Lifespan Pt 2 (Terms)
1/11
Earn XP
Description and Tags
Lectures 5-7
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
12 Terms
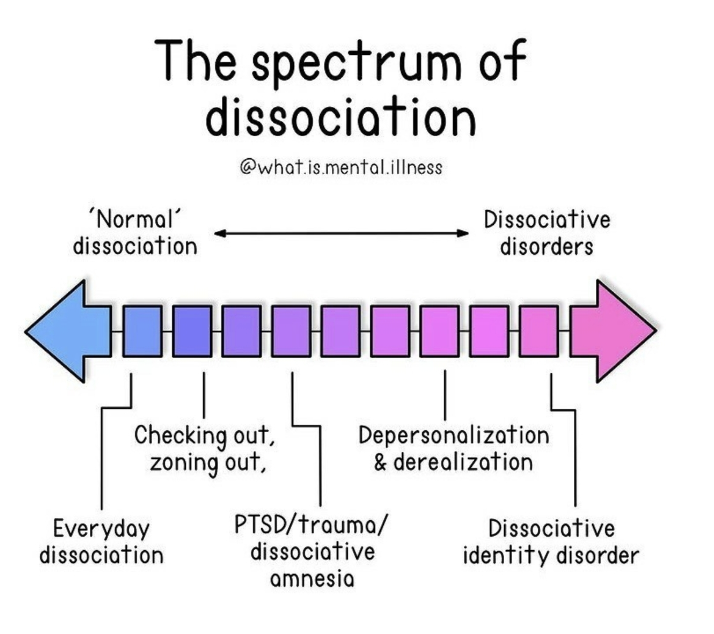
What is depersonalization vs derealization? Provide examples of each . Of note?
Both types of dissociation
Depersonalization: Experiences of unreality, detachment, or being an outside observer with respect to one’s thoughts, feelings, sensations, body, or actions (ex. perceptual alterations, distorted sense of time, unreal or absent self, emotional and or physical numbing)
Derealization: Experiences of unreality or detachment with respect to surroundings (ex. individuals/ objects are experienced as unreal, dreamlike, foggy, lifeless or visually distorted
Of note for DPDR suicide and NSSI risk is high
Describe the posttraumatic framework for understanding DID (3 stages). Example for help understanding.
3 steps, then provide an example (5 stages).
Early & Severe trauma → Dissociation as a defense to cope with trauma → Compartmentalizing experiences and memories
Example of the Posttraumatic Framework for DID
A child grows up in a home with chronic, severe abuse (physical, s****l, or emotional), beginning very early in life.
Because the child cannot escape, their mind uses dissociation to cope—essentially “checking out” during overwhelming events.
Over time, the child learns to mentally separate different experiences:
The part of them that goes to school
The part that takes the abuse
The part that manages daily responsibilities
The part that holds fear, anger, or traumatic memories
These separated states eventually become more elaborated “parts” or identity states, each holding different memories, emotions, or roles.
As an adult, the person may experience gaps in memory, loss of continuity, or feeling like different parts of them handle different situations—hallmarks of DID.
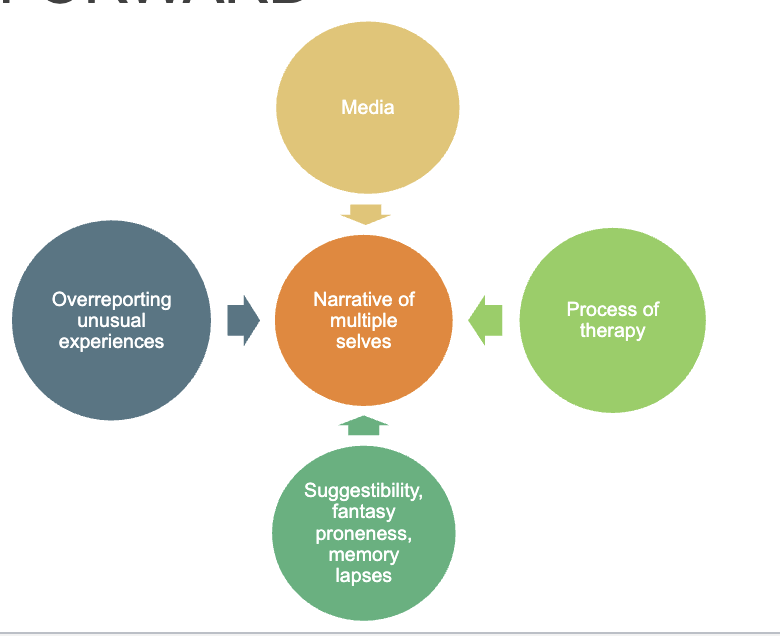
Describe the sociocognitive framework for understanding DID
The the 4 components: MPSO
“My Parmesan Smells Odd”
DID is a “true disorder of self-perception in which individuals come to believe in and act based on narratives of distinct indwelling selves.”
Media: Media increases public awareness of DID, making the idea more available as a way to understand one’s experiences.
Process of therapy: Certain therapeutic styles may unintentionally reinforce or shape dissociative symptoms.
Asking leading questions about “parts”
Using hypnosis or guided imagery
Therapist expectations that DID should be present
Suggestibility, A tendency for expectations, authority figures, fantasy, and cultural narratives to shape how individuals interpret and experience dissociation, leading symptoms to be organized around socially reinforced concepts such as “parts” or “alters.”
Over-reporting of unusual experiences: Basically, paying too much attention to certain kinds of dissociative sensations could make a person more prone to developing this (Attentional Attributions)
Some individuals may overreport or interpret normal experiences as pathological:
Daydreaming → “losing time”
Mood shifts → “switching”
Internal conflict → “different parts”
This isn’t intentional lying; it reflects:
Misinterpretation of symptoms
High distress
Desire for explanation or validation
This overreporting feeds into a growing narrative of multiplicity.
Overall: development of this disorder in an inorganic way: societal cognitive factors
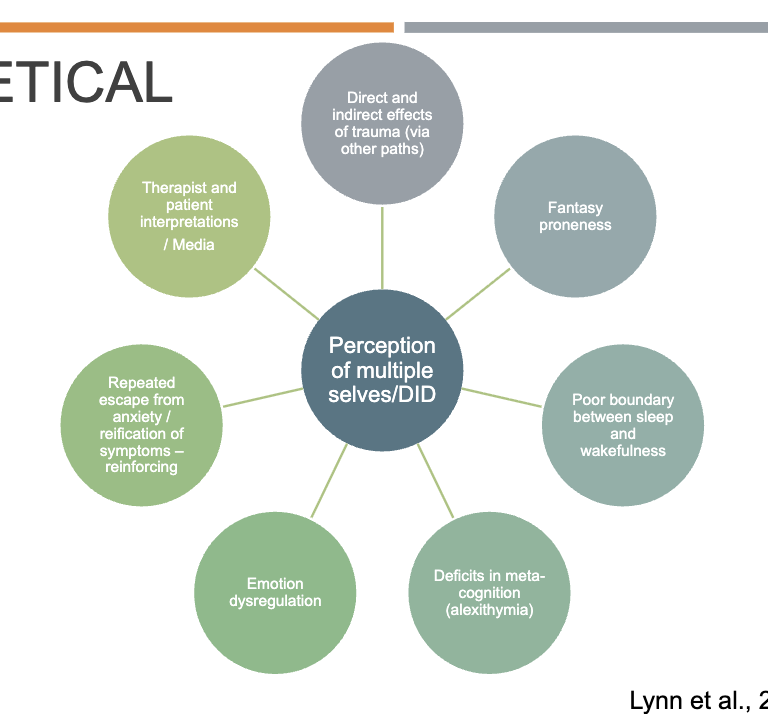
Describe the transtheoretical framework for understanding DID
Combination of _____ and ______ framework for understanding DID.
Added elements:
One physiological, one behavioral, 2 emotional
Idea here: a combination of the sociocognitive and posttraumatic framework for understanding DID, with some added elements:
Boundary issues between sleep and wakefulness
Avoidance/ escape using DID can perpetuate/reinforce these tendencies.
Deficits in meta cognition (alexithymia): Difficulty identifying/ describing one’s own emotions
Emotion Dysregulation
Who founded the harm reduction framework?
What is the HR framework?
Focuses on reducing the negative ____, _____, and _______ consequences of _______ without
Emphasizes that…
Goal:
Mark Tyndall: leading harm reduction researcher
Harm reduction: A pubic health approach that focuses on reducing the negative health, social, and legal consequences of drug use without requiring people to stop using drugs.
Tyndall emphasizes that any positive change is success, even if drug use continues. Approach is evidence-based, nonjudgemental, and person-centered.
The goal is to keep people alive and as healthy as possible, not to force abstinence.
(L6) What is a behavioral addiction? Benefits of including these in DSM? Harms?
Definition?
What do Billieux et al. argue?
Benefits? (4)
Harms? (5)
A behavioral addiction is excessive, impairing involvement in a non-substance behavior that resembles substance addiction—but Billieux et al. argue that many so-called behavioral addictions are poorly defined, atheoretical, and overpathologize normal behaviors.
DSM includes gambling disorder within SUDs and Internet gaming disorder as a condition for further study
Benefits
Legitimizes real disorders: Gives clinical recognition to behaviors that cause genuine impairment.
Improves access to treatment
DSM inclusion → insurance coverage + evidence-based care.Stimulates research and clearer criteria
Leads to more rigorous studies and better diagnostic precision.Aligns with biological + cognitive data
Especially for gambling disorder, where evidence parallels substance addiction.Harms
Risk of overpathologizing normal behaviors
Everyday hobbies can be mislabeled as addiction using weak methods.
Poor diagnostic specificity
Many proposed behavioral addictions lack unique mechanisms or strong evidence: Why lack of unique mechanisms matters:
If a proposed behavioral addiction relies on broad, nonspecific mechanisms shared across many disorders and normal behaviors, the diagnosis lacks construct validity and risks overpathologizing everyday activities.Created from anecdote + copied criteria
Often based on:anecdotal cases,
substance-use criteria pasted onto behaviors,
predictable correlations with impulsivity, so the behavior is not necessarily an addiction.
Billieux et al., 2015
Ignoring context + natural recovery
Many excessive behaviors are temporary and situational.One-size-fits-all treatment risk
Labeling everything as addiction can lead to inappropriate SUD-style interventions.Dilutes the meaning of “addiction”
Overexpansion weakens the construct and public trust.
Describe a few biological risk factors for substance use disorders? (7)
GEBTN
Green Elves Bring The New year.
Genetics: around 50% of risk, polygenic. Influences drug metabolism pathways, brain development, personality traits like impulsivity and sensation seeking, and stress reactivity. Family history: pretty big biological red flag
Epigenetics: early life stress and timing of exposure can influence whether genes are expressed
infleunced by factors such as early life stress
timing of substance exposure (in utero or early postnatal expsosure to drugs particularly bad).
Brain development (adolescence= high risk): Reward circuits mature early, but executive control circuits mature late (mid 20s). Early exposure to drugs slows down executive function development. Social deprivation during infancy and early childhood leads to delayed maturation and impaired brain connectivity (could increase impulsivity). Drinking before 15.
Biological trait vulnerabilities: impulsivity, sensation seeking, high stress sensitivity (all have physiological markers in brain)
Neurotransmitter system. Lower D2 receptor availability may be a risk factor, because this presents a reduced protective effect. Lower D2 Receptors: make rewarding stimuli feel less satisfying and drive stronger seeking of external rewards.
What are the differences between DPDR and DID?
DPDR
No alters
Don’t need amnesia
Intact reality testing
DID
Need both alters and amnesia
Reality testing can be impaired
Often the result of severe, chronic trauma
Arguments for and against harm reduction model?
List some forms of harm reduction.
Pro
Prevents
Reduces
Connects people to
Decreases
Improves community
Reduces
Prevents ____
Engages people who... (and supports ____)
Against:
Enables
Communities worry that
Some believe resources should prioritize
______ objections:
Concerns that programs
Political resistance:
What does most empirical evidence support?
Arguments For Harm Reduction Interventions
(Supervised injection sites, methadone clinics, fentanyl test strips, wound care)
Benefits
Prevents overdose deaths (supervised sites intervene immediately).
Reduces infectious disease (HIV, hepatitis C) by reducing needle sharing.
Connects people to care (treatment, housing, medical services).
Decreases public disorder (less public injection, fewer discarded syringes).
Improves community safety (evidence shows no increase in crime).
Reduces stigma and increases trust in medical systems.
Cost-effective: prevents expensive emergency and hospital care.
Supports autonomy and engages people who are not ready for abstinence.
Arguments Against Harm Reduction Interventions
(These are common criticisms, even if not supported by evidence)
“Enables drug use” or sends the message that drug use is acceptable.
Communities worry these sites could increase local drug activity or crime.
Some believe resources should prioritize abstinence-based treatment only.
Moral objections: viewed by some as conflicting with traditional beliefs about addiction and responsibility.
Concerns that programs like safe supply or methadone replace one drug with another.
Political resistance: programs may be seen as controversial or difficult to fund.
Important note:
Most empirical evidence contradicts the negative claims—supervised sites reduce harm without increasing crime or encouraging new drug users.
How does the harm reduction framework differ from the abstinence-only framework?
For each, describe…
Goal
View of drug use
View of relapse
Engagement
Underlying philosophy (two words for each to sumamrize)
Goal
Harm Reduction: Reduce harm; survival first.
Abstinence-Only: Stop all use.
View of Drug Use
Harm Reduction: Drug use exists on a continuum; people deserve care regardless.
Abstinence-Only: Drug use must be eliminated for recovery to occur.
View of Relapse
Harm Reduction: Expected and planned for.
Abstinence-Only: Often seen as failure or noncompliance.
Engagement
Harm Reduction: Low-barrier, flexible, nonjudgmental.
Abstinence-Only: High-barrier; may exclude people who aren’t abstinent.
Underlying Philosophy
Harm Reduction: Pragmatism + compassion → keep people safe enough to survive long enough to stabilize.
Abstinence-Only: Morality + personal responsibility → recovery requires total cessation.
What are the benefits vs drawbacks of early intervention for psychosis/ schizophrenia? How do race/ demographics play into this debate.
Benefit philosophy
Overall message, plus
shorter duration of psychosis is…
If _______can be identified early, clinicians may ____ or _____ full psychosis.
Drawback philosophy
early diagnosis may be ______ (why?), and risk labels are _______ and _____.
Most at-risk individuals…
Risk of ______ and self _____
Risk of unnecessary ________
How do race/ other factors play into the debate
______ may be worse for minority groups. Why?
Early _______ symptoms are non specific and common in ______ (ex?)
Because biomarkers do not exist, clinicians may rely more heavily on…(3)
Based on readings for week 7
Side 1- Early intervention is beneficial: catch symptoms early, intervene quickly, and prevent worsening—similar to MI, stroke, and cancer treatment. This logic is intuitively attractive for illnesses like schizophrenia, which traditionally have poor long-term outlooks
Shorter duration of untreated psychosis is linked to better outcomes (longer untreated psychosis predicts worse functioning and symptom severity)
Additionally, if subtle symptoms can be identified early, clinicians may prevent or delay full psychosis and provide supportive care before major decline occurs.
Side 2- why early intervention may be harmful: early diagnosis may be extremely unreliable.
Early symptoms are nonspecific and highly common. Early symptoms (such as functional decline, odd experiences, anxiety, subjective cognitive changes) appear in depression, bipolar disorder, substance use, and young people who are simply stressed.
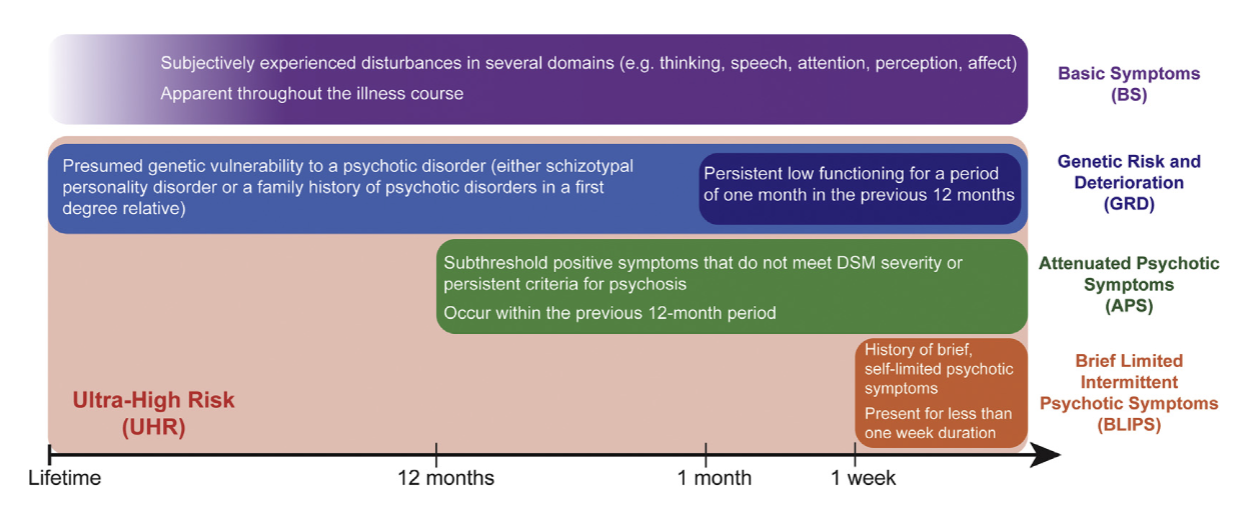
Risk labels are inconsistent and highly confusing (pictured)
Most at-risk individuals never even transition into psychosis (76% do not).
Risk of stigma, self-stigma, and psychosocial harm (shame, fear, lowered expectations, social withdrawal)
Risk of unnecessary exposure to antipsychotic medication.
How do race/ other demographic factors play into the debate?
Stigma may be worse for minority groups- most studies exclude ethnic minority groups, may be underestimating how harmful “at risk” labels are for minority communities
Early “psychosis like” symptoms are nonspecific and common in distressed populations. Minoritized groups disproportionately experience
trauma
immigration stress
social isolation
discrimination
Overpathologizing minority youth becomes more likely: Because reliable, validated biomarkers for psychiatric disorders currently do not exist and early symptoms are nonspecific, clinicians may rely more heavily on:
cultural assumptions
behavior interpreted through bias
communication differences
This increases the risk that minority youth are:
mislabeled,
overdiagnosed,
placed in at-risk programs unnecessarily
Explain how race plays into the diagnosis of schizophrenia versus mood disorders.
Obert meta-analysis results?
How much more likely to receive a schizophrenia diagnosis compared to white individuals?
Has this disparity changed over time?
Different reports of symptoms?
Black americans report more…
Perceptions from clinicians
Possible Explanations?
Obert meta-analysis results:
Black individuals were 2.42 times more likely to receive a schizophrenia diagnosis compared to white individuals. (strongest finding)
This disparity existed across both structured and unstructured methods (both rule based diagnostic approaches and informal interviewing)
Disparities have remained stable over time.
Reports of psychotic and mood symptoms differ in different racial groups
Black Americans report more psychotic symptoms, fewer manic symptoms, and more somatic symptoms. (go back to link on ppt slide 13)
Perceptions of psychotic (vs mood) symptoms differ for different racial groups
Clinicians are sometimes more likely to diagnose Black Americans with psychosis versus a mood disorder
Black Americans are also more likely to be hospitalized and receive higher antipsychotic doses.
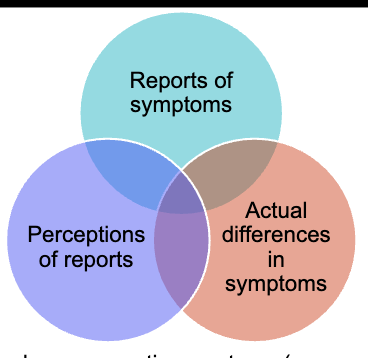
Difference in diagnosis results from differences in reports, perceptions, and actual differences in symptoms (so a combination of reasons)
Potential explanations: different cultural manifestations of symptoms, clinician bias, discrimination, poverty, less access to mental healthcare, social stigma.