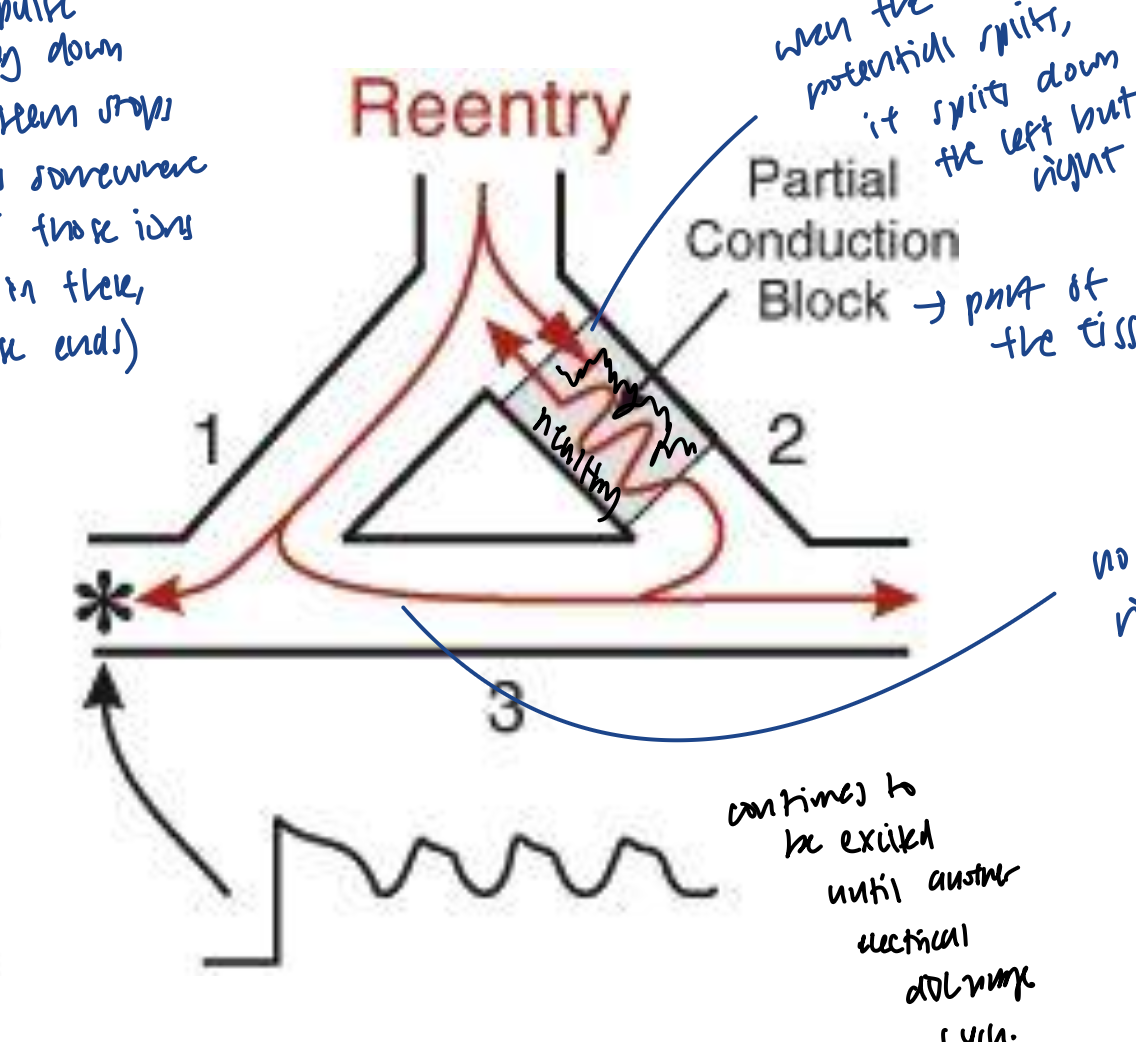
What happens in a reentry?
there is a partial conduction block, where part of the tissue is dead
when action potential travels down the branches of purkinje fiber, it continues to path 1, but not path fully 2 because of the partial blocked dead tissue
action potential from path 1 cannot get canceled out because of the partial dead tissue blocking the traveling in path 2
thus, action potential travels the other side of the dead tissue and reexcite the cells that are beginning to repolarized
this leads to early afterdepolarizations
this is called a reentry loop because cells from SA node are depolarized by the same SA node pace without a new pace
Tachycardia Caused by Reentry
How would you fix a reentry?
can use Ca2+ channel blocker drugs to extend refractory period in non-pacemaker cells so when that same action potential re-enters, it will hit a cell that can’t be reactivated again
Global & Local Reentry
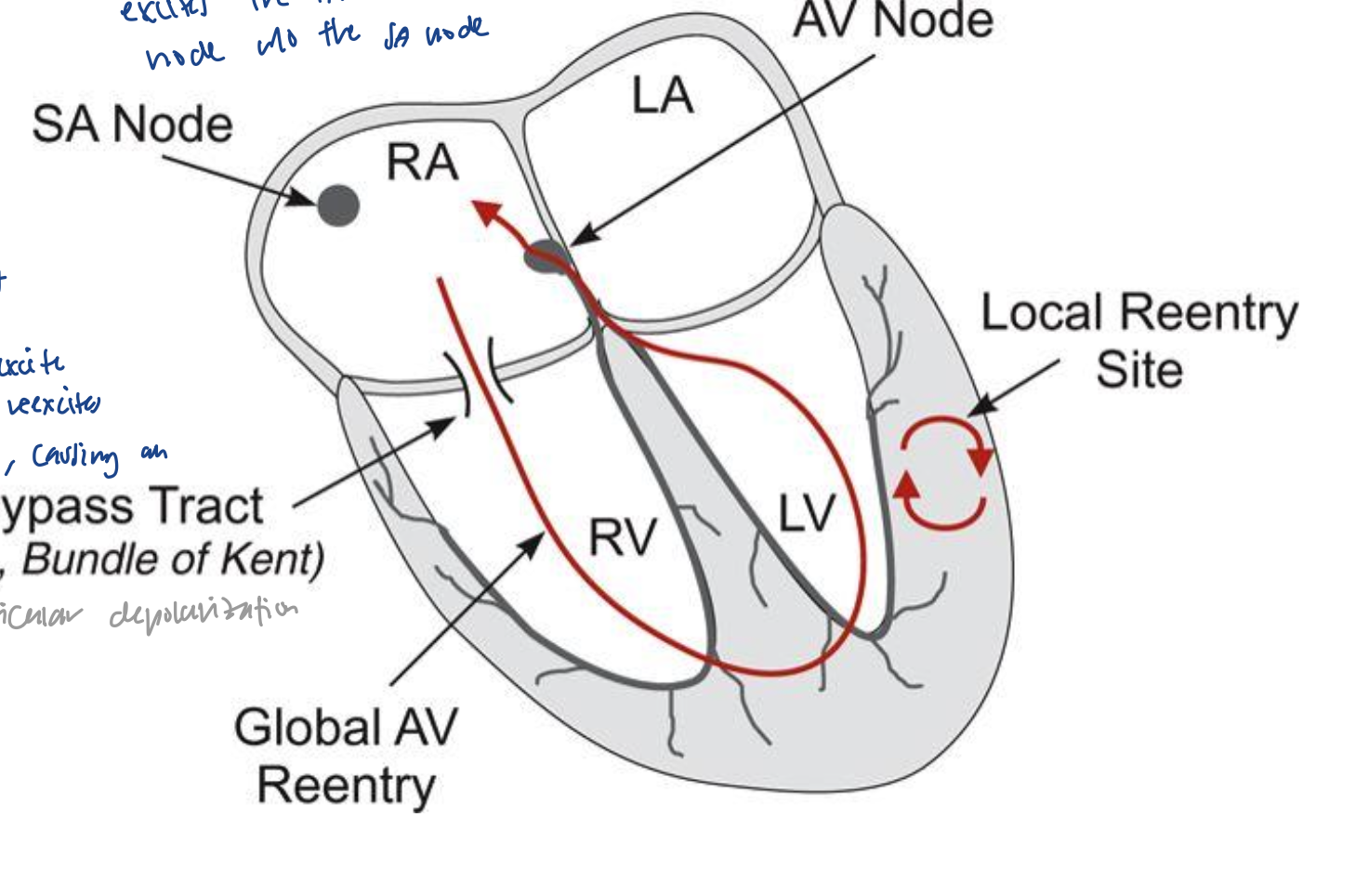
What is a global reentry loop?
AV node is excited without the SA node
action potential goes to ventricles without the purkinje fibers, and goes via the bypass tract (bundle of kent). then, goes back up to reexcite the AV node
The Electrocardiogram
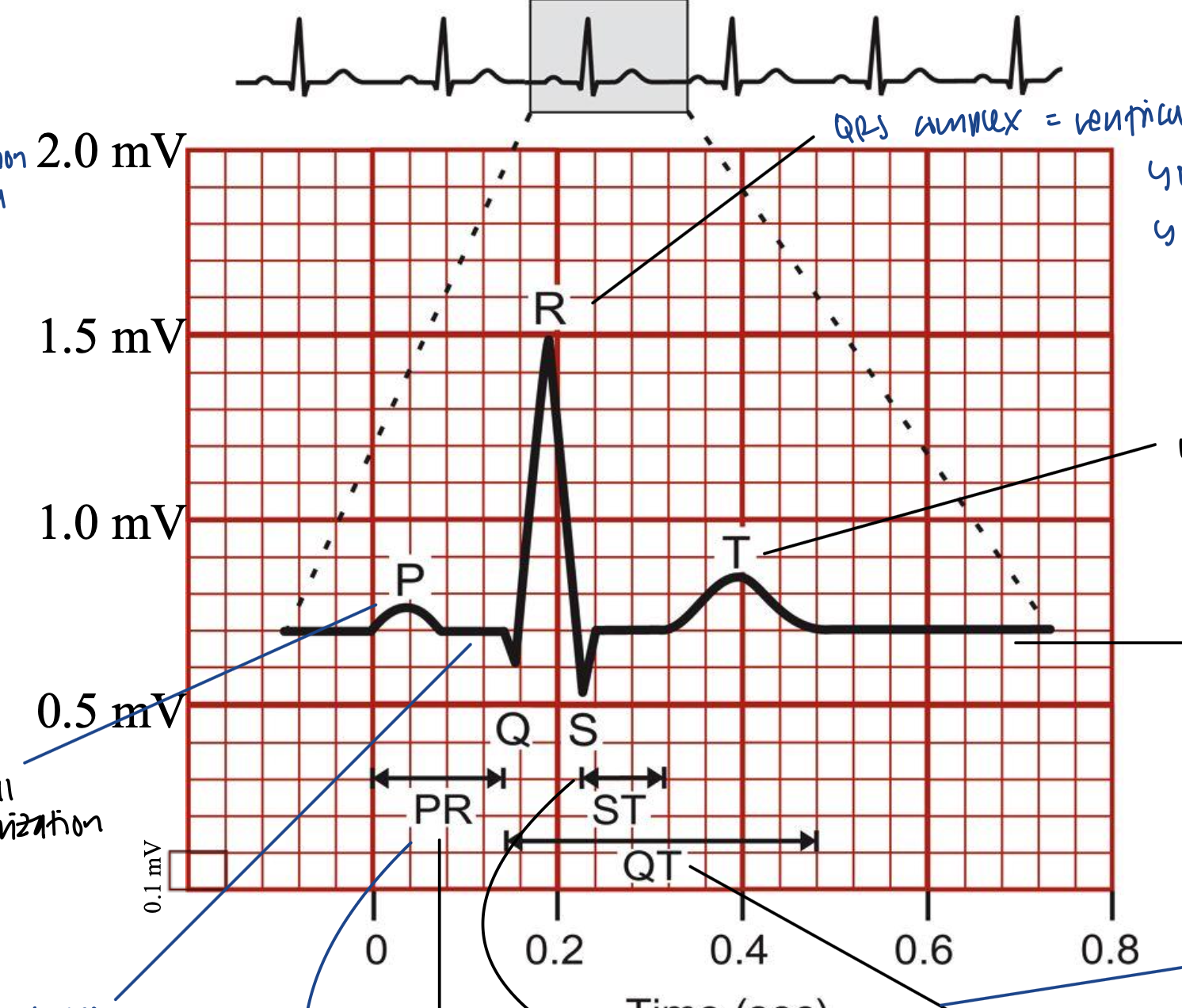
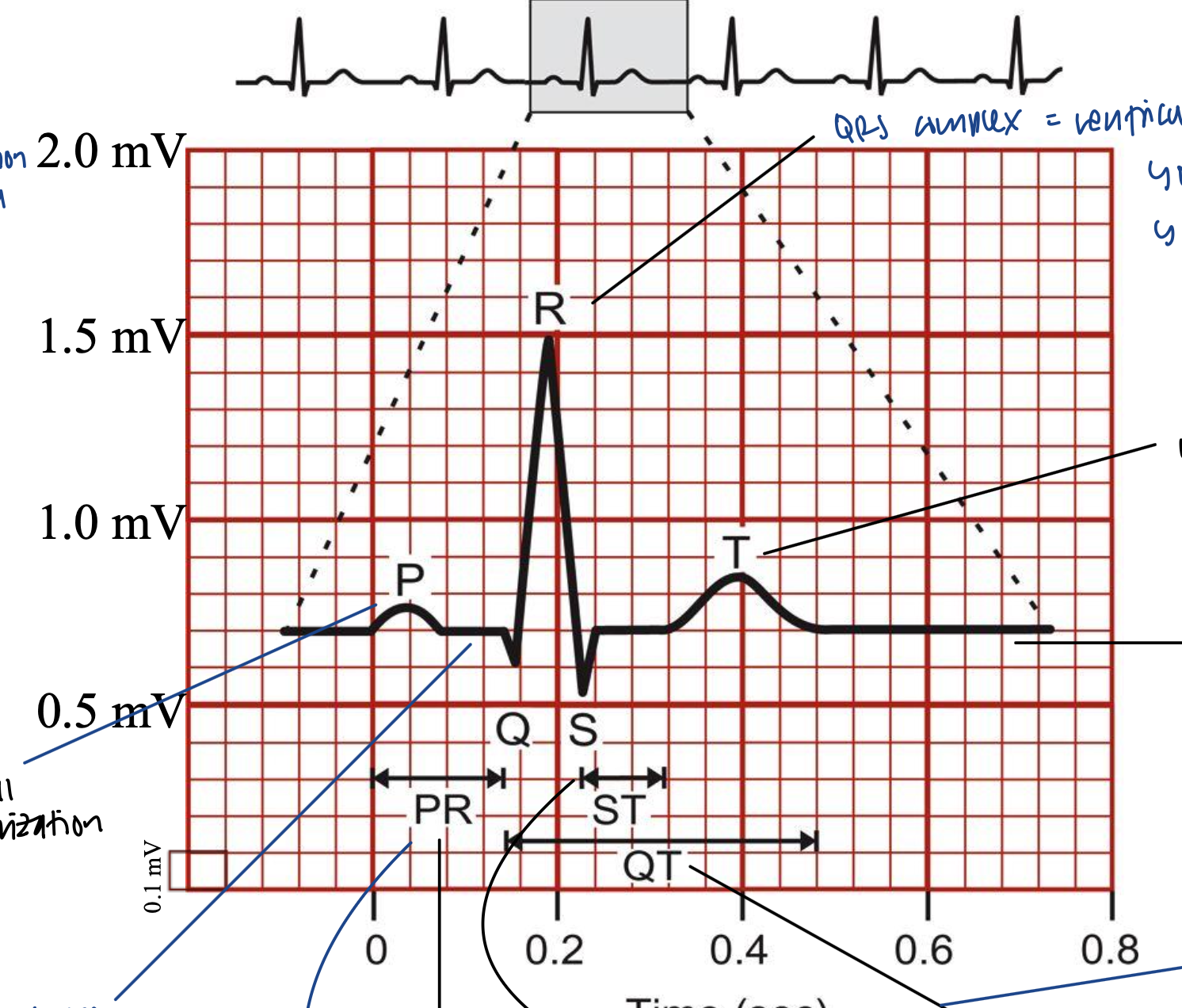
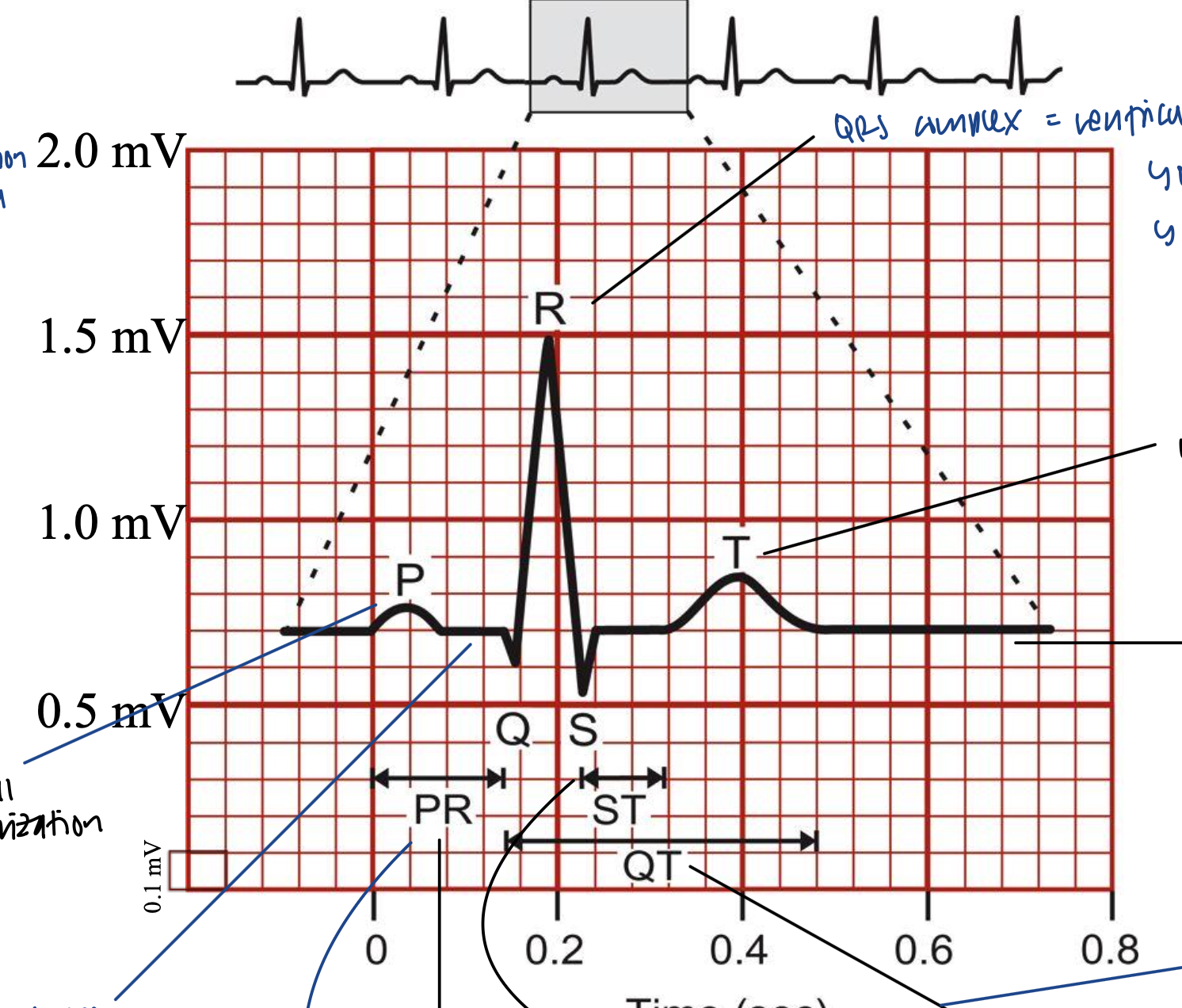
What is the P wave?
atrial depolarization
The Electrocardiogram
Can we see the repolarization of the P wave on an ECG tracing?
we cannot see the repolarization of the P wave on tracing because it is masked by ventricular depolarization
The Electrocardiogram
What is the QRS complex?
ventricular depolarization
happens very fast
The Electrocardiogram
What is the T wave?
ventricular repolarization
lasts longer than QRS depolarization
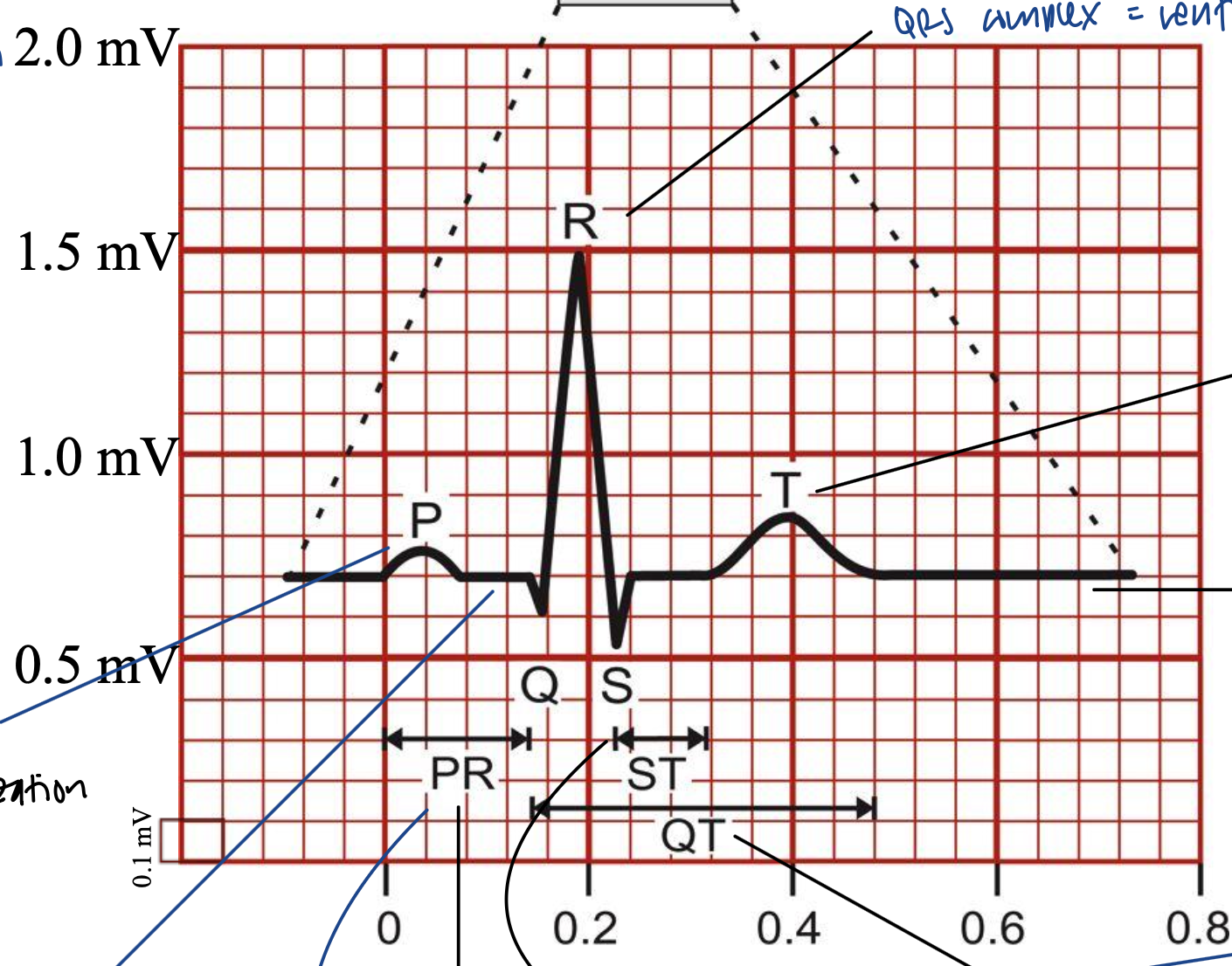
The Electrocardiogram
What is the PR segment?
isoelectric (zero voltage) for a bit between atrial and ventricular depolarization
time for action potential to travel to AV node
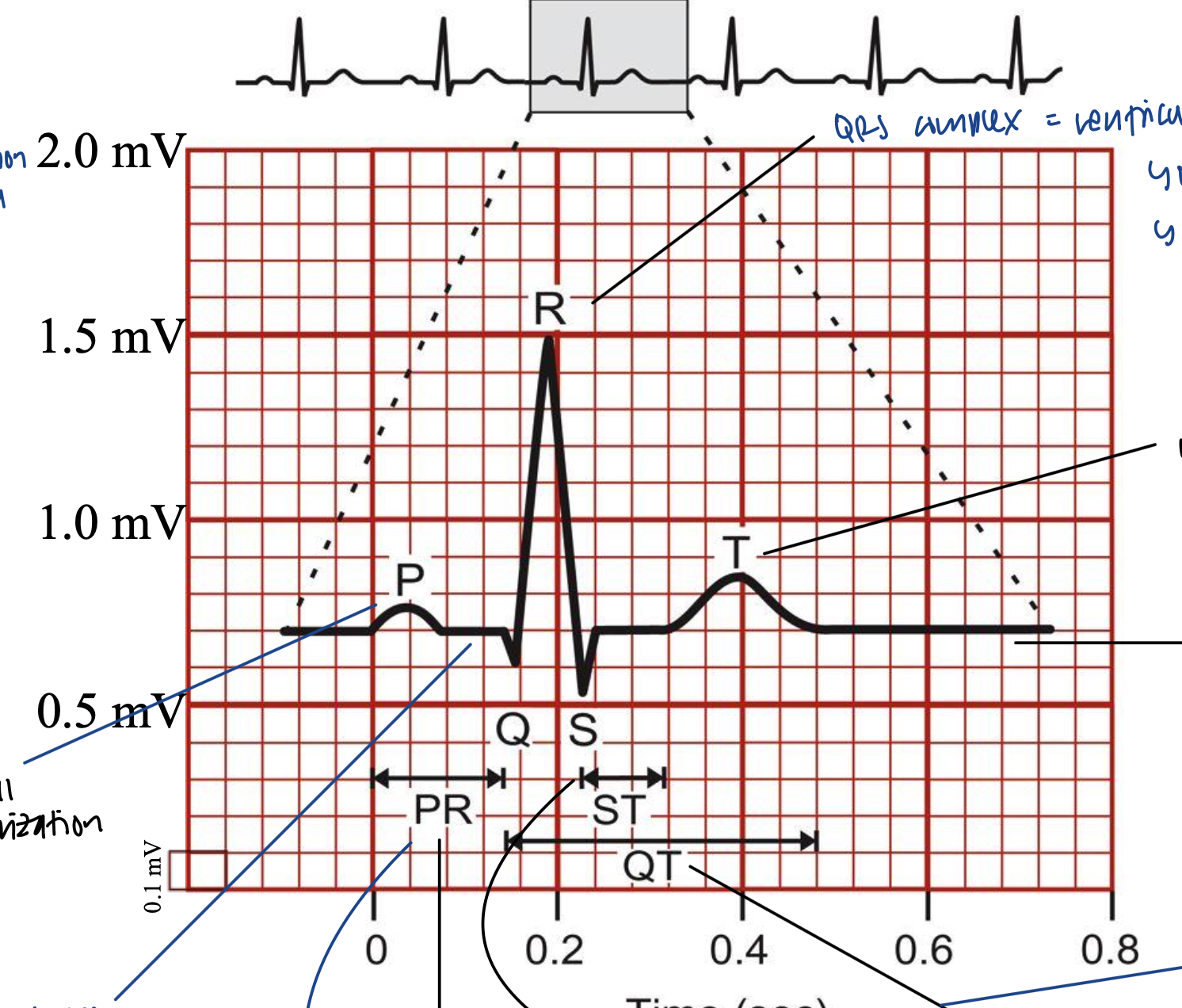
The Electrocardiogram
What is the ST segment?
squeezing/active ejection from ventricle
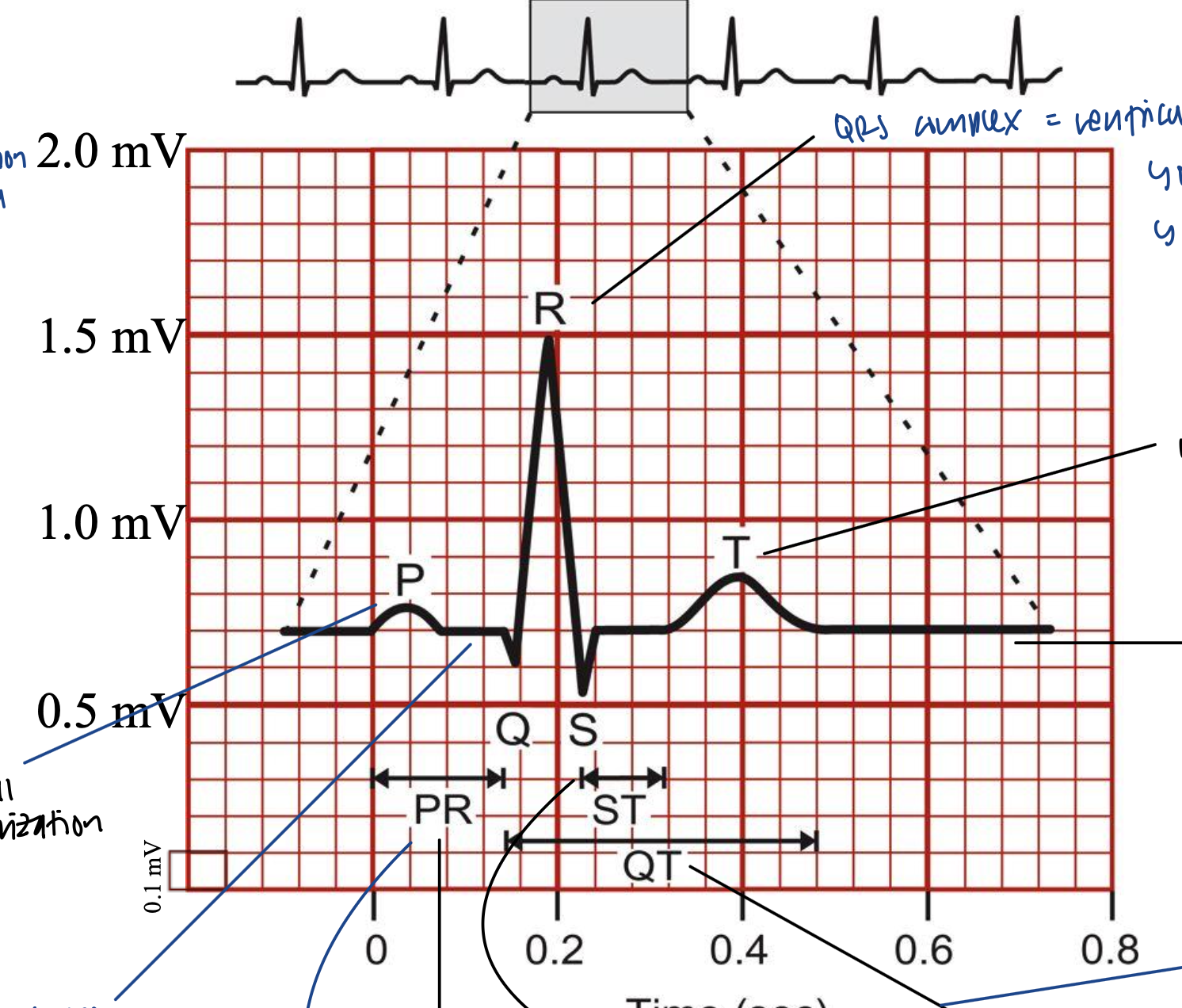
The Electrocardiogram
What is the QT segment?
entire duration for ventricle to eject, contract, and relax
ventricular depolarization and repolarization
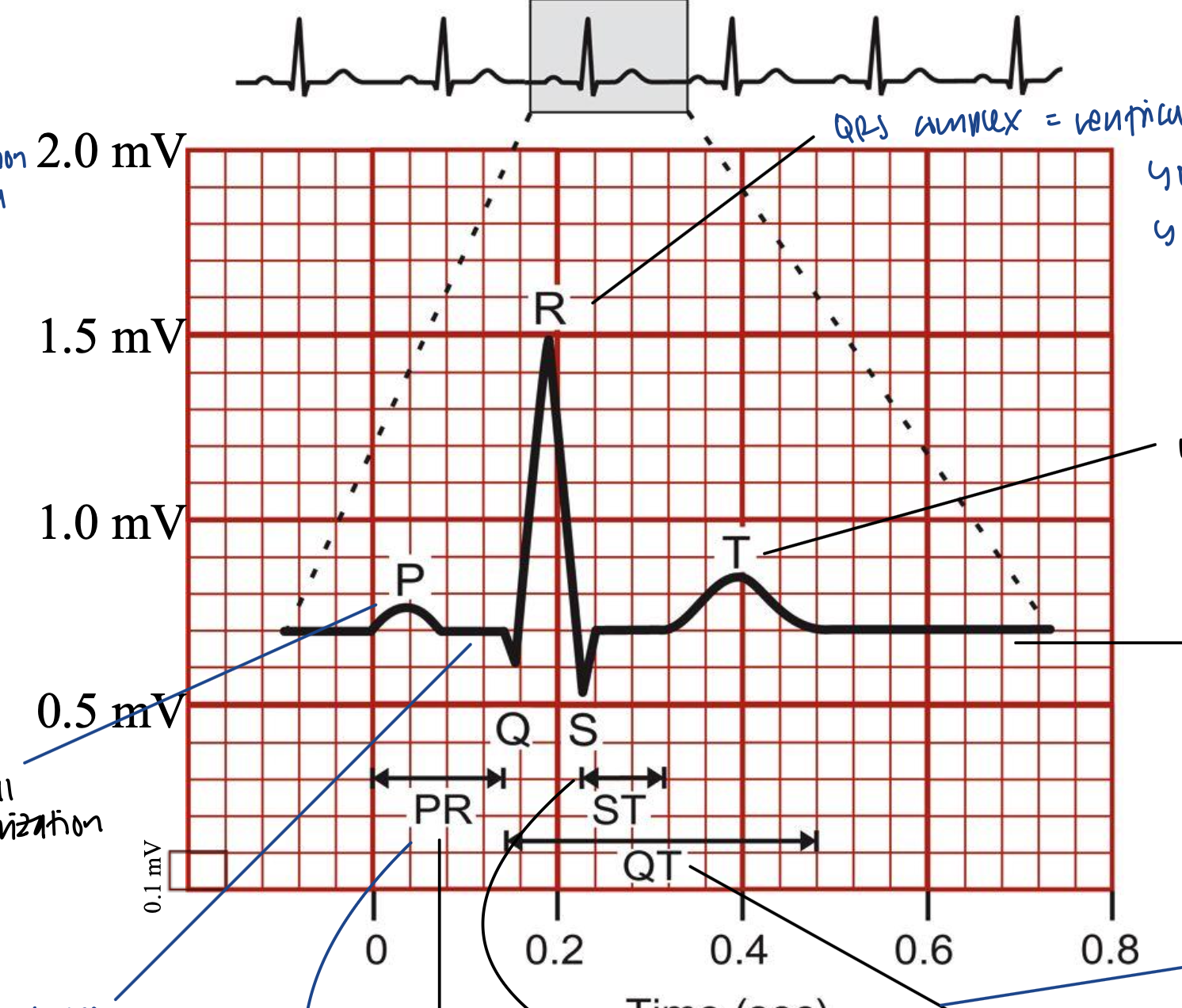
The Electrocardiogram
Elevation/depression of what is important?
elevation/depression of ST segment is important
The Electrocardiogram
What are the normal duration of a P wave, QRS complex, T wave, PR interval, ST segment, and QT interval?
P wave = 0.08-0.10 s
QRS complex: 0.06-0.10 s
T wave: cannot be measured
PR interval: delay 0.12-0.20
ST segment: cannot be measured
QT interval: 0.20-0.40 (but can be changed based on action potential duration)
ECG Interpretation
When is the heart in sinus rhythm?
when P waves (atrial depolarizations) lead directly to QRS (ventricular depolarizations) in a 1 to 1 fashion
basically ventricular depolarization is triggered by atrial
ECG Interpretation
What is sinus tachycardia and sinus bradycardia?
sinus tachycardia is 100+ bpm
sinus bradycardia is < 60 bpm
ECG Interpretation
What is normal stuff coming from QRS complex?
amplitude greater than 0.5 mV in at least one standard lead
upper limit of normal amplitude is 2.5 to 3.0 mV
small septal Q waves amplitude less than 1/3 of the amplitude of the R wave
ECG Interpretation
What is normal stuff coming from ST segment?
isoelectric, slanting upwards to the T wave
can be slightly elevated (up to 2 mm)
never normally depressed greater than 0.5mm in any lead
ECG Interpretation
What is normal stuff coming from T wave?
normally rounded and asymmetrical with a more gradual ascent than descent
isolated T wave inversion is generally normal in adults
ECG Interpretation
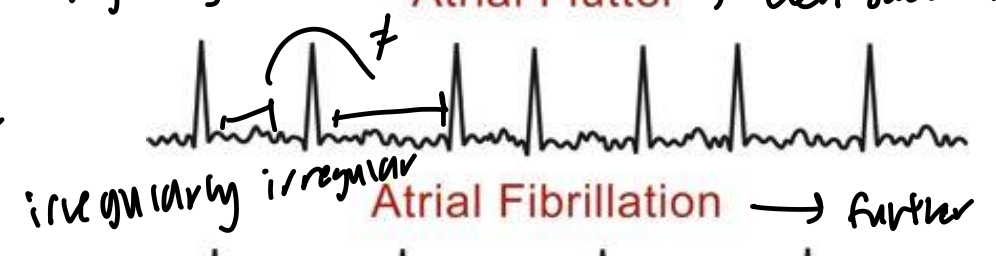
Atrial flutter?
even saw-teeth
different clusters of atrial depolarized but independent of the SA node
“irregularly regular”
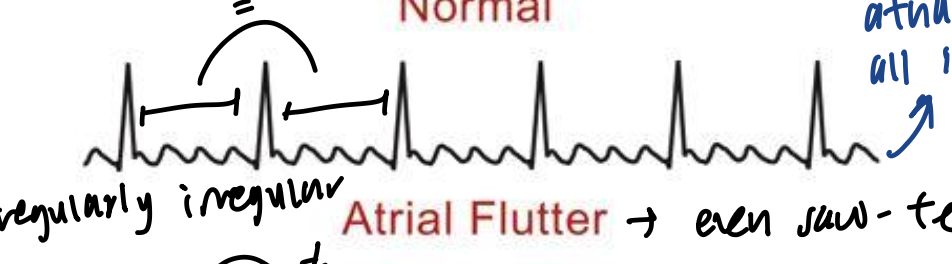
ECG Interpretation
Atrial fibrillation?
further deinvolvement of atrial depolarized state
individual cells are depolarizing together
“irregularly irregular”
ECG Interpretation
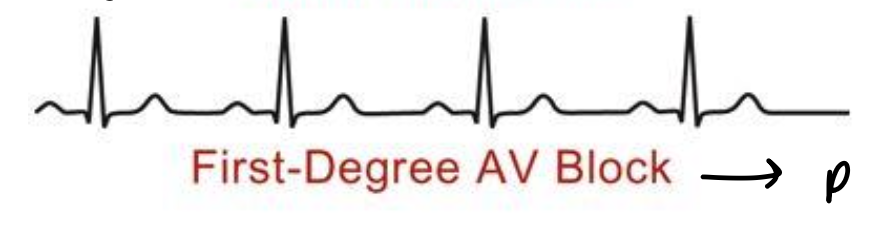
First-degree AV block?
P coupled to QRS but AV nodal delay, making intervals longer
ECG Interpretation
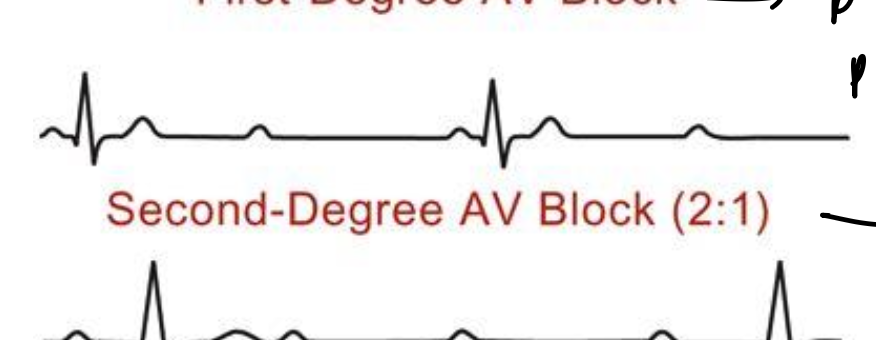
Second-degree AV block (2:1)?
every two P wave is a QRS wave
half of the action potentials are blocked by the AV node
ECG Interpretation
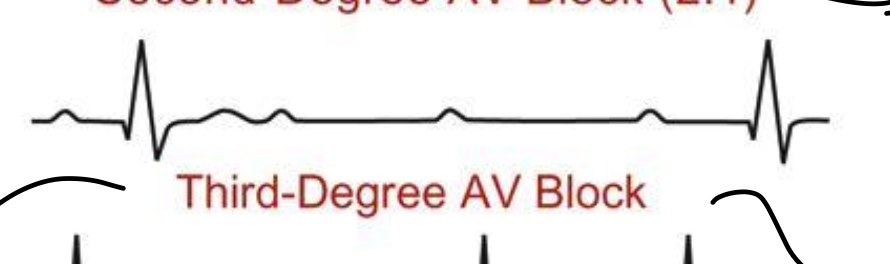
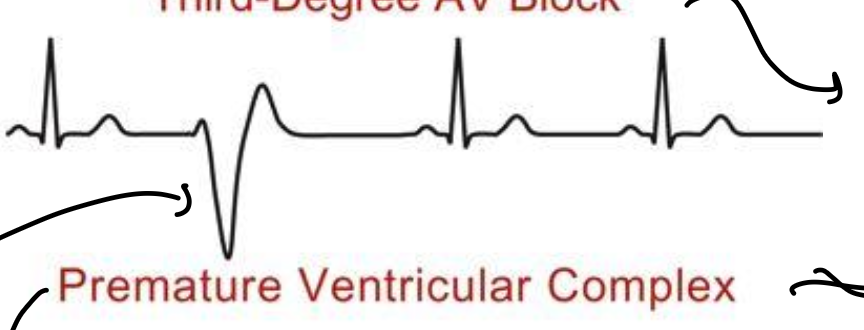
Third-degree AV block?
complete AV nodal is blocked
cannot predict when P wave would become a QRS
ECG Interpretation
Premature Ventricular Complex?
has global reentry loop
normal until a lot happens
ECG Interpretation
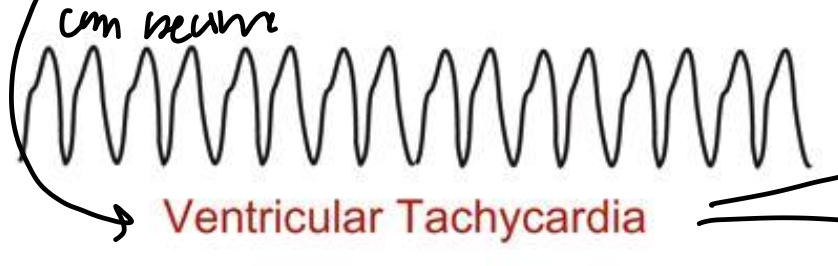
Ventricular Tachycardia?
ventricular coupling is not driven from atrial coupling
no P/T waves are visible because ventricular rate is so high
ECG Interpretation
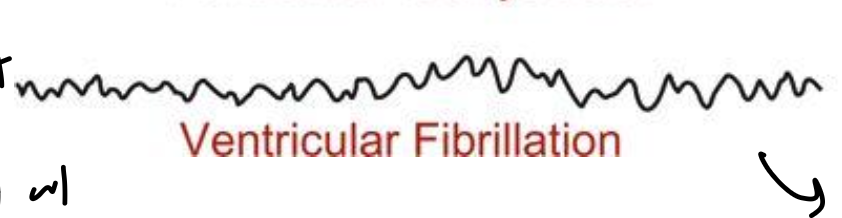
Ventricular fibrillation?
filling so low that cannot supply to body
no contractions as ejection from ventricle stopped
Volume Conductor Principles & Rules of Interpretation
What are 3 things that can influence ECG waveform?
location of electrodes on body’s surface
conduction pathways & conduction speed
changes in muscle mass
Electrical Vectors
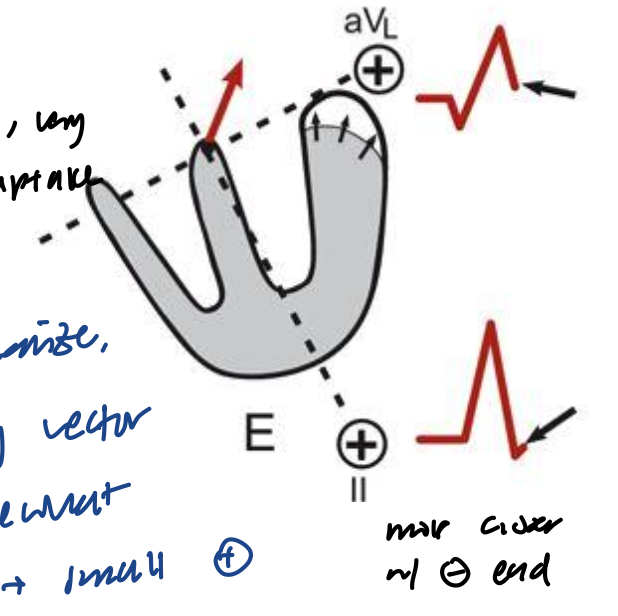
What happens when the SA node fires? What does each individual wave represent? What is the sum of all of these?
a wave of depolarization spreads in several directions throughout the atria
each individual wave represents an individual electrical vector
by summing each of these individual vectors, you get a mean electrical vector
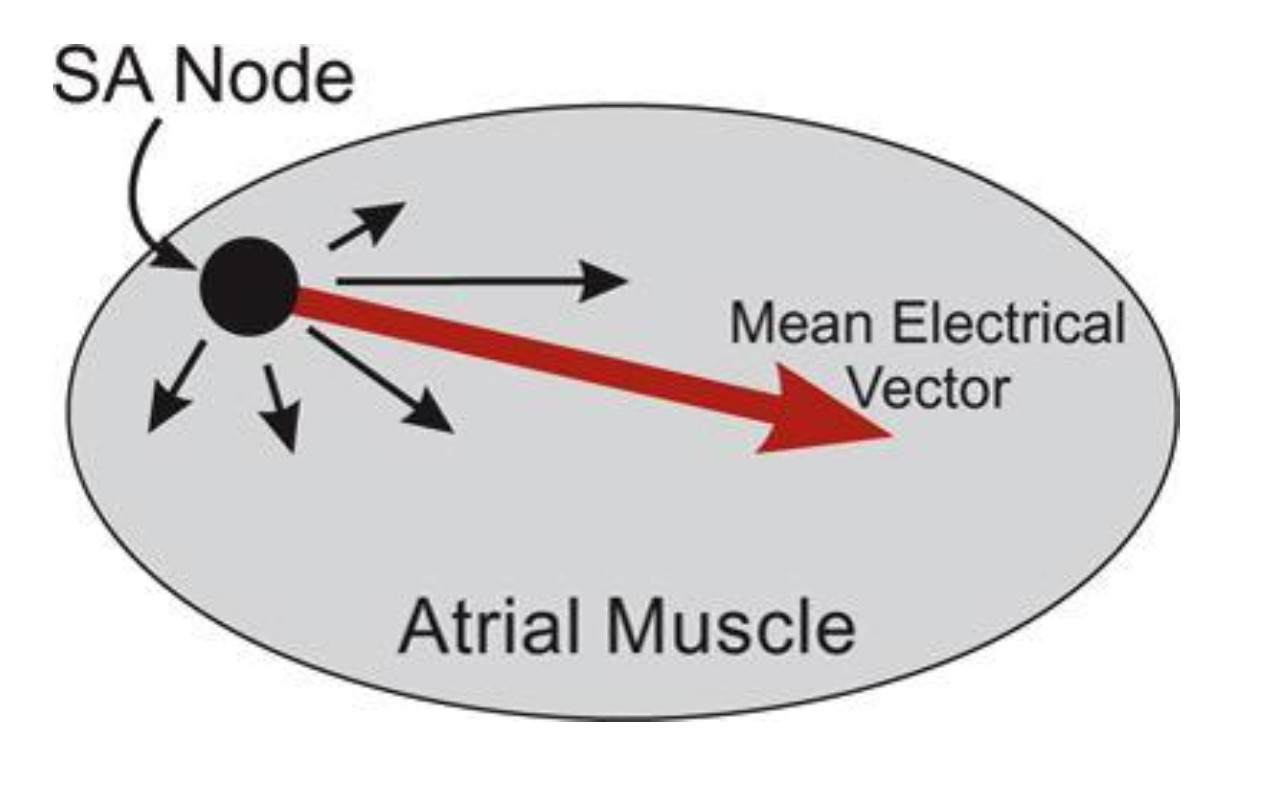
Electrical Vectors
Direction of the mean electrical vector relative to the positive and negative electrodes determines what?
polarity of waveform
magnitude of waveform
Electrical Vectors
Summing mean vectors from several different ECG leads determines what?
determines the mean electrical axis of the heart
used to diagnosically identify left and right deviations
The Electrocardiogram
What are the 5 rules of interpreting an ECG?
wave of depolarization traveling towards a + electrode results in a + deflection
wave of repolarization traveling towards a + electrode results in a - deflection
a wave of depolarization/repolarization perpendicular to an electrode axis produces no net deflection
amplitude of the measured potentials depends on the orientation of the + electrode relative to the mean vector
voltage amplitude ± is related to the mass of tissue undergoing depolarization/repolarization
The Electrocardiogram
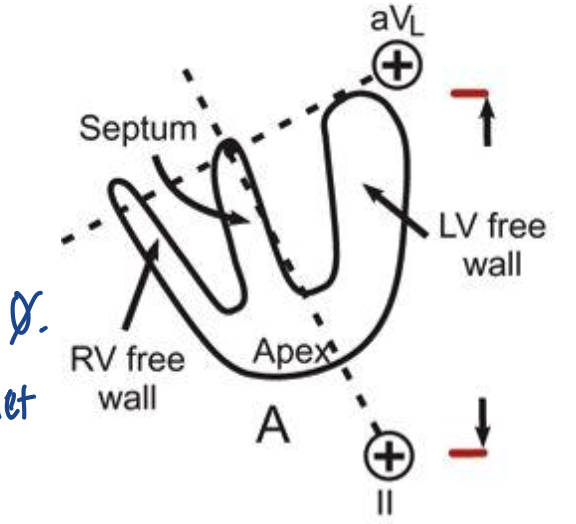
What is happening here?
no electrical vectors, so the reading is 0
heart is quiet here
The Electrocardiogram
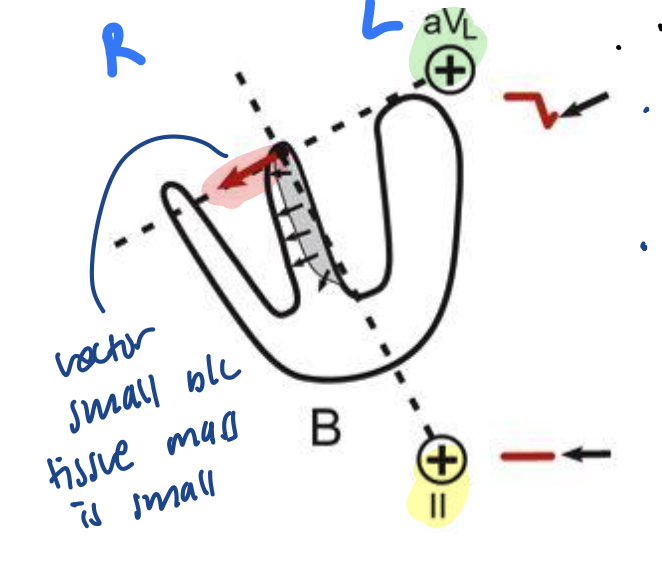
What is happening here?
initial electrical transduction
first region to depolarize is the interventricular septum
avL will have a negative voltage because the vector is moving away from the + of avL (Q wave of QRS)
Lead II has no change in voltage because the vector is perpendicular to lead II axis
The Electrocardiogram
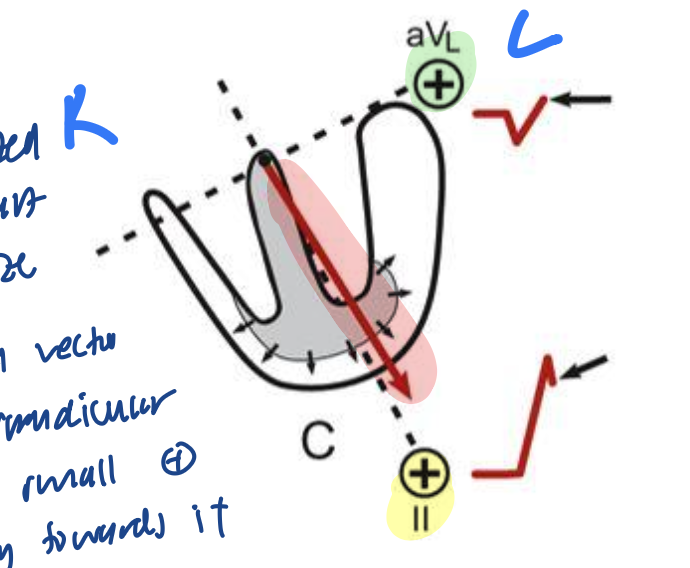
What is happening here?
septum is completely depolarized and apex of heart starts to depolarize
avL has a small + voltage because the vector is close to being perpendicular to the avL axis but leaning a bit towards avL’s +
lead II is very positive and has a tall deflection because the vector is almost completely pointing towards lead II’s + (R wave of QRS)
The Electrocardiogram
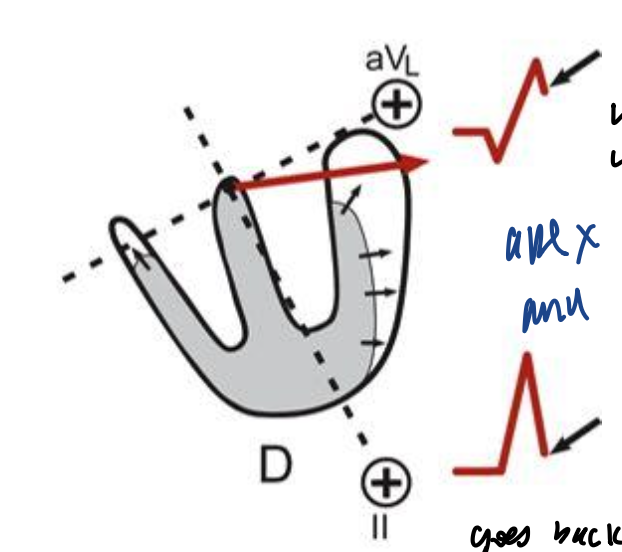
What is happening here?
apex and right ventricle completely depolarized and left ventricle is starting to depolarize
avL has a + voltage because the vector is close to avL’s +
lead II has a slightly + charge because vector is almost perpendicular to lead II’s axis but slightly leaning towards lead II’s +
The Electrocardiogram
What is happening here?
last regions of left ventricle depolarized
avL small + voltage because vector is almost perpendicular to avL’s axis and slightly leaning towards avL’s + charge
lead II is negative because the vector is pointing away from lead II (S wave of QRS)
The Electrocardiogram
What is happening here?
ventricles are completely depolarized
voltage reading is back to 0
The Electrocardiogram
What is the placement of recording electrodes called?
limb leads: Einthoven’s triangle
Einthoven’s triangle
What are the limb leads and their charges?
RA (right arm): lead II - and lead I -
LA (left arm): lead I + and lead III -
LL (left leg): lead II + and lead III +
RL (right leg): reference electrode for recording purposes
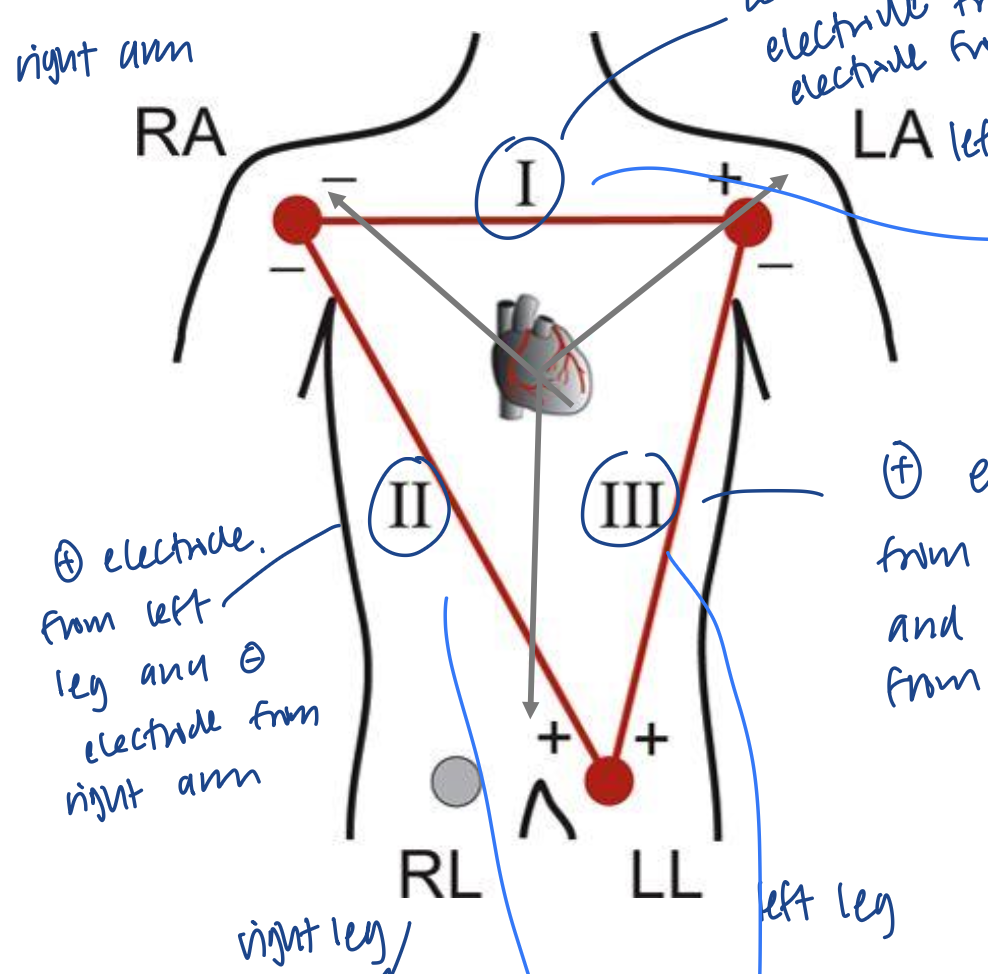
Einthoven’s triangle
What are the leads?
Lead I: between RA’s - and LA’s +
Lead II: between RA’s - and LL’s +
Lead III: between LA’s - and LL’s +
Axial Reference System
What is the axial reference system?
three limbs of Einthoven’s triangle broken apart, collapsed, and superimposed over the heart
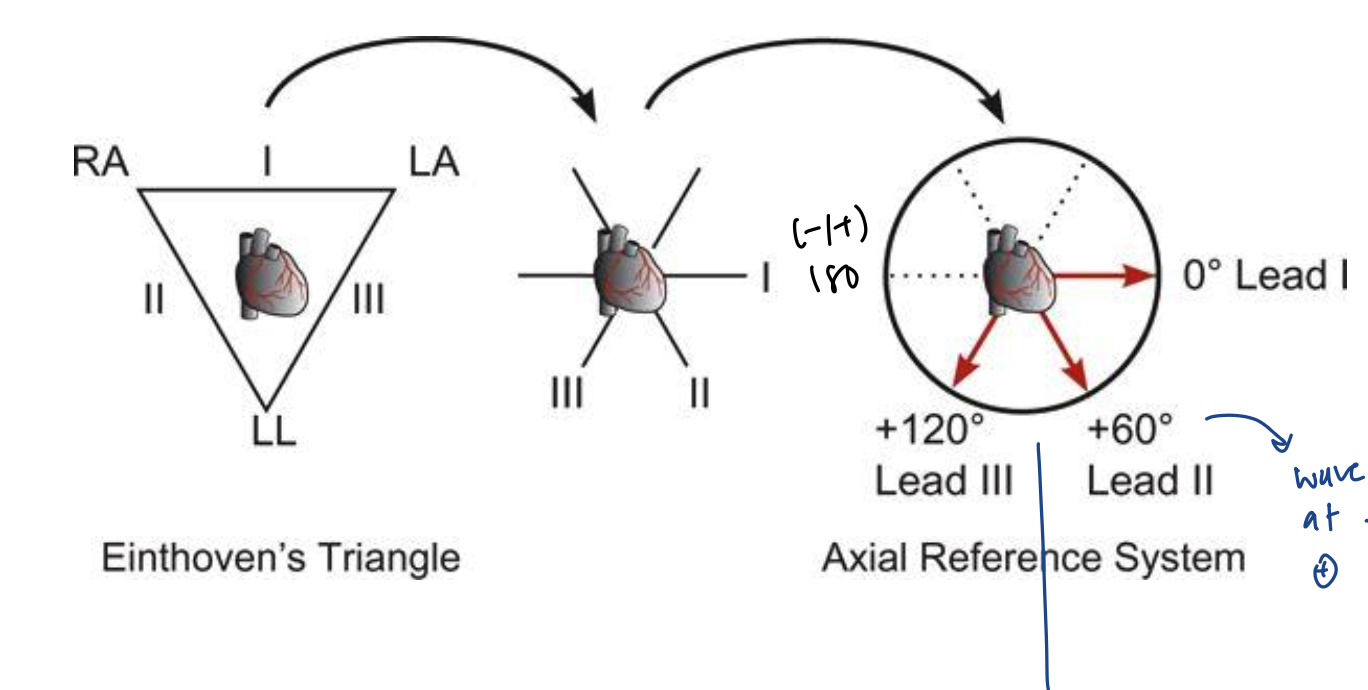
Axial Reference System
What else is added to the axial reference system?
3 leads in addition to the 3 bipolar limb leads
aVL - left arm
aVR - right arm
aVF - foot
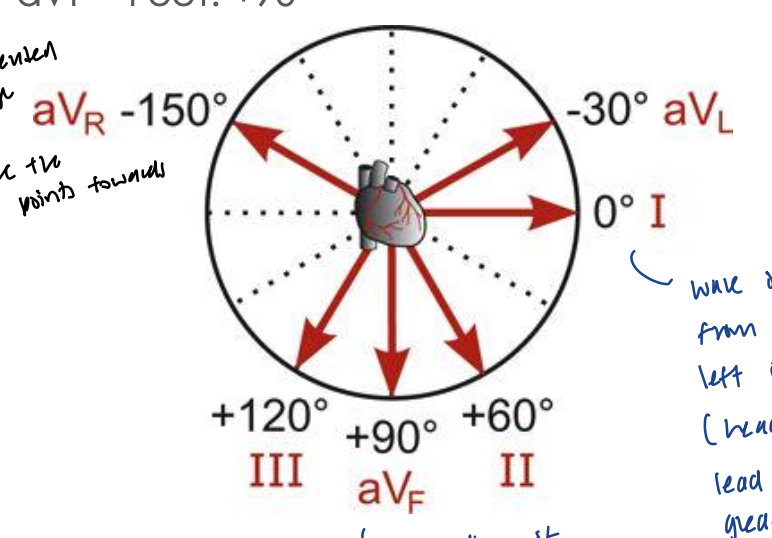
Axial Reference System
How do you determine the mean electrical axis?
can use the 6 leads to estimate mean electrical axis with the axial reference system
mean electrical axis corresponds to the axis that is perpendicular to the lead axis with the smallest net QRS amplitude
aka perependicular to the most biphasic lead
can estimate exact axis and if there is an axis deviation
will not be able to determine exact axis with this method
Axial Reference System
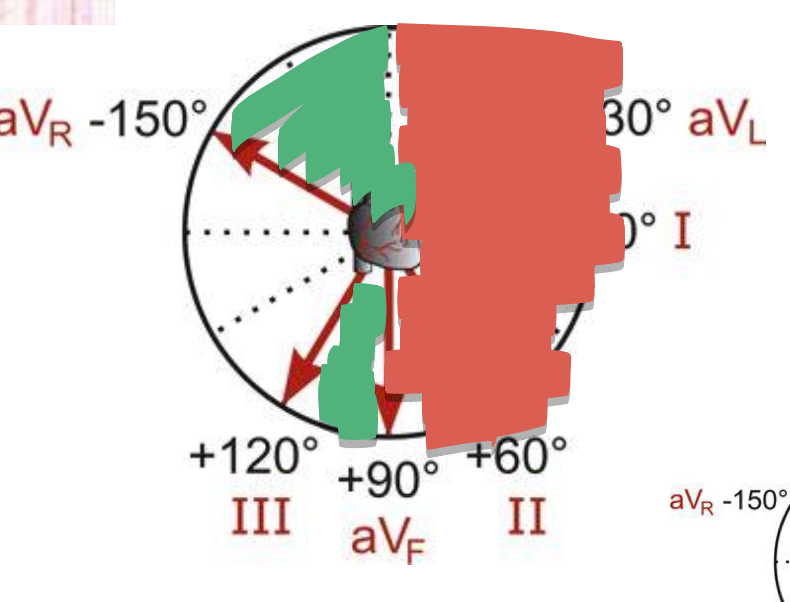
Draw a circle and label the ranges of the axis deviations
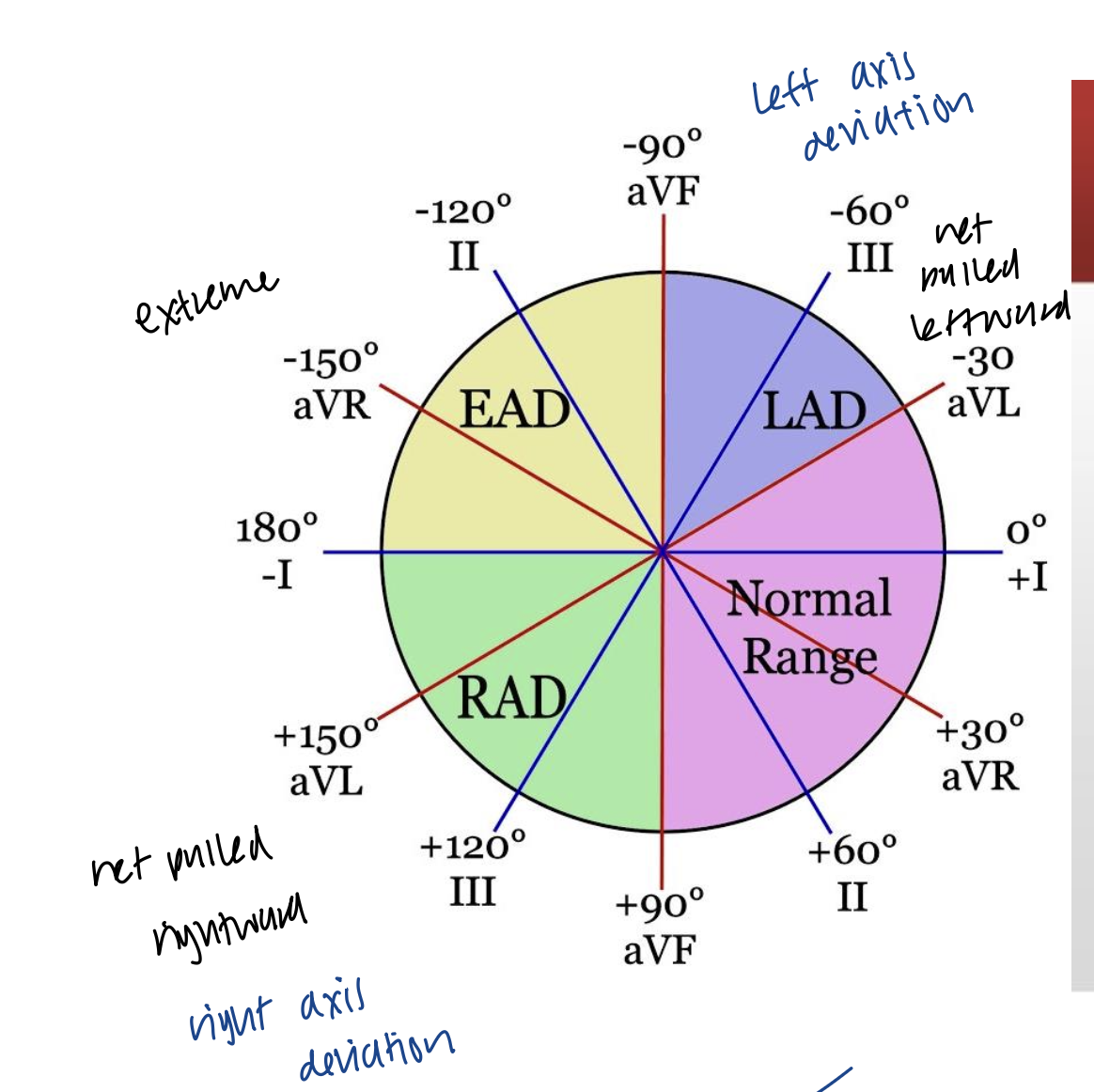
Axial Reference System
Why can axis deviations occur?
can occur because of the physical position of the heart within the chest
or changes in sequence of ventricular activation, or ventricular regions are incapable of being activated due to deflected tissue
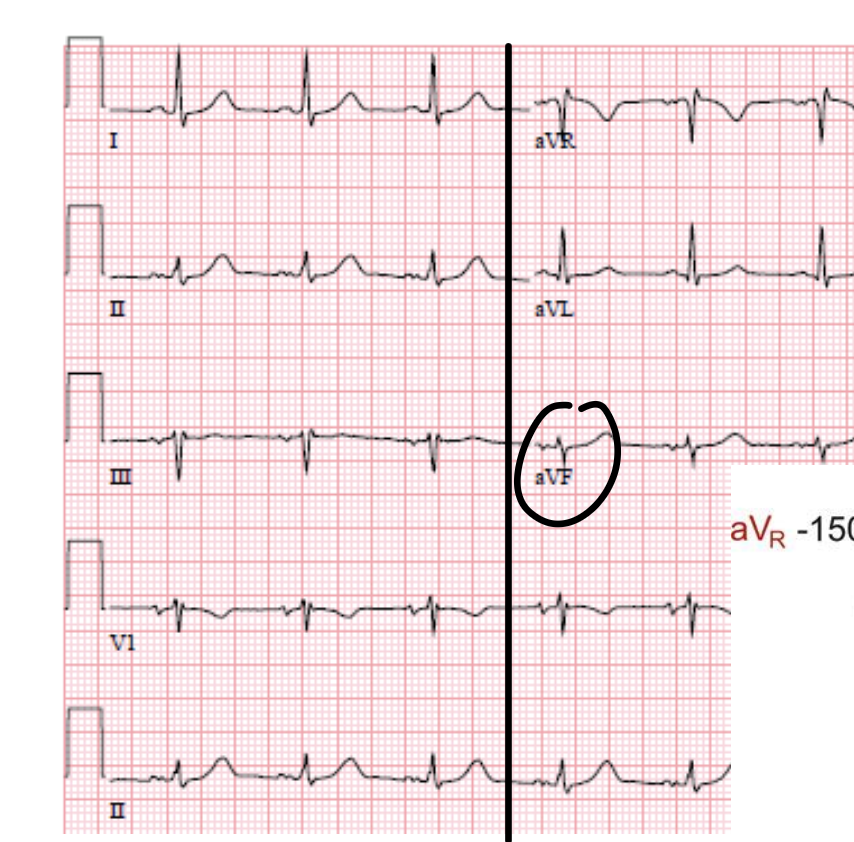
Axial Reference System
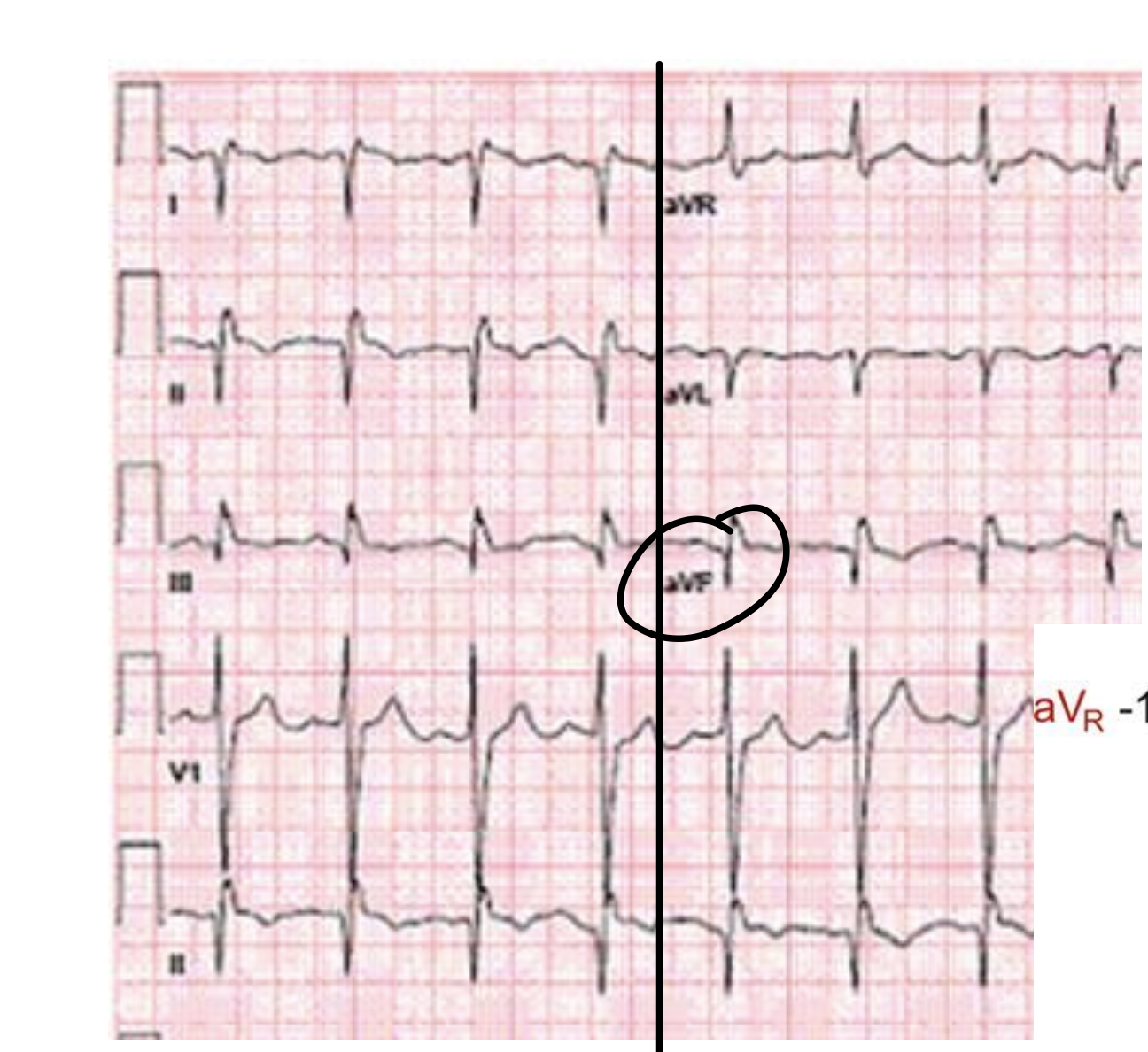
With the axial reference system, walk me through which axial deviation this person might have
find the most biphasic tracing → aVF
what is perpendicular to aVF? → lead I
is lead I’s tracing + and -? → +
is lead II’s tracing more + or -? → +
what is perpendicular to lead II? → aVL
is aVL’s tracing more + or - ? → more +
is the mean electrical axis closer to lead II or avL? → probably closer to avL because it has taller positive deflections
is there an axis devation? → could be LAD (left axis deviation)
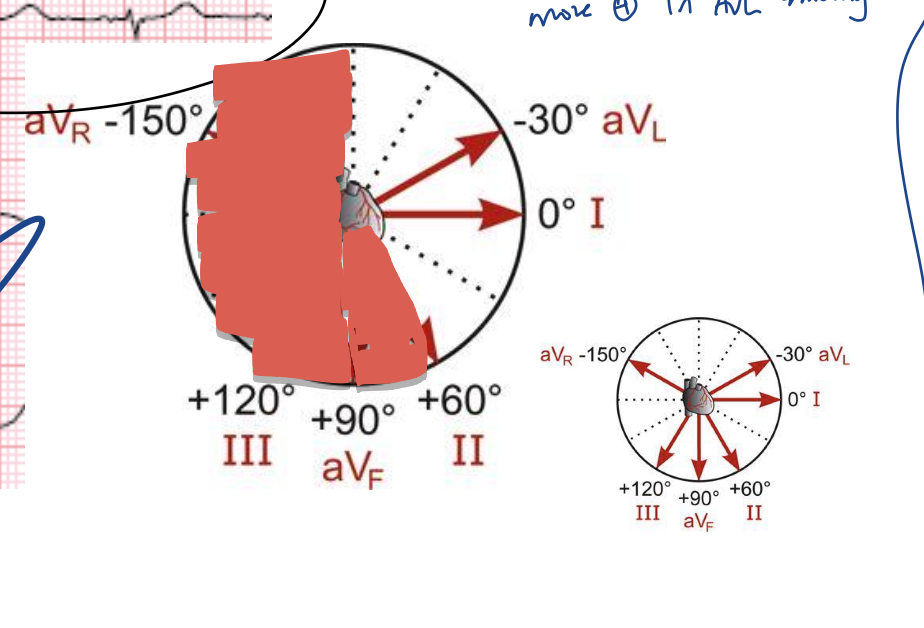
Axial Reference System
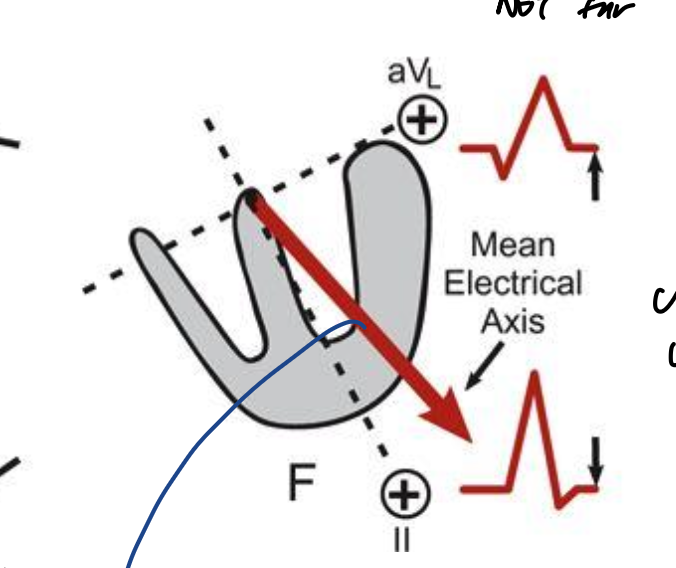
With the axial reference system, walk me through which axial deviation this person might have
biphasic: aVF
what is perpendicular to aVF? → Lead I
is lead I’s tracing + or - ? → -
is lead III’s tracing + or - ? → +
what is perpendicular to lead III? →aVR
is aVR’s tracing + or - ? → more +
is it closer to lead III or aVR? → closer to aVR since the + deflections are higher
any possible axial deviations? → could be EAD