Lecture 1: Introduction to Mental Health and Illness
1/23
Earn XP
Description and Tags
MBB2
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
24 Terms
Mental Health
is a state of mental well-being that enables people to cope with the stresses of life,
realize their abilities, learn well and work well, and contribute to their community
Mental illness
a clinically diagnosable disorder that
significantly interferes with an individual’s
cognitive, emotional or social abilities
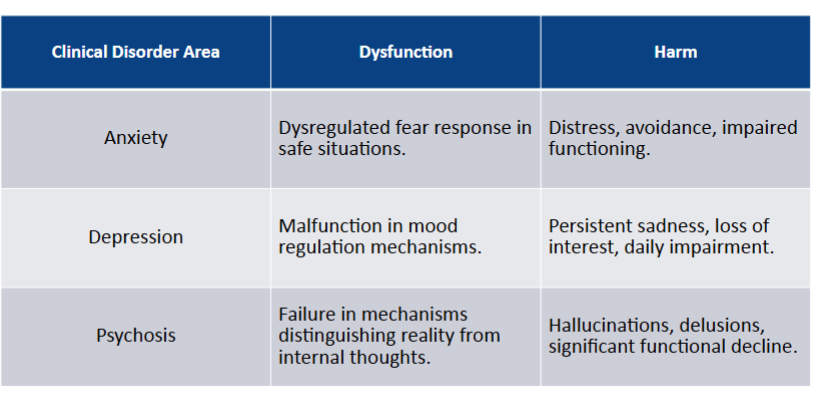
Wakefield’s HDA defines mental disorders by two criteria
Dysfunction – a failure of an internal neurobiological or
mental mechanism to perform its natural (evolved)
functionHarm – this dysfunction results in harm judged by
societal standards
This model combines biological facts with cultural values
to define mental disorder
Mental Disorder
is a syndrome characterized by clinically significant
disturbance in an individual’s cognition, emotion regulation, or behaviour that
reflects a dysfunction in the psychological, biological, or developmental processes
underlying mental functioning.
Applying the Wakefield HDA Model: Examples
-
What is not a ‘Mental Disorder’?
An expectable or culturally approved response to a common stressor or loss, such as the death of a
loved one
Approaches to Classification Models
-
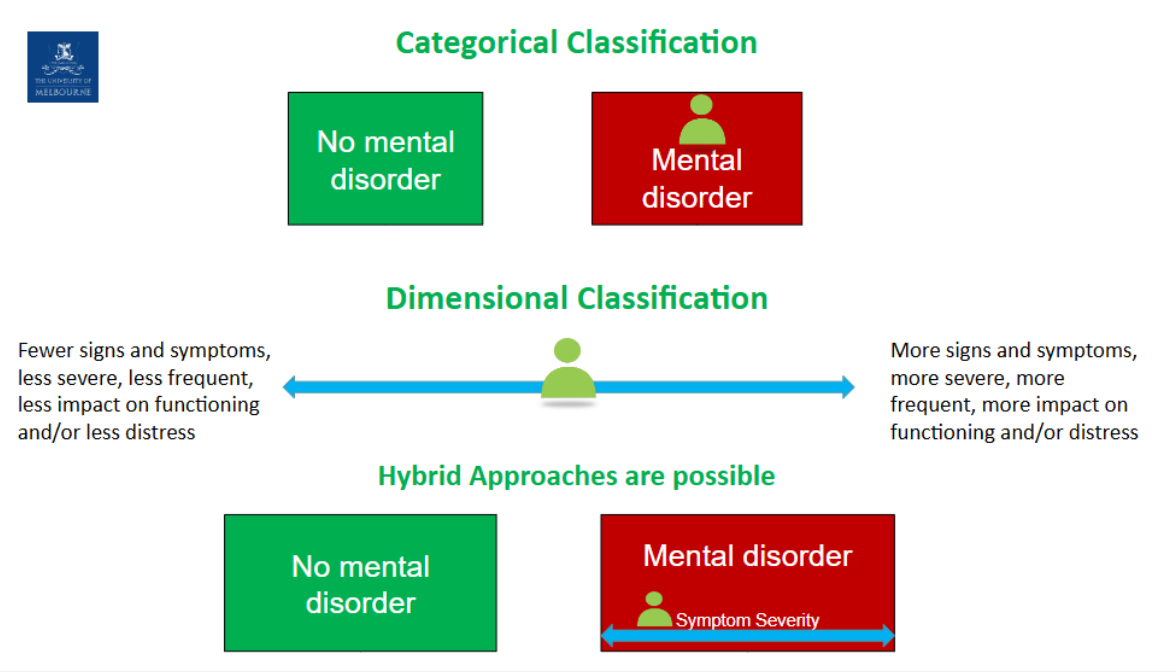
Strengths and Limitations to Categorical
Better clinical and administrative utility - clinicians
are often required to make dichotomous decisions.Easier communication
Strengths and Limitations to Dimensional
Closely model lack of sharp boundaries between
disorders, between disorders and normalityHave greater capacity to detect change, facilitate
monitoringCan develop treatment-relevant symptom targets-
not simply aiming at resolution of disorder (most
treatments actually target symptoms, not disorders)
Strengths and Limitations to Hybrid
People’s life experiences differ. This variability across individuals
extends to states of mental health and illness as does the degree to
which we are resilient against or vulnerable to, the latterIt is quite complex which makes it unreliable
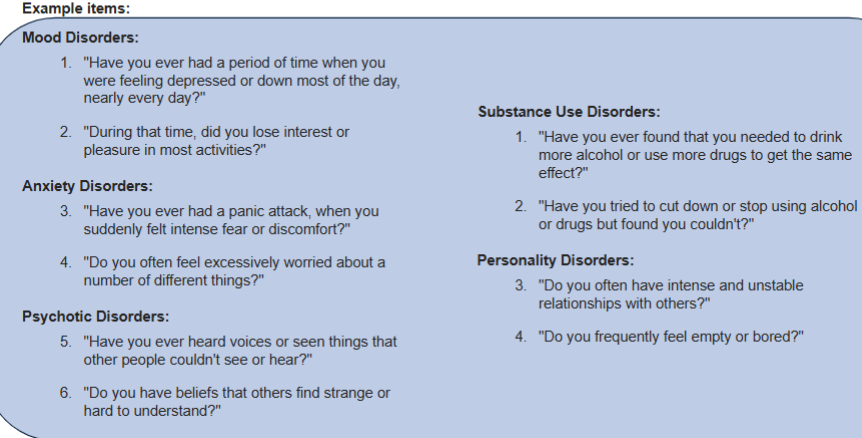
DSM-5-TR Diagnosis
Diagnosis will be made on the basis of:
• Clinical Interviews – clinician and client semi-/structured
• Text descriptions – in DSM covering how disorders present
• Diagnostic criteria – does presentation match checklistCurrently presenting symptoms and severity - e.g. depressed mood
Rule out disorder due to general medical condition – e.g. due to hypothyroidism
Rule out disorder due to direct effects of a substance - e.g. alcohol induced
Establish boundary with no mental disorder
• Clinical Significance/Cultural Norms. E.g bereavement vs clinically significant depressionDetermine specific primary disorder(s)
• Multiple diagnoses possibleAdd subtypes/specifiers
• severity (mild moderate, severe – with or without
psychotic features)
• treatment relevant (poor insight, atypical, etc.)
• longitudinal course (with/without full inter-episode
recovery, seasonal pattern)
Semi-Structured Interview Example: Mental
State Exam (MSE)
-
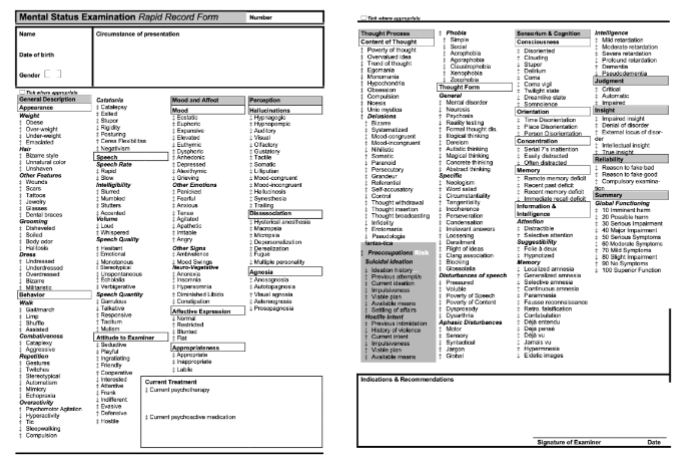
Structured Clinical Interview for DSM-5-TR
(SCID-5-TR)
-
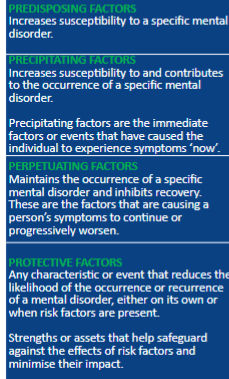
Case formation
-
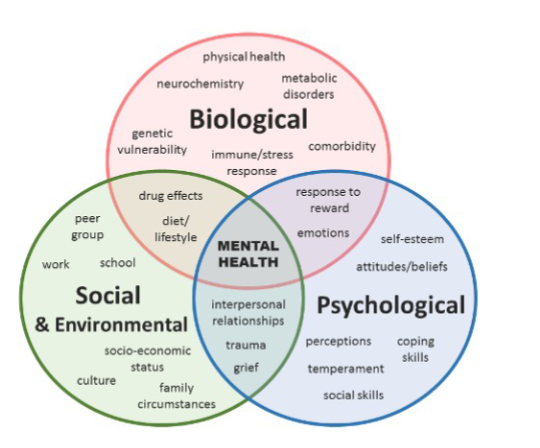
Biopsychosocial Paradigm
-
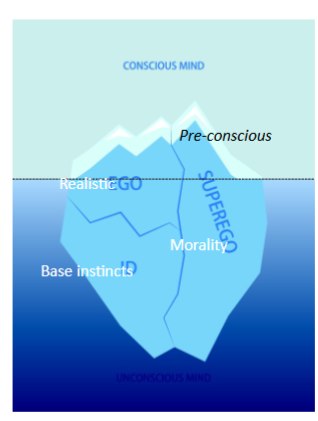
Psychoanalytic Paradigm (Freud)
Freud believe the unconscious has a
profound influence on what we do
and how we feel in day-to-day life.
• Psychopathology caused by unresolved
childhood conflicts and repressed desires.
• Only through gaining awareness of
unconscious processes can individuals
resolve and recover
Behavioural Paradigm (Watson, skinner)
Goals of behavioural interventions include:
interrupt and/or
change
maladaptive
stimulus-response
associations;reinforce adaptive
behaviour.
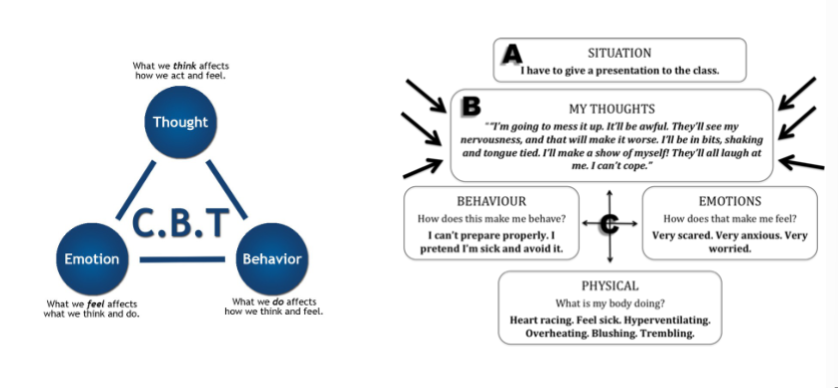
Cognitive Paradigm (Beck)
-
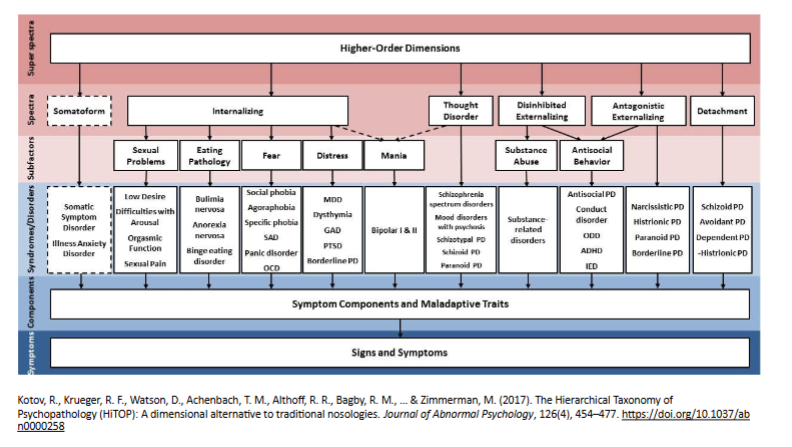
Hierarchical Taxonomy of Psychopathology
-
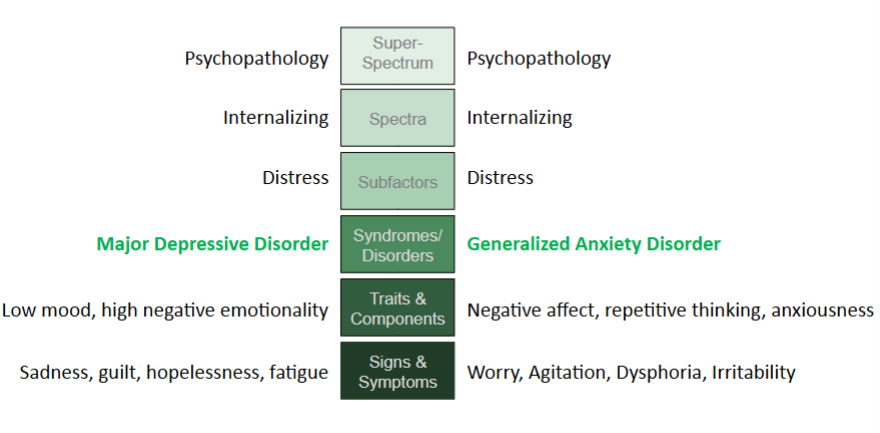
Example Case: DSM vs HiTOP
The DSM-5-TR model sees this as two separate disorders that are co-occurring (or ‘co-morbid’).
• Treatment might focus on two distinct conditions.
The HiTOP model sees these as part of a shared internalizing spectrum rather than two separate disorders.
• Treatment could focus on core emotional dysregulation rather than treating two distinct conditions.
HiTOP Model: MDD and GAD Example
-
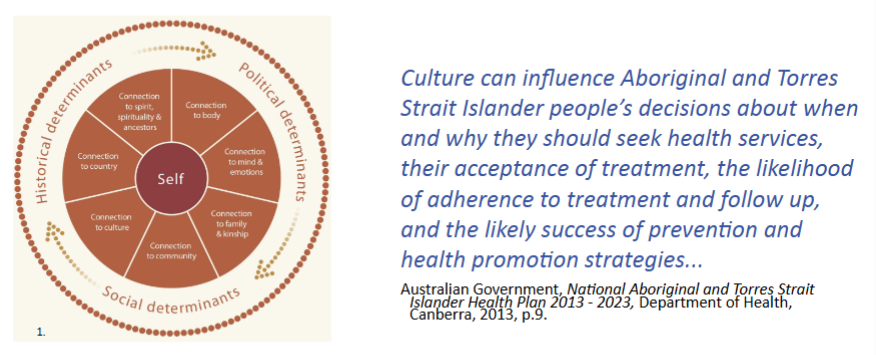
Cultural Models: Australian First Nations Model of Social and
Emotional Wellbeing
-
Anti-Psychiatry Perspectives
Psychiatrists including:
- Thomas Szasz: mental illness is a myth (e.g. no
disease identified)
- J.D. Laing: psychiatry inappropriately
pathologizes human distress (e.g. schizophrenia
symptoms are a normal response to adversity).
Social theorists like Michel Foucault and Erving
Goffman argued:
- psychiatry enforces societal norms.
- serves to marginalise and stigmatise those
with psychological problems.
- is coercive, pseudoscientific, and socially
constructed.
- causes harm
Cultural Models: Mad Pride
Mad Pride
A social and political movement.
Grounded in protest and challenge of stigma,
discrimination, and historical psychiatric practices
that infringe on human rights.
Pride in the self as a complex whole that incorporates
madness into identity.
Reclamation of pejorative terminology. Parallels with
LGBTIQA+ Pride movement.