MIC: Lecture Ch 17 - Immunization and Vaccination
1/52
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
53 Terms
What are the types of acquired immunity
Natural: active and passive
Artificial: active and passive
what is naturally acquired active immunity
immunity develops after antigens (e.g. microbial pathogens) enter the body by natural processes (like infections) and in response, the body’s immune system forms antibodies and memory cells
how does naturally acquired active immunity respond
by forming antibodies and memory cells
what are the length of immunity for naturally acquired active immunity
- life long immunity: smallpox, measles, chickenpox, yellow fever
- immunity may be lost after only a few years: diphtheria, tetanus
- immunity may be lost for a lesser period: influenza, pneumonia
what is naturally acquired passive immunity
when antibodies produced in the body of an individual (mother) are naturally transferred into the body of other individual (child)
what types of antibodies are transferred from mother to infant
IgA antibodies are transferred from mother to infant in breast milk during nursing
what are IgA antibodies also called and how long do they live
called maternal antibodies → IgA antibodies are short lived and most will remain with the child for ~3-6 months
what is artificially acquired active immunity
when a carefully chosen antigen (e.g vaccine, toxid) is intentionally introduced into a body to be immunized
why is artificially acquired active immunity artificial and active
artificial because the antigens are intentionally or purposely introduced
active because the recipient’s immune system synthesizes antibodies
what is artificially acquired passive immunity
known as antibody therapy, by the introduction of antibody-rich serum (blood plasma devoid of clotting factors) taken from diseased individual who has recovered and given to a susceptible individual currently with disease.
*referred to as monoclonal or convalescent therapy
what type of response do the antibodies in artificially acquired passive immunity allow for
an immediate response from the individual with the disease, but the presence of the antibodies is only 2-3 weeks
what type of immunity are anti-serum and anti-venom
delivered as a form of artificially acquired passive immunity
what are examples of protections from artificially acquired passive immunity
- viral diseases like hepatitis B, chickenpox, COVID-19
- bacteria diseases like botulism, diphtheria, tetanus, staphylococcal poisoning, where toxins are involved in disease causation
how is antivenom produced
using horses injected with small amounts of venom, which causes production of antibodies
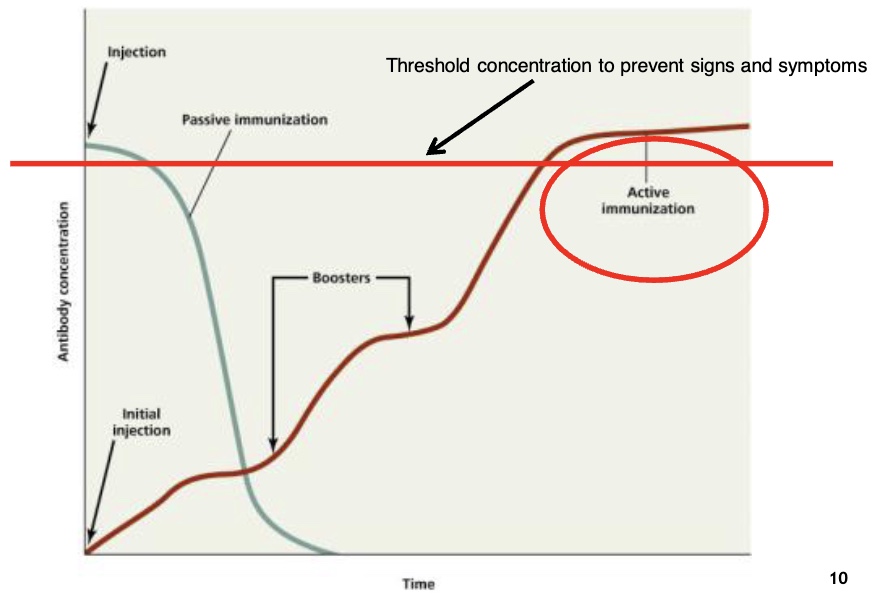
where is passive immunity on the threshold when first injected
right above threshold with no signs and symptoms
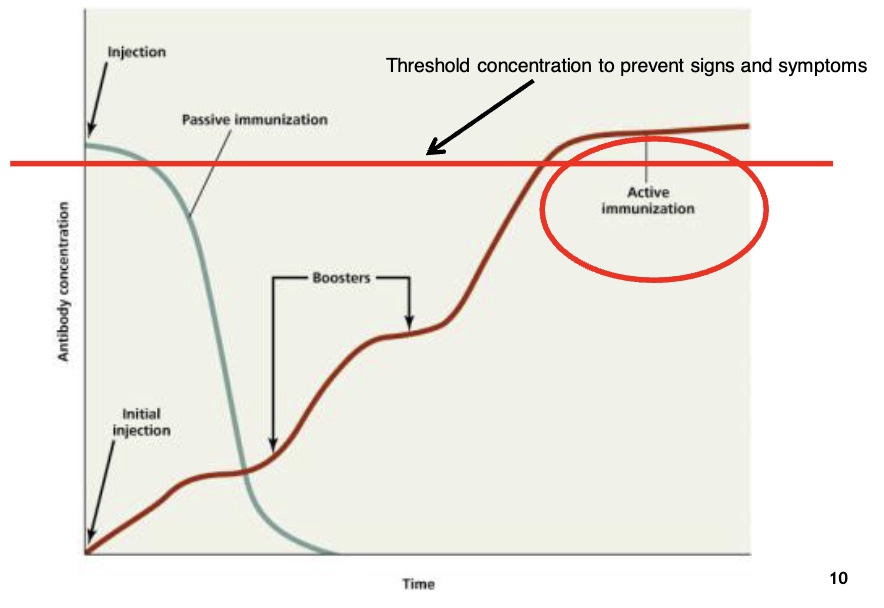
where is active immunity on the threshold when first injected
below threshold and needs boosters to get it all the way to active immunization and above threshold to prevent signs and symptoms
what are the general types of vaccines
- attenuated (live, weakened)
- killed (inactive)
- subunit/toxoid
- vector based recombinant
*vaccines do not prevent contamination/infection, it prevents symptoms
what was the history of smallpox vaccine
Edward Jenner used variolation (the first treatment regimen for smallpox where material from smallpox sore is introduced into healthy individuals) and decreased the small pox break out
what was the standard method of vaccination in the UK
calf lymph/cowpox postules
→ concept: attenuated live viruses
what is virus subtypes determined by
the H and N antigen on the surface of the virus → 15 variations of H and 9 variations of N
what does it mean for the parts of the antigen that vary from strain to strain with the flu
each flu season, the epitopes will be different, so the antibodies from the previous year’s vaccine will not bind (shown by the blue region)
what does it mean for the parts of the antigen that are conserved from strain to strain with the flu
each flu season, the epitopes are similar to the previous year’s virus and the antibodies from the previous year’s vaccine should bind BUT this region does not prevent the binding of the virus to the host cell (shown by the red region)
what is an attenuated (live, weakened) vaccine
microbe that has been cultivated under conditions that disable their virulent properties (humoral and cell mediated response)
what are the 3 methods to design an attenuated vaccine
remove virulence genes from microbe
use closely-related but less dangerous organisms to produce a broad immune response (cowpox will offer immunity for smallpox)
microbe has been cultivated under different conditions
what happens when microbe has been cultivated under different conditions in attenuated vaccine
culturing the microbe in alternative cell lines with closely related receptors, microbe will learn to grow better nonhuman cell lines, and when exposed to human cells, the microbes will slowly replicate and the immune system will be able to build a strong response
what is the #1 producer of eggs
pharmaceutical industry because they harvest viruses in eggs and replicate them
what are killed/inactivated vaccines
contained killed, but previously virulent, microorganisms that has been inactivated with chemicals or heat → it stimulates humoral immunity that will create a response to multiple epitopes of the microbe
what do killed/inactivated vaccines stimulate
the humoral response will create a response to multiple epitopes of the microbe. It stimulates a TH response that promotes antibody-mediated immunity
what must killed/inactivated vaccines not do
must no change the shape of antigens (epitopes) of the microbe.
*heat can cause proteins to misfold and change shape
why are killed/inactive vaccines safer but less effective
safer because organisms cannot replicate or mutate
less effective because the immune system will only create 1 humoral response, unless boosters are given → must give multiple doses (boosters) to get achieve active immunity
what is the manufacturing process of killed/inactivated vaccine
virus → live cells → virus inactivated by chemicals → purification and impurity removal → vaccine stock in bulk → filling and packaging
what are subunit vaccines
antigenic fragments (proteins) of microbe can create an immune response (a small piece of the microbe)
what must subunit vaccines be able to do
elicit an immune response to protect the individual from signs and symptoms
what are the protein subunits of hepatitis B and HPV of subunit vaccines
Hepatitis B: composed of viral envelope protein
Human papillomavirus (HPV): composed of capsid protein
what are modified toxins of subunit vaccines
tetanus, diphtheria, rattlesnake toxoid (dogs)
what does a subunit vaccine stimulate
antibody-mediated immunity
why are subunit vaccines safer but less effective
safer because no risk of replication
less effective because it requires multiple doses (boosters)
what is vector based recombinant vaccines
the genes for antigens of pathogens inserted into non-pathogen → non-pathogens are injected into an individual and will express the genes from the pathogen to elicit an immune response
*johnson and johnson uses adenovirus vector vaccine
what is the vaccinia virus
cowpox infection that has uniquely large DNA genome for a virus that is required to express its genes. It protects the person against lethal smallpox infection
what is the current vector based research trying to do
attempting to clone multiple genes from different pathogens into Vaccinia virus to offer immunity to smallpox, bacillus anthracis (anthrax), human papillomavirus (HPV), human immunodeficiency virus (HIV), herpes simplex
what are the 2 types of cancer vaccines
- vaccines that protect an individual from a viral infection that can result in cancer such as HPV or Hepatitis B (subunit vaccine)
- vaccines that treat existing cancer, called treatment vaccines or therapeutic vaccines → work to boost body’s immune system, and elicit a cell mediated response known cancer antigens
why does the Vaccinia virus need a uniquely large DNA genome and what roles does it play
it’s required to express its genes:
- required for encoding various enzymes and proteins
- involved in viral DNA replication and gene transcription
- express attachment proteins
why do researchers need to clone genes from other organisms into the Vaccinia virus
to create antigens for immunity
what are the methods of administration for a vaccine
direction injection, inhalation or nasal spray, oral, subcutaneous
what is direct injection (method of administration)
direct into bloodstream or intermuscular but will not induce secretory antibodies in mucus membranes → stimulate immune response in lymph nodes
what is inhalation or nasal spray (method of administration)
- fast method, easy, but tends to not make it to bloodstream, very little response in lymph nodes
- may induce secretory antibodies (IgA) in mucus membranes
what is oral (method of administration)
- must not be deactivated by low pH of stomach acids and be able to diffuse from intestine/stomach
- may induce secretory antibodies (IgA) in mucus membranes
what is subcutaneous (method of administration)
- induced just under skin (epidermis)
- allows microorganisms to replicate locally and NOT throughout body
- can induce a systemic immune response
what is the importance/drawback of direct injection of a vaccine
- it will place the antigens in the tissues and elicit an immune response in the lymphatic system
- drawback: it will allow microbe into the body and the immune system will start its protection in the lymphatic system
what is the importance/drawback of inhalation/oral vaccine
- it will place antigens in the mucus membrane
- this could elicit a localized response by M-cell and Peyer’s patch
- this would activate B-cells to produce IgA antibodies in mucus membranes, preventing microbe from crossing mucus membrane
- drawback: mucociliary clearance of the vaccine, thus, low level response
what are vaccine safety and problems
- general side effects: interferon response
- residual virulence: attenuated vaccine - can become pathogenic
- vaccine recalls: gardasil (HPV) and covid-19 J&J vaccine
- contamination: 2004 flu vaccine contamination
- public misconceptions: like with Jenny McCarthy and MMR vaccine causing autism
- stability: always an issue
- allergic reaction
- research cost/government
what is herd immunity (does everyone need to be vaccinated)
describes a type of immunity that occurs when the vaccination of a portion of the population (or heard) provides protection to unprotected individuals
→ higher proportion of individuals who are immune = lower likelihood that a susceptible person will contact infectious individual
what type of vaccine is the COVID 19 BioNTech/Pfizer/Modern
mRNA, which contains a lipid container hold mRNA