Cardiovascular Regulatory Mechanisms (Exam 4)
1/54
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
55 Terms
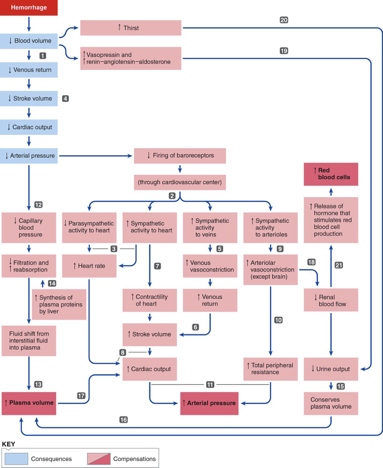
Describe the anatomy of the arteries
Made of thick wall of smooth muscle and connective tissue and behaves like a baloon
Capillaries
-smallest of vessels
-arterioles branch within the organs into capillaries across which all exchanges are made with surrounding cells
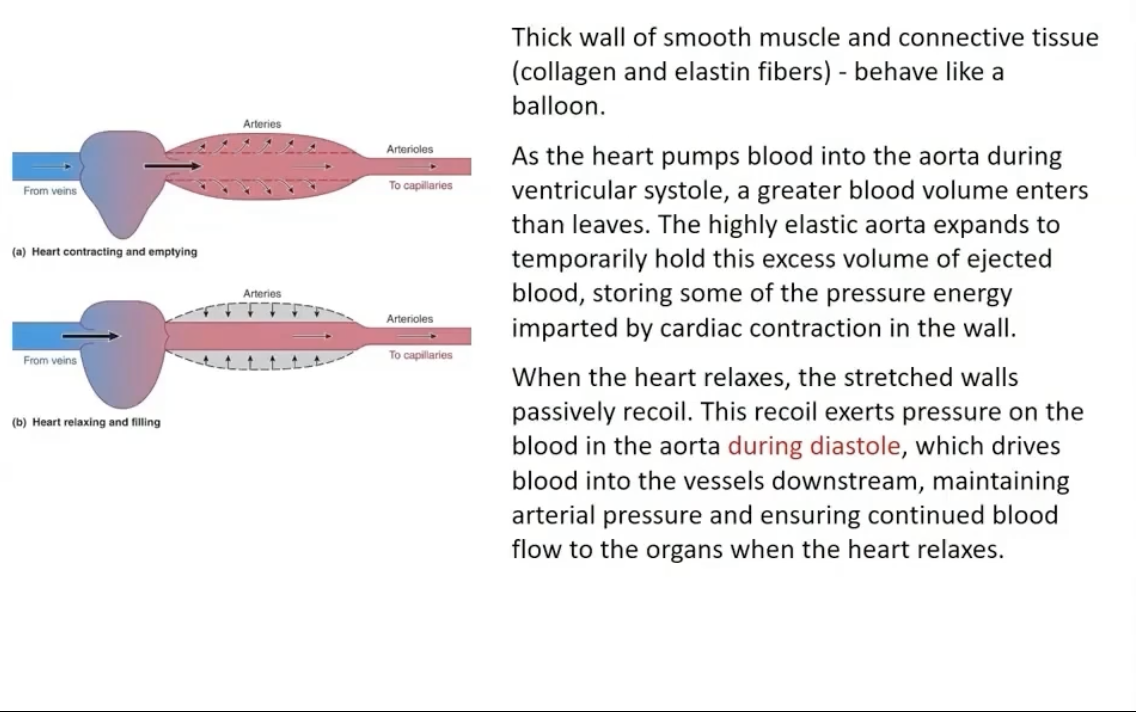
Aorta/Arteries Roles
-Rapid-transit passageways for blood from the heart to the organs
-Act as a pressure reservoir to drive blood when the heart relaxes (Diastole)
How do arteries maintain arterial pressure during diastole?
the elastic recoil exerts pressur eon the blood in the aorta during diastole, which drives blood into the vessels downstream
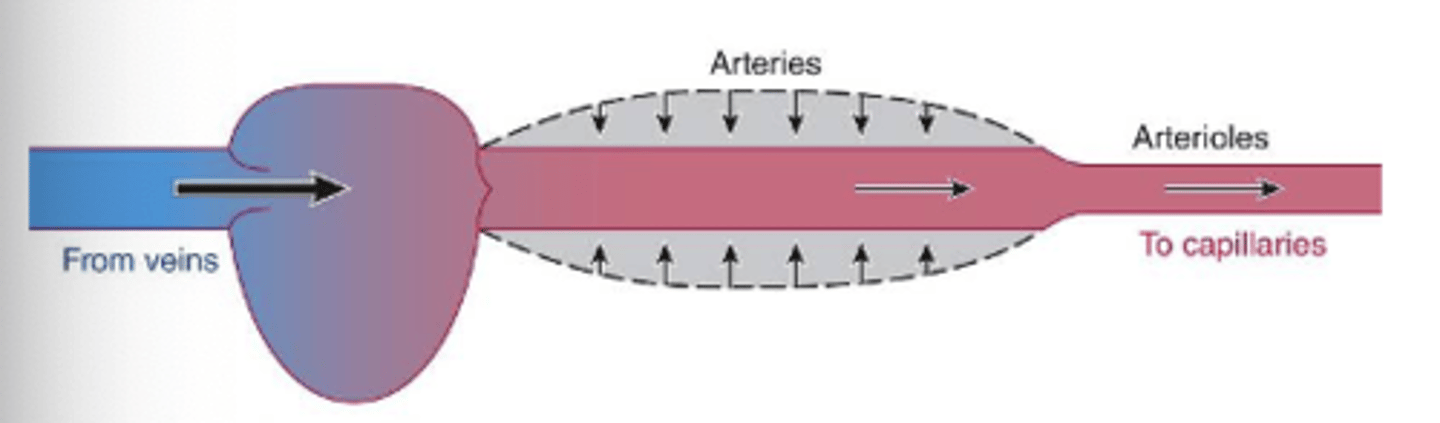
how can blood flow and arterial pressure be maintained when the heart relaxes?
the elastic recoil of arteries contributes to the pressure and flow, even when the heart is at rest
why does arterial pressure not fall to 0 mmHg during diastole when ventricular pressure does?
elastic recoil of arteries and the next cardiac contraction refills the arteries before all the blood drains off
Why do arterioles provide the majority of resistance to the vascular tree?
COLLECTIVELY the capillaries do not offer as much resistance to flow as arterioles (due to branching/increased surface area)
what is the pressure fall from blood entering arterioles to entering the capillaries
93 mmHg to 38 mmHg
What 2 things does controlling the radius of the arterioles help to do?
Variably distribute cardiac output among target organs
Helps regulate arterial BP
the thick layer of smooth muscle in arteriolar walls
-innervated by sympathetic nerve fibers
-sensitive to many local chemical changes, few circulating hormones, and mechanial factors (stretch)
What innervates the smooth muscle of arterioles?
sympathetic nervous system
What is the smooth muscle in arterioles sensitive to?
chemical changes
hormones and stretch
What is vascular tone?
A state of partial constriction
arterioles are always somewhat contracted
Factors Responsible for Vascular Tone
the smooth muscle in arterioles is tonic and will always have enough ca channels open to maintain a partial contraction → myogenic self-induced contractile activity
Sympathetic fibers are constantly releasing norepinephrine (enhances vascular tone)
Factors that increase arteriolar tone
-Increase in O2
-Decrease in CO2
-Increase in sympathetics stimulation
-Increase in Myogenic Activity
-Increase in Endothelin
-Vasopressin; Cold
Factors that decrease arteriolar tone
-Decrease in myogenic activity
-Decrease in O2
-Increase in CO2
-Increase in Nitric Oxide
-Decrease in sympathetics stimulation
-Histamine release; Heat
How are materials exchanged across capillaries at target organs?
through Diffusion
How do capillaries maximize surface area and time available for exchange?
Thin walled (one cell layer thick)
Small diameter
Branch extensively
Numerous amounts of them
Blood flows the slowest in these
what 3 features of capillaries make them perfect for maximizing exchange between plasma and ECF?
large surface area
small radii
slow blood velocity
What is a metarteriole? Important feature of them?
a channel that runs between arterioles and venules
surrounded by smooth muscle
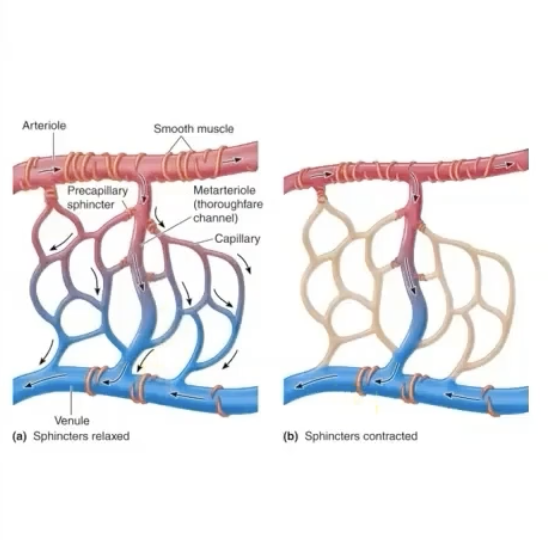
Describe Pre-capillary Sphincters
-Not innervated
-Have high degree of myogenic tone
Sensitive to local metabolic changes
Act as stopcocks to control blood flow through particular capillaries
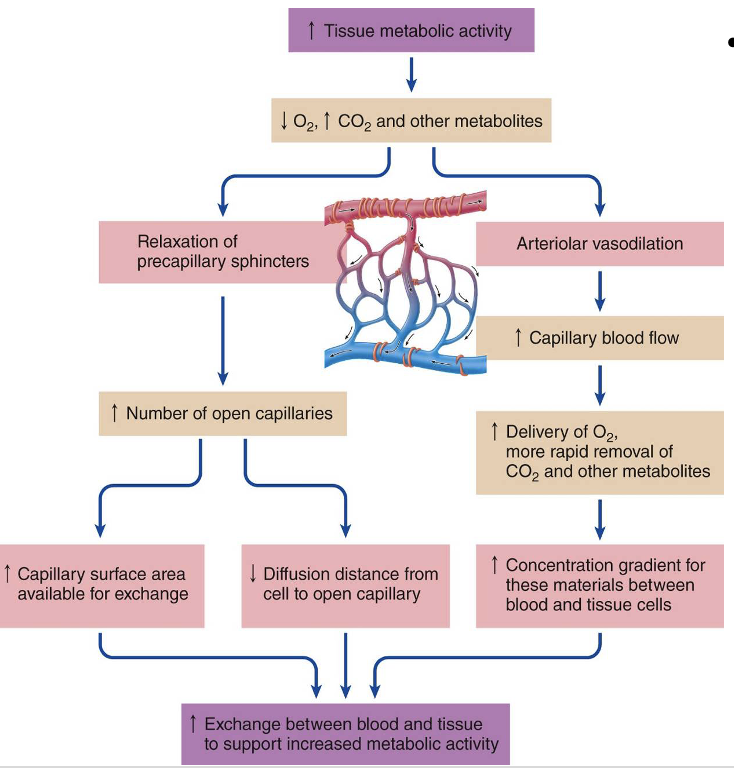
When a muscle becomes more active, what happens to the precapillary muscles supplying the capillaries?
A greater % of them relax in response to chemical changes
total volume and surface area increase.
Diffusion distance between cells and capillaries decreases
What happens concurrently with the relaxation of pre-capillary muscle to aid in increased blood flow to active organs?
arteriolar vasodilation
Blood flow through tissue is regulated by what 2 major factors?
Degree of resistance by arterioles in the organ
Number of open capillaries (controlled by pre capillary sphincters)
What acts as the go between for blood and tissue cells?
interstitial fluid
Is exchange across the capillary wall between plasma and Interstitial fluid passive or active? Why?
Largely passive diffusion
(only limited vesicular transport requires energy)
Because the capillaries are really permeable and exchange is rlly thorough → interstitial fluid is the same composition as incoming arterial blood
What two ways is exchange between blood and surrounding tissue accomplished?
passive diffusion (primary method)
bulk flow
What effects whether a capillary will be leaky or not?
how tightly endothelial cells are joined
whether fenestrations are present (varies between different organs)
What is bulk flow?
protein-free plasma filters out of the capillary, mixes with surrounding inter fluid, and is then reabsorbed
-Does NOT play an important role in exchange of solutes, but it is very important for distribution of ECF
Explain the process of ultrafiltration
a process in which the pressure inside the capillary exceeds the pressure in the ECF, and fluid is pushed out through the capillary pores
Why does bulk flow occur?
due to differences in the hydrostatic and colloid osmotic pressures between plasma and interstitial fluid
What pressures influence fluid movement into and out of the capillary?
out: capillary blood pressure and interstitial fluid colloid osmotic pressure
in: plasma-colloid osmotic pressure and interstitial fluid hydrostatic pressure
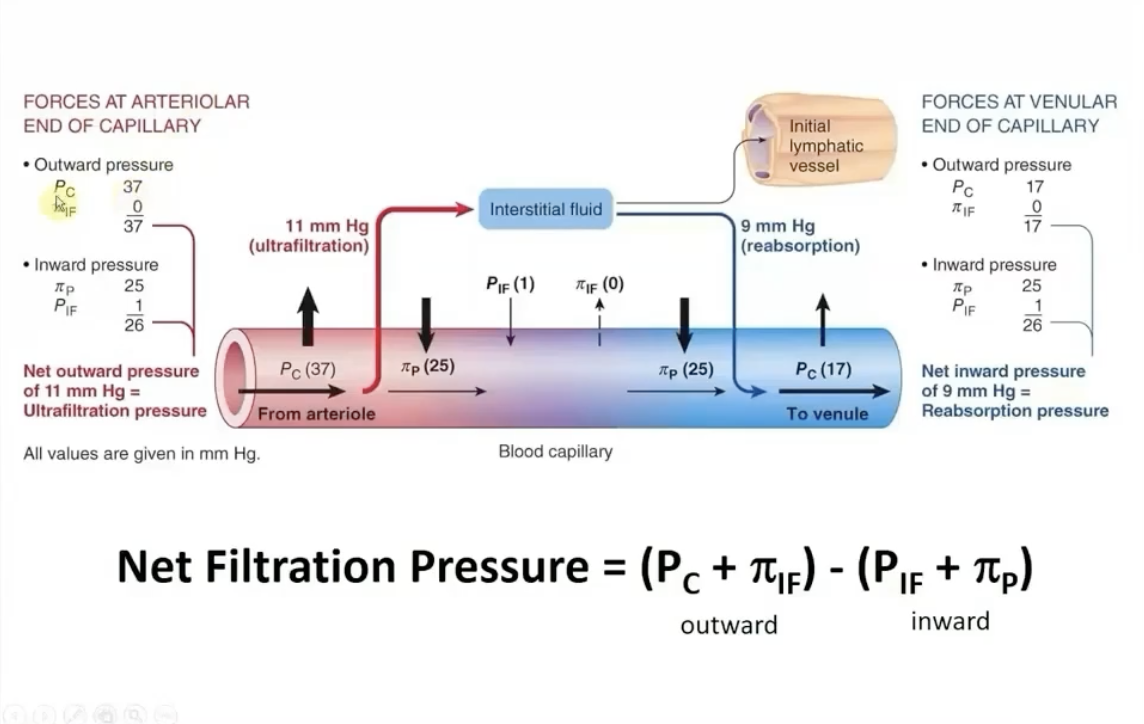
If plasma proteins pathologically leak into the interstitial fluid, how does that affect fluid movement involving the capillaries?
fluid is moved out of the capillaries and into the interstitial fluid
How does the extra fluid that is filtered out of the capillaries get reabsorbed? What does this system do?
By the Lymphatic system (one way vessel)
Provides an accessory route for this fluid to be returned to the blood
works like a sewer system that carries away excess rainwater so floods don’t occur
How does blood leaving the capillary beds get back to the heart?
Through the venous system
capillaries drain into venules which converge to form veins that exit the organ
What happens ot the total cross sectional area of the venous system as blood approaches the heart?
it decreases as smaller veins converge into lesser, larger cessels (blood flow speeds up)
Why are veins called capacitance vessels?
because of their storage capacity. when CO increases and more vascular beds open, venous blood is transferred to the arterial side of the systemic circulation
What factors enhance venous return to the heart?
-Sympathetic fibers inducing vasoconstriction
-Skeletal muscle activity
-Venous valves
-Respiratory activity
-Cardiac "suction"
What is the key principle of autoregulation of blood flow?
as BP increases, vessels constrict to reduce blood flow
BP decreases, vessels dilate to decrease blood flow
→ this all allows organs to maintain stable perfusion
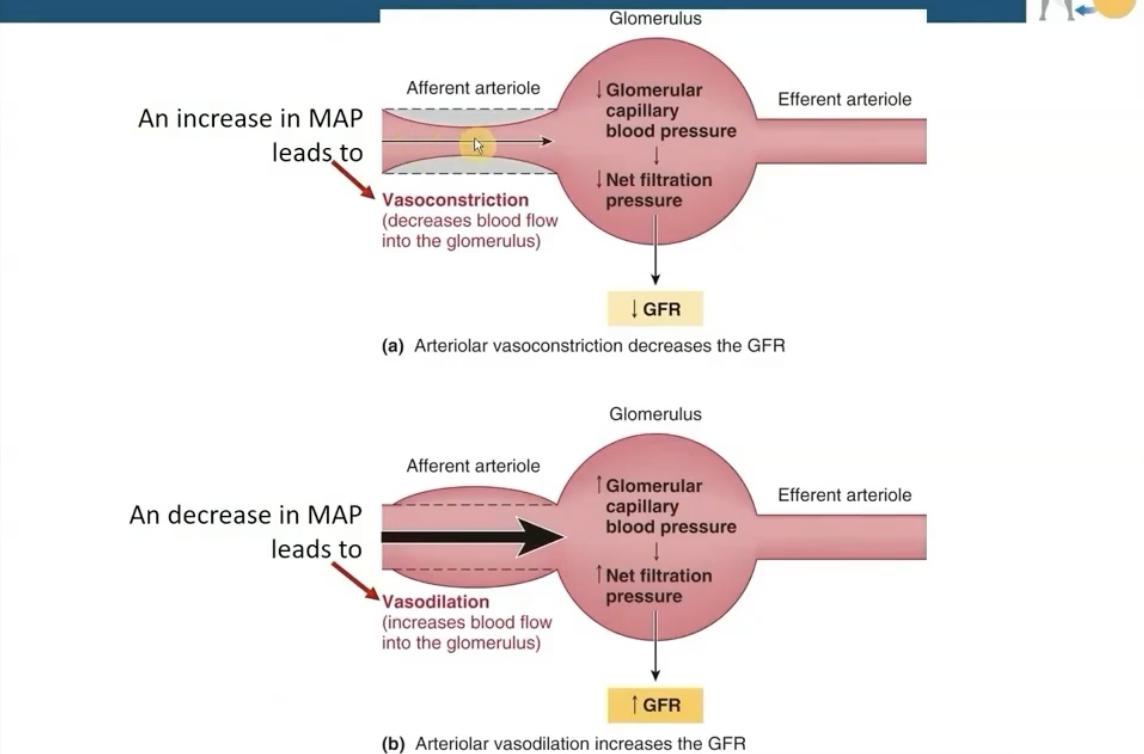
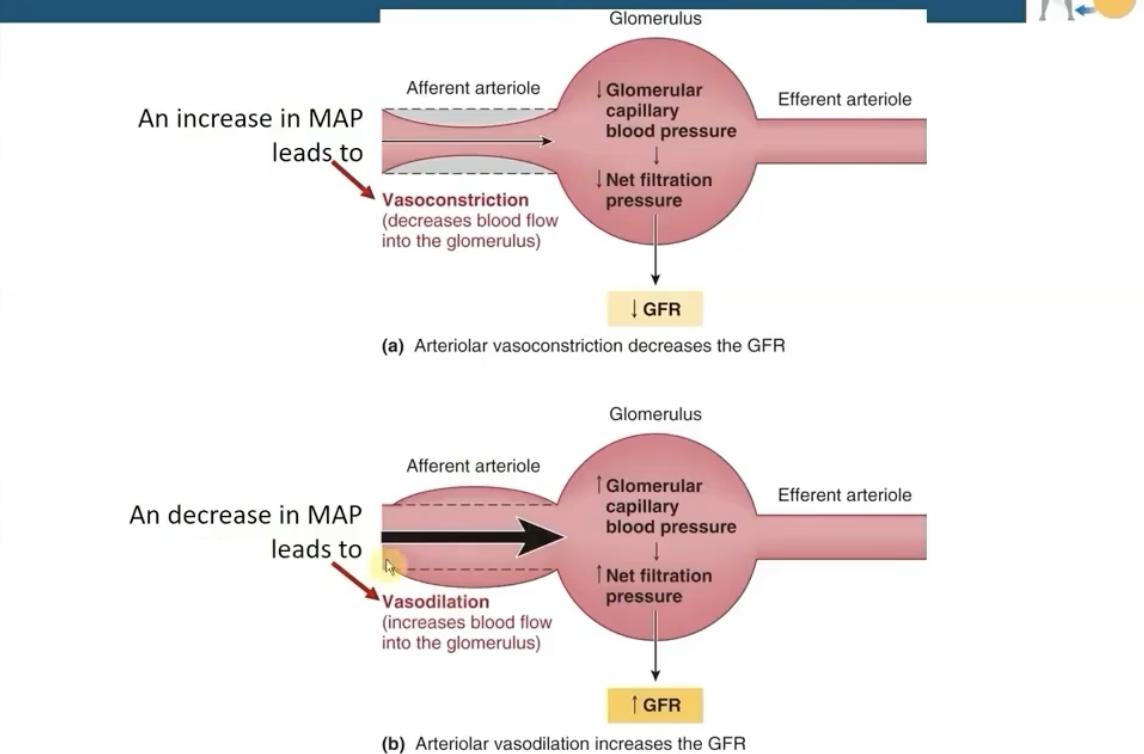
An Increase in MAP leads to what in Autoregulation at the kidneys?
Vasoconstriction in afferent arterioles (Decreases blood flow into the glomerulus)
Decrease in GFR
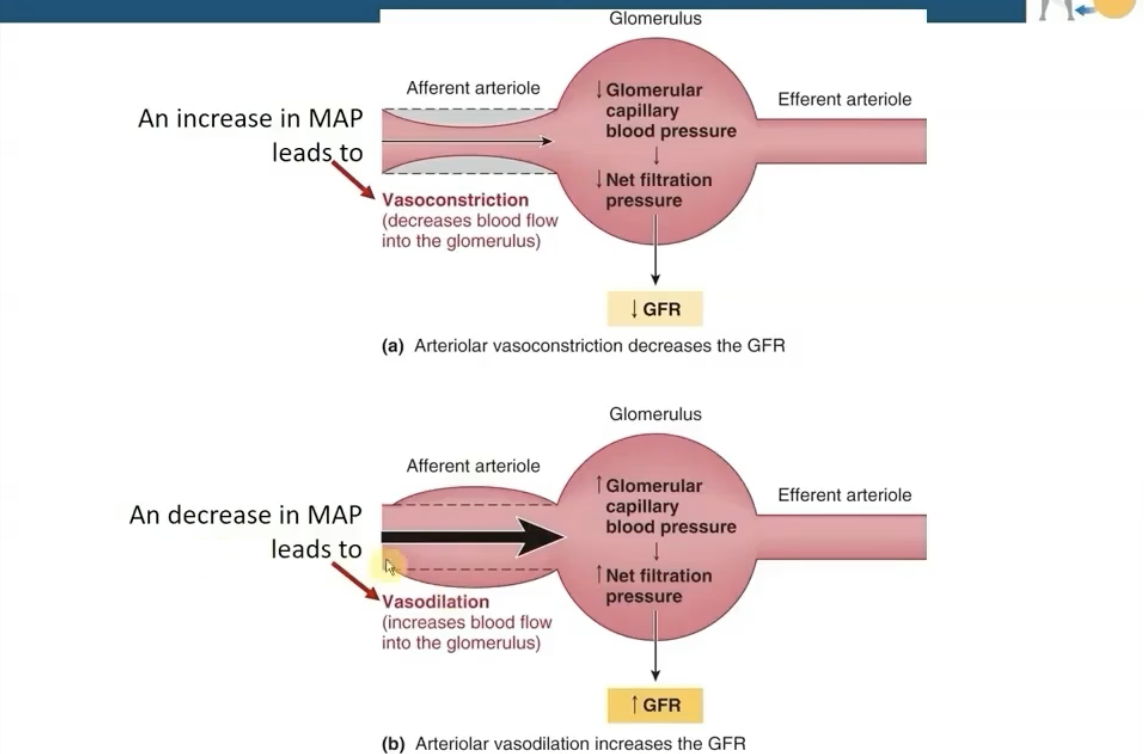
A decrease in MAP leads to what in Autoregulation at the kidneys?
Vasodilation (increases blood flow into the glomerulus)
Increase in GFR
What do arterioles do when arterial pressure gets around 100?
they auto-regulate by vasoconstricting to insure that renal blood flow is kept constant
when it get’s way way too high, they won’t fight back as much and renal blood flow will increase
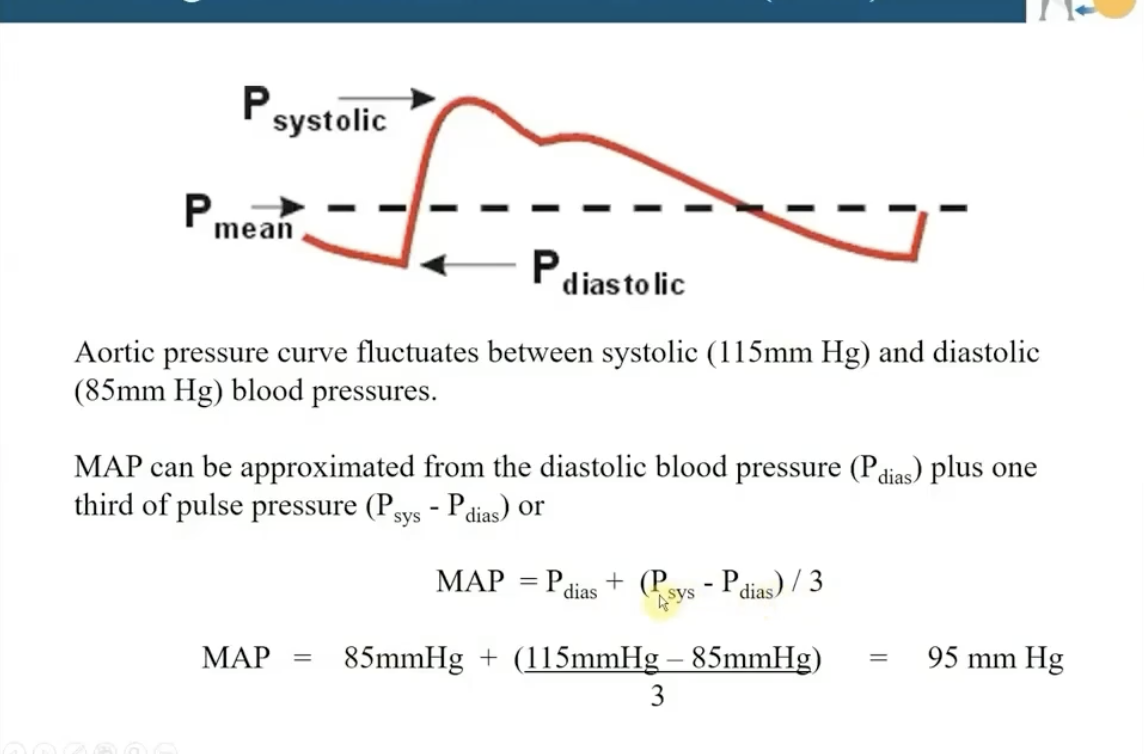
What is the mean arterial pressure
mean pressure in the artery that is measured by baroreceptors
Can use systolic/diastole pressures to assess MAP
How is Mean Arterial Pressure (MAP) Calculated?
MAP = P (Diastolic) + (P sys - P dias)/3
Why is MAP highly regulated?
Must be high enough to provide sufficient pressure for blood flow to the tissues
Pressure must not be too high because it could create extra work for the heart and increase risk of vascular damage
What factors mainly contribute to determining MAP?
Cardiac output (flow)
Total Peripheral Resistance
P= F x TPR
What makes short-term adjustments from deviations of MAP
made by alterations in cardiac output & total peripheral resistance
-Mediated by ANS
What makes long-term adjustments from deviations of MAP?
involves adjusting total blood volume
Restores normal salt & water balance through regulating urine output and thirst
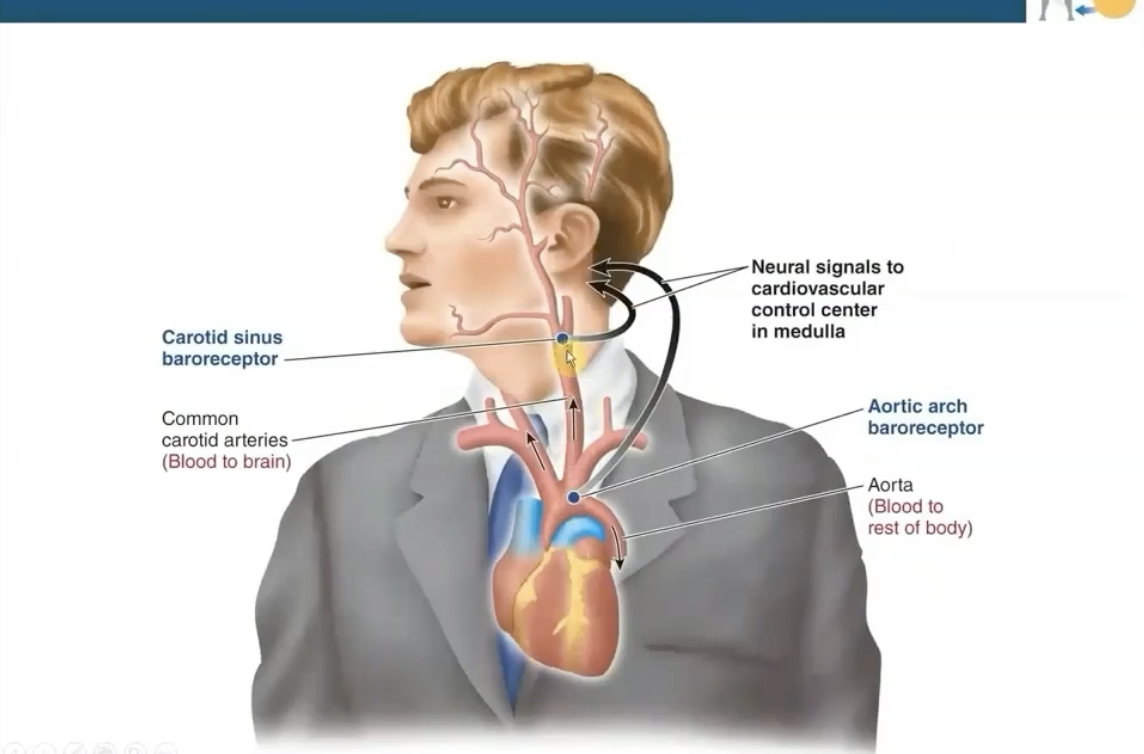
What are baroreceptors at the carotid sinus & the Aortic Arch?
Mechanoreceptors sensitive to changes in MAP
Located before bifurcations to ensure adequate blood flow to the brain and the rest of the body
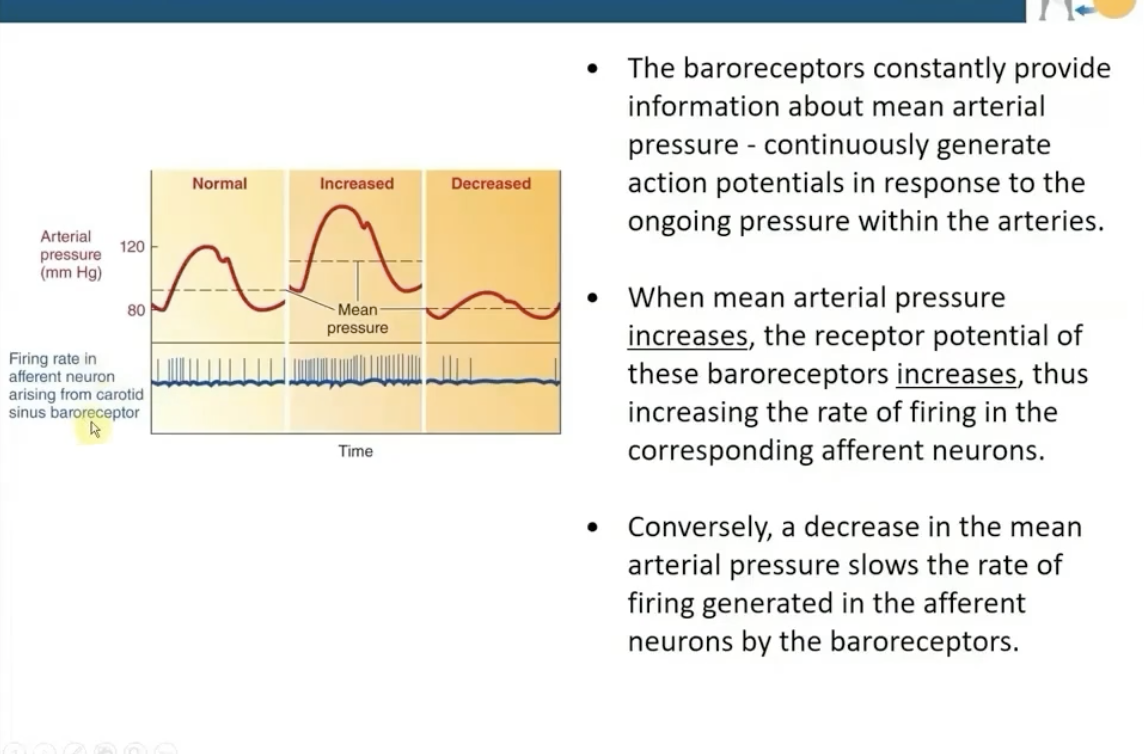
When MAP is increased, what will happen with the baroreceptors?
The receptor potential of these baroreceptors increases
this increases the rate of firing in the corresponding afferent neurons
and vice versa
Where is the integrating center for the cardiovascular system for MAP located? What does it do?
Located within the medulla within the brain stem
It receives afferent impulses about the MAP state
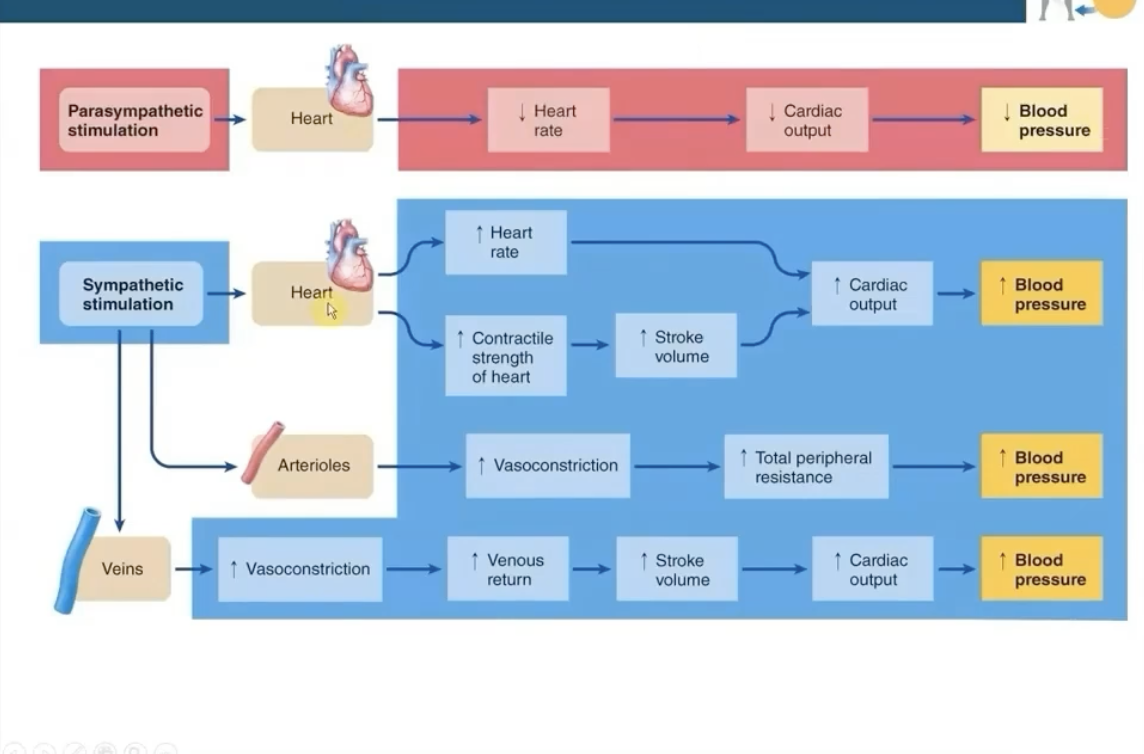
What system regulates the efferent pathway of the cardiovascular system for MAP?
The ANS
Alters the ratio between sympathetic & parasympathetic activity to the heart and blood vessels
Any change in MAP triggers baroreceptors to do what in an attempt to restore blood pressure?
adjust CO and total peripheral resistance (vasodilation/vasoconstriction)
What is circulatory shock?
Inadequacy of blood flow leading to deterioration of vital tissues and organ function
MAP < 60mmHg
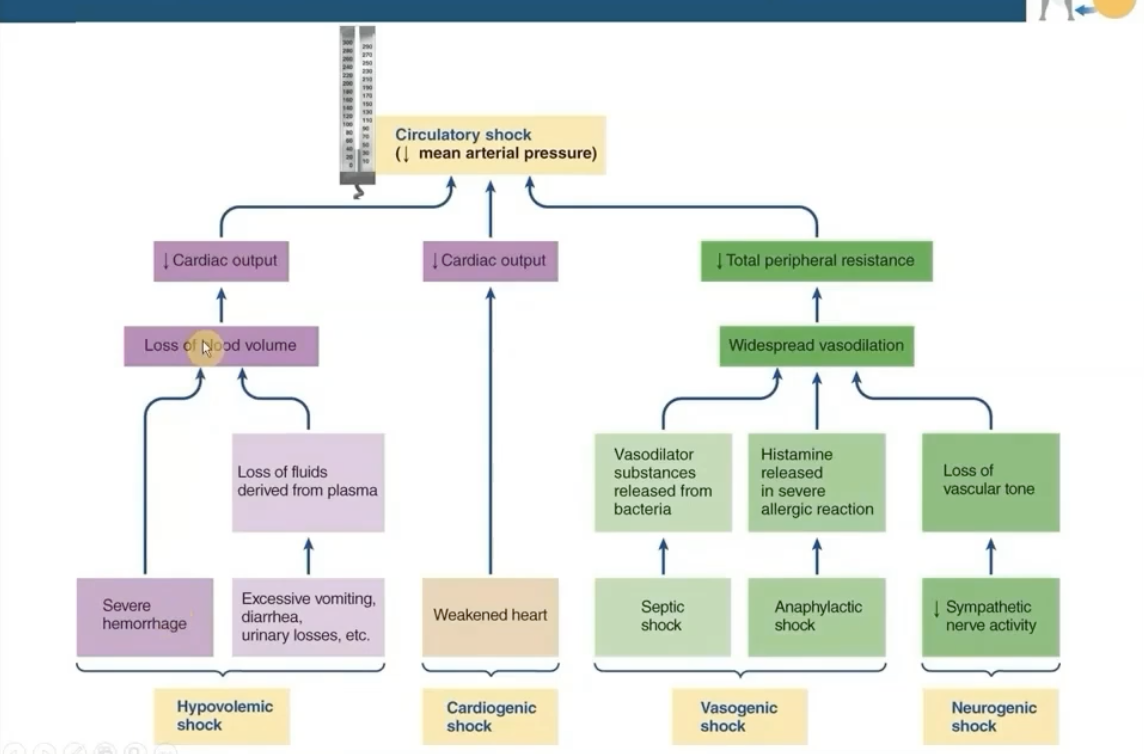
What is vasogenic shock and what are its effects of vasogenic shock on the cardiac system?
septic shock or anaphylaxis → widespread vasodilation → decreased peripheral resistance → lower MAP <60 (circulatory shock)