Derm Packet #4-Viral and Fungal Skin Infections
1/64
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
65 Terms
What is the etiologic agent of warts?
human papilloma virus (HPV)
How many serotypes of HPV are there?
over 100
non-gential warts
common (hands/feet), periungual (around fingernails and toenails), flat, filiform (long, threadlike), and plantar types
genital warts (condyloma acuminata)
strains 6 and 11 cause 90%
How many strains are high risk for cancer?
12, but 70% is caused by 16/18
common warts (verruca vulgaris)
dome shaped with irregular surfaces, common in children

Where are verruca vulgaris most common?
hands and knees, but can occur anywhere on the body
How are verruca vulgaris spread?
skin to skin contact, contact with contaminated surfaces, and autoinoculation
autoinoculation
refers to spreading a microorganism by contact with a lesion on one's own body
common wart treatment
-first-line treatment: salicylic acid (Compound W) apply to wart as liquid 1-2x a day (OTC and inexpensive)
-liquid nitrogen: two freeze-thaw cycles (one cycle is up to 3 min) are administered every 2-4 weeks for several visits
-surgical removal (scalpel) or laser therapy (vaporization of warts) only if recurrent
-benign neglect: leave them alone and sometimes they resolve on their own (could be 1-2 years)
*its common for viral infections to come back until immunity is built against it, so the warts could come back with any of these treatments*
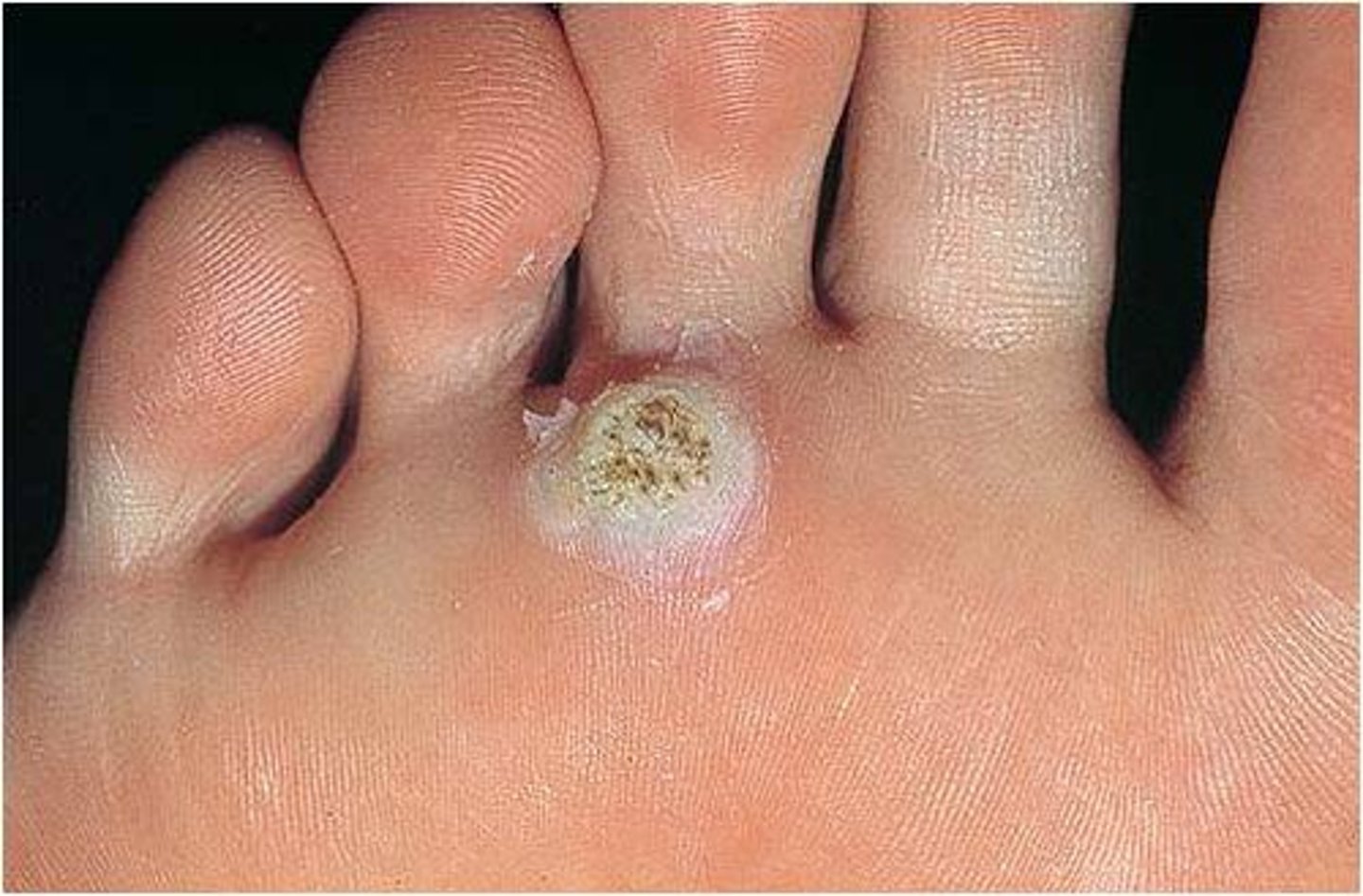
plantar wart
occur on the plantar surfaces of the feet. because of the forces on the feet from walking, the warts grow into the foot and become calloused (harder to treat, harder to eradicate)
can be very painful if walked on a lot
may resolve spontaneously with no therapy
in immunocompromised patients, may be widespread and intractable

Why are plantar warts so resilient?
every wart has its own supply of blood and nerves
solitary wart
on its own

mosaic wart
many, form patterns

plantar wart treatmemt
-cut duct tape size of lesion and leave in place for 6 days, remove, wash skin, and gently debride (this removes the oxygen), can be repeated until it goes away
-OTC topical salicylic acid preparations used for 8-12 weeks, cure rate is 75% (might be initial treatment)
-cryotherapy ablation with liquid nitrogen, cure rate is 50%
-prior to surgery/laser can scrape off calloused skin with a razor blade to help penetrate blood supply
-surgical removal/laser treatment (may still recur)
What treatment should not be used with diabetics?
salicylic acid
debride
rub off skin, specifically dead tissue
deep palmoplantar warts (myrmecia)
type of plantar wart characterized by a deeper, endophytic growth pattern and are often associated with HPV type 1, showing a distinct histological appearance with keratohyalin inclusions
flat warts
smooth, skin colored lesions that develop on the face, trunk, elbows, and knees

heck disease
is a cutaneous condition characterized by white to pinkish papules that occur diffusely in the oral cavity. It is caused by the human papilloma virus types 13 and 32.
buccal/gingival mucosal tissue, tongue/upper lip

condyloma acuminata
infection of genital or anal skin by HPV, lesions spread rapidly over moist areas as well as symmetric surfaces of the labia or rectum

What HPV serotypes are responsible for >90% of genital warts?
6 & 11
What do condyloma lesions look like?
lesions are pale pink to white, warty-like raised papules, may coalesce to form large cauliflower like masses
How to identify condyloma acuminata
identification may be difficult
use white vinegar (acetic acid) to bathe the suspected lesion. if acuminata, lesion will turn white
make sure to separate labia
pap smear, biopsy, colposcopy might be used to make the diagnosis (easier way to look at cervix if you think the cervix has warts)
condyloma acuminata treatmemt
podofilox (Condylox) is applied by pt twice daily x 3 consecutive days a week for cycles of 4-6 weeks
imiquimod (Aldara) 5% cream once daily on 3 alternate days per week for 8-12 weeks
surgical removal may be indicated in cases resistant to other treatments (usually last step)
electric cauterization
condyloma acuminata prevention
Gardasil: vaccine-most cases of cervical cancer are caused by genital warts
herpes simplex
viral infection, primary or recurrent, characterized by grouped vesicles on an erythematous base on skin or mucous membrane

types of herpes simplex
type 1 (HSV1) or type 2 (HSV2)
herpes simplex transmission
skin to skin, skin to mucosa, mucosa to mucosa (viral shedding)
herpes simplex primary infection
occurs with multiple, painful lesions, fever, lymphadenopathy, general malaise (might just not feel right)
herpes simplex secondary lesions
have similar lesions and symptoms but less severe, shorter duration, 1-2 weeks
prodrome
sometimes can tell outbreak is coming from tingling/itching
herpes simplex treatment
Acyclovir 200mg TT tab po TID x7-10 days (only comes in 200 mg tab)
Valacyclovir, Famcyclovir
What's another name for herpes zoster?
shingles
herpes zoster
decline in t cell mediated immunity to VSV (varicella zoster virus), reactivation of varicella virus due to cold, stress, age, medical conditions

herpes zoster symptoms
unilateral pain (key to this, pain doesn't cross midline), vesicular lesions limited to a dermatome, pain/burning.itching will often precede rash (1-5 days), presents as clustered vesicles of varying sizes, lesions do not cross midline of the body, lesions continue to develop for 3-5 days, scab over in approx 10 days
herpes zoster treatment
Acyclovir 800mg 5x per day x 7 days, valacyclovir, famcyclovir
give within 72 hours of symptoms to prevent post-herpetic neuralgia and shorten course
pain management incudes topical cream, Tylenol, advil, narcotics (don't love to use narcotics cuz tolerance/addiction)
post herpetic neuralgia
continuance of pain, burning after lesions go away, pts might take meds/ go away on own, pts still have bad pain to nerve root, lasts > 3 months after lesions resolve
most common complication, risk increases with age
herpes zoster complications
herpes zoster ophthalmicus, Ramsay-Hunt syndrome, post herpetic neuralgia, encephalitis
herpes zoster ophthalmicus
goes into eye, needs to go to optomologist

ramsay-hunt syndrome
facial nerve affected, not common, paralysis/hearing loss

encephalitis
inflammation of the brain
herpes zoster prevention
zostavax: shingles vaccine recommended by CDC for pts over 60 for routine immunization, helps reduce the risk of developing shingles and post herpetic neuralgia
vaccination against varicella: chicken pox vaccine, most pts won't remember if they had it or not since they were most likely children
fungal skin diseases
superficial fungal infections are the most common of mucocutaneous infections
two common groups of fungal skin diseases
dermatophytes and candida (yeast)
dermatophytes
unique fungi that infect nonviable keratinized cutaneous structures
What's another name for dermatophytes?
tinea
How are dermatophytes classified?
according to their site of infection
tinea corporis
presents as irregularly shaped scaly patches and plaques, often with a raised erythematous border and central clearing, occurs on the trunk arm and leg, may be a single lesion or multiple lesions, more commonly known as ringworm

tinea corporis treatment
topical antifungals (cream/lotions)
tinea capitis
"ringworm" of the scalp, usually occurs in children from 2-10 years old
wide range of presentations including, scaling, broken hair, painful inflammation and possible scarring alopecia
make sure to separate all hair and take time with PE

alopecia
hair loss
tinea capitis treatment
oral antifungals (topical antifungals only if hair is short and only small areas affected, long hair won't be penetrate-able with topicals_
tinea pedis
dermatophyte infection of the feet, "Athlete's foot"
erythema, scaling, erosions, macerations, and/or bullae
often asymptomatic, but may be associated with itching

tinea pedis prevention
use of shower shoes in public facilities, keep feet dry
tinea pedis treatmemt
topical antifungals
tinea cruris
dermatophytosis of the groin, pubic regions, and thigh, lesions are large, scaling well demarcated dell red to brown plaques, asymptomatic or mild itching

What is tinea cruris called in men?
jock itch
predisposing factors of tinea cruris
jumidity, tight clothing, obesity
tinea cruris treatment
topical antifungals
list of topical antifungals
Clotrimazole twice daily, OTC
Econazole (spectazole) once daily, Rx only
Ketoconazole once daily, Rx only
Miconazole twice daily, OTC
candida
fungal infection caused by yeast, most commonly candida albicans, but can also be candida globerata or candida tropicalis
candidal infections can affect any anatomical structure
the very young and very old are at greatest risk, as well as those with compromised immune systems
thrush
oral candiditis treated with medicated mouth wash

intertrigo
candida infection in the intertriginous areas (two skin surfaces rub together)
rash begins with vesiculopustules which rupture, causing maceration
lesions coalesce and satellite lesions are visible near the margins

intertrigo treatment
topical: nystatin, clotrimazole
oral: fluconazole (difclucan) 1 day pill, 150 mg