Adaptive Immunity 1
1/27
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
28 Terms
What is adaptive immunity
Adaptive immunity is part of the humoral adaptive response
Producing antibodies [Soluble serum proteins analysed via electrophoresis]
To combat infections, especially when Innate Immunity barriers have been COMPROMISED.
What are the most abundant proteins in serum
Albumin
Gamma globulins (Ig or antibodies), with IgG being predominant and IgM also critical for defending infections.
Which antibodies are most important for infection defense?
IgG and IgM are most important for defending infections
IgG is key in vaccinations, while IgM provides the initial rapid response.
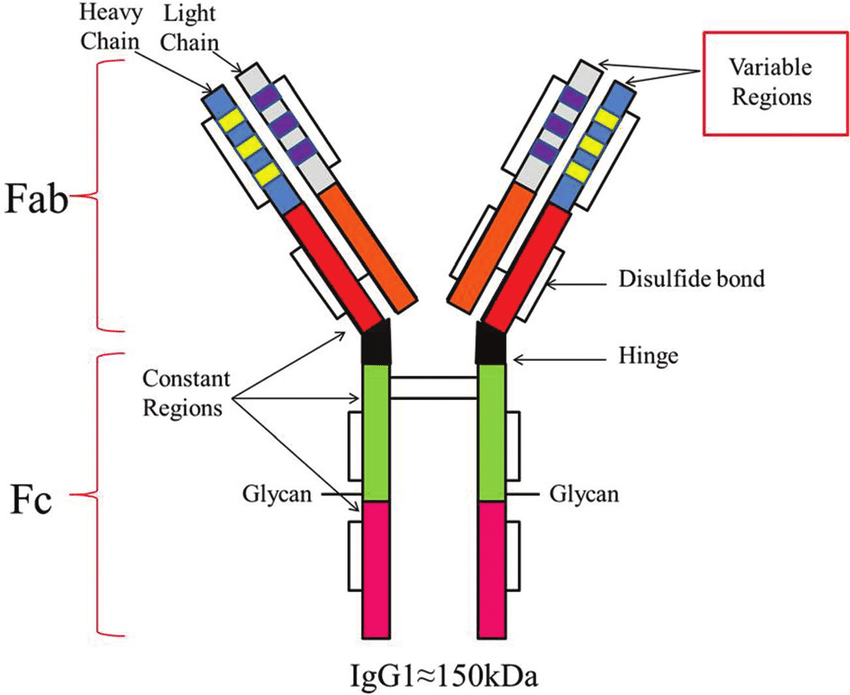
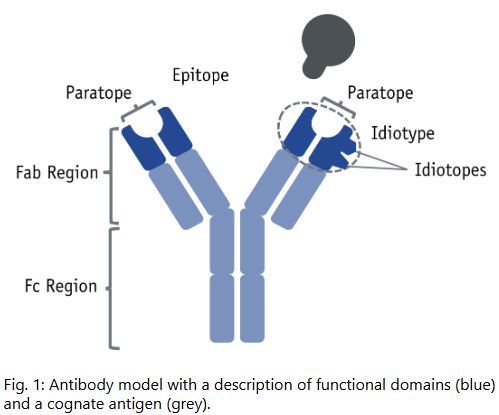
What is the basic structure of an antibody
Antibodies are tetramer molecules with four polypeptide chains:
Two identical light chains
Two identical heavy chains
Joined by disulfide linkages into a Y-shape
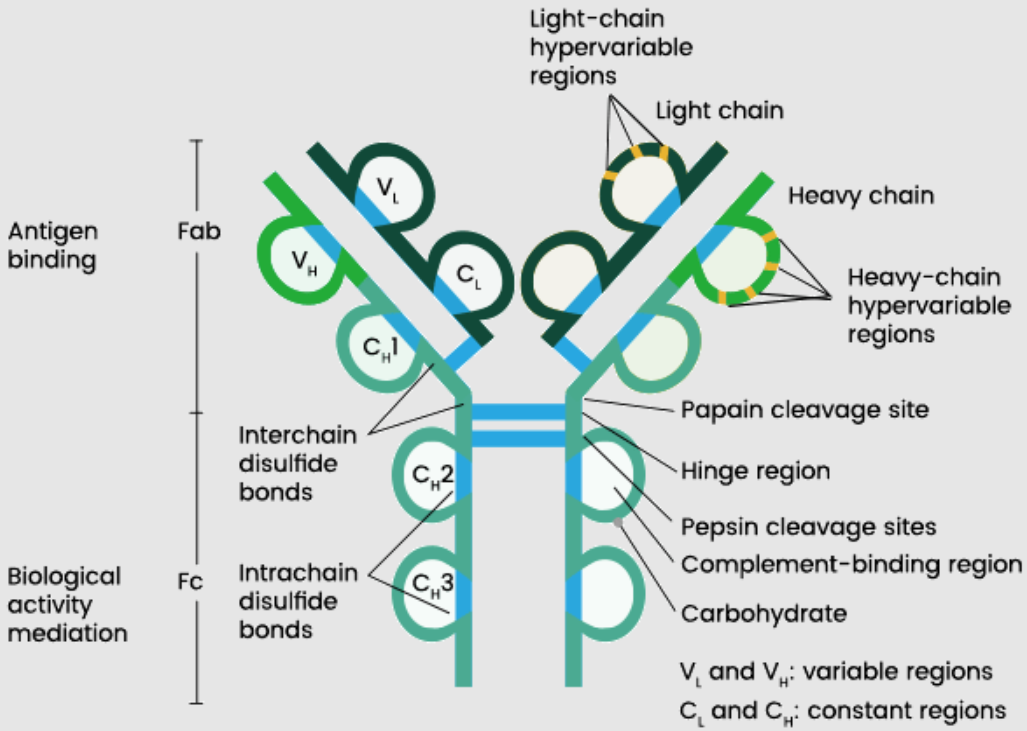
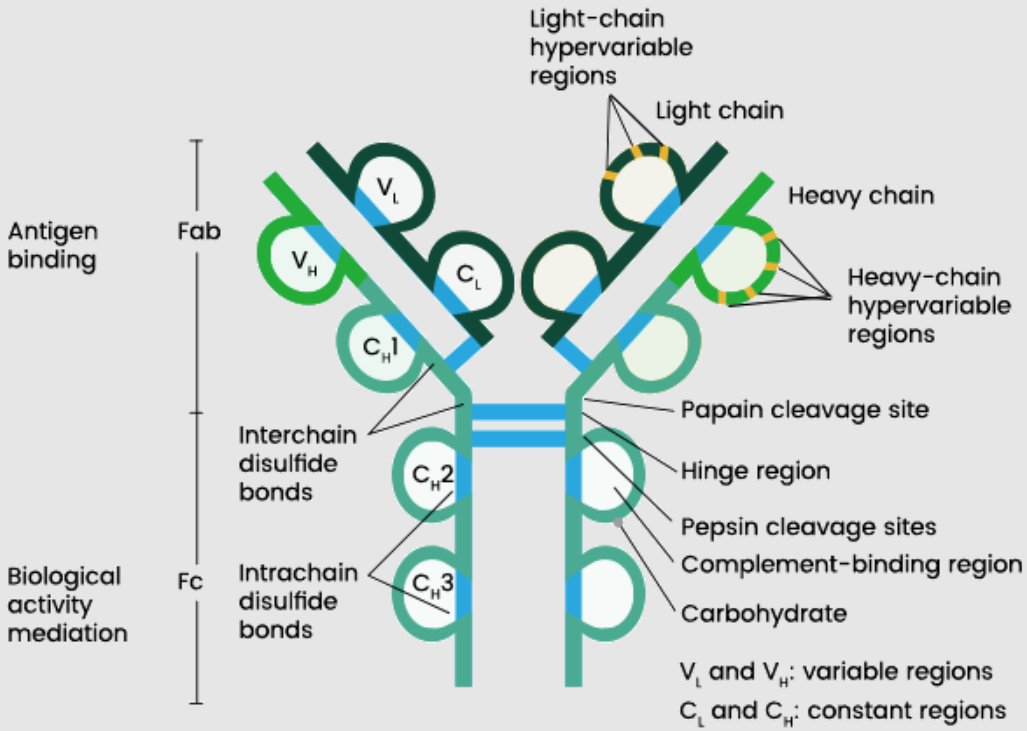
What are the regions of an antibody
The N-terminal regions (FAB - Fragments for Antigen Binding) on the Y-prongs bind non-self antigens
The C-terminal region (FC - First Crystallised) at the base does NOT BIND but interacts with immune cells.
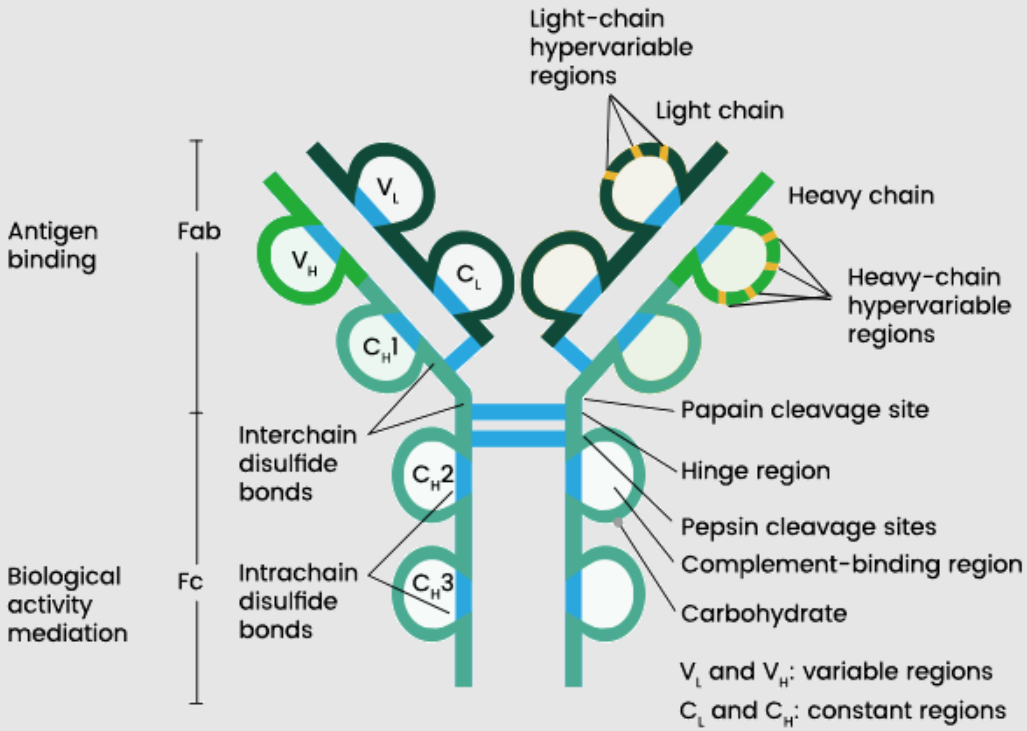
How can antibodies be fragmented
Antibodies can be degraded using enzymes like Papain to separate FAB (antigen-binding) and FC (crystallizable) regions for study or function.
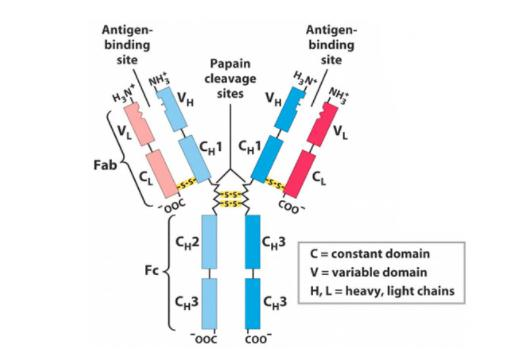
What is the structure of IgG1
IgG1 is a protein with a primary amino acid sequence folding into secondary (hairpin loops), tertiary, and quaternary structures
N-terminal variable regions bind non-self antigens, with conserved regions at the C-terminus.
What structural variation (unrelated to specificity) exists in antibodies and their components?
IgE is a heterotetramer
2 IgG molecules COMBINED forms IgA via C-terminal disulfide linkages
IgD and IgE vary by disulfide POSITIONING, affecting half-life and distribution
IgM is five IgG units LINKED, with 10 antigen-binding sites.
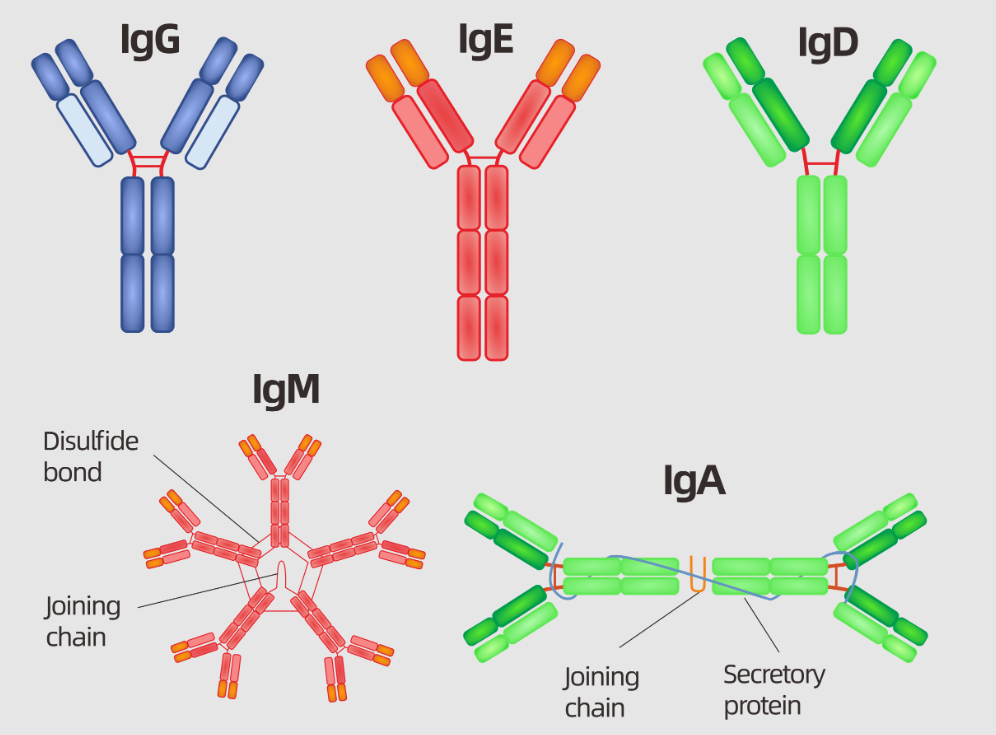
Why is IgM the first antibody response
IgM, with 10 antigen-binding sites and a longer half-life, is the first antibody secreted for a fast, broad response to new pathogens.
As there are multiple sites for antigen binding!
What are epitopes
An epitope is the part of an antigen that the host's immune system recognizes, eliciting the immune response to an invading pathogen.
Epitopes are individual variable regions on antigens, determined by amino acid sequences, targeted by antibodies
Vaccines can target multiple epitopes for a robust immune response.
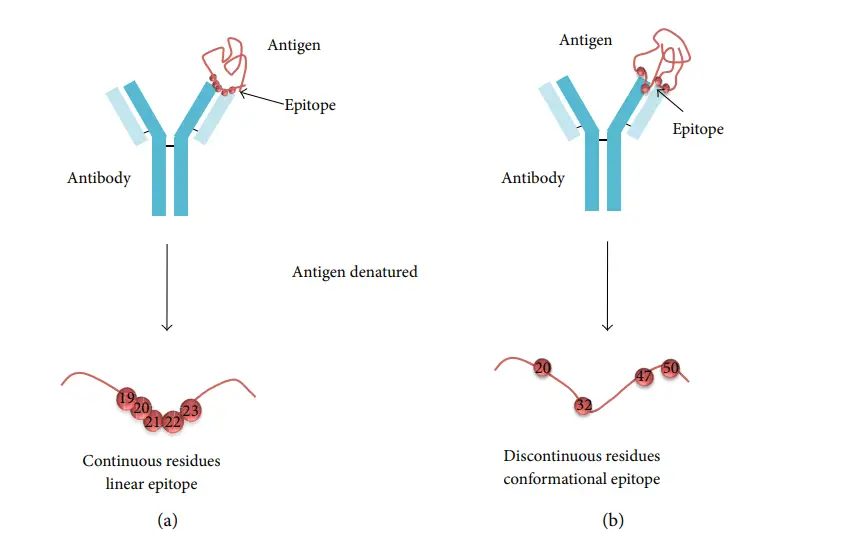
How does antigen structure affect antibody binding
Antigens fold into secondary, tertiary, and quaternary structures
External amino acids (Epitopes) are antibody targets, while buried ones are not, with intraspecies variation possible
What are idiotypes and isotypes in antigens
Idiotypes are hypervariable amino acid sequences in an organism's variable region. Epitope is a component of the Idiotype!
Isotypes are species-specific
With Allotypes reflecting interspecies isotype variation.
—
Idiotype sequence of aa which is very hyper variable corresponding to the antigen binding site
There is folding of the idiotype region so it will wrap around the antigen giving the protein-protein interaction which is non-covalent (ionic, hydrogen bonding, hydrophobic interactions) so it isn’t a permanent bond (can unform depending on conditions)
What interactions occur in the idiotype region
Folding up of the idiotype region causes:
Dynamic, Non-covalent protein-protein interactions
(Ionic, electrostatic, hydrogen, hydrophobic)
Forming and unforming based on conditions.
Structural Variation RELATED to Antibody Specificity
Related to the different types of organisms
At N terminal (variable region) - Idiotype sequence of aa which is very hyper variable corresponding to the antigen binding site
There is folding of the idiotype region so it will wrap around the antigen giving the protein-protein interaction which is non-covalent (ionic, hydrogen bonding, hydrophobic interactions) so it IS NOT a PERMANENT bond (can unform depending on conditions)
What is the humoral component of adaptive immunity
The humoral component involves B cells (from myeloid precursor bone marrow stem cells)
Producing antibodies when contacting non-self antigens, known as antibody generators AND acute phase / complement proteins.
Where do antibodies originate
Antibodies are produced by Plasma cells
They originate from B-cell stem cells in bone marrow
Processed via Bursa processing (named from chicken discovery)
Into mature B lymphocytes in the spleen (primary lymphoid tissue).
B Cells differentiate into Plasma Cells and Memory B Cells
How do B cells respond to antigens
B cells in contact with antigens differentiate and divide into 1) Plasma cells (with extensive ER for antibody synthesis) and 2) Memory B cells (stored in secondary lymphoid tissue).
—
Plasma cells AND memory B cells
B stem cells develop into B lymphocytes from Bursa processing. They are then stored in secondary lymphoid tissues such as the spleen or lymphatic glands.
Bursa processing for our B cells happens in the spleen. The spleen is our primary lymphoid tissue- Where B cells mature.
Plasma is the antibody secreting cell.
Memory B cells are laid down in the secondary lymphoid tissue for when you come into contact next with the same antigen. Memory B cells are usually found in secondary lymphoid organs such as the spleen or the lymph nodes.
Upon second time contact, the memory B cells will turn on and differentiate to become plasma cells. This is called the clonal selection theory.
What are the roles of plasma and memory B cells
1) Plasma cells secrete antibodies until clonal exhaustion and death
—
2) Memory B cells, laid down in secondary lymphoid tissue, activate and convert to plasma cells upon re-exposure to the antigen.
What is the clonal selection model
Antibodies come from ONE Memory B-cell clone with singular specificity due to its N-terminal amino acid sequence
Binding ONE specific antigen-sensitive cell to trigger proliferation and differentiation into plasma and memory cells.
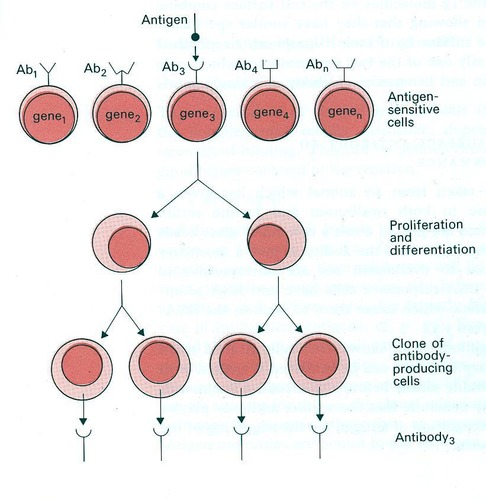
What is the primary immune response
It involves the activation of B and T cells in presence of antigen
Where B cells are differentiating into plasma cells which produce antibodies.
The primary response is slower, with IgM as the first antibody secreted due to its numerous antigen binding sites, facilitating a broad initial response to a new antigen.
—
Slower to select the clone that is specific to the antigen/ the specific epitope of the antigen which has to proliferate and differentiate to get enough antibodies to be detected.
Simultaneously, memory cells will be laid down in the secondary lymphoid tissue in preparation for a secondary response
What is the secondary immune response
Memory B cells and memory T cells (formed during the primary response) quickly recognise and respond to REOCCURRING antigen exposure.
Memory B cells rapidly differentiate into plasma cells that predominantly produce IgG.
IgG is more efficient (higher affinity, crosses placenta, opsonizes pathogens).
Some memory cells are retained (not all are used up) to ensure long-term immunity for future encounters.
—
The secondary response is immediate, using IgG from memory B cells, key to vaccination success for rapid, specific pathogen defense.
This bypasses the need for initial antigen presentation and clonal selection, leading to a much faster and stronger response.
What are the characteristics of the humoral adaptive immune response
Characteristics include:
Memory for secondary responses
Specificity to epitopes
Tolerance to avoid cross-reactivity with self-proteins (preventing autoimmunity).
How is antibody diversity generated
Antibody diversity arises from:
Gene splicing of conserved [Introns] and variable [Exons] regions
Somatic mutation
mRNA splicing variations
—
V(D)J recombination is the process by which the variable regions of antibodies are assembled from separate gene segments.
It occurs in the bone marrow during B cell development, before B cells encounter antigens and differentiate into plasma cells or memory B cells.
Exons: Coding sequences (V, D, J, and C segments)
V (Variable) segments: Contribute to the antigen-binding site.
D (Diversity) segments: Add further variability (only present in heavy chains, not light chains).
J (Joining) segments: Connect the variable region to the constant region.
C (Constant) segments: Encode the constant region of the antibody (e.g., Cμ for IgM, Cγ1 for IgG1 after class switching).
—
D-J Recombination: A D segment joins a J segment, removing unwanted segments.
V-DJ Recombination: A V segment joins the DJ exon, forming a VDJ exon.
The final gene includes the VDJ exon (variable region) and a C segment (constant region), producing an IgM heavy chain initially.
![<p>Antibody diversity arises from:</p><ol><li><p><strong><mark data-color="purple" style="background-color: purple; color: inherit">Gene splicing of conserved [Introns] and variable [Exons] regions</mark></strong></p></li><li><p><strong><mark data-color="purple" style="background-color: purple; color: inherit">Somatic mutation</mark></strong></p></li><li><p><strong><mark data-color="purple" style="background-color: purple; color: inherit">mRNA splicing variations</mark></strong></p></li></ol><p>—</p><p><strong><mark data-color="purple" style="background-color: purple; color: inherit">V(D)J recombination</mark></strong> is the process by which the variable regions of antibodies are assembled from separate gene segments.</p><p><strong><mark data-color="purple" style="background-color: purple; color: inherit">It occurs in the bone marrow during B cell development, before B cells encounter antigens and differentiate into plasma cells or memory B cells.</mark></strong></p><p><strong><em>Exons: Coding sequences (V, D, J, and C segments)</em></strong></p><ul><li><p><strong>V (Variable)</strong> segments: Contribute to the antigen-binding site.</p></li><li><p><strong>D (Diversity)</strong> segments: Add further variability (only present in heavy chains, not light chains).</p></li><li><p><strong>J (Joining)</strong> segments: Connect the variable region to the constant region.</p></li><li><p><strong>C (Constant)</strong> segments: Encode the constant region of the antibody (e.g., Cμ for IgM, Cγ1 for IgG1 after class switching).</p></li></ul><p>—</p><ul><li><p><strong>D-J Recombination</strong>: A D segment joins a J segment, removing unwanted segments.</p></li><li><p><strong>V-DJ Recombination</strong>: A V segment joins the DJ exon, forming a VDJ exon.</p></li><li><p>The final gene includes the VDJ exon (variable region) and a C segment (constant region), producing an IgM heavy chain initially.</p></li></ul><p></p>](https://knowt-user-attachments.s3.amazonaws.com/0596560e-3039-44cd-bfa3-b265c6b1f3b3.png)
How do antibodies link adaptive and innate immunity
Antibodies act as variable adapter molecules
N-terminal binding to bacteria activates innate immunity via the conserved C-terminal FC region
This is recognised by phagocyte FC receptors for opsonisation.
How does antibody opsonization enhance phagocytosis
Antibody opsonisation binds antigens at the N-terminus
With the FC region recognised by phagocyte FC receptors
Increasing adherence and targeting for engulfment.
How does the classical complement pathway activate
The classical pathway requires antibody presence:
Antigen on a bacterial surface is opsonised by antibody at the N-terminus
Binding C1 at the FC region to form antibody C1 (AC1)
Then adding C4 and C2 to create AC142 (equivalent to C3 convertase so fragments C3 into C3a and C3b).
C3a has a chemotactic role and causes granulation of mast cells
AC142 can also bind to C3 giving AC1423 (C3b) then be a target for phagocytic cells / any cell that has a C3B receptor on it.
—
Gives an enzyme and esterase activity
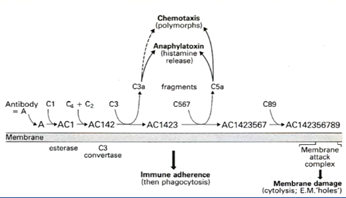
What does C3 convertase do in the classical pathway
AC142 (C3 convertase) fragments C3 into:
C3b (opsonizes bacteria for phagocytosis)
and
C3a (triggers chemotaxis and mast cell granulation).
What happens in gram-negative infections with the complement cascade
For gram-negative organisms:
The cascade forms C5 convertase from C3b and C3 convertase
Releasing:
C5a (chemotaxis, mast cell granulation)
and
C5b, which recruits proteins to form a membrane attack complex
Puncturing the bacterial membrane.
What does Humoral component mean?
Soluble proteins that have a function in immunity:
Acute proteins
Complement proteins → COMPLEMENT PATHWAY/ ALTERNATIVE PATHWAY is the humoral component of Innate Immunity
Antibodies → ANTIBODIES is the humoral component of the Adaptive Immunity