Pharmacology, Therapeutics, and Prescribing
1/80
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
81 Terms
What term describes:
A chemical substance, typically of known structure, which, when administered to a living organism, produces a biological effect?
Any substance (other than food) used to prevent, diagnose, treat or relieve symptoms of a disease or abnormal condition?
Drug
What term describes a drug formulated (developed with other ingredients) to prevent, diagnose, treat or relieve symptoms of a disease or abnormal conditions?
Medicine
What term describes:
The safe and effective use of medicines within healthcare?
Applied pharmacology, i.e. application of pharmacology to patient care?
Therapeutics
What term describes:
To say what treatment someone should have?
To lay down, in writing or otherwise, as a rule or a course of action to be followed?
Advise or authorise the use of (a medicine or treatment) for someone, especially in writing?
To say what medical treatment someone should have?
To tell someone what they must have or do, or to make a rule or something?
Patient-centred prescribing: putting the patient at the centre of everything we do as clinicians?
Prescribing
What term describes labelling from stock & supplying a clinically appropriate medicine to a patient/client/carer, usually against a written prescription, for self-administration by another professional, and to advise on safe & effective use?
Dispensing
What term describes the giving of a drug by one of several means (outlets), e.g. oral?
Administration
What term describes testing the measurement of specific drugs and/or their breakdown products (metabolites) at timed intervals?
Monitoring
What term describes a specific, measured quantity of a medicine, nutrient, or pathogen that is delivered as a unit and is taken or recommended to be taken at one particular time?
Dose
What term describes the physical form that medication is used in e.g. tablet, cream, ointment?
Dosage form
What term describes the process in which different chemical substances, including the active drug, are combined to produce a final medicinal product; the components of a medicine?
Formulation
What term describes the location at which the drug is administered e.g. oral or intravenous?
Administration route
What term describes the location at which the drug is administered e.g. oral, intravenous?
Administration route
What term describes how often a patient takes medication?
Frequency of administration
What term describes the frequency (dosing interval) and dose at which a drug is to be administered; the specific schedule of doses of a medicine administered to patients?
Dosage regimen
What term describes a medicine that is patented and sold under the company that developed it?
Branded medicine
What term describes the copy of a branded medicine?
Generic medicine
Which administration route is by mouth?
Oral (PO)
Under the tongue?
Sublingual (SL)
Between the gums and cheek?
Buccal (bucc.)
Through the anus into the rectum?
Rectal (PR)
Into the vaginal cavity?
Vaginal (PV)
Directly to the skin?
Topical (top.)
By routes other than the digestive tract i.e. injection or infusion?
Parenteral (intradermal (IM), subcutaneous (SQ), intramuscular (IM), and intravenous (IV))
Directly to the airways?
Respiratory (inhalation/nebulisation routes)
Through the nose?
Nasal
Into the eyes?
Ocular (occ.)
(Left eye - l.e., right eye - r.e.)
Into the ear?
Optic
Give nine different types of oral dosage forms
Tablet
Capsule
Solution
Granule
Dry powder
Suspension
Emulsion
Syrup
Gel
A solution is?
Water-based
A syrup is?
Glucose-based
What must you do a suspension?
Reshape often to prevent build-up at the bottom of the bottle
What must you do to an emulsion?
Reshake before use
What is in a tablet?
Binder
Disintegrating
Preservative
Lubricant
Which component of a tablet helps break it down?
Effervescent
Which component of a tablet improves the flow of powders by reducing friction between the tablet and metal surfaces during compression and ejection?
Lubricant
What are five advantages of oral administration?
Patient preference (painless, easy, portable)
Cheap (to both manufacture and administer)
Variety of dosage forms available
High dose is possible
Can use modified release approaches (where drug release from medicine changes over time)
What are three disadvantages of oral administration?
Not suitable for particular patients e.g. unconscious
Extensive first-pass metabolism, which may require large doses to achieve desired therapeutic effect
Give ten different types of topical dosage forms
Cream
Ointment
Lotion
Paste
Gel
Solution
Aerosol
Foam
Patch
Shampoo
What type of emulsion is cream?
Oil-and-water (O&W)
50/50 ratio
What type of emulsion is ointment?
Water-in-oil (W/O)
What type of emulsion is lotion?
Oil-in-water (O/W)
A paste is?
Semi-solid
A gel is?
More aerated
What is solution suspended in?
Water or other thin liquid
What term describes the scientific study of the action & effects of drugs on living systems and the interaction of drugs with living systems?
Pharmacology
What term describes the branch of pharmacology concerned with the effects of drugs and their mechanism of action?
Pharmacodynamics
What term describes the branch of pharmacology concerned with the movement of drugs within the body?
Pharmacokinetics
Give the four main types of drug receptors
G-protein coupled receptors
Ligand-gated ion channels
Intracellular receptors
Tyrosine kinase-coupled receptors
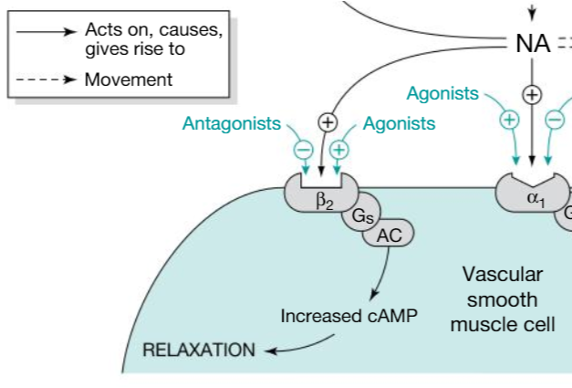
Give an example of a drug that acts on G-Protein coupled receptors and what it is used for
Drug: Salbutamol
Use: Treats asthma
Explain the five steps that occur when salbutamol binds to G-Protein coupled receptors
Bind to the ß2 adrenoceptor
G Protein-Couple receptor mediated activation of Adenylate Cyclase
Increase Cyclic AMP (cAMP)
Activation of Protein Kinase A (PKA)
Smooth muscle relaxation (dilation of bronchioles)
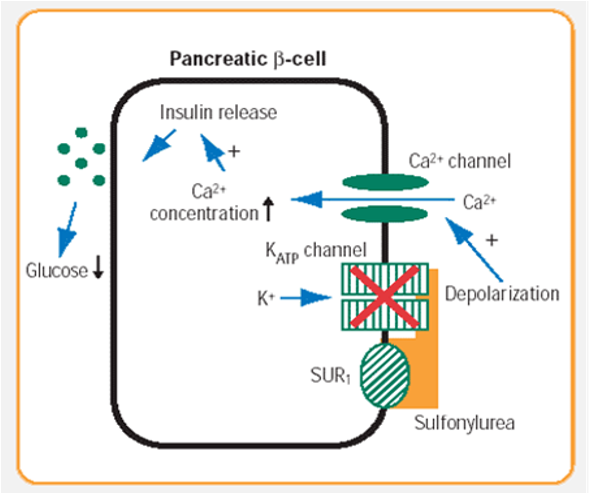
Give an example of a drug that binds to ligand-gated ion channels and its use
Drug: Sulfonylureas
Use: Treats type 2 diabetes
Explain the four steps that occur when sulfonylureas binds to ligand-gated ion channels
Bind to KATP channels, closing them and preventing movement of potassium out of the cell
Resultant depolarisation leads to influx of Ca2+ ions
Increased intracellular calcium ion concentration leads to increased insulin release
Increased insulin levels leads to reduction in glucose level
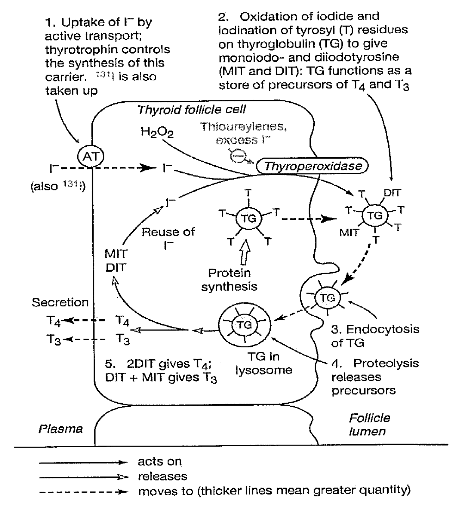
Give an example of a drug that binds to intracellular receptors and its use
Drug: Thionamide
Use: Inhibits thyroid hormone synthesis (treats an overactive thyroid by stopping it from producing excess hormones)
Explain the three steps that occur when thionamides bind to intracellular receptors
Inhibition of ‘Thyroperoxidase’
Reduced oxidation of iodine and iodination of tyrosyl residues on thyroglobulin, leading to less MIT and DIT
Less MIT and DIT = less T3 and T4 (two hormones which contribute to homeostatic regulation)
Give the four stages of pharmacokinetics
Absorption (and bioavailability)
Distribution
Metabolism
Elimination
ADME
Which term describes the transportation of the un-metabolised drug from the side of administration to the circulatory system (i.e. blood vessels)?
Absorption
What term describes the extent (how much) and rate (how quickly) to which an active drug is absorbed from the medicine and reaches systemic circulation?
Bioavailability
What can also impact absorption?
Food/drink
What term describes the disbursement of an un-metabolised drug as it moves through the body’s blood and tissues?
Distribution
Drugs do what depending on their chemical structure and other factors?
Distribute in different amounts into different parts of the body
Drugs distribute in different amounts into different parts of the body depending on what?
Their chemical structure and other factors
What term describes the chemical alteration of drugs by various bodily systems to create compounds which are more easily excreted from the body?
Metabolism
Where does metabolism mostly take place?
In the liver via enzymes following absorption
Where can metabolism also take place in?
Other organs e.g. GI wall and kidneys
Metabolism is an?
Evolutionary ‘protective’ measure known as ‘first-pass metabolism’
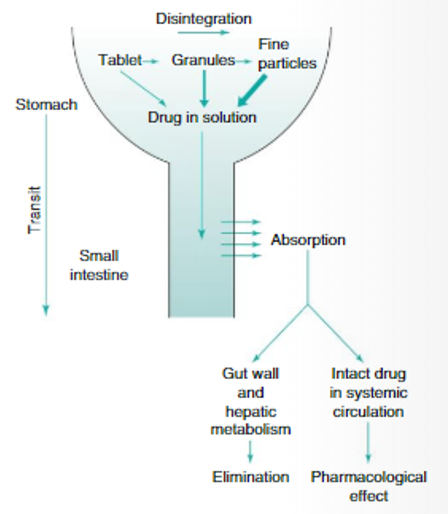
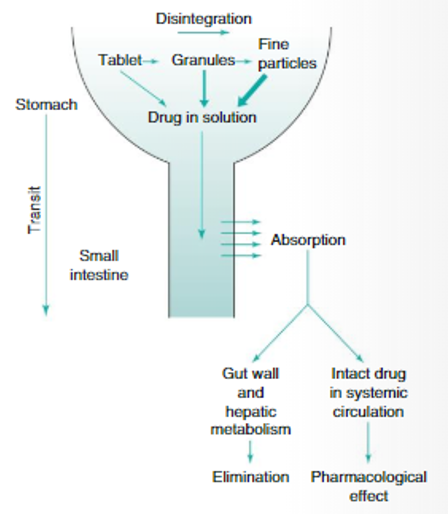
What term describes the metabolism of a drug in the gut wall or liver before it enters the systemic circulation(, meaning only a proportion of the drug reaches the circulation)?
First-pass metabolism
Where does the absorbed drug first enter in first-pass metabolism?
The portal vein which leads to the liver
→ Then enters ‘systemic circulation’ i.e. the rest of the body
In metabolism, the original drug molecule and/or metabolites are?
Pharmacologically active
What term describes the removal of an administered drug from the body (either in the un-metabolised or metabolised form)?
Elimination
Where does elimination mostly occur?
Via the kidneys (renal)
Where does elimination occur to a lesser extent?
Via:
Perspiration (sweat)
Tears
Saliva
Respiration
Milk
Faeces
Bile
Beyond absorption…
…distribution, metabolism, and elimination happen…?
Simultaneously at varied rates i.e. speed, which is affected by many factors
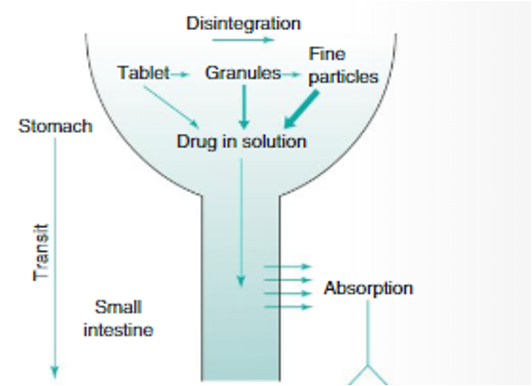
Explain the four steps that occur during absorption of a paracetamol tablet
Tablet swallowed
Tablet disintegrates in the stomach, where the drug (paracetamol) dissolves in gastric fluids i.e. drug is in solution
Drug (paracetamol) in solution passes into the small intestine
Drug absorbs across the wall of the small intestine
Explain the three steps that occur during distribution of a paracetamol tablet
Some of the absorbed paracetamol reaches systemic circulation (i.e. blood vessels) straight away
Via blood vessels, the drug then ‘distributes’ into extracellular fluids (i.e. leaves blood vessels) where it can interact with receptors
This drug-receptor interaction exerts the pharmacological effect
Explain the three stages that occur during metabolism of a paracetamol tablet
Some of the paracetamol is metabolised in the gut wall after it crosses the gut wall
Some of the absorbed paracetamol is metabolised in the liver before it even enters systemic circulation (i.e. blood vessels)
Most remaining paracetamol which reaches systemic circulation (i.e. blood vessels) is eventually metabolised by the liver
Explain what occurs during elimination of a paracetamol tablet
Of the administered dose, all is excreted via the kidneys as urine
During elimination, in the urine, what percentage of the original dose of the paracetamol tablet are metabolites?
95-98%
During elimination, in the urine, what percentage of the original dose of the paracetamol tablet is the original paracetamol molecule?
2-5%
What is the liquid portion of the blood called?
Plasma
What components of the blood are suspended (‘held in’) plasma?
Red blood cells
White blood cells
Platelets
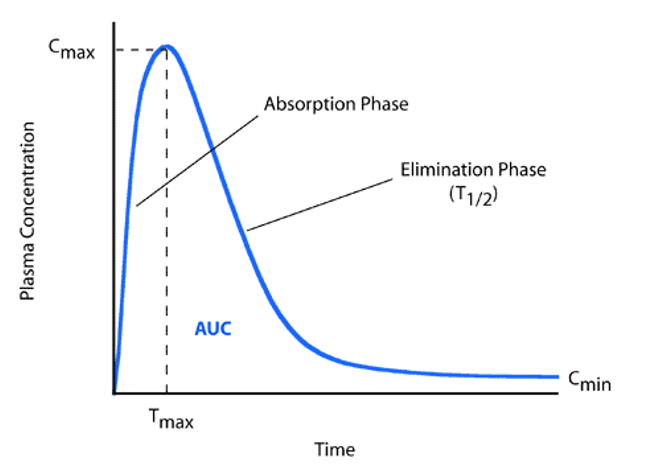
What does the plasma concentration/time curve shows?
The amount of drug in plasma (plasma concentration) and how that changes over time