Digestion - Stomach and Pancreas
1/25
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
26 Terms
Function and location of parietal cells
Secretion of HCl and intrinsic factor
Epithelial lining of stomach in gastric pits
Function and location of Enterochromaffin-like cell
Releases histamine
Gastric pit epithelium
Function and location of G cells
Produce gastrin
Gastric pit epithelia
Function and location of D cells
Produce somatostatin (which inhibits acid production)
Function and location of mucous neck cells
Secrete mucous and bicarbonate
gastric pit epithelium
3 molecules that stimulate gastric acid secretion
Gastrin
Histamine
ACh
Function and location of chief cells
Release pepsinogen - protein digesting enzymes
gastric pit epithelium
What is the endocrine signal that stimulate gastric acid production
Gastrin - is released by G-cells into blood, where it then reaches parietal cells
What is the paracrine signal that stimulate gastric acid production
Histamine - is released from a neighbouring gastric ECL (enterochromaffin-like) cell to the parietal cell
What is the neurocrine signal that stimulate gastric acid production
ACh - Is released from neurons of Vagus nerve to parietal cell
Most powerful acid secreting molecule
Histamine
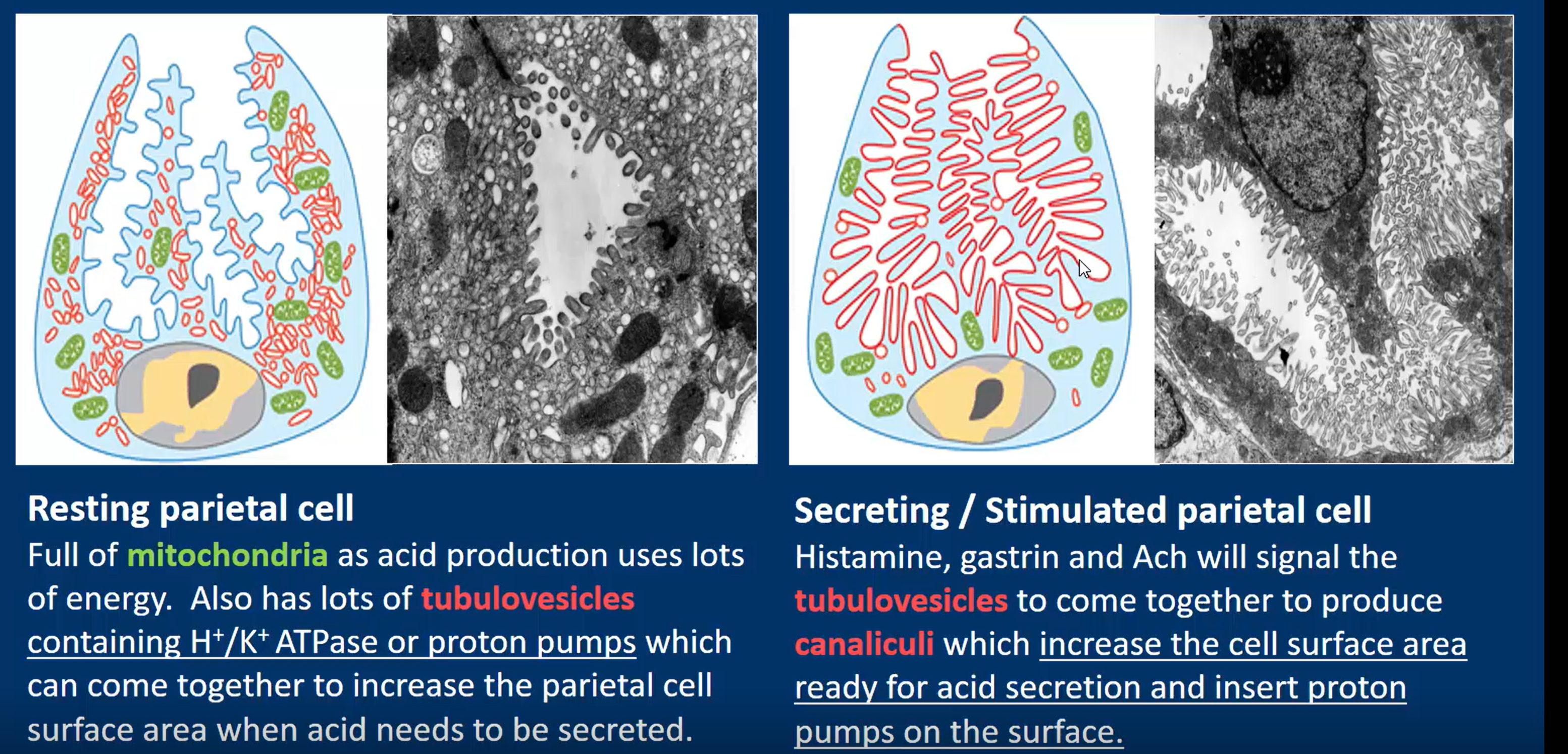
Structural differences between a resting, and stimulated parietal cell
resting
Full of tubulovesicles containing H+/K+ ATPase (proton pumps), which come together to increase surface area when required
Stimulated
Tubulovesicles come together to form canaliculi to increase SA, and insert proton pumps on the surface
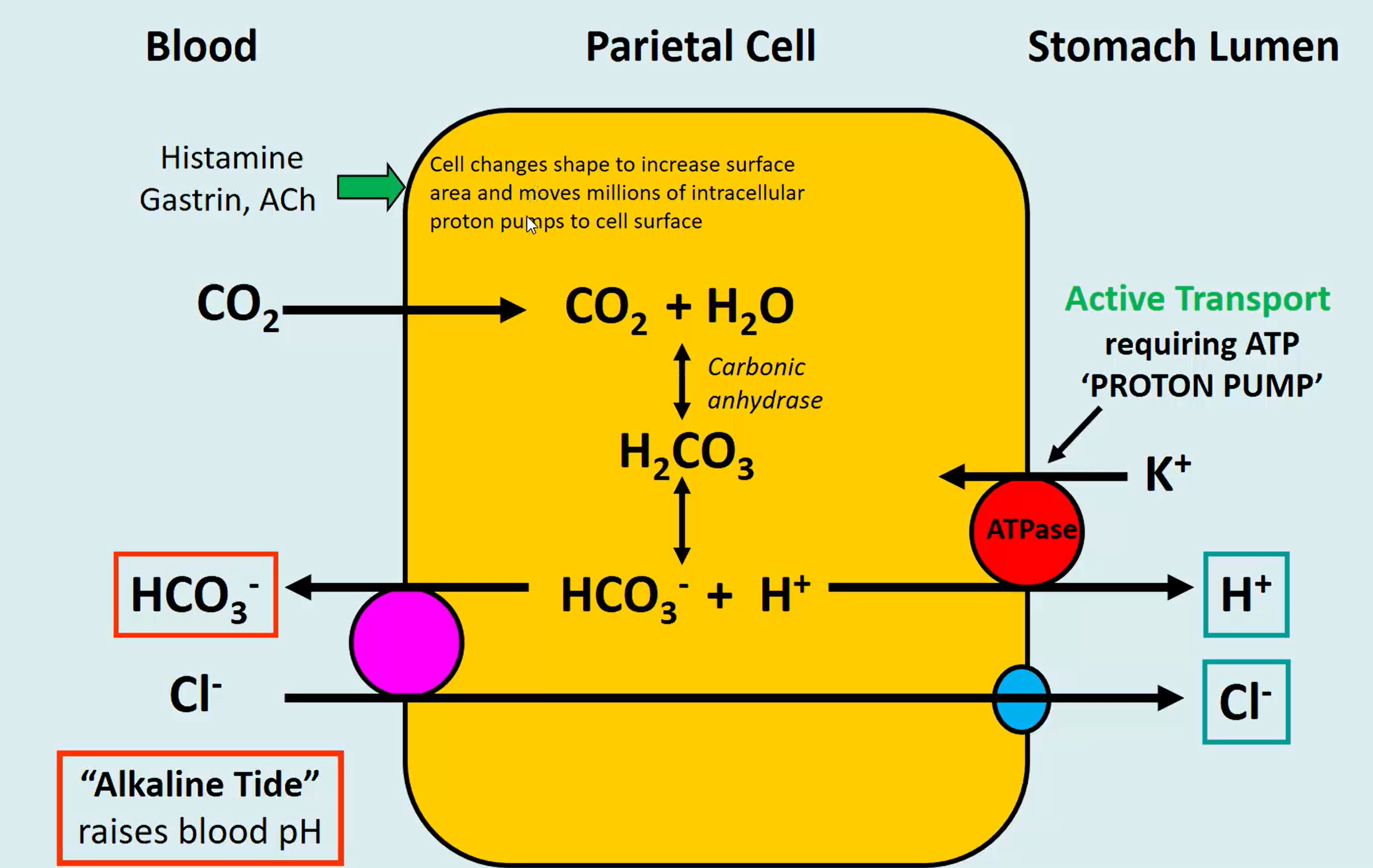
Why does blood pH increase when HCl is created
In the diagram is shows for every HCl made, it requires the movement of a HCO3 bicarbonate into the blood, thus raising the pH of the blood as it absorbs the circulating H+ ions in the blood. - this temporary rise in blood pH is called alkaline tide
3 phases of gastric secretion
Cephalic - brain
Gastric - stomach
Intestinal - intestines
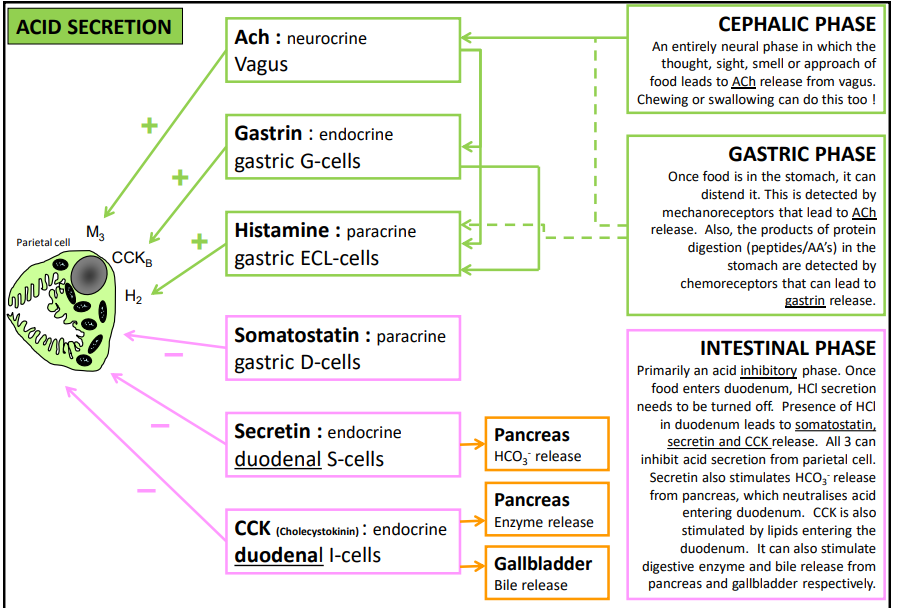
What happens in the cephalic phase and what triggers it
Neural trigger - sight/smell/thought of food, chewing and swallowing can also trigger this
Releases ACh
What happens in the gastric phase and what triggers it
Mechanoreceptors detecting stomach stretch and chemoreceptors checking for peptides and amino acids in stomach.
Releases gastrin
What happens in the intestinal phase and what triggers it
Inhibitory phase - triggered by HCl in duodenum.
Releases somatostatin, secretin, and CCK, all inhibitors of HCl production in parietal cell.
Extra CCK release can be triggered by lipid presence
CCK also stimulates HCO3- release, neutralising HCl in duodenum
Also stimulates digestive enzyme and bile release
Where do pancreatic juices and bile enter the duodenum?
Ampulla of Vater
Function of secretin
Stimulates bicarbonate release, to neutralise HCl, and inhibits HCl production via stimulating somatostatin release
What endocrine cells are in the pancreas and what do they produce?
Islets of Langerhands
produce somatostatin, glucagon, and insulin
What exocrine function does the pancreas perform?
Acinar cells release enzymatic juices into duodenum, which break down most digestible foodtypes
Duct cells secrete aqueous NAHCO3 solution
How is pancreatic secretion regulated?
Minor secretion during cephalic and gastric phases, as stimulation by vagal nerve fibres cause release of pancreatic juice
Acidic chyme causes secretin to release, and fatty/protein-rich chyme causes release of cholecystokinin (CCK). These molecules come from the enteroendocrine walls of the duodenum
CCK and secretin enter bloodstream
When CCK and secretin reach pancreas, they stimulate release of enzymatic pancreatic juice, and bicarbonate-rich juice respectively.
Functions of CCK
Stimulate gall bladder bile release
Stimulate enzyme-rich pancreas secretion
Stimulate HCO3- release
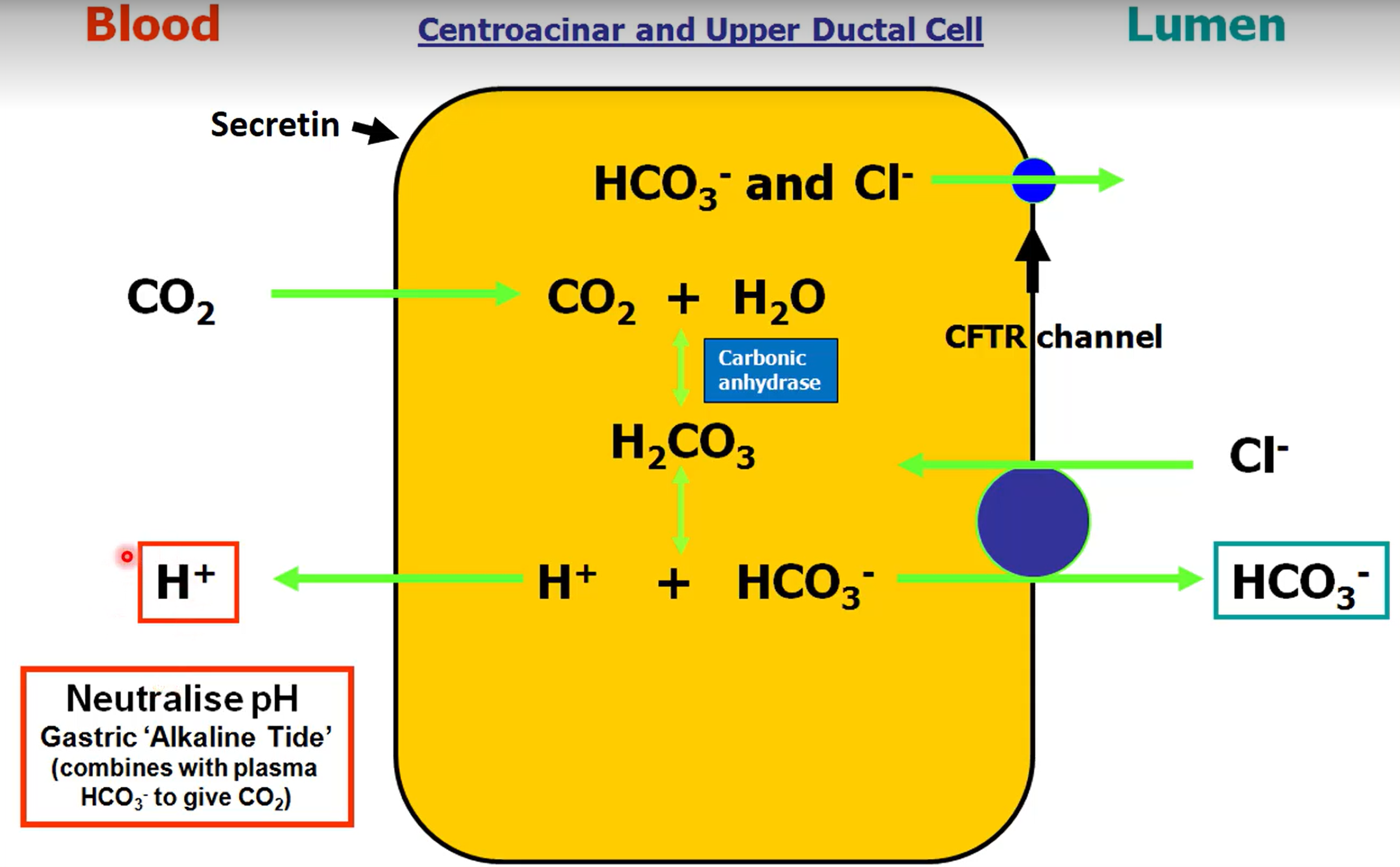
How does the duct cell in the pancreas neutralise alkaline tide
Duct cell create HCO3- molecules by breakdown of carbonic acid. It releases the bicarbonate into the lumen of the duct for release into duodenum, and releases H+ into the blood, neutralising the bicarbonate in the blood from acid production.
Why are pancreatic enzymes secreted as proenzymes (zymogens)
To prevent autodigestion of the pancreas.
When do the pancreatic zymogens become active enzymes, and what enzyme oes this
Trypsin causes the zymogens to become enzymes when they reach the small intestine